Cryo plus Ultrasound Therapy, a Novel Rehabilitative Approach for Football Players with Acute Lateral Ankle Injury Sprain: A Pilot Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Intervention
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Future Perspectives
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walls, R.J.; Ross, K.A.; Fraser, E.J.; Hodgkins, C.W.; Smyth, N.A.; Egan, C.J.; Calder, J.; Kennedy, J.G. Football injuries of the ankle: A review of injury mechanisms, diagnosis and management. World J. Orthop. 2016, 7, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.; McGovern, R. Managing ankle ligament sprains and tears: Current opinion. Open. Access. J. Sport. Med. 2016, 7, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Knapik, D.M.; Trem, A.; Sheehan, J.; Salata, M.J.; Voos, J.E. Conservative Management for Stable High Ankle Injuries in Professional Football Players. Sports Health 2018, 10, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Al Attar, W.S.A.; Khaledi, E.H.; Bakhsh, J.M.; Faude, O.; Ghulam, H.; Sanders, R.H. Injury prevention programs that include balance training exercises reduce ankle injury rates among soccer players: A systematic review. J. Physiother. 2022, 68, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Nadler, A.; Tsung, J.W.; Rabiner, J.E. Point-of-Care Ultrasonography for Ankle Injuries in Children. Pediatr. Emerg. Care 2022, 38, E17–E22. [Google Scholar] [CrossRef]
- Clanton, T.O.; Matheny, L.M.; Jarvis, H.C.; Jeronimus, A.B. Return to Play in Athletes Following Ankle Injuries. Sports Health 2012, 4, 471–474. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.P.; Hong, Y.; Chan, L.K.; Yung, P.S.H.; Chan, K.M. A systematic review on ankle injury and ankle sprain in sports. Sport Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Thevendran, G.; Kadakia, A.R.; Giza, E.; Haverkamp, D.; D’Hooghe, J.P.; Veljkovic, A.; Abdelatif, N.M.N. Acute foot and ankle injuries and time return to sport. Sicot-J 2021, 7, 27. [Google Scholar] [CrossRef]
- Marotta, N.; Moggio, L.; Calafiore, D.; Prestifilippo, E.; Spanó, R.; Tasselli, A.; Drago Ferrante, V.; Invernizzi, M.; de Sire, A.; Ammendolia, A. Efficacy of Proprioceptive Training on Plantar Pressure and Jump Performance in Volleyball Players: A Proof-of-Principle Study. Sensors 2023, 23, 1906. [Google Scholar] [CrossRef]
- Gaddi, D.; Mosca, A.; Piatti, M.; Munegato, D.; Catalano, M.; Di Lorenzo, G.; Turati, M.; Zanchi, N.; Piscitelli, D.; Chui, K.; et al. Acute Ankle Sprain Management: An Umbrella Review of Systematic Reviews. Front. Med. 2022, 9, 868474. [Google Scholar] [CrossRef]
