Jones Fracture in the National Football League
Abstract
:1. Introduction
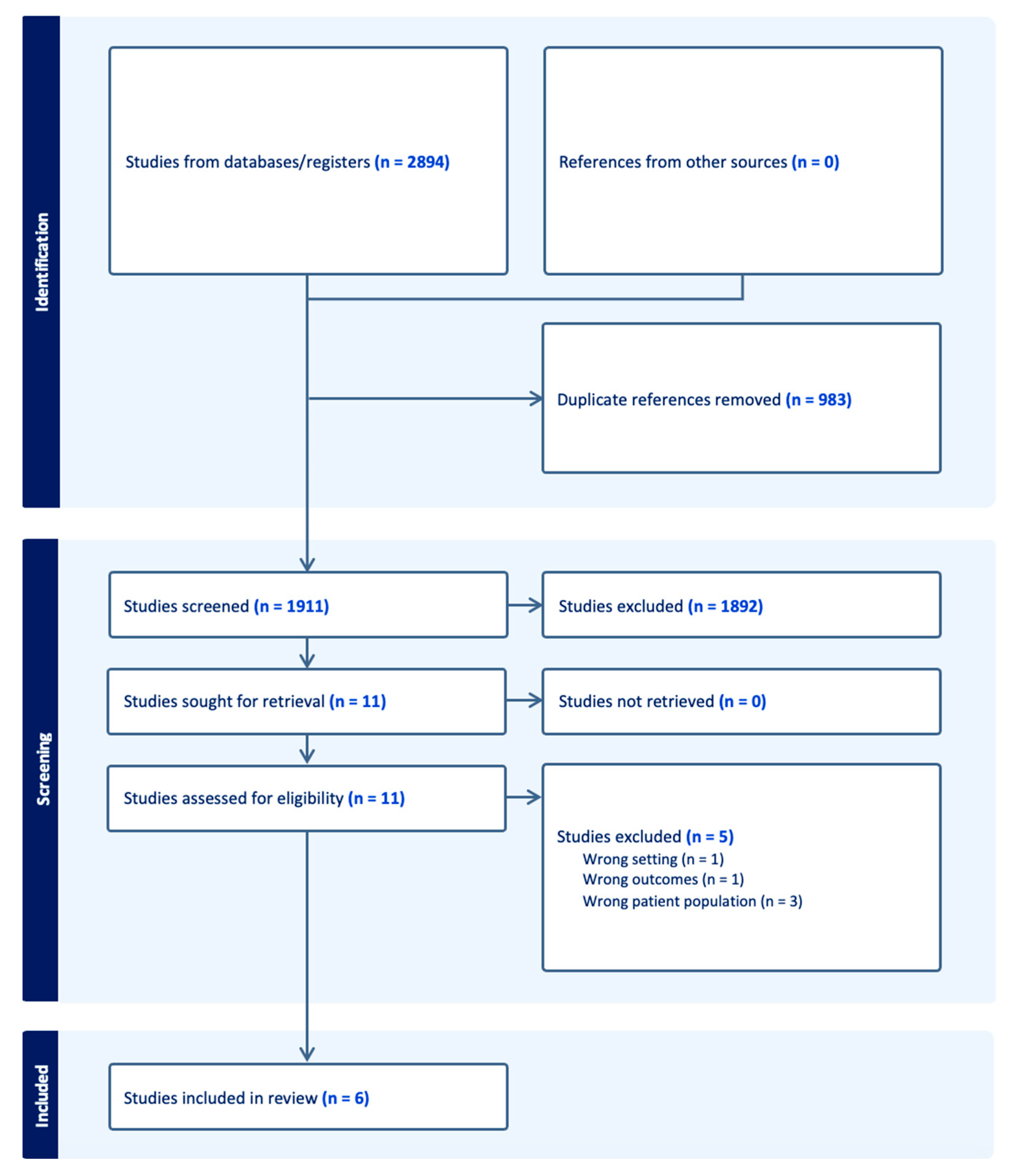
2. Materials and Methods
2.1. Search and Screening of the Literature
2.2. Risk of Bias and Quality Assessment
3. Results
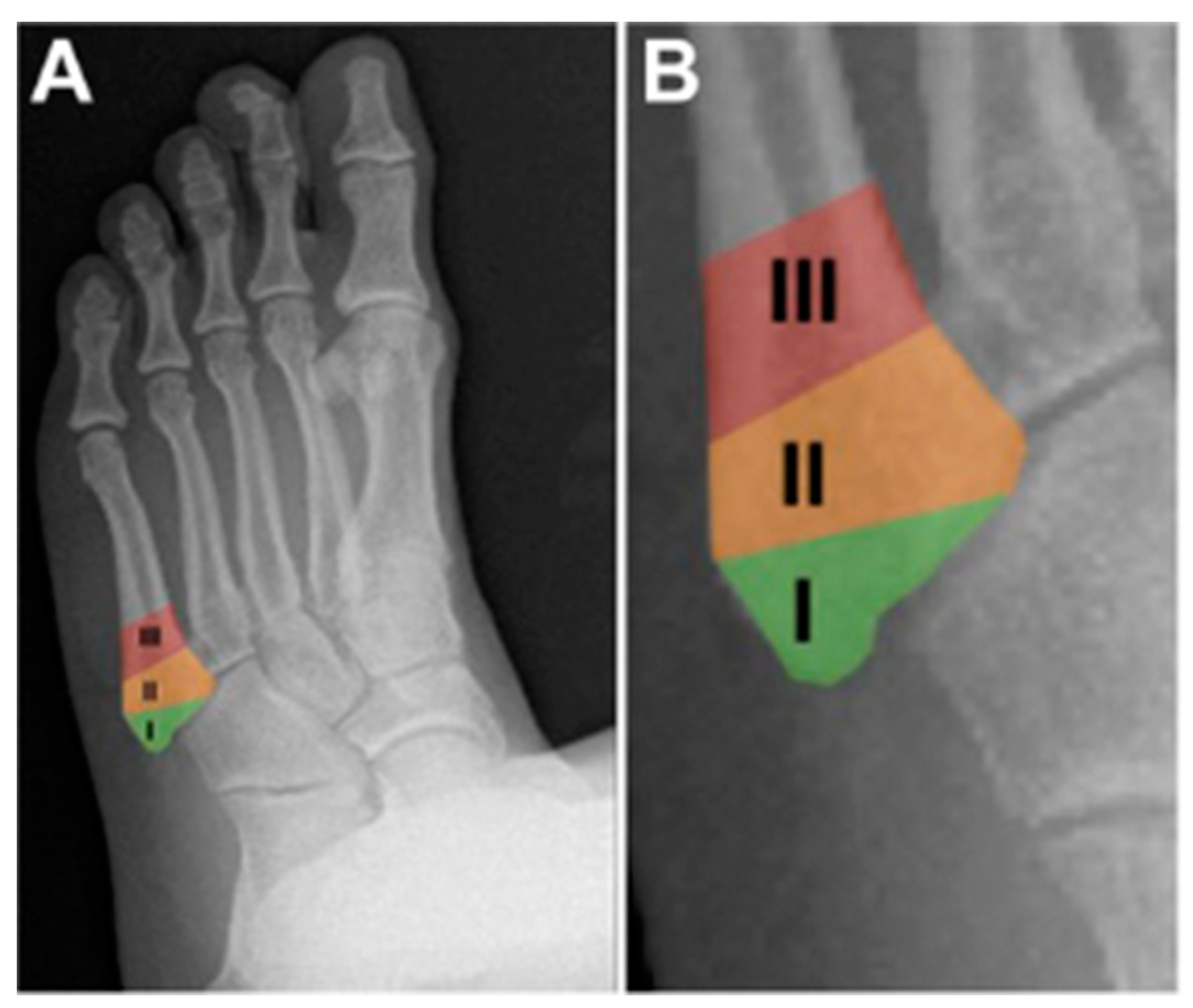
3.1. Classification
3.2. Diagnosis
3.3. Treatment Considerations
3.3.1. Non-Operative Treatment
3.3.2. Surgical Treatment Techniques
3.4. Rehabilitation and Return to Play
3.5. Complications
3.6. NFL RTP and Outcomes
3.6.1. Treatment Methodology
3.6.2. RTP Outcomes
3.6.3. Draft Prospective and NFL Performance
4. Discussion
4.1. Overview
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

| Nonrandomized Cohort Studies | ||||||
|---|---|---|---|---|---|---|
| MINORS | Tu 2018 [6] | Spang 2018 [5] | Singh 2018 [15] | Lareau 2016 [14] | Carreira 2013 [2] | Low 2004 [11] |
| A clearly stated aim | 2 | 2 | 2 | 2 | 2 | 2 |
| Inclusion of consecutive patients | 2 | 2 | 1 | 2 | 2 | 2 |
| Prospective collection of data | 0 | 0 | 0 | 0 | 2 | 1 |
| Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 |
| Unbiased assessment of study endpoint | 1 | 2 | 1 | 2 | 2 | 1 |
| Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 |
| Loss to follow up less than 5% | 2 | 2 | 2 | 2 | 2 | 2 |
| Prospective calculation of the study size | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 11 | 12 | 10 | 12 | 14 | 12 |
References
- Sammarco, G.J. The Jones fracture. Instr. Course Lect. 1993, 42, 201–205. [Google Scholar]
- Carreira, D.S.; Sandilands, S.M. Radiographic Factors and Effect of Fifth Metatarsal Jones and Diaphyseal Stress Fractures on Participation in the NFL. Foot Ankle Int. 2013, 34, 518–522. [Google Scholar] [CrossRef]
- Hsu, A.R.; Anderson, R.B. Foot and Ankle Injuries in American Football. Am. J. Orthop. 2016, 45, 358–367. [Google Scholar]
- Petrisor, B.A.; Ekrol, I.; Court-Brown, C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006, 27, 172–174. [Google Scholar] [CrossRef]
- Spang, R.C.; Haber, D.B.; Beaulieu-Jones, B.R.; Stupay, K.L.; Sanchez, G.; Sanchez, A.; Murphy, C.P.; Whalen, J.M.; Van Allen, J.J.; Price, M.D.; et al. Jones Fractures Identified at the National Football League Scouting Combine: Assessment of Prognostic Factors, Computed Tomography Findings, and Initial Career Performance. Orthop. J. Sports Med. 2018, 6, 2325967118790740. [Google Scholar] [CrossRef]
- Tu, L.A.; Knapik, D.M.; Sheehan, J.; Salata, M.J.; Voos, J.E. Prevalence of Jones Fracture Repair and Impact on Short-Term NFL Participation. Foot Ankle Int. 2018, 39, 6–10. [Google Scholar] [CrossRef]
