The Effect of Task-Oriented Basketball Training on Motor Skill-Related Fitness in Children with Developmental Coordination Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
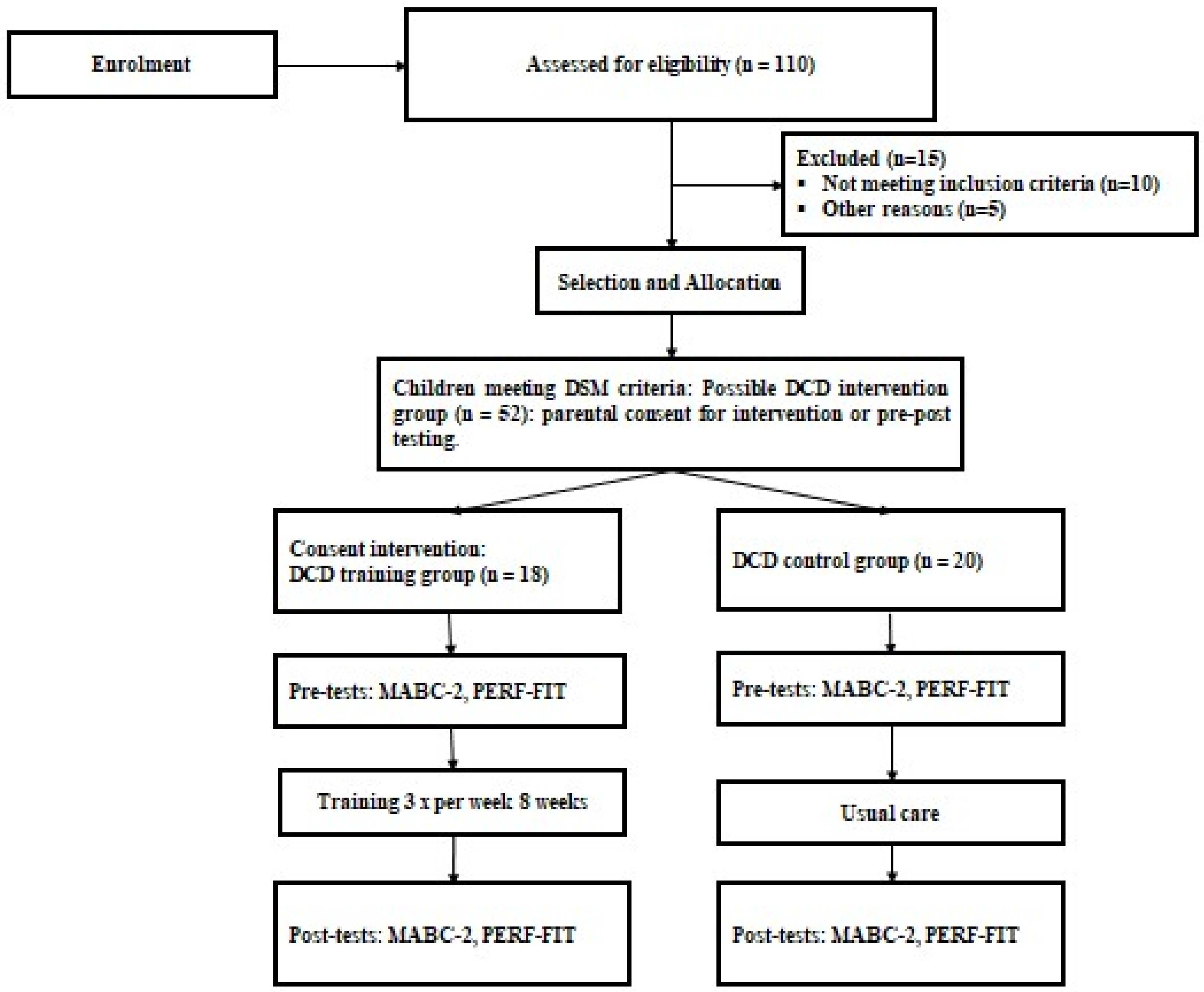
2.2. Participants
2.3. Measurements
2.3.1. The Movement Assessment Battery for Children-2 (MABC-2)
2.3.2. Performance and Fitness Test Battery (PERF-FIT)
2.4. Training Program
2.5. Statistical Procedure
3. Results
3.1. Participants
3.2. Comparison Between Type of Intervention on Pre- and Post-Data
3.2.1. MABC-2
3.2.2. PERF-FIT Motor Skill Performance
3.2.3. PERF-FIT Agility and Power
4. Discussion
4.1. Limitations and Perspectives
4.2. Practical Implications
- Integrate structured motor skill programs into physical education or extracurricular activities to address motor challenges alongside academic learning [22].
