Effects of the Practice of Movement Representation Techniques in People Undergoing Knee and Hip Arthroplasty: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy for Study Identification
2.2. Selection of Studies
2.3. Data Extraction
2.4. Risk of Bias Assessment Tool
2.5. Strategy for Data Synthesis
3. Results
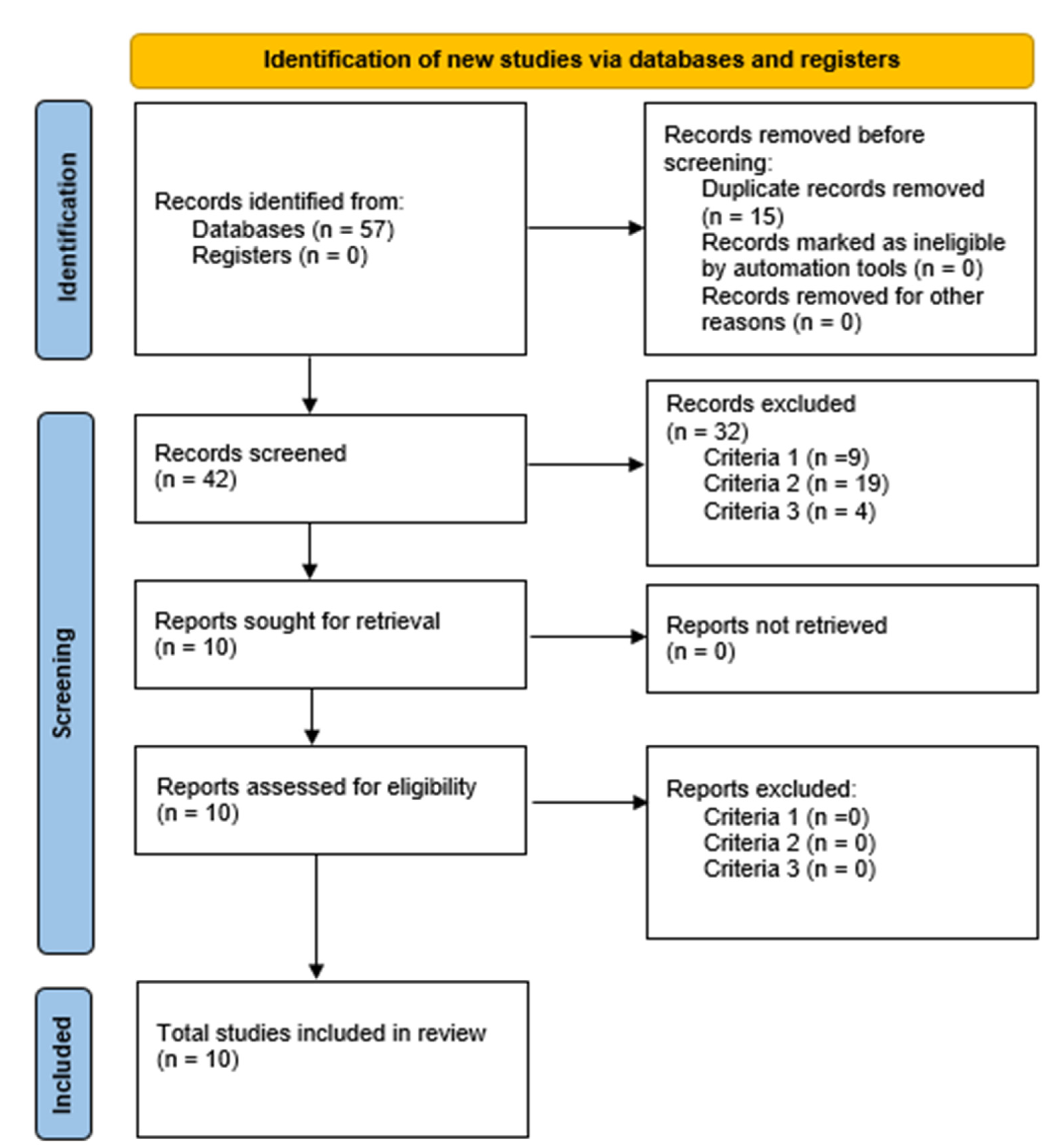
3.1. Literature Search
3.2. General Characteristics of the Studies
3.3. Risk of Bias in Articles
3.4. Characteristics of Interventions Using Movement Representation Techniques (MRT)
3.5. Effect of Motion Representation Techniques
4. Discussion
4.1. What Are the Main Results?
4.2. About the Population
4.3. About the Intervention Based on MRT
4.4. The Effects of Movement Representation Techniques
4.5. What Are the Limitations of This Review and the Review Processes Used?
4.6. Contributions, Clinical Implications, and Future Lines of Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barahona, M.; Prieto, J.P.; Ceron, F.; Catalán, J.; Infante, C.; Barrientos, C. Evolución epidemiológica de la artroplastia de cadera y rodilla durante 17 años en pacientes con artrosis severa en un Hospital Chileno. Rev. Chil. Ortop. Traumatol. 2021, 62, e77–e83. [Google Scholar] [CrossRef]
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 328 Diseases and Injuries for 195 Countries, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Anwer, S.; Sarkar, B.; Paul, A.K.; Anwar, D. Effect of 6-Week Retro or Forward Walking Program on Pain, Functional Disability, Quadriceps Muscle Strength, and Performance in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial (Retro-Walking Trial). BMC Musculoskelet. Disord. 2019, 20, 159. [Google Scholar] [CrossRef] [PubMed]
- Gerdesmeyer, L.; Al Muderis, M.; Gollwitzer, H.; Harrasser, N.; Stukenberg, M.; Clifford, M.-A.; Toepfer, A. 19 Years Outcome after Cementless Total Hip Arthroplasty with Spongy Metal Structured Implants in Patients Younger than 65 Years. BMC Musculoskelet. Disord. 2016, 17, 429. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Marusic, U.; Grosprêtre, S.; Paravlic, A.; Kovač, S.; Pišot, R.; Taube, W. Motor Imagery during Action Observation of Locomotor Tasks Improves Rehabilitation Outcome in Older Adults after Total Hip Arthroplasty. Neural Plast. 2018, 2018, 5651391. [Google Scholar] [CrossRef]
- Günther, K.-P.; Haase, E.; Lange, T.; Kopkow, C.; Schmitt, J.; Jeszenszky, C.; Balck, F.; Lützner, J.; Hartmann, A.; Lippmann, M. Persönlichkeitsprofil und Komorbidität: Gibt es den “schwierigen Patienten” in der primären Hüftendoprothetik? Orthopäde 2015, 44, 555–565. [Google Scholar] [CrossRef]
- Mannion, A.F.; Nauer, S.; Arsoy, D.; Impellizzeri, F.M.; Leunig, M. The Association between Comorbidity and the Risks and Early Benefits of Total Hip Arthroplasty for Hip Osteoarthritis. J. Arthroplast. 2020, 35, 2480–2487. [Google Scholar] [CrossRef]
- Karlsen, A.P.H.; Wetterslev, M.; Hansen, S.E.; Hansen, M.S.; Mathiesen, O.; Dahl, J.B. Postoperative Pain Treatment after Total Knee Arthroplasty: A Systematic Review. PLoS ONE 2017, 12, e0173107. [Google Scholar] [CrossRef]