- Hoffman, J.R. The applied physiology of American football. Int. J. Sports Physiol. Perform. 2008, 3, 387–392. [Google Scholar] [CrossRef]
- Solarino, G.; Bortone, I.; Vicenti, G.; Bizzoca, D.; Coviello, M.; Maccagnano, G.; Moretti, B.; D’Angelo, F. Role of biomechanical assessment in rotator cuff tear repair: Arthroscopic vs mini-open approach. World J. Orthop. 2021, 12, 991–1000. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Andrews, J.R. Shoulder muscle recruitment patterns and related biomechanics during upper extremity sports. Sports Med. 2009, 39, 569–590. [Google Scholar] [CrossRef]
- Goodloe, J.B.; Cregar, W.M.; Caughman, A.; Bailey, E.P.; Barfield, W.R.; Gross, C.E. Surgical Management of Proximal Fifth Metatarsal Fractures in Elite Athletes: A Systematic Review. Orthop. J. Sports Med. 2021, 9, 23259671211037647. [Google Scholar] [CrossRef]
- Low, K.; Noblin, J.D.; Browne, J.E.; Barnthouse, C.D.; Scott, A.R. Jones fractures in the elite football player. J. Surg. Orthop. Adv. 2004, 13, 156–160. [Google Scholar]
- Abed, V.; Fine, R.; Fine, R.; Hawk, G.S.; Conley, C.; Jacobs, C.; Stone, A.V. Return to Play, Performance, and Economic Analysis of National Football League Players After Lisfranc Injury. Orthop. J. Sports Med. 2023, 11, 23259671231159935. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lareau, C.R.; Hsu, A.R.; Anderson, R.B. Return to Play in National Football League Players After Operative Jones Fracture Treatment. Foot Ankle Int. 2016, 37, 8–16. [Google Scholar] [CrossRef]
- Singh, S.K.; Larkin, K.E.; Kadakia, A.R.; Hsu, W.K. Risk Factors for Reoperation and Performance-Based Outcomes After Operative Fixation of Foot Fractures in the Professional Athlete: A Cross-Sport Analysis. Sports Health 2018, 10, 70–74. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Stewart, I.M. Jones’s Fracture: Fracture of Base of Fifth Metatarsal. Clin. Orthop. Relat. Res. 1960, 16, 190–198. [Google Scholar]
- Torg, J.S.; Balduini, F.C.; Zelko, R.R.; Pavlov, H.; Peff, T.C.; Das, M. Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J. Bone Joint Surg. Am. 1984, 66, 209–214. [Google Scholar] [CrossRef]
- Dameron, T.B., Jr. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J. Bone Joint Surg. Am. 1975, 57, 788–792. [Google Scholar] [CrossRef]
- Lawrence, S.J.; Botte, M.J. Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle 1993, 14, 358–365. [Google Scholar] [CrossRef]
- Dameron, T.B., Jr. Fractures of the Proximal Fifth Metatarsal: Selecting the Best Treatment Option. J. Am. Acad. Orthop. Surg. 1995, 3, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Michalski, M.P.; Ingall, E.M.; Kwon, J.Y.; Chiodo, C.P. Reliability of Fifth Metatarsal Base Fracture Classifications and Current Management. Foot Ankle Int. 2022, 43, 1034–1040. [Google Scholar] [CrossRef] [PubMed]