- Implement sport-based, task-oriented training, such as basketball, to improve specific motor skills and enhance coordination and agility in everyday tasks.
- Adjust group sizes based on children’s motor skill levels and comorbidities, ensuring that children with more complex needs receive adequate support. In those cases, smaller groups may be necessary for effective intervention [4].
- Incorporate activities that promote skill transfer to real-life contexts, helping children apply learned motor skills to daily functional tasks.
- Recognize the cognitive benefits of motor training, as it can enhance attention, visual perception, and other cognitive functions alongside physical skill development [66].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Haga, M. The relationship between physical fitness and motor competence in children. Child Care Health Dev. 2008, 34, 329–334. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; View Article; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar]
- Blank, R.; Barnett, A.L.; Cairney, J.; Green, D.; Kirby, A.; Polatajko, H.; Rosenblum, S.; Smits-Engelsman, B.; Sugden, D.; Wilson, P.; et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev. Med. Child Neurol. 2019, 61, 242–285. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Ferguson, G.; Jelsma, J.; Versfeld, P.; Smits-Engelsman, B. Using the ICF framework to explore the multiple interacting factors associated with developmental coordination disorder. Curr. Dev. Disord. Rep. 2014, 1, 86–101. [Google Scholar] [CrossRef]
- Steenbergen, B.; Valtr, L.; Dunford, C.; Prunty, M.; Bekhuis, H.; Temlali, T.Y.; van Abswoude, F.; Lust, J.M.; Warlop, G.; Augustijn, M.; et al. Awareness about developmental coordination disorder. Front. Public Health 2024, 12, 1345257. [Google Scholar] [CrossRef] [PubMed]
- Schott, N.; Alof, V.; Hultsch, D.; Meermann, D. Physical fitness in children with developmental coordination disorder. Res. Q. Exerc. Sport 2007, 78, 438–450. [Google Scholar] [CrossRef]
- Ferguson, G.D.; Aertssen, W.F.; Rameckers, E.A.; Jelsma, J.; Smits-Engelsman, B.C. Physical fitness in children with developmental coordination disorder: Measurement matters. Res. Dev. Disabil. 2014, 35, 1087–1097. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, J.G.; Harris, S.; Klassen, A. Quality of life domains affected in children with developmental coordination disorder: A systematic review. Child Care Health Dev. 2013, 39, 562–580. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.H.; Smits-Engelsman, B.; Caeyenberghs, K.; Steenbergen, B.; Sugden, D.; Clark, J.; Mumford, N.; Blank, R. Cognitive and neuroimaging findings in developmental coordination disorder: New insights from a systematic review of recent research. Dev. Med. Child Neurol. 2017, 59, 1117–1129. [Google Scholar] [CrossRef] [PubMed]
- Rivilis, I.; Hay, J.; Cairney, J.; Klentrou, P.; Liu, J.; Faught, B.E. Physical activity and fitness in children with developmental coordination disorder: A systematic review. Res. Dev. Disabil. 2011, 32, 894–910. [Google Scholar] [CrossRef]
- Reynolds, J.E.; Alvares, G.A.; Williams, J.; Froude, E.; Elliott, C.; McIntyre, S.; Whitehouse, A.J.; Evans, K.L.; Reid, S.L.; Cairney, J.; et al. Investigating the impact of developmental coordination difficulties across home, school, and community settings: Findings from the Australian Impact for DCD survey. Res. Dev. Disabil. 2024, 147, 104712. [Google Scholar] [CrossRef] [PubMed]
- King-Dowling, S.; Rodriguez, C.; Missiuna, C.; Timmons, B.W.; Cairney, J. Health-related Fitness in Preschool Children with and without Motor Delays. Med. Sci. Sports Exerc. 2018, 50, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Cairney, J.; Veldhuizen, S. Is developmental coordination disorder a fundamental cause of inactivity and poor health-related fitness in children? Dev. Med. Child Neurol. 2013, 55, 55–58. [Google Scholar] [CrossRef]
