Investigation of the Therapeutic Potential of Organic Nitrates in Mortality Reduction Following Acute Myocardial Infarction in Hyperlipidemia Patients: A Population-Based Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Inclusion
2.2. Study Cohorts
2.3. Assessment
2.4. Data Analyses
3. Results
3.1. Baseline Characteristics
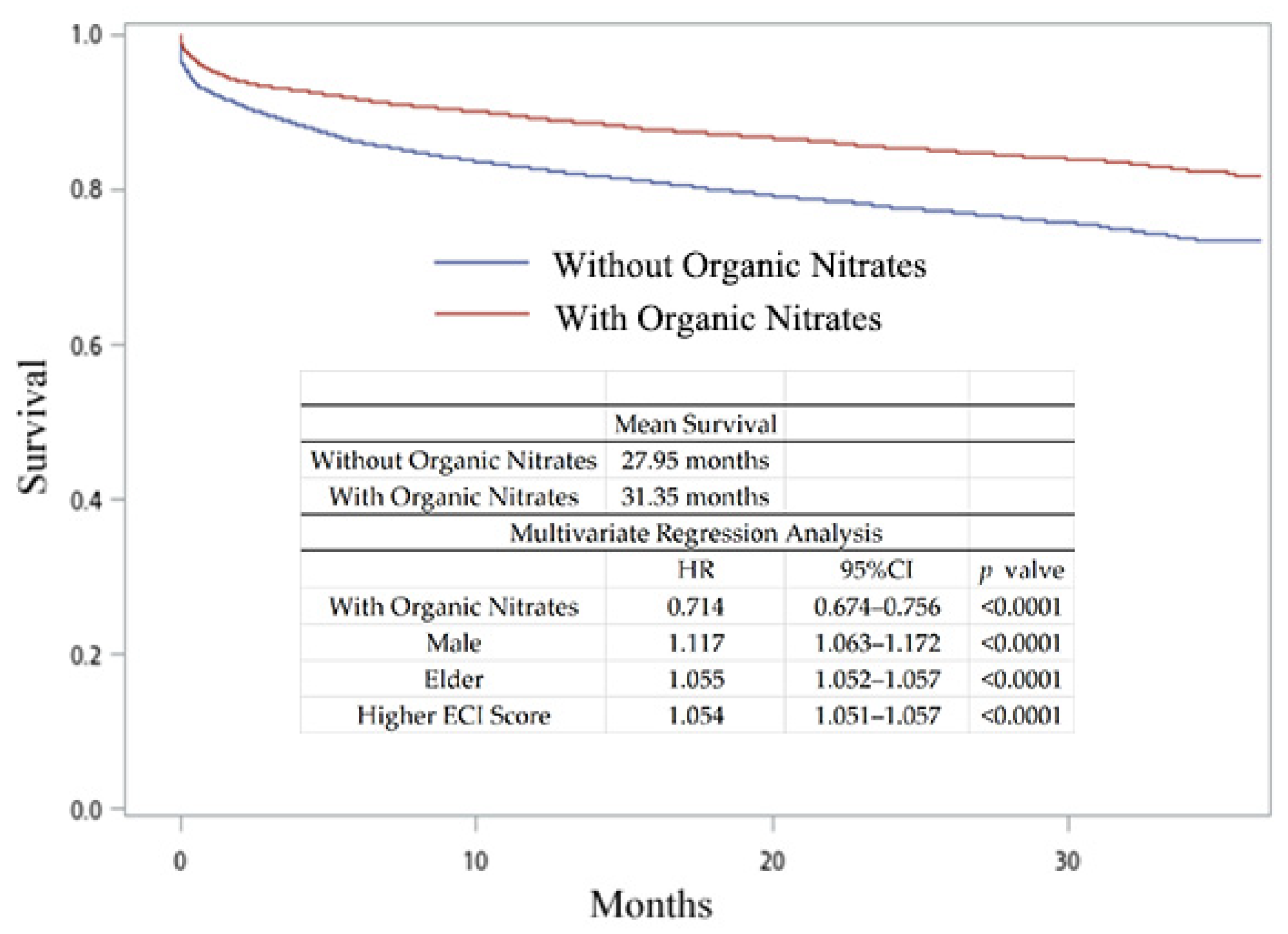
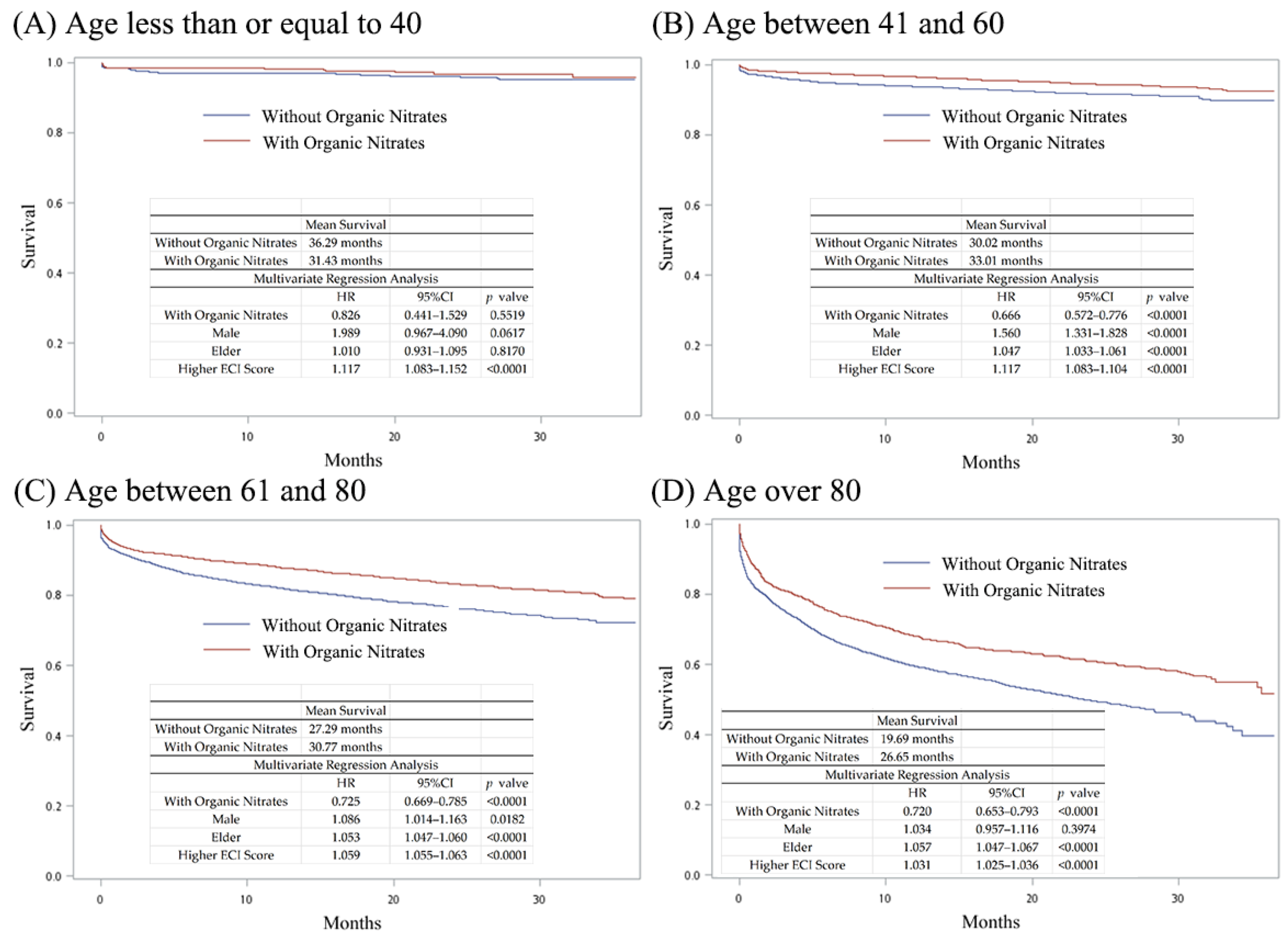
3.2. Medication Usage of Hyperlipidemia Patients with AMI and Their Survival with or without Organic Nitrates
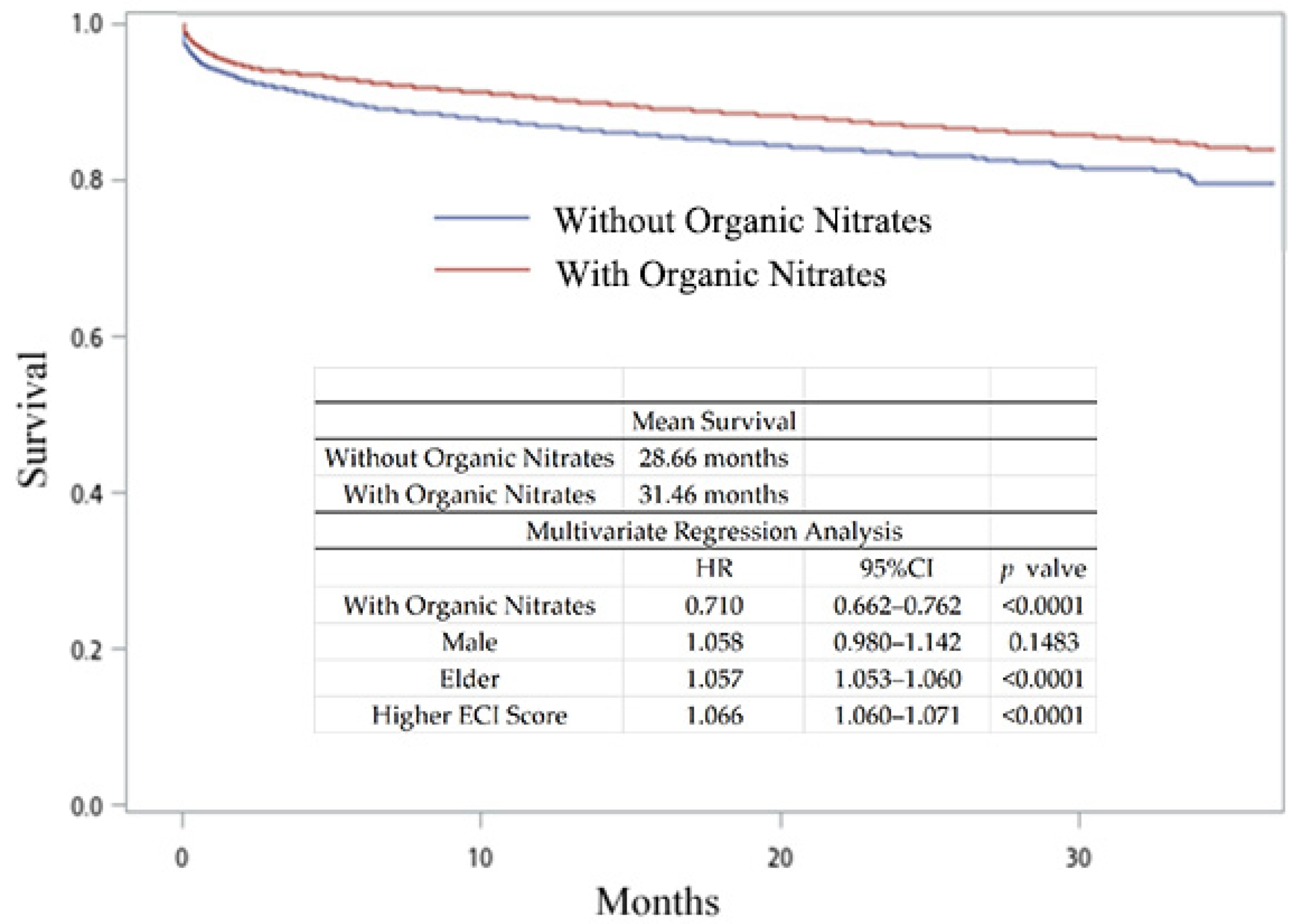
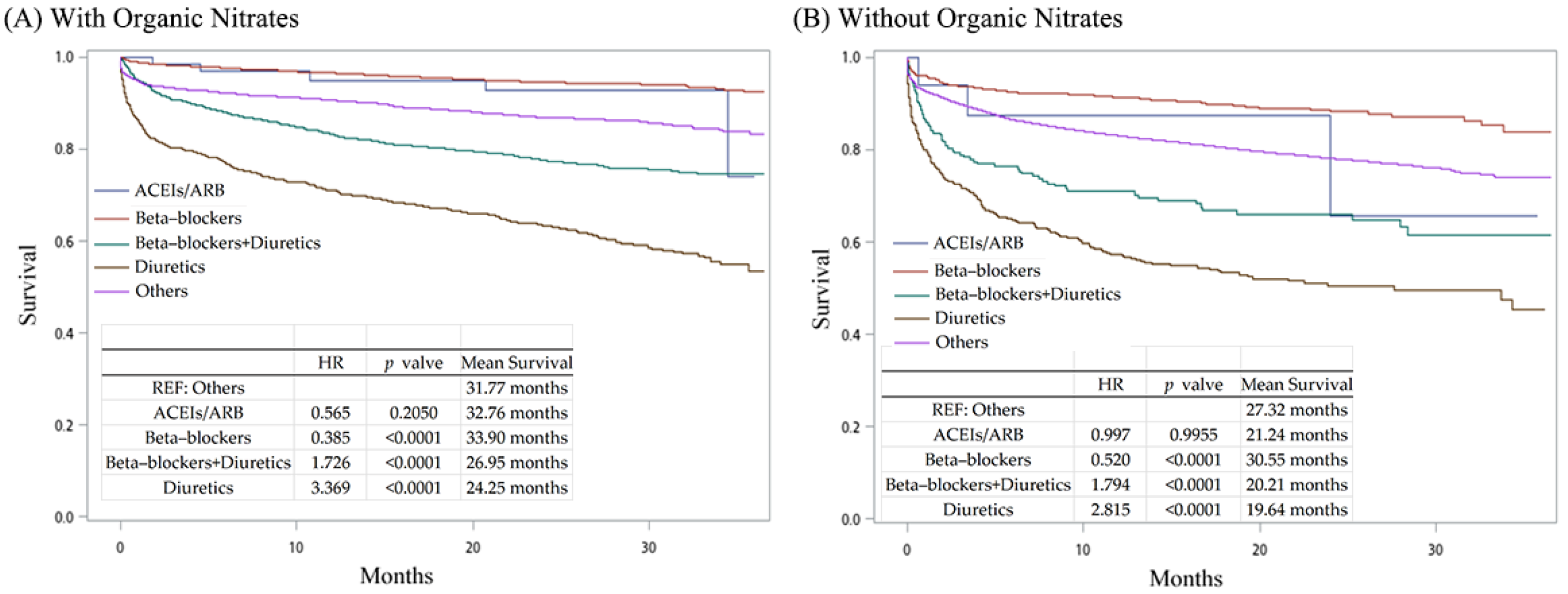
3.3. Survival of Hyperlipidemia Patients with AMI Prescribed Different Treatments
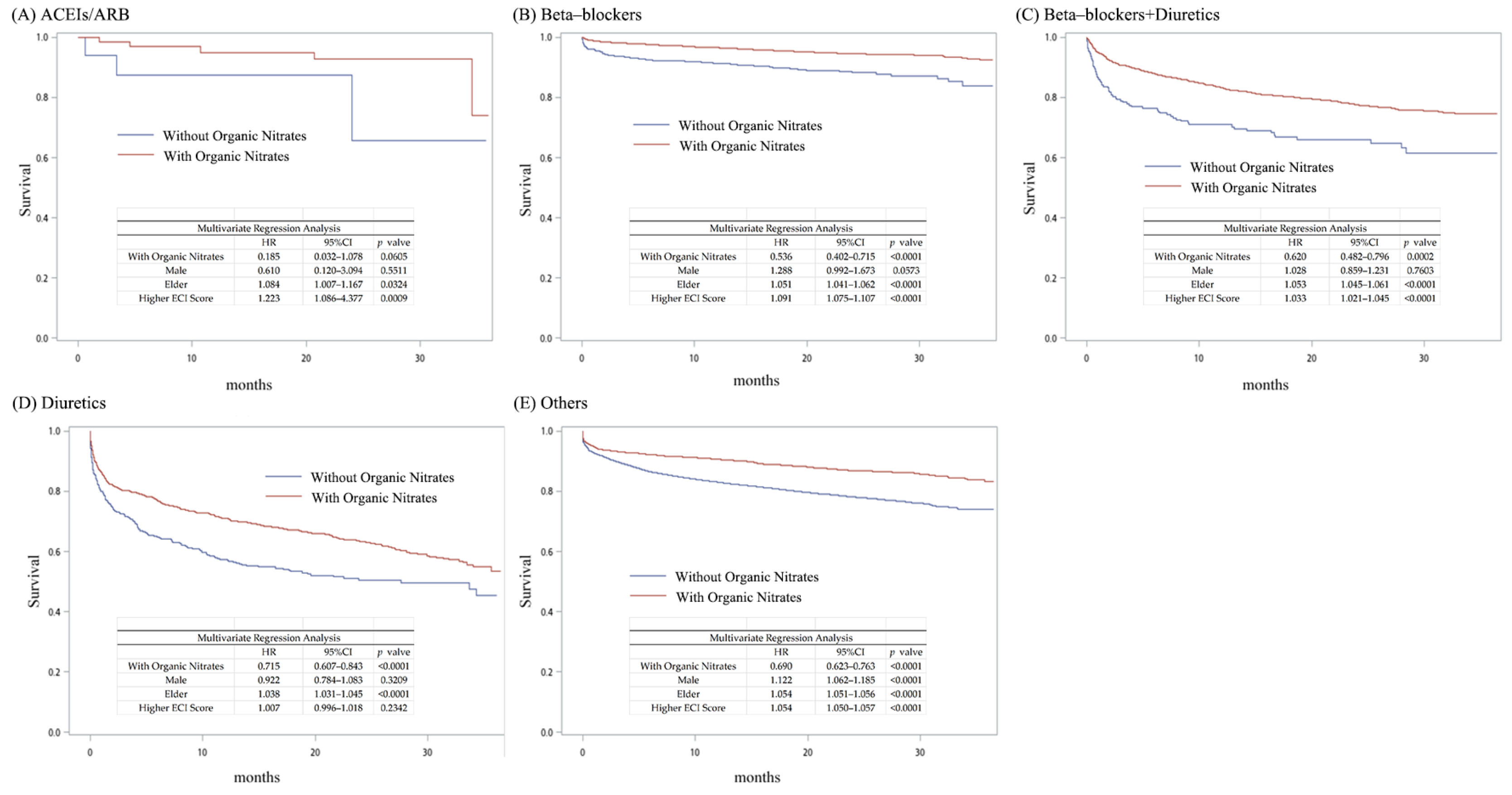
3.4. The Importance of Organic Nitrates in the Survival of Hyperlipidemia Patients with Acute Myocardial Infarction Prescribed Different Treatments
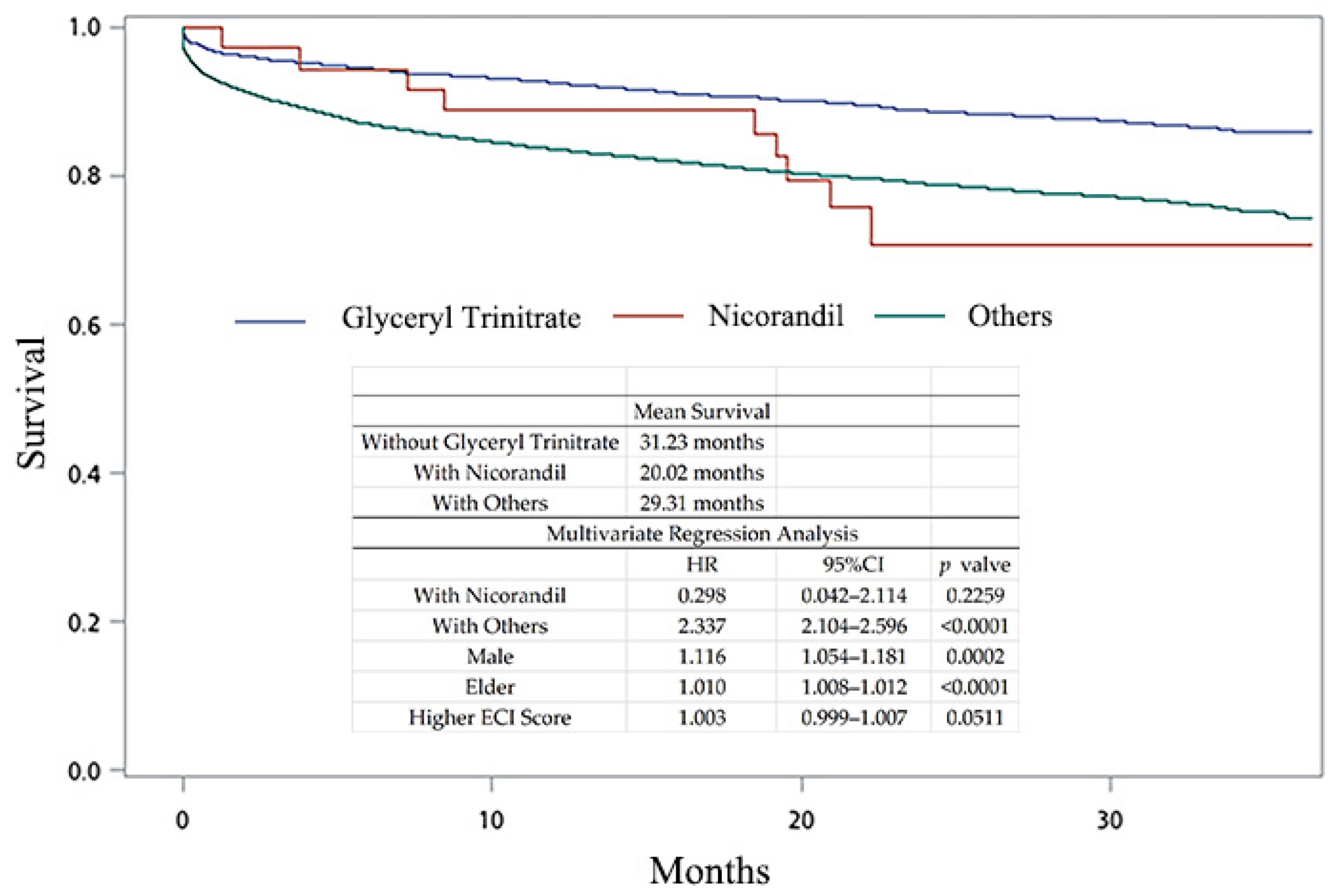
3.5. The Difference in NO-Enhancing Agents for the Survival of Hyperlipidemia Patients with Acute Myocardial Infarction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pan, W.H.; Wu, H.J.; Yeh, C.J.; Chuang, S.Y.; Chang, H.Y.; Yeh, N.H.; Hsieh, Y.T. Diet and health trends in Taiwan: Comparison of two nutrition and health surveys from 1993–1996 and 2005–2008. Asia Pac. J. Clin. Nutr. 2011, 20, 238–250. [Google Scholar] [PubMed]
- Pan, W.H.; Chiang, B.N. Plasma lipid profiles and epidemiology of atherosclerotic diseases in Taiwan—A unique experience. Atherosclerosis 1995, 118, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.B.; Kim, J.R.; Hwang, J.Y. Epidemiology of myocardial infarction in Korea: Hospitalization incidence, prevalence, and mortality. Epidemiol. Health 2022, 44, e2022057. [Google Scholar] [CrossRef]
- Cho, K.H.; Shin, M.H.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Kim, J.H.; Ahn, Y.; Kim, H.S.; Hur, S.H.; Lee, S.R.; et al. Incidence, Relevant Patient Factors, and Clinical Outcomes of the Misdiagnosis of ST-Segment-Elevation Myocardial Infarction: Results From the Korea Acute Myocardial Infarction Registry. J. Am. Heart Assoc. 2023, 12, e029728. [Google Scholar] [CrossRef] [PubMed]