- Metzl, J.A.; Bowers, M.W.; Anderson, R.B. Fifth Metatarsal Jones Fractures: Diagnosis and Treatment. JAAOS-J. Am. Acad. Orthop. Surg. 2022, 30, e470–e479. [Google Scholar] [CrossRef] [PubMed]
- Riegger, M.; Muller, J.; Giampietro, A.; Saporito, A.; Filardo, G.; Treglia, G.; Guidi, M.; Candrian, C. Forefoot Adduction, Hindfoot Varus or Pes Cavus: Risk Factors for Fifth Metatarsal Fractures and Jones Fractures? A Systematic Review and Meta-Analysis. J. Foot Ankle Surg. 2022, 61, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Raikin, S.M.; Slenker, N.; Ratigan, B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: The Jones fracture. Am. J. Sports Med. 2008, 36, 1367–1372. [Google Scholar] [CrossRef]
- Fleischer, A.E.; Stack, R.; Klein, E.E.; Baker, J.R.; Weil, L., Jr.; Weil, L.S., Sr. Forefoot Adduction Is a Risk Factor for Jones Fracture. J. Foot Ankle Surg. 2017, 56, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Khairul Faizi Mohammad, B.Y. Nonoperative Treatment—Proximal articular fractures of the 5th metatarsal (Jones fracture). In AO Surgery Reference; Nousiainen, M.T., Buckley, R., Eds.; Available online: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/metatarsals/release-notes (accessed on 1 December 2023).
- Bezuglov, E.; Zholinsky, A.; Chernov, G.; Khaitin, V.; Goncharov, E.; Waskiewicz, Z.; Barskova, E.; Lazarev, A. Conservative Treatment of the Fifth Metatarsal Bone Fractures in Professional Football Players Using Platelet-Rich Plasma. Foot Ankle Spec. 2022, 15, 62–66. [Google Scholar] [CrossRef]
- Nishikawa, D.R.C.; Aires Duarte, F.; Saito, G.H.; Bang, K.E.; Monteiro, A.C.; Prado, M.P.; de Cesar Netto, C. Treatment of Zone 1 Fractures of the Proximal Fifth Metatarsal With CAM-Walker Boot vs Hard-Soled Shoes. Foot Ankle Int. 2020, 41, 508–512. [Google Scholar] [CrossRef]
- Attia, A.K.; Taha, T.; Kong, G.; Alhammoud, A.; Mahmoud, K.; Myerson, M. Return to Play and Fracture Union After the Surgical Management of Jones Fractures in Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2021, 49, 3422–3436. [Google Scholar] [CrossRef]
- Bernstein, D.T.; Mitchell, R.J.; McCulloch, P.C.; Harris, J.D.; Varner, K.E. Treatment of Proximal Fifth Metatarsal Fractures and Refractures With Plantar Plating in Elite Athletes. Foot Ankle Int. 2018, 39, 1410–1415. [Google Scholar] [CrossRef]
- Chloros, G.D.; Kakos, C.D.; Tastsidis, I.K.; Giannoudis, V.P.; Panteli, M.; Giannoudis, P.V. Fifth metatarsal fractures: An update on management, complications, and outcomes. EFORT Open Rev. 2022, 7, 13–25. [Google Scholar] [CrossRef]