- Højer Karlsen, A.P.; Geisler, A.; Petersen, P.L.; Mathiesen, O.; Dahl, J.B. Postoperative Pain Treatment after Total Hip Arthroplasty: A Systematic Review. Pain 2015, 156, 8–30. [Google Scholar] [CrossRef]
- Anger, M.; Valovska, T.; Beloeil, H.; Lirk, P.; Joshi, G.P.; Van de Velde, M.; Raeder, J.; The PROSPECT Working Group; The European Society of Regional Anaesthesia and Pain Therapy; Joshi, G.P.; et al. PROSPECT Guideline for Total Hip Arthroplasty: A Systematic Review and Procedure-specific Postoperative Pain Management Recommendations. Anaesthesia 2021, 76, 1082–1097. [Google Scholar] [CrossRef]
- Emmerzaal, J.; Corten, K.; van der Straaten, R.; De Baets, L.; Van Rossom, S.; Timmermans, A.; Jonkers, I.; Vanwanseele, B. Movement Quality Parameters during Gait Assessed by a Single Accelerometer in Subjects with Osteoarthritis and Following Total Joint Arthroplasty. Sensors 2022, 22, 2955. [Google Scholar] [CrossRef] [PubMed]
- Kolk, S.; Minten, M.J.M.; van Bon, G.E.A.; Rijnen, W.H.; Geurts, A.C.H.; Verdonschot, N.; Weerdesteyn, V. Gait and Gait-Related Activities of Daily Living after Total Hip Arthroplasty: A Systematic Review. Clin. Biomech. 2014, 29, 705–718. [Google Scholar] [CrossRef]
- Judd, D.L.; Dennis, D.A.; Thomas, A.C.; Wolfe, P.; Dayton, M.R.; Stevens-Lapsley, J.E. Muscle Strength and Functional Recovery during the First Year after THA. Clin. Orthop. Relat. Res. 2014, 472, 654–664. [Google Scholar] [CrossRef]
- Rasch, A.; Dalén, N.; Berg, H.E. Muscle Strength, Gait, and Balance in 20 Patients with Hip Osteoarthritis Followed for 2 Years after THA. Acta Orthop. 2010, 81, 183–188. [Google Scholar] [CrossRef]
- Behrendt, F.; Zumbrunnen, V.; Brem, L.; Suica, Z.; Gäumann, S.; Ziller, C.; Gerth, U.; Schuster-Amft, C. Effect of Motor Imagery Training on Motor Learning in Children and Adolescents: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 9467. [Google Scholar] [CrossRef] [PubMed]
- Mulder, T. Motor Imagery and Action Observation: Cognitive Tools for Rehabilitation. J. Neural Transm. 2007, 114, 1265–1278. [Google Scholar] [CrossRef] [PubMed]
- Grezes, J.; Decety, J. Functional Anatomy of Execution, Mental Simulation, Observation, and Verb Generation of Actions: A Meta-Analysis. Hum. Brain Mapp. 2001, 12, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Thieme, H.; Morkisch, N.; Rietz, C.; Dohle, C.; Borgetto, B. The Efficacy of Movement Representation Techniques for Treatment of Limb Pain—A Systematic Review and Meta-Analysis. J. Pain 2016, 17, 167–180. [Google Scholar] [CrossRef]
- MacIntyre, T.E.; Madan, C.R.; Moran, A.P.; Collet, C.; Guillot, A. Motor Imagery, Performance and Motor Rehabilitation. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2018; Volume 240, pp. 141–159. ISBN 978-0-444-64187-8. [Google Scholar]