- Statescu, C.; Anghel, L.; Tudurachi, B.S.; Leonte, A.; Benchea, L.C.; Sascau, R.A. From Classic to Modern Prognostic Biomarkers in Patients with Acute Myocardial Infarction. Int. J. Mol. Sci. 2022, 23, 9168. [Google Scholar] [CrossRef]
- Miura, M.; Yamasaki, M.; Uemura, Y.; Yoshikawa, M.; Miyauchi, K.; Tanaka, H.; Miyachi, H.; Yamashita, J.; Suzuki, M.; Yamamoto, T.; et al. Effect of Statin Treatment and Low-Density Lipoprotein-Cholesterol on Short-Term Mortality in Acute Myocardial Infarction Patients Undergoing Primary Percutaneous Coronary Intervention—Multicenter Registry From Tokyo CCU Network Database. Circ. J. 2016, 80, 461–468. [Google Scholar] [CrossRef]
- Hickson, R.P.; Robinson, J.G.; Annis, I.E.; Killeya-Jones, L.A.; Fang, G. It’s Not Too Late to Improve Statin Adherence: Association Between Changes in Statin Adherence from Before to After Acute Myocardial Infarction and All-Cause Mortality. J. Am. Heart Assoc. 2019, 8, e011378. [Google Scholar] [CrossRef]
- Stone, N.J.; Robinson, J.G.; Lichtenstein, A.H.; Bairey Merz, C.N.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2889–2934. [Google Scholar] [CrossRef]
- Christensen, D.M.; Strange, J.E.; Phelps, M.; Schjerning, A.M.; Sehested, T.S.G.; Gerds, T.; Gislason, G. Age- and sex-specific trends in the incidence of myocardial infarction in Denmark, 2005 to 2021. Atherosclerosis 2022, 346, 63–67. [Google Scholar] [CrossRef]
- Becker, R.C.; Burns, M.; Gore, J.M.; Spencer, F.A.; Ball, S.P.; French, W.; Lambrew, C.; Bowlby, L.; Hilbe, J.; Rogers, W.J. Early assessment and in-hospital management of patients with acute myocardial infarction at increased risk for adverse outcomes: A nationwide perspective of current clinical practice. The National Registry of Myocardial Infarction (NRMI-2) Participants. Am. Heart J. 1998, 135, 786–796. [Google Scholar] [CrossRef]