- Halabchi, F.; Hassabi, M. Acute ankle sprain in athletes: Clinical aspects and algorithmic approach. World J. Orthop. 2020, 11, 534–558. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Andrenelli, E.; Negrini, F.; Lazzarini, S.G.; Patrini, M.; Ceravolo, M.G.; International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action. Rehabilitation and COVID-19: The Cochrane Rehabilitation 2020 rapid living systematic review. Update as of August 31st, 2020. Eur. J. Phys. Rehabil. Med. 2020, 56, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; de Sire, A.; Gimigliano, A.; Demeco, A.; Moggio, L.; Vescio, A.; Iona, T.; Ammendolia, A. Impact of COVID-19 lockdown on the epidemiology of soccer muscle injuries in Italian Serie A professional football players. J. Sports Med. Phys. Fit. 2022, 62, 356–360. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Marotta, N.; Lippi, L.; Scaturro, D.; Farì, G.; Liccardi, A.; Moggio, L.; Letizia Mauro, G.; Ammendolia, A.; Invernizzi, M. Pharmacological treatment for acute traumatic musculoskeletal pain in athletes. Medicina 2021, 57, 1208. [Google Scholar] [CrossRef]
- Marotta, N.; Ferrillo, M.; Demeco, A.; Ferrante, V.D.; Inzitari, M.T.; Pellegrino, R.; Pino, I.; Russo, I.; de Sire, A.; Ammendolia, A. Effects of Radial Extracorporeal Shock Wave Therapy in Reducing Pain in Patients with Temporomandibular Disorders: A Pilot Randomized Controlled Trial. Appl. Sci. 2022, 12, 3821. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Inzitari, M.T.; Caruso, M.G.; Ammendolia, A.; Enix, D. Neuromuscular electrical stimulation and shortwave diathermy in unrecovered Bell palsy: A randomized controlled study. Medicine 2020, 99, e19152. [Google Scholar] [CrossRef]
- Van Den Bekerom, M.P.J.; Van Der Windt, D.A.W.M.; Ter Riet, G.; Van Der Heijden, G.J.; Bouter, L.M. Therapeutic ultrasound for acute ankle sprains. Eur. J. Phys. Rehabil. Med. 2012, 48, 325–334. [Google Scholar] [CrossRef]
- Papadopoulos, E.S.; Mani, R. The Role of Ultrasound Therapy in the Management of Musculoskeletal Soft Tissue Pain. Int. J. Low. Extrem. Wounds 2020, 19, 350–358. [Google Scholar] [CrossRef]
- Hubbard, T.J.; Denegar, C.R. Does cryotherapy improve outcomes with soft tissue injury? J. Athl. Train. 2004, 39, 278–279. [Google Scholar]
- Collins, N.C. Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? Emerg. Med. J. 2008, 25, 65–68. [Google Scholar] [CrossRef]
- Miranda, J.P.; Silva, W.T.; Silva, H.J.; Mascarenhas, R.O.; Oliveira, V.C. Effectiveness of cryotherapy on pain intensity, swelling, range of motion, function and recurrence in acute ankle sprain: A systematic review of randomized controlled trials. Phys. Ther. Sport. 2021, 49, 243–249. [Google Scholar] [CrossRef]