- Cumming, J.; Ramsey, R. Imagery Interventions in Sport. In Advances in Applied Sport Psychology: A Review, 1st ed.; Mellalieu, S., Hanton, S., Eds.; Routledge: London, UK, 2008. [Google Scholar] [CrossRef]
- Braun, S.; Kleynen, M.; van Heel, T.; Kruithof, N.; Wade, D.; Beurskens, A. The Effects of Mental Practice in Neurological Rehabilitation; a Systematic Review and Meta-Analysis. Front. Hum. Neurosci. 2013, 7, 390. [Google Scholar] [CrossRef]
- De Vries, S.; Mulder, T. Motor Imagery and Stroke Rehabilitation: A Critical Discussion. Acta Derm. Venereol. 2007, 39, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Lebon, F.; Guillot, A.; Collet, C. Increased Muscle Activation Following Motor Imagery During the Rehabilitation of the Anterior Cruciate Ligament. Appl. Psychophysiol. Biofeedback 2012, 37, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Zapparoli, L.; Sacheli, L.M.; Seghezzi, S.; Preti, M.; Stucovitz, E.; Negrini, F.; Pelosi, C.; Ursino, N.; Banfi, G.; Paulesu, E. Motor Imagery Training Speeds Up Gait Recovery and Decreases the Risk of Falls in Patients Submitted to Total Knee Arthroplasty. Sci. Rep. 2020, 10, 8917. [Google Scholar] [CrossRef] [PubMed]
- Paravlic, A.H.; Pisot, R.; Marusic, U. Specific and General Adaptations Following Motor Imagery Practice Focused on Muscle Strength in Total Knee Arthroplasty Rehabilitation: A Randomized Controlled Trial. PLoS ONE 2019, 14, e0221089. [Google Scholar] [CrossRef]
- Li, R.; Du, J.; Yang, K.; Wang, X.; Wang, W. Effectiveness of Motor Imagery for Improving Functional Performance after Total Knee Arthroplasty: A Systematic Review with Meta-Analysis. J. Orthop. Surg. Res. 2022, 17, 65. [Google Scholar] [CrossRef]
- Ferrer-Peña, R.; Cuenca-Martínez, F.; Romero-Palau, M.; Flores-Román, L.M.; Arce-Vázquez, P.; Varangot-Reille, C.; Suso-Martí, L. Effects of Motor Imagery on Strength, Range of Motion, Physical Function, and Pain Intensity in Patients with Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Braz. J. Phys. Ther. 2021, 25, 698–708. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Pirali, C.; Isgrò, M.; Vanti, C.; Buraschi, R.; Negrini, S. Effects of Action Observation Therapy in Patients Recovering from Total Hip Arthroplasty Arthroplasty: A Prospective Clinical Trial. J. Chiropr. Med. 2016, 15, 229–234. [Google Scholar] [CrossRef]
- Briones-Cantero, M.; Fernández-de-las-Peñas, C.; Lluch-Girbés, E.; Osuna-Pérez, M.C.; Navarro-Santana, M.J.; Plaza-Manzano, G. Patricia Martín-Casas Effects of Adding Motor Imagery to Early Physical Therapy in Patients with Knee Osteoarthritis Who Had Received Total Knee Arthroplasty: A Randomized Clinical Trial. Pain Med. 2020, 21, 3548–3555. [Google Scholar] [CrossRef]
- Paravlic, A.H.; Maffulli, N.; Kovač, S.; Pisot, R. Home-Based Motor Imagery Intervention Improves Functional Performance Following Total Knee Arthroplasty in the Short Term: A Randomized Controlled Trial. J. Orthop. Surg. Res. 2020, 15, 451. [Google Scholar] [CrossRef] [PubMed]