- Tu, J.V.; Austin, P.C.; Walld, R.; Roos, L.; Agras, J.; McDonald, K.M. Development and validation of the Ontario acute myocardial infarction mortality prediction rules. J. Am. Coll. Cardiol. 2001, 37, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Ji, Z.; Zhang, R.; Lu, W.; Ma, G.; Qu, Y. The effect of nicorandil in patients with acute myocardial infarction undergoing percutaneous coronary intervention: A systematic review and meta-analysis. Ir. J. Med. Sci. 2020, 189, 119–131. [Google Scholar] [CrossRef]
- Li, M.; Liu, Y.; Wang, H. Diagnosis and prognosis of myocardial infarction in a patient without obstructive coronary artery disease during bronchoscopy: A case study and literature review. BMC Cardiovasc. Disord. 2020, 20, 185. [Google Scholar] [CrossRef]
- Mahmarian, J.J.; Moye, L.A.; Chinoy, D.A.; Sequeira, R.F.; Habib, G.B.; Henry, W.J.; Jain, A.; Chaitman, B.R.; Weng, C.S.; Morales-Ballejo, H.; et al. Transdermal nitroglycerin patch therapy improves left ventricular function and prevents remodeling after acute myocardial infarction: Results of a multicenter prospective randomized, double-blind, placebo-controlled trial. Circulation 1998, 97, 2017–2024. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Shih, J.C.; Tsai, M.H.; Chung, C.H. Long-term survival and renal outcomes of thrombotic microangiopathy in pregnancy: A retrospective cohort study. Int. J. Gynaecol. Obs. Obstet. 2023, 163, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.H.; Wang, Y.J.; Jiao, X.; Lee, C.Y. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for aortic stenosis in Taiwan: A population-based cohort study. PLoS ONE 2023, 18, e0285191. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.Y.; Warren-Gash, C.; Smeeth, L.; Chen, P.C. Data resource profile: The National Health Insurance Research Database (NHIRD). Epidemiol. Health 2018, 40, e2018062. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Asensio-Lopez, M.C.; Soler, F.; Pascual-Figal, D.; Fernandez-Belda, F.; Lax, A. Doxorubicin-induced oxidative stress: The protective effect of nicorandil on HL-1 cardiomyocytes. PLoS ONE 2017, 12, e0172803. [Google Scholar] [CrossRef]