- Kwiecien, S.Y.; McHugh, M.P. The cold truth: The role of cryotherapy in the treatment of injury and recovery from exercise. Eur. J. Appl. Physiol. 2021, 121, 2125–2142. [Google Scholar] [CrossRef] [PubMed]
- Thacoor, A.; Sandiford, N.A. Cryotherapy following total knee arthroplasty: What is the evidence? J. Orthop. Surg. 2019, 27, 2309499019832752. [Google Scholar] [CrossRef]
- Garcia, C.; Karri, J.; Zacharias, N.A.; Abd-Elsayed, A. Use of Cryotherapy for Managing Chronic Pain: An Evidence-Based Narrative. Pain Ther. 2021, 10, 81–100. [Google Scholar] [CrossRef]
- Agostini, F.; Bernetti, A.; Santilli, G.; Damiani, C.; Santilli, V.; Paoloni, M.; Mangone, M. Efficacy of ultrasound therapy combined with cryotherapy in pain management and rehabilitation in patients with Achilles tendinopathy: A retrospective observational study. Clin. Ter. 2023, 174, 148–151. [Google Scholar] [CrossRef]
- Costantino, C.; Vulpiani, M.C.; Romiti, D.; Vetrano, M.; Saraceni, V.M. Cryoultrasound therapy in the treatment of chronic plantar fasciitis with heel spurs, A randomized controlled clinical study. Eur. J. Phys. Rehabil. Med. 2014, 50, 39–47. [Google Scholar]
- Lee, K.-S.; Wang, J.-W.; Lee, D.Y.; Yu, J.H.; Kim, J.S.; Kim, S.G.; Hong, J. heon Effects of Progressive Core and Ankle Muscle Strengthening Exercises Using Thera-Band on Body Balance. J. Korean Phys. Ther. 2022, 34, 121–127. [Google Scholar] [CrossRef]
- Bleakley, C.M.; Taylor, J.B.; Dischiavi, S.L.; Doherty, C.; Delahunt, E. Rehabilitation Exercises Reduce Reinjury Post Ankle Sprain, But the Content and Parameters of an Optimal Exercise Program Have Yet to Be Established: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 1367–1375. [Google Scholar] [CrossRef]
- Logan, C.A.; Asnis, P.D.; Provencher, M.T. The role of therapeutic modalities in surgical and nonsurgical management of orthopaedic injuries. J. Am. Acad. Orthop. Surg. 2017, 25, 556–568. [Google Scholar] [CrossRef] [PubMed]
- Kemler, E.; Van De Port, I.; Backx, F.; Van Dijk, C.N. A systematic review on the treatment of acute ankle sprain: Brace versus other functional treatment types. Sport Med. 2011, 41, 185–197. [Google Scholar] [CrossRef]
- Swiontkowski, M.F. A Systematic Review on the Treatment of Acute Ankle Sprain: Brace versus Other Functional Treatment Types. Yearb. Orthop. 2011, 2011, 93–96. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Delahunt, E.; Holden, S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br. J. Sports Med. 2017, 51, 113–125. [Google Scholar] [CrossRef]
- Charly Daniel, D. Effects of ultrasound therapy with taping PNF training and PNF training with taping in treatment and rehabilitation of sports injuries of high ankle sprain. J. Dr. NTR Univ. Health Sci. 2017, 6, 92. [Google Scholar] [CrossRef]