- Moukarzel, M.; Di Rienzo, F.; Lahoud, J.-C.; Hoyek, F.; Collet, C.; Guillot, A.; Hoyek, N. The Therapeutic Role of Motor Imagery during the Acute Phase after Total Knee Arthroplasty: A Pilot Study. Disabil. Rehabil. 2019, 41, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Moukarzel, M.; Guillot, A.; Di Rienzo, F.; Hoyek, N. The Therapeutic Role of Motor Imagery during the Chronic Phase after Total Knee Arthroplasty: A Pilot Randomized Controlled Trial. Eur. J. Phys. Rehabil. Med. 2019, 55, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Villafañe, J.H.; Isgrò, M.; Borsatti, M.; Berjano, P.; Pirali, C.; Negrini, S. Effects of Action Observation Treatment in Recovery after Total Knee Replacement: A Prospective Clinical Trial. Clin. Rehabil. 2017, 31, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Koo, K.; Park, D.K.; Youm, Y.S.; Cho, S.D.; Hwang, C.H. Enhanced Reality Showing Long-Lasting Analgesia after Total Knee Arthroplasty: Prospective, Randomized Clinical Trial. Sci. Rep. 2018, 8, 2343. [Google Scholar] [CrossRef] [PubMed]
- Yap, B.W.D.; Lim, E.C.W. The Effects of Motor Imagery on Pain and Range of Motion in Musculoskeletal Disorders: A Systematic Review Using Meta-Analysis. Clin. J. Pain 2019, 35, 87–99. [Google Scholar] [CrossRef]
- Cho, H.; Kim, J.; Lee, G.-C. Effects of Motor Imagery Training on Balance and Gait Abilities in Post-Stroke Patients: A Randomized Controlled Trial. Clin. Rehabil. 2013, 27, 675–680. [Google Scholar] [CrossRef]
- Silva, S.; Borges, L.R.; Santiago, L.; Lucena, L.; Lindquist, A.R.; Ribeiro, T. Motor Imagery for Gait Rehabilitation after Stroke. Cochrane Database Syst. Rev. 2020, 9, CD013019. [Google Scholar] [CrossRef]
- Poiroux, E.; Cavaro-Ménard, C.; Leruez, S.; Lemée, J.M.; Richard, I.; Dinomais, M. What Do Eye Gaze Metrics Tell Us about Motor Imagery? PLoS ONE 2015, 10, e0143831. [Google Scholar] [CrossRef][Green Version]
- Decety, J. The Neurophysiological Basis of Motor Imagery. Behav. Brain Res. 1996, 77, 45–52. [Google Scholar] [CrossRef]
- Sabaté, M.; González, B.; Rodríguez, M. Brain Lateralization of Motor Imagery: Motor Planning Asymmetry as a Cause of Movement Lateralization. Neuropsychologia 2004, 42, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Guerra, Z.F.; Lucchetti, A.L.G.; Lucchetti, G. Motor Imagery Training After Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Neurol. Phys. Ther. 2017, 41, 205–214. [Google Scholar] [CrossRef] [PubMed]
- García Carrasco, D.; Aboitiz Cantalapiedra, J. Efectividad de la imaginería o práctica mental en la recuperación funcional tras el ictus: Revisión sistemática. Neurología 2016, 31, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.E.; Guillot, A.; Di Rienzo, F.; Cumming, J. Comparing Self-Report and Mental Chronometry Measures of Motor Imagery Ability. Eur. J. Sport Sci. 2015, 15, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Lebon, F.; Byblow, W.D.; Collet, C.; Guillot, A.; Stinear, C.M. The Modulation of Motor Cortex Excitability during Motor Imagery Depends on Imagery Quality: Imagery Quality and Corticomotor Excitability. Eur. J. Neurosci. 2012, 35, 323–331. [Google Scholar] [CrossRef]