- Cheung, C.N.; Lui, T.H. Proximal Fifth Metatarsal Fractures: Anatomy, Classification, Treatment and Complications. Arch. Trauma. Res. 2016, 5, e33298. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, M.; DeSandis, B.; Allen, A.; Levitsky, M.; O’Malley, Q.; Williams, R. Operative Treatment of Fifth Metatarsal Jones Fractures (Zones II and III) in the NBA. Foot Ankle Int. 2016, 37, 488–500. [Google Scholar] [CrossRef] [PubMed]
- Young, K.W.; Kim, J.S.; Lee, H.S.; Jegal, H.; Park, Y.U.; Lee, K.T. Operative Results of Plantar Plating for Fifth Metatarsal Stress Fracture. Foot Ankle Int. 2020, 41, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Albloushi, M.; Alshanqiti, A.; Qasem, M.; Abitbol, A.; Gregory, T. Jones type fifth metatarsal fracture fixation in athletes: A review and current concept. World J. Orthop. 2021, 12, 640–650. [Google Scholar] [CrossRef]
- Larson, C.M.; Almekinders, L.C.; Taft, T.N.; Garrett, W.E. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am. J. Sports Med. 2002, 30, 55–60. [Google Scholar] [CrossRef]
- Wright, R.W.; Fischer, D.A.; Shively, R.A.; Heidt, R.S.; Nuber, G.W. Refracture of proximal fifth metatarsal (Jones) fracture after intramedullary screw fixation in athletes. Am. J. Sports Med. 2000, 28, 732–736. [Google Scholar] [CrossRef]
- Smith, J.W.; Arnoczky, S.P.; Hersh, A. The intraosseous blood supply of the fifth metatarsal: Implications for proximal fracture healing. Foot Ankle 1992, 13, 143–152. [Google Scholar] [CrossRef]
- Rosenberg, G.A.; Sferra, J.J. Treatment strategies for acute fractures and nonunions of the proximal fifth metatarsal. J. Am. Acad. Orthop. Surg. 2000, 8, 332–338. [Google Scholar] [CrossRef]
- Nolte, P.; Anderson, R.; Strauss, E.; Wang, Z.; Hu, L.; Xu, Z.; Steen, R.G. Heal rate of metatarsal fractures: A propensity-matching study of patients treated with low-intensity pulsed ultrasound (LIPUS) vs. surgical and other treatments. Injury 2016, 47, 2584–2590. [Google Scholar] [CrossRef]
- Blum, A.; Zarqh, O.; Peleg, A.; Sirchan, R.; Blum, N.; Salameh, Y.; Ganaem, M. Vascular inflammation and endothelial dysfunction in fracture healing. Am. J. Orthop. 2012, 41, 87–91. [Google Scholar]
- Jiao, H.; Xiao, E.; Graves, D.T. Diabetes and Its Effect on Bone and Fracture Healing. Curr. Osteoporos. Rep. 2015, 13, 327–335. [Google Scholar] [CrossRef]
- Karlamangla, A.S.; Burnett-Bowie, S.M.; Crandall, C.J. Bone Health During the Menopause Transition and Beyond. Obstet. Gynecol. Clin. N. Am. 2018, 45, 695–708. [Google Scholar] [CrossRef]