- Aekplakorn, W.; Taneepanichskul, S.; Kessomboon, P.; Chongsuvivatwong, V.; Putwatana, P.; Sritara, P.; Sangwatanaroj, S.; Chariyalertsak, S. Prevalence of Dyslipidemia and Management in the Thai Population, National Health Examination Survey IV, 2009. J. Lipids 2014, 2014, 249584. [Google Scholar] [CrossRef]
- Antman, E.M.; Anbe, D.T.; Armstrong, P.W.; Bates, E.R.; Green, L.A.; Hand, M.; Hochman, J.S.; Krumholz, H.M.; Kushner, F.G.; Lamas, G.A.; et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation 2004, 110, e82–e292. [Google Scholar] [PubMed]
- Nakatani, D.; Sakata, Y. Are beta blockers still necessary for all survivors of acute myocardial infarction? J. Thorac. Dis. 2017, 9, 3616–3619. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, S.; Street, W.N.; Polgreen, L.A. Machine learning approaches to predict the 1-year-after-initial-AMI survival of elderly patients. BMC Med. Inf. Inform. Decis. Mak. 2022, 22, 115. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zhao, G.; Zhou, M.; Wang, G.; Ma, C.; Smith, S.C., Jr.; Fonarow, G.C.; Morgan, L.; Que, B.; Ai, H.; et al. Early ACEI/ARB use and in-hospital outcomes of acute myocardial infarction patients with systolic blood pressure <100 mmHg and undergoing percutaneous coronary intervention: Findings from the CCC-ACS project. Front. Cardiovasc. Med. 2022, 9, 1003442. [Google Scholar] [CrossRef]
- Tisminetzky, M.; Gurwitz, J.; Chen, H.Y.; Erskine, N.; Yarzebski, J.; Gore, J.; Lessard, D.; Goldberg, R. Identification and Characteristics of Low-Risk Survivors of an Acute Myocardial Infarction. Am. J. Cardiol. 2016, 117, 1552–1557. [Google Scholar] [CrossRef]
- Jugdutt, B.I.; Warnica, J.W. Intravenous nitroglycerin therapy to limit myocardial infarct size, expansion, and complications. Effect of timing, dosage, and infarct location. Circulation 1988, 78, 906–919. [Google Scholar] [CrossRef]