- Bakker, M.; Overeem, S.; Snijders, A.H.; Borm, G.; van Elswijk, G.; Toni, I.; Bloem, B.R. Motor Imagery of Foot Dorsiflexion and Gait: Effects on Corticospinal Excitability. Clin. Neurophysiol. 2008, 119, 2519–2527. [Google Scholar] [CrossRef]
- Breckenridge, J.D.; Ginn, K.A.; Wallwork, S.B.; McAuley, J.H. Do People with Chronic Musculoskeletal Pain Have Impaired Motor Imagery? A Meta-Analytical Systematic Review of the Left/Right Judgment Task. J. Pain 2019, 20, 119–132. [Google Scholar] [CrossRef]
- Wallwork, S.B.; Leake, H.B.; Peek, A.L.; Moseley, G.L.; Stanton, T.R. Implicit Motor Imagery Performance Is Impaired in People with Chronic, but Not Acute, Neck Pain. PeerJ 2020, 8, e8553. [Google Scholar] [CrossRef]
- Stanton, T.R.; Lin, C.-W.C.; Smeets, R.J.E.M.; Taylor, D.; Law, R.; Lorimer Moseley, G. Spatially Defined Disruption of Motor Imagery Performance in People with Osteoarthritis. Rheumatology 2012, 51, 1455–1464. [Google Scholar] [CrossRef]
- Gentile, E.; Brunetti, A.; Ricci, K.; Bevilacqua, V.; Craighero, L.; de Tommaso, M. Movement Observation Activates Motor Cortex in Fibromyalgia Patients: A FNIRS Study. Sci. Rep. 2022, 12, 4707. [Google Scholar] [CrossRef]
- Pastora-Bernal, J.M.; Estebanez-Pérez, M.J.; Lucena-Anton, D.; García-López, F.J.; Bort-Carballo, A.; Martín-Valero, R. The Effectiveness and Recommendation of Motor Imagery Techniques for Rehabilitation after Anterior Cruciate Ligament Reconstruction: A Systematic Review. JCM 2021, 10, 428. [Google Scholar] [CrossRef] [PubMed]
- Herranz-Gómez, A.; Gaudiosi, C.; Angulo-Díaz-Parreño, S.; Suso-Martí, L.; La Touche, R.; Cuenca-Martínez, F. Effectiveness of Motor Imagery and Action Observation on Functional Variables: An Umbrella and Mapping Review with Meta-Meta-Analysis. Neurosci. Biobehav. Rev. 2020, 118, 828–845. [Google Scholar] [CrossRef] [PubMed]
- Ji, E.K.; Wang, H.H.; Jung, S.J.; Lee, K.B.; Kim, J.S.; Jo, L.; Hong, B.Y.; Lim, S.H. Graded Motor Imagery Training as a Home Exercise Program for Upper Limb Motor Function in Patients with Chronic Stroke: A Randomized Controlled Trial. Medicine 2021, 100, e24351. [Google Scholar] [CrossRef] [PubMed]
- Paravlic, A.H. Motor Imagery and Action Observation as Appropriate Strategies for Home-Based Rehabilitation: A Mini-Review Focusing on Improving Physical Function in Orthopedic Patients. Front. Psychol. 2022, 13, 826476. [Google Scholar] [CrossRef] [PubMed]
- Naish, K.R.; Houston-Price, C.; Bremner, A.J.; Holmes, N.P. Effects of Action Observation on Corticospinal Excitability: Muscle Specificity, Direction, and Timing of the Mirror Response. Neuropsychologia 2014, 64, 331–348. [Google Scholar] [CrossRef] [PubMed]
- Chholak, P.; Niso, G.; Maksimenko, V.A.; Kurkin, S.A.; Frolov, N.S.; Pitsik, E.N.; Hramov, A.E.; Pisarchik, A.N. Visual and Kinesthetic Modes Affect Motor Imagery Classification in Untrained Subjects. Sci. Rep. 2019, 9, 9838. [Google Scholar] [CrossRef]