- Kinkade, S. Evaluation and treatment of acute low back pain. Am. Fam. Physician 2007, 75, 1181–1188. [Google Scholar]
- Costello, J.T.; Algar, L.A.; Donnelly, A.E. Effects of whole-body cryotherapy (−110 °C) on proprioception and indices of muscle damage. Scand. J. Med. Sci. Sport 2012, 22, 190–198. [Google Scholar] [CrossRef]
- Olaussen, M.; Holmedal, Ø.; Lindbaek, M.; Brage, S. Physiotherapy alone or in combination with corticosteroid injection for acute lateral epicondylitis in general practice: A protocol for a randomised, placebo-controlled study. BMC Musculoskelet Disord. 2009, 10, 152. [Google Scholar] [CrossRef][Green Version]
- Martins, C.N.; Moraes, M.B.; Hauck, M.; Guerreiro, L.F.; Rossato, D.D.; Varela, A.S.; da Rosa, C.E.; Signori, L.U. Effects of cryotherapy combined with therapeutic ultrasound on oxidative stress and tissue damage after musculoskeletal contusion in rats. Physiotherapy 2016, 102, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Malanga, G.A.; Yan, N.; Stark, J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad. Med. 2015, 127, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Farahbod, F. The efficacy of thermotherapy and cryotherapy on pain relief in patients with acute low back pain, a clinical trial study. J. Clin. Diagn. Res. 2014, 8, LC01–LC04. [Google Scholar] [CrossRef] [PubMed]
- Marques, J.P. Comment—Diagnosis, Treatment and Prevention of Ankle Sprains: Update of an Evidence-based Clinical Guideline. Rev. Med. Desportiva Inf. 2019, 10, 25. [Google Scholar] [CrossRef]
- Vuurberg, G.; Hoorntje, A.; Wink, L.M.; Van Der Doelen, B.F.W.; Van Den Bekerom, M.P.; Dekker, R.; Van Dijk, C.N.; Krips, R.; Loogman, M.C.M.; Ridderikhof, M.L.; et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br. J. Sports Med. 2018, 52, 956. [Google Scholar] [CrossRef] [PubMed]
- Kennet, J.; Hardaker, N.; Hobbs, S.; Selfe, J. Cooling efficiency of 4 common cryotherapeutic agents. J. Athl. Train. 2007, 42, 343–348. [Google Scholar]
- Herring, S.A.; Kibler, W.B.; Putukian, M. The team physician and the return-to-play decision: A consensus statement—2012 update. Med. Sci. Sports Exerc. 2012, 44, 2446–2448. [Google Scholar] [CrossRef]
- Herring, S.A.; Bergfeld, J.A.; Boyd, J.; Duffey, T.; Fields, K.B.; Grana, W.A.; Indelicato, P.; Kibler, W.B.; Pallay, R.; Putukian, M.; et al. The team physician and return-to-play issues: A consensus statement. Med. Sci. Sports Exerc. 2002, 34, 1212–1214. [Google Scholar] [CrossRef]
- Laker, S.R. Return-to-Play Decisions. Phys. Med. Rehabil. Clin. N. Am. 2011, 22, 619–634. [Google Scholar] [CrossRef] [PubMed]
- Creighton, D.W.; Shrier, I.; Shultz, R.; Meeuwisse, W.H.; Matheson, G.O. Return-to-play in sport: A decision-based model. Clin. J. Sport Med. 2010, 20, 379–385. [Google Scholar] [CrossRef]