- Del Buono, M.G.; Moroni, F.; Montone, R.A.; Azzalini, L.; Sanna, T.; Abbate, A. Ischemic Cardiomyopathy and Heart Failure After Acute Myocardial Infarction. Curr. Cardiol. Rep. 2022, 24, 1505–1515. [Google Scholar] [CrossRef]

| Year | 2016 | 2017 | 2018 |
|---|---|---|---|
| OPD ≥ 2 | 2,169,346 | 2,333,994 | 2,451,335 |
| IPD | 96,284 | 101,918 | 108,978 |
| Patients with hyperlipidemia (N) * | 2,208,962 (9.28%) | 2,374,463 (9.94%) | 2,495,158 (10.42%) |
| Gender | |||
| Female | 1,081,974 (48.98%) | 1,164,910 (49.06%) | 1,226,360 (49.15%) |
| Male | 1,102,406 (49.91%) | 1,182,746 (49.81%) | 1,238,586 (49.64%) |
| Unknown | 24,582 (1.11%) | 26,807 (1.13%) | 30,212 (1.21%) |
| Age | |||
| ≤40 | 131,375 (5.95%) | 138,925 (5.85%) | 144,687 (5.80%) |
| 41–50 | 282,721 (12.80%) | 300,845 (12.67%) | 315,106 (12.63%) |
| 51–60 | 616,257 (27.90%) | 645,965 (27.20%) | 662,774 (26.56%) |
| 61–70 | 661,683 (29.95%) | 735,553 (30.98%) | 785,010 (31.46%) |
| 71–80 | 353,718 (16.01%) | 374,190 (15.76%) | 395,136 (15.84%) |
| ≥81 | 147,492 (6.68%) | 162,233 (6.83%) | 173,479 (6.95%) |
| Unknown | 15,716 (0.71%) | 16,752 (0.71%) | 18,966 (0.76%) |
| Acute myocardial infarction (N) | 14,688 (0.66%) | 16,034 (0.68%) | 10,388 (0.42%) |
| (665 per 100,000) | (675 per 100,000) | (416 per 100,000) |
| Without Organic Nitrates | With Organic Nitrates | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ACEIs/ ARB (17) | Beta-Blockers (552) | Beta-Blockers + Diuretics (223) | Diuretics (496) | Others (28,456) | ACEIs/ ARB (72) | Beta- Blockers (4312) | Beta- Blockers + Diuretics (2360) | Diuretics (1263) | Others (3359) | |
| Gender | ||||||||||
| Male | 7 (41.18%) | 408 (73.91%) | 136 (60.99%) | 286 (57.66%) | 19,909 (69.96%) | 57 (79.17%) | 3553 (82.40%) | 1656 (70.17%) | 848 (67.14%) | 2531 (75.35%) |
| Female/Unknown | 10 (58.82%) | 144 (26.09%) | 87 (39.01%) | 210 (42.34%) | 8442 (29.67%) | 15 (20.83%) | 759 (17.6%) | 704 (29.83%) | 415 (32.86%) | 828 (24.65%) |
| Age | ||||||||||
| ≤40 | 0 (0.00%) | 18 (3.26%) | 54 (24.22%) | 5 (1.01%) | 931 (3.27%) | 3 (4.17%) | 247 (5.73%) | 47 (1.99%) | 15 (1.19%) | 147 (3.48%) |