- Iacono, A.D.; Ashcroft, K.; Zubac, D. Ain’t Just Imagination! Effects of Motor Imagery Training on Strength and Power Performance of Athletes during Detraining. Med. Sci. Sport. Exerc. 2021, 53, 2324–2332. [Google Scholar] [CrossRef]
- Monteiro, K.B.; Cardoso, M.d.S.; Cabral, V.R.d.; Santos, A.O.B.d.; da Silva, P.S.; de Castro, J.B.P.; Vale, R.G.d. Effects of Motor Imagery as a Complementary Resource on the Rehabilitation of Stroke Patients: A Meta-Analysis of Randomized Trials. J. Stroke Cerebrovasc. Dis. 2021, 30, 105876. [Google Scholar] [CrossRef]
- Temporiti, F.; Ruspi, A.; De Leo, D.; Ugolini, A.; Grappiolo, G.; Avanzini, P.; Rizzolatti, G.; Gatti, R. Action Observation and Motor Imagery administered the day before surgery enhance functional recovery in patients after total hip arthroplasty: A randomized controlled trial. Clin. Rehabil. 2022, 36, 1613–1622. [Google Scholar] [CrossRef]
- Bidet-Ildei, C.; Deborde, Q.; Francisco, V.; Gand, E.; Blandin, Y.; Delaubier, A.; Jossart, A.; Rigoard, P.; Billot, M.; David, R. The Added Value of Point-Light Display Observation in Total Knee Arthroplasty Rehabilitation Program: A Prospective Randomized Controlled Pilot Study. Medicina 2022, 58, 868. [Google Scholar] [CrossRef]


| Criterion | Description |
|---|---|
|
|
| Containing interventions of motion representation techniques such as motor imagery, grade motor imagery, action observation, mirror therapy, and movement representation techniques [19]. |
|
|
| Valuing the following:
|
|
|
| Author | Year | Country | Population (Age m ± SD) | Sex (M%) | Sex (F%) | CS | Intervention | Variables | Type of Design |
|---|---|---|---|---|---|---|---|---|---|
| Marusic, U. [6] | 2018 | Slovenia | 21 (EXP 64.4 ± 4.1; CON 63.1 ± 5.6) | 14 (66.7%) | 7 (33.3%) | THA | AOT + MI | Physical function and cognitive function | RCT |
| Zapparoli, L. [25] | 2020 | Italy | 48 (66.4 ± 7.7) | 20 (41.7%) | 28 (58.3%) | TNA | MI | functionality, knee ROM, knee pain intensity, gait analysis and risk of falls | RTC with placebo |
| ParavlicI, A. [26] | 2019 | Slovenia | 34 (61.1 ± 5.3) | 19 (55.9%) | 15 (44.1%) | TNA | MI | physical function, spatiotemporal gait parameters, reported author physical function, and cognitive performance | RCT of parallel groups |
| Villafañe, J.H. [31] | 2016 | Italy | 24 (69 ± 8.5) | 10 (41.7%) | 14 (58.3%) | THA | AOT | Hip pain intensity, hip ROM, functionality, and quality of life | PCE |
| Briones-Cantero, M. [32] | 2020 | Spain | 24 (EXP 73 ± 5; CON 72 ± 6) | 15 (62.5%) | 9 (37.5%) | TNA | MI | pain-related disability, knee pain intensity, knee ROM, pain sensitivity to pressure | RCT of parallel groups |
| Paravlic, A.H. [33] | 2020 | Slovenia | 26 (EXP 61.69 ± 5.19; CON 58.85 ± 5.24) | 14 (53.8%) | 12 (46.2%) | TNA | MI | maximum voluntary isometric strength of knee extension, voluntary activation of knee extension, functionality, ROM knee, intensity of knee pain, maximum grip strength and reported author function | RCT of parallel groups |