- Brinker, M.R.; O’Connor, D.P.; Monla, Y.T.; Earthman, T.P. Metabolic and endocrine abnormalities in patients with nonunions. J. Orthop. Trauma. 2007, 21, 557–570. [Google Scholar] [CrossRef]


| (a) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Study Group (Year) | Sample Size | Treatment | RTP Outcomes | Overall Outcomes | Position Data | Complications | Revision Outcomes | Quality Assessment |
| Low, 2004 [11] | NFL Combine (1988–2002) | 86 Jones fractures | Non-operative, operative (IM screw) | 86% RTP in 6–12 weeks | Operative: 43/46 fractures healed without problems, | Higher incidence of fractures in offensive vs. defensive players (61% vs. 39%). Most common positions: offensive, defensive linemen | Non-operative: 20% nonunion Operative: 7% nonunion | NR | 12 |
| Carreira, 2013 [2] | NFL Combine (2004–2009) | 45 Jones fractures | Operative (IM Screw) | NR | no significant differences in being drafted, increased number of players who played <10 games in NFL | NR | NR | NR | 14 |
| Lareau, 2016 [14] | NFL athletes (2004–2014) | 25 Jones fractures | Operative (IM screw + BMAC + DBM) | 25/25 (100%) RTP, average 8.7 weeks | 80% still playing by end of season, average of 2.7 season played post-injury, 2 pro-bowl players after surgery | NR | 12% refracture + required revision surgery | NR | 12 |
| Singh, 2018 [15] | NFL athletes (1986–2016) | 17 Jones Fractures | Operative | RTP median = 189 days (27 weeks) | Drop in performance level after surgery, mean average career after surgery: 3.8 +/− 3.7 years | NR | No refractures | NR | 10 |
| Spang, 2018 [5] | NFL Combine (2009–2015) | 72 Jones fractures | Operative (IM Screw) | 67/72 (93%) athletes did not miss any collegiate games | 46/72 players >2 years in NFL, higher mean overall draft pick number, more athletes undrafted, lower fantasy scores, lower snap percentages | Tight ends more likely to have Jones fractures, defensive backs and running backs have lower risk | 50% showed incomplete healing at Combine | NR | 12 |
| Tu, 2018 [6] | NFL Combine (2012–2015) | 40 Jones Fractures | Operative (IM screw +/− BMAC + DBM) | Average time from surgery to Combine: 27 +/− 22.3 months | No limitations in strength/ROM, no increased risk of going undrafted, playing, or starting in NFL games | Highest prevalence of fracture repair in defensive lineman, highest rate of fracture in tight ends | 7.5% re-fracture rate requiring revision surgery, incomplete bony union in 8% fractures | RTP 15 weeks for re-fractures, no association between RTP and refracture rate, 100% had CT evidence of union | 11 |
| (b) | |||||||||
| Author, Year | Study Conclusion | ||||||||