| 41–60 | 3 (17.65%) | 234 (42.39%) | 78 (15.73%) | 8865 (31.15%) | 24 (33.33%) | 2011 (46.64%) | 686 (29.07%) | 266 (21.06% | 1272 (37.87%) | |
| 61–80 | 10 (58.82%) | 239 (43.30%) | 106 (47.53%) | 251 (50.60%) | 13,698 (48.14%) | 34 (47.22%) | 1761 (40.84%) | 1190 (50.42%) | 653 (51.70%) | 1565 (46.59%) |
| ≥81 | 4 (25.53%) | 61 (11.05%) | 63 (28.25%) | 162 (32.66%) | 4962 (17.44%) | 11 (15.28%) | 293 (6.79%) | 437 (18.52%) | 329 (26.05%) | 375 (11.16%) |
| Mean | 72.41 | 62.96 | 70.97 | 73.18 | 66.19 | 63.77 * | 60.09 *** | 67.20 *** | 70.80 *** | 63.31 *** |
| Std | 9.82 | 13.08 | 13.20 | 12.76 | 13.73 | 13.08 | 12.61 | 13.14 | 12.74 | 13.24 |
| Comorbidity | ||||||||||
| Congestive heart failure | 4 (23.53%) | 112 (20.29%) | 127 (53.95%) | 326 (65.73%) | 10,317 (36.26%) | 12 (16.67%) | 804 (18.65%) | 1355 (57.42%) | 877 (69.44%) | 843 (25.10%) *** |
| Cardiac arrhythmias | 5 (29.41%) | 120 (21.74%) | 64 (28.70%) | 156 (31.45%) | 6078 (21.36%) | 14 (19.44%) | 679 (15.75%) *** | 567 (24.03%) | 344 (27.24%) | 681 (20.27%) |
| Valvular disease | 30 (5.43%) | 28 (12.56%) | 65 (13.10%) | 2362 (8.30%) | 3 (4.17%) | 201 (4.66%) | 224 (9.49%) | 164 (12.98%) | 267 (7.95%) | |
| Hypertension, uncomplicated | 15 (88.24%) | 373 (67.57%) | 159 (71.30%) | 329 (66.33%) | 18,554 (65.20%) | 66 (91.67%) | 2766 (64.15%) | 1566 (66.36%) | 853 (67.54%) | 2173 (64.69%) |
| Hypertension, complicated | 10 (58.82%) | 194 (35.14%) | 106 (47.53%) | 261 (52.62%) | 12,927 (45.43%) | 33 (45.83%) | 1447 (33.56%) | 1147 (48.60% | 676 (53.52%) | 1287 (38.31%) *** |
| Diabetes, uncomplicated | 3 (17.65%) | 72 (13.04%) | 49 (21.97%) | 132 (26.61%) | 5367 (18.86%) | 8 (11.11%) | 515 (11.94%) | 497 (21.06%) | 333 (26.37%) | 600 (17.86%) |
| Diabetes, complicate | 10 (58.82%) | 210 (38.04%) | 126 (56.50%) | 288 (58.06%) | 13,615 (47.85%) | 44 (61.11%) | 1691 (39.22%) | 1286 (54.49%) * | 707 (55.98%) | 1416 (42.16%) *** |