| Moukarzel, M. [34] | 2017 | France | 20 (69.60 ± 3.25) | 4 (20%) | 16 (80%) | TNA | MI | knee pain, knee rom, knee circumference, quadriceps strength and functionality | RCT |
| MouKarzel, M. [35] | 2019 | France | 24 (70 ± 2.89) | 4 (16.7%) | 20 (83.3%) | TNA | MI | ipsilateral quadriceps strength, maximum knee flexion during rocking phase and functionality | RCT |
| Villafañe, J.H. [36] | 2016 | Italy | 31 (EXP 70.4 ± 7.5; CON 70.1 ± 7.7) | 10 (32.3%) | 21 (67.7%) | TNA | AOT | Knee pain intensity, quality of life, function, and gait | RCT Pilot |
| Koo, K.L. [37] | 2018 | South Korea | 42 (FULL 65.00 ± 6.97; HALF 63.71 ± 5.09) | 10 (23.8%) | 32 (76.2%) | TNA | AR | knee pain at rest and activity, ROM knee | RCT, prospective, parallel group |
| Total n = 294 | n = 120 (40.8%) | n = 174 (59.2%) |
| Author [Reference] | Groups | Frequency | Treatment | Extension | Duration | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MRT | CPT | ||||||||||
| Days/Week | AOT | MI | ER | AM | PM | TP | WI | Weeks | Minutes | ||
| Marusic, U. [6] | Control | 3 | – | – | – | NS | NS | NS | NS | 9 | NS |
| Intervention | 3 | ✓ | ✓ | – | NS | NS | NS | NS | 9 | NS | |
| Zapparoli, L. [25] | Control | 6 | – | – | – | ✓ | ✓ | ✓ | ✓ | 2 | 70 |
| Intervention | 6 | – | ✓ | – | ✓ | ✓ | ✓ | ✓ | 2 | NS | |
| Paravlic, A.H. [26] | Control | 5 | – | – | – | ✓ | ✓ | ✓ | ✓ | 5 | NS |
| Intervention | 5 | – | ✓ | – | ✓ | ✓ | ✓ | ✓ | 5 | NS | |
| Villafañe, J.H. [31] | Control | 5 | – | – | – | ✓ | ✓ | ✓ | ✓ | 2 | 15 |
| Intervention | 5 | ✓ | – | – | ✓ | ✓ | ✓ | ✓ | 2 | 30 | |
| Briones-Cantero, M. [32] | Control | 5 | – | – | – | ✓ | ✓ | ✓ | – | 1 | 30 |
| Intervention | 5 | – | ✓ | – | ✓ | ✓ | ✓ | – | 1 | 30 | |
| Paravlic, A.H. [33] | Control | 5 | – | – | – | ✓ | ✓ | ✓ | ✓ | 4 | NS |
| Intervention | 5 | – | ✓ | – | ✓ | ✓ | ✓ | ✓ | 4 | 45–60 | |
| Moukarzel, M. [34] | Control | 3 | – | – | – | ✓ | ✓ | ✓ | ✓ | 4 | 60 |
| Intervention | 3 | – | ✓ | – | ✓ | ✓ | ✓ | ✓ | 4 | 75 | |
| Moukarzel, M. [35] | Control | 3 | – | – | – | ✓ | ✓ | ✓ | ✓ | 4 | 60 |
| Intervention | 3 | – | ✓ | – | ✓ | ✓ | ✓ | ✓ | 4 | 60 | |
| Villafañe, J.H. [36] | Control | 5 | – | – | – | ✓ | ✓ | ✓ | ✓ | 2 | 100 |
| Intervention | 5 | ✓ | – | – | ✓ | ✓ | ✓ | ✓ | 2 | 100 | |
| Koo, K.L. [37] | HTI | 5 | – | – | – | NS | ✓ | NS | ✓ | 1 | 30 |
| FTI | 5 | – | – | ✓ | NS | ✓ | NS | ✓ | 2 | 30 | |
| Ref. | Groups | Physical | Functionality | Cognitive | Quality of Life | Other | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain | Strength | Rom | Speed | Gait | Functional Capacity | Motor Visualization Capability | Cognitive Performance | ||||
| [6] | Co | ↓TUG, ↓FSST, ↓S&D-TW(GS), ↓S&D-TW(OTV) |  S&D-TW(CP), S&D-TW(CP),  S&D-CP(CP) S&D-CP(CP) | ||||||||
| In |  *TUG, ↑*FSST, *TUG, ↑*FSST,  S&D-TW(GS), S&D-TW(GS),  *S&D-TW(OTV) *S&D-TW(OTV) | ↑*S&D-TW(CP), ↑S&D-CP(CP) | |||||||||
| [25] | Co |  VAS VAS | ↑P-ROM | ↑TUG, ↑GTS, ↑AR-GET | ↑FIS, ↑BARTHEL, FNF |  MIQI, MIQI,  HWT HWT | |||||