| Low, 2004 [11] | IM screw fixation of Jones fracture is the treatment of choice for elite college and professional football athletes. | ||||||||
| Carreira, 2013 [2] | No statistically significant difference in NFL participation after Jones fracture, though there was a trend towards decreased participation. | ||||||||
| Lareau, 2016 [14] | IM screw fixation and aggressive rehabilitation protocol allowed for early RTP and low refracture rate in NFL athletes. All players returned to play. | ||||||||
| Singh, 2018 [15] | Regardless of sport or fracture location, athletes returned to play at a high rate after foot fracture location and had excellent post-operative performance levels. | ||||||||
| Spang, 2018 [5] | On CT scan, 50% of all NFL Combine players with a previous Jones fracture had incomplete healing. Players with fractures had lower position-specific performance scores over the first 2 years of career. Players with lower CT scores started fewer games and were drafted later. | ||||||||
| Tu, 2018 [6] | Players with Jones fracture repair did not have a significantly increased risk of going undrafted or having decreased participation in their first NFL season. | ||||||||
| Jones Fracture in the NFL | |
|---|---|
| Incidence | 17.8% of all foot fractures |
| Average time to RTP | Range: 6–27 weeks |
| Incidence of complications | Operative management: refracture: 4–12%; incomplete healing: 7–50% Non-operative management: 20% nonunion |
| Main treatment modality | Intramedullary screw fixation; may also include BMAC + DBM |
| Rehabilitation | Non-weight bearing → toe-touch weight bearing → increase exercise intensity incrementally +/− low intensity pulsed ultrasound bone stimulator |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, E.J.; Anastasio, A.T.; Stauffer, T.; Grant, C.; Wu, C.J.; Wu, K.A.; Kaplan, S.; Lau, B.C. Jones Fracture in the National Football League. Sports 2024, 12, 7. https://doi.org/10.3390/sports12010007
Luo EJ, Anastasio AT, Stauffer T, Grant C, Wu CJ, Wu KA, Kaplan S, Lau BC. Jones Fracture in the National Football League. Sports. 2024; 12(1):7. https://doi.org/10.3390/sports12010007
Chicago/Turabian StyleLuo, Emily J., Albert T. Anastasio, Taylor Stauffer, Caitlin Grant, Christine J. Wu, Kevin A. Wu, Samantha Kaplan, and Brian C. Lau. 2024. "Jones Fracture in the National Football League" Sports 12, no. 1: 7. https://doi.org/10.3390/sports12010007
APA StyleLuo, E. J., Anastasio, A. T., Stauffer, T., Grant, C., Wu, C. J., Wu, K. A., Kaplan, S., & Lau, B. C. (2024). Jones Fracture in the National Football League. Sports, 12(1), 7. https://doi.org/10.3390/sports12010007