| Renal failure | 0 (0.00%) | 7 (1.27%) | 3 (1.35%) | 11 (2.22%) | 380 (1.34%) | ≤3 (≤4.2%) | 49 (1.14%) | 35 (1.48%) | 25 (1.98%) | 42 (1.25%) |
| ECI score | ||||||||||
| Mean | 12.53 | 10.75 | 15.72 | 17.36 | 13.02 | 10.56 | 10.07 ** | 14.76 * | 16.63 * | 11.34 *** |
| Std | 6.52 | 6.15 | 6.71 | 7.32 | 7.12 | 5.44 | 5.73 | 6.91 | 6.83 | 6.65 |
| Without Organic Nitrates | With Organic Nitrates | |
|---|---|---|
| Gender | ||
| Male | 8357 (77.01%) | 8357 (77.01%) |
| Female/Unknown | 2495 (22.99%) | 2495 (22.99%) |
| Age | ||
| ≤40 | 383 (3.53%) | 383 (3.53%) |
| 41–60 | 4056 (37.38%) | 4056 (37.38%) |
| 61–80 | 5069 (46.71%) | 5069 (46.71%) |
| ≥81 | 1344 (12.38%) | 1344 (12.38%) |
| Mean | 63.90 | 63.90 |
| Std | 13.09 | 13.09 |
| Comorbidity | ||
| Congestive heart failure | 3524 (32.47%) | 3641 (33.55%) |
| Cardiac arrhythmias | 2040 (18.80%) | 2135 (19.67%) |
| Valvular disease | 706 (6.51%) | 765 (7.05%) |
| Peripheral vascular disorders | 350 (3.23%) | 346 (3.19%) |
| Hypertension, uncomplicated | 7007 (64.57%) | 7125 (65.66%) |
| Hypertension, complicated | 4587 (42.27%) | 4359 (40.17%) ** |
| ECI Score | ||
| Mean | 11.91 | 11.91 |
| Std | 6.34 | 6.34 |
| Median | 11 | 11 |
| Glyceryl Trinitrate | Nicorandil | Others | |
|---|---|---|---|
| Patient Number | 3954 (9.62%) | 36 (0.09%) | 37,120 (90.29%) |
| Gender | |||
| Male | 3130 (79.16%) | 29 (80.56%) | 26,232 (70.67%) |
| Female | 824 (20.84%) | 7 (19.44%) | 10,888 (29.33%) |
| Age | |||
| ≤40 | 208 (5.26%) | 0 (0.00%) | 1206 (3.25%) |
| 41–60 | 1677 (42.41%) | 16 (44.44%) | 11,799 (31.79%) |
| 61–80 | 1665 (41.11%) | 13 (36.11%) | 17,829 (48.03%) |
| ≥81 | 404 (10.22%) | 7 (19.44%) | 6286 (16.93) |
| Mean | 61.90 | 65.61 | 65.97 *** |
| Std | 13.38 | 13.79 | 13.67 |
| Comorbidity | |||
| Congestive heart failure | 1186 (29.99%) | 19 (52.78%) ** | 13,572 (36.56%) *** |
| Cardiac arrhythmias | 700 (17.70%) | 16 (44.44%) | 7994 (21.54%) *** |
| Valvular disease | 286 (7.23%) | 3057 (8.24%) * | |
| Pulmonary circulation disorders | 23 (0.58%) | 398 (1.07%) ** | |