- Shrier, I. Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making. Br. J. Sports Med. 2015, 49, 1311–1315. [Google Scholar] [CrossRef]
- Matheson, G.O.; Shultz, R.; Bido, J.; Mitten, M.J.; Meeuwisse, W.H.; Shrier, I. Return-to-play decisions: Are they the team Physician’s responsibility? Clin. J. Sport. Med. 2011, 21, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Richie, D.H.; Izadi, F.E. Return to play after an ankle sprain: Guidelines for the podiatric physician. Clin. Podiatr. Med. Surg. 2015, 32, 195–215. [Google Scholar] [CrossRef]
- Salameh, M.; Hantouly, A.T.; Rayyan, A.; Dabbas, J.; Toubasi, A.A.; Hartnett, D.A.; Blankenhorn, B. Return to Play After Isolated Syndesmotic Ligamentous Injury in Athletes: A Systematic Review and Meta-analysis. Foot Ankle Orthop. 2022, 7, 24730114221096482. [Google Scholar] [CrossRef]
- Vancolen, S.Y.; Nadeem, I.; Horner, N.S.; Johal, H.; Alolabi, B.; Khan, M. Return to Sport After Ankle Syndesmotic Injury: A Systematic Review. Sports Health 2019, 11, 116–122. [Google Scholar] [CrossRef]
- de Sire, A.; Demeco, A.; Marotta, N.; Moggio, L.; Palumbo, A.; Iona, T.; Ammendolia, A. Anterior Cruciate Ligament Injury Prevention Exercises: Could a Neuromuscular Warm-Up Improve Muscle Pre-Activation before a Soccer Game? A Proof-of-Principle Study on Professional Football Players. Appl. Sci. 2021, 11, 4958. [Google Scholar] [CrossRef]
- Polzer, H.; Kanz, K.G.; Prall, W.C.; Haasters, F.; Ockert, B.; Mutschler, W.; Grote, S. Diagnosis and treatment of acute ankle injuries: Development of an evidence-based algorithm. Orthop. Rev. 2012, 4, e5. [Google Scholar] [CrossRef]
- Muftic, M.; Miladinovic, K. Therapeutic ultrasound and pain in degenerative diseases of musculoskeletal system. Acta Inform. Medica 2013, 21, 170–172. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Marotta, N.; Demeco, A.; Moggio, L.; Paola, P.; Marotta, M.; Iona, T.; Invernizzi, M.; Leigheb, M.; Ammendolia, A. Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study. Diagnostics. 2021, 11, 997. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Group Exp (n = 13) | Group Cnt (n = 12) | p-Value |
|---|---|---|---|
| Age (y), mean ± SD (range) | 22.5 ± 12.4 (18 to 41) | 23.1 ± 11.5 (21 to 38) | 0.114 |
| Weight (kg) | 75.1 ± 13 (47 to 88) | 77 ± 14 (50 to 92) | 0.085 |
| Body mass index, mean ± SD | 23.2 ± 4 (19 to 29) | 22.9 ± 5 (18 to 30) | 0.102 |
| NRS (0–10), mean ± SD | 7.69 ± 2.19 | 7.79 ± 1.19 | 0.214 |
| EQ-5D-3L Index, mean ± SD | 0.5 ± 0.3 | 0.6 ± 0.2 | 0.112 |
| FADI (0–104), mean ± SD | 32.9 ± 10.5 | 28.3 ± 10.6 | 0.079 |
| T0 | T1 | ∆T0-T1 | T2 | ∆T1-T2 | T3 | ∆T2-T3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| p | ES | p | ES | p | ES | ||||||