| In | ↑*VAS | ↑P-ROM | ↑*TUG, ↑GTS, ↑*AR-GET | ↑FIS, ↑BARTHEL, *FNF | ↑*MIQI,  HWT HWT | ||||||
| [26] | Co | ↑ MIEK, ↑SSC | ↑SWS, ↑SRSDT, ↑BWS, ↑DTBWS | ↑SSP,  DSP, *↑SL, *↑cadencia DSP, *↑SL, *↑cadencia |  LEFS LEFS | ↑KIC,  EVIC, ↑IVIC EVIC, ↑IVIC | ↑baseline ↑SSWS, ↑SMR | ||||
| In | *↑ MIEK, *↑SSC | *↑SWS, *↑SRSDT, *↑BWS, *↑DTBWS | *↑SSP, * DSP, ↑SL, ↑cadencia DSP, ↑SL, ↑cadencia |  LEFS LEFS | *↑KIC,  EVIC,*↑IVIC EVIC,*↑IVIC | ↑baseline, ↑SSWS, ↑SMR | |||||
| [31] | Co | ↑VAS | ↑A-ROM-HA, ↑P-ROM-HA | ↑TINETTI, ↑LEQUESNE, BARTHEL (N.D) | ↑SF-36 PF,  SF-36MHF SF-36MHF | ||||||
| [32] | Co | ↑VAS,  PPT PPT |  KFKE-ROM KFKE-ROM | ↑WOMAC | |||||||
| [33] | Co | ↑OL-VAS, ↑NOL-VAS | ↓ MIEK, ↓VA-OL,  MVIS-UL, MVIS-UL,  VA-UL, VA-UL,  DAR DAR | ↑OL-KF, ↑OL-KE,  NOL-KF, NOL-KF,  NOL-KE NOL-KE | ↓TUG |  OKS OKS | |||||
| [34] | Co | ↑VAS | ↑ MIEK |  A-ROM, A-ROM,  P-ROM P-ROM | ↑TUG |  KC KC | |||||
| In | *↑VAS | *↑ MIEK | ↑A-ROM, ↑P-ROM | ↑TUG |  KC KC | ||||||
| [35] | Co | ↑ MIEK | ↑MKFR | ↑TUG, ↑6MWT | ↑OKS, ↑SCT | ||||||
| In | ↑ MIEK | *↑MKFR | ↑TUG, ↑6MWT | ↑OKS, *↑SCT | |||||||
| [36] | Co | ↑VAS | ↑A-ROM, ↑P-ROM | ↑TINETTI, ↑LEQUESNE, ↑BARTHEL | ↑SF-36 PF,  SF-36MHF, CDRS (ND) SF-36MHF, CDRS (ND) | ||||||
| In | ↑VAS | ↑A-ROM, ↑P-ROM | ↑TINETTI, ↑LEQUESNE, ↑BARTHEL | ↑SF-36 PF,  SF-36MHF, CDRS (NS) SF-36MHF, CDRS (NS) | |||||||
| [37] | *Co | ↑VAS | ↑SSC | ↑A-ROM | ↑GAD, ↑6MWT | ↑WOMAC |  GDSSF GDSSF | ||||
| In | *↑VAS | ↑SSC | *↑A-ROM | ↑GAD, ↑6MWT | ↑WOMAC |  GDSSF GDSSF | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riquelme-Hernández, C.; Reyes-Barría, J.P.; Vargas, A.; Gonzalez-Robaina, Y.; Zapata-Lamana, R.; Toloza-Ramirez, D.; Parra-Rizo, M.A.; Cigarroa, I. Effects of the Practice of Movement Representation Techniques in People Undergoing Knee and Hip Arthroplasty: A Systematic Review. Sports 2022, 10, 198. https://doi.org/10.3390/sports10120198
Riquelme-Hernández C, Reyes-Barría JP, Vargas A, Gonzalez-Robaina Y, Zapata-Lamana R, Toloza-Ramirez D, Parra-Rizo MA, Cigarroa I. Effects of the Practice of Movement Representation Techniques in People Undergoing Knee and Hip Arthroplasty: A Systematic Review. Sports. 2022; 10(12):198. https://doi.org/10.3390/sports10120198
Chicago/Turabian StyleRiquelme-Hernández, Cristóbal, Juan Pablo Reyes-Barría, Abner Vargas, Yaynel Gonzalez-Robaina, Rafael Zapata-Lamana, David Toloza-Ramirez, Maria Antonia Parra-Rizo, and Igor Cigarroa. 2022. "Effects of the Practice of Movement Representation Techniques in People Undergoing Knee and Hip Arthroplasty: A Systematic Review" Sports 10, no. 12: 198. https://doi.org/10.3390/sports10120198
APA StyleRiquelme-Hernández, C., Reyes-Barría, J. P., Vargas, A., Gonzalez-Robaina, Y., Zapata-Lamana, R., Toloza-Ramirez, D., Parra-Rizo, M. A., & Cigarroa, I. (2022). Effects of the Practice of Movement Representation Techniques in People Undergoing Knee and Hip Arthroplasty: A Systematic Review. Sports, 10(12), 198. https://doi.org/10.3390/sports10120198