| Peripheral vascular disorders | 149 (3.77%) | 1513 (4.08%) | |
| Hypertension, uncomplicated | 2580 (65.25%) | 28 (77.78%) | 24,244 (65.31%) |
| Hypertension, complicated | 1458 (36.87%) | 17 (47.22%) | 16,613 (44.75%) *** |
| Other neurological disorders | 32 (0.81%) | 562 (1.51%) *** | |
| Chronic pulmonary disease | 3884 (98.23%) | 36 (100.00%) | 36,430 (98.14%) |
| Diabetes, uncomplicated | 623 (15.76%) | 5 (13.89) | 6948 (18.72%) *** |
| Diabetes, complicate | 1664 (42.08%) | 18 (50.00%) | 17,711 (47.71%) *** |
| Renal failure | 46 (1.16%) | 4 (11.11%) *** | 503 (1.36%) |
| ECI Score | |||
| Mean | 11.35 | 14.42 ** | 12.97 *** |
| Std | 6.58 | 7.40 | 7.09 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, A.-S.; Hung, C.-L.; Lai, T.-S.; Chung, C.-H. Investigation of the Therapeutic Potential of Organic Nitrates in Mortality Reduction Following Acute Myocardial Infarction in Hyperlipidemia Patients: A Population-Based Cohort Study. J. Pers. Med. 2024, 14, 124. https://doi.org/10.3390/jpm14010124
Lee A-S, Hung C-L, Lai T-S, Chung C-H. Investigation of the Therapeutic Potential of Organic Nitrates in Mortality Reduction Following Acute Myocardial Infarction in Hyperlipidemia Patients: A Population-Based Cohort Study. Journal of Personalized Medicine. 2024; 14(1):124. https://doi.org/10.3390/jpm14010124
Chicago/Turabian StyleLee, An-Sheng, Chung-Lieh Hung, Thung-Shen Lai, and Ching-Hu Chung. 2024. "Investigation of the Therapeutic Potential of Organic Nitrates in Mortality Reduction Following Acute Myocardial Infarction in Hyperlipidemia Patients: A Population-Based Cohort Study" Journal of Personalized Medicine 14, no. 1: 124. https://doi.org/10.3390/jpm14010124
APA StyleLee, A.-S., Hung, C.-L., Lai, T.-S., & Chung, C.-H. (2024). Investigation of the Therapeutic Potential of Organic Nitrates in Mortality Reduction Following Acute Myocardial Infarction in Hyperlipidemia Patients: A Population-Based Cohort Study. Journal of Personalized Medicine, 14(1), 124. https://doi.org/10.3390/jpm14010124