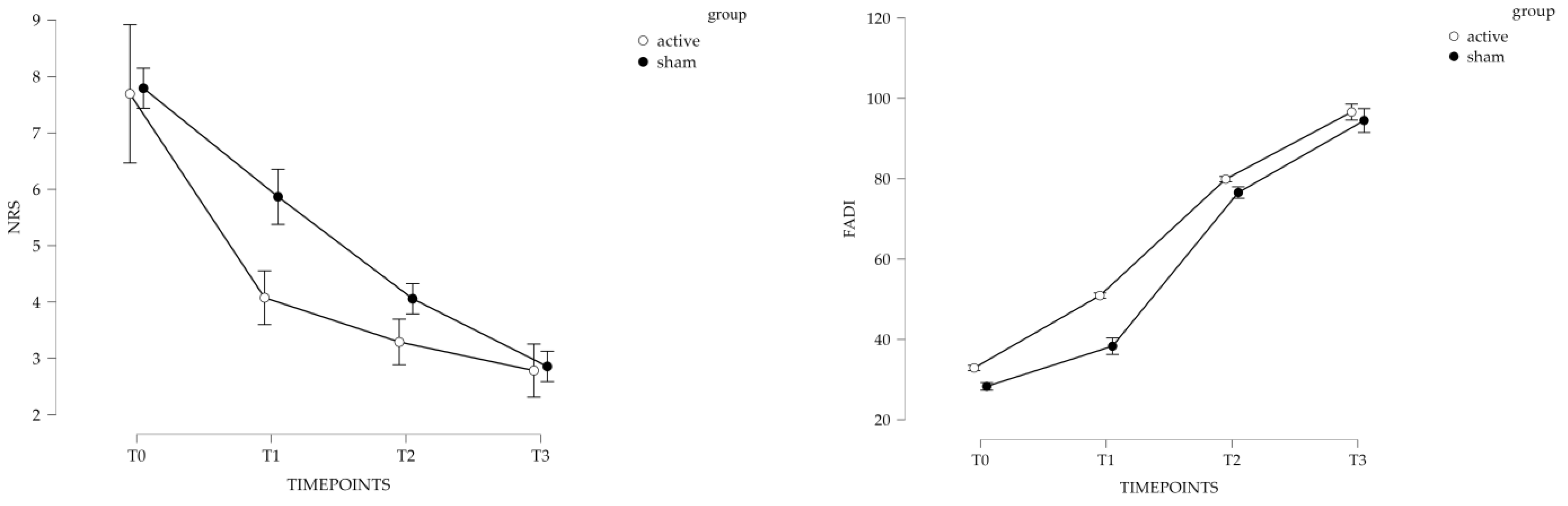
| NRS (0–10) | active | 7.69 ± 2.19 | 4.08 ± 1.29 | 0.006 | −0.9 | 3.29 ± 1.05 | 0.041 | −0.3 | 2.78 ± 0.91 | 0.083 | −0.5 |
| sham | 7.79 ± 1.19 | 5.87 ± 1.19 | 0.009 | −0.6 | 4.06 ± 1.37 | 0.052 | −0.4 | 2.86 ± 1.37 | 0.042 | −0.5 | |
| FADI (0–104) | active | 32.9 ± 10.5 | 50.9 ± 10.3 | 0.031 | 0.7 | 79.9 ± 8.5 | 0.005 | 0.7 | 96.6 ± 7.6 | 0.012 | 0.6 |
| sham | 28.3 ± 10.6 | 38.3 ± 11.5 | 0.027 | 0.5 | 76.6 ± 11.2 | 0.009 | 0.5 | 94.5 ± 7.1 | 0.039 | 0.6 | |
| EQ-5D-3L | active | 0.5 ± 0.3 | 0.6 ± 0.2 | 0.106 | 0.1 | 0.7 ± 0.3 | 0.093 | 0.0 | 0.7 ± 0.3 | 0.0 | −0.7 |
| sham | 0.6 ± 0.2 | 0.7 ± 0.3 | 0.124 | 0.1 | 0.7 ± 0.2 | 0.082 | 0.0 | 0.7 ± 0.2 | 0.0 | −0.7 | |
| T0 | T1 | T2 | T3 | ANOVA-RM | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| p -Value | ES | p -Value | ES | p -Value | ES | p -Value | ES | p-Value | ||
| NRS | active | 0.744 | −0.06 | 0.003 | −0.69 | 0.212 | −0.65 | 0.534 | −0.06 | 0.002 |
| sham | ||||||||||
| FADI | active | 0.2 | 0.20 | 0.021 | 0.57 | 0.345 | 0.23 | 0.386 | 0.21 | 0.039 |
| sham | ||||||||||
| EQ-5D-3L Index | active | 0.106 | 0.11 | 0.127 | 0.21 | 0.242 | 0.13 | 0.342 | 0.09 | 0.128 |
| sham | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ammendolia, A.; de Sire, A.; Lippi, L.; Ammendolia, V.; Spanò, R.; Reggiani, A.; Invernizzi, M.; Marotta, N. Cryo plus Ultrasound Therapy, a Novel Rehabilitative Approach for Football Players with Acute Lateral Ankle Injury Sprain: A Pilot Randomized Controlled Trial. Sports 2023, 11, 180. https://doi.org/10.3390/sports11090180
Ammendolia A, de Sire A, Lippi L, Ammendolia V, Spanò R, Reggiani A, Invernizzi M, Marotta N. Cryo plus Ultrasound Therapy, a Novel Rehabilitative Approach for Football Players with Acute Lateral Ankle Injury Sprain: A Pilot Randomized Controlled Trial. Sports. 2023; 11(9):180. https://doi.org/10.3390/sports11090180
Chicago/Turabian StyleAmmendolia, Antonio, Alessandro de Sire, Lorenzo Lippi, Valerio Ammendolia, Riccardo Spanò, Andrea Reggiani, Marco Invernizzi, and Nicola Marotta. 2023. "Cryo plus Ultrasound Therapy, a Novel Rehabilitative Approach for Football Players with Acute Lateral Ankle Injury Sprain: A Pilot Randomized Controlled Trial" Sports 11, no. 9: 180. https://doi.org/10.3390/sports11090180
APA StyleAmmendolia, A., de Sire, A., Lippi, L., Ammendolia, V., Spanò, R., Reggiani, A., Invernizzi, M., & Marotta, N. (2023). Cryo plus Ultrasound Therapy, a Novel Rehabilitative Approach for Football Players with Acute Lateral Ankle Injury Sprain: A Pilot Randomized Controlled Trial. Sports, 11(9), 180. https://doi.org/10.3390/sports11090180