- Brellenthin, A.G.; Lee, D.-C. Physical activity and the development of substance use disorders: Current knowledge and future directions. Prog. Prev. Med. 2018, 3, e0018. [Google Scholar] [CrossRef] [PubMed]
- Sujatha, B.; Somasundaram, S.; Alagesan, J.; Vikram Adhitya, P.S. Developmental coordination disorder in school children—A systematic review. Biomedicine 2022, 42, 1156–1161. [Google Scholar]
- Cairney, J.; Veldhuizen, S.; King-Dowling, S.; Faught, B.E.; Hay, J. Tracking cardiorespiratory fitness and physical activity in children with and without motor coordination problems. J. Sci. Med. Sport 2017, 20, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Tsiotra, G.D.; Nevill, A.M.; Lane, A.M.; Koutedakis, Y. Physical fitness and developmental coordination disorder in Greek children. Pediatr. Exerc. Sci. 2009, 21, 186–195. [Google Scholar] [CrossRef]
- De Meester, A.; Stodden, D.; Goodway, J.; True, L.; Brian, A.; Ferkel, R.; Haerens, L. Identifying a motor proficiency barrier for meeting physical activity guidelines in children. J. Sci. Med. Sport 2018, 21, 58–62. [Google Scholar] [CrossRef]
- Izadi-Najafabadi, S.; Ryan, N.; Ghafooripoor, G.; Gill, K.; Zwicker, J.G. Participation of children with developmental coordination disorder. Res. Dev. Disabil. 2019, 84, 75–84. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Verbecque, E. Pediatric care for children with developmental coordination disorder, can we do better? Biomed. J. 2022, 45, 250–264. [Google Scholar] [CrossRef] [PubMed]
- Adams, I.L.; Lust, J.M.; Wilson, P.H.; Steenbergen, B. Compromised motor control in children with DCD: A deficit in the internal model?—A systematic review. Neurosci. Biobehav. Rev. 2014, 47, 225–244. [Google Scholar] [CrossRef] [PubMed]
- Biotteau, M.; Chaix, Y.; Albaret, J.-M. What do we really know about motor learning in children with developmental coordination disorder? Curr. Dev. Disord. Rep. 2016, 3, 152–160. [Google Scholar] [CrossRef]
- McQuillan, V.A.; Swanwick, R.A.; Chambers, M.E.; Schlüter, D.K.; Sugden, D.A. A comparison of characteristics, developmental disorders and motor progression between children with and without developmental coordination disorder. Hum. Mov. Sci. 2021, 78, 102823. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Jelsma, D.; Coetzee, D. Do We Drop the Ball When We Measure Ball Skills Using Standardized Motor Performance Tests? Children 2022, 9, 367. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, R.A.; Lee, T.D.; Winstein, C.; Wulf, G.; Zelaznik, H.N. Motor Control and Learning: A Behavioral Emphasis: Human Kinetics; Human Kinetics: Champaign, IL, USA, 2018. [Google Scholar]
- Christensen, D.L. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill. Summ. 2016, 65, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Bonney, E.; Jelsma, L.D.; Ferguson, G.D.; Smits-Engelsman, B.C. Learning better by repetition or variation? Is transfer at odds with task specific training? PLoS ONE 2017, 12, e0174214. [Google Scholar] [CrossRef] [PubMed]
- Geuze, R.H. Static balance and developmental coordination disorder. Hum. Mov. Sci. 2003, 22, 527–548. [Google Scholar] [CrossRef] [PubMed]
- Smits-Engelsman, B.; Vincon, S.; Blank, R.; Quadrado, V.H.; Polatajko, H.; Wilson, P.H. Evaluating the evidence for motor-based interventions in developmental coordination disorder: A systematic review and meta-analysis. Res. Dev. Disabil. 2018, 74, 72–102. [Google Scholar] [CrossRef]
- Button, C.; Seifert, L.; Chow, J.Y.; Araújo, D.; Davids, K. Dynamics of Skill Acquisition: An Ecological Dynamics Approach; Human Kinetics Publishers: Champaign, IL, USA, 2021. [Google Scholar]
- Zhu, Y.; Xu, C.; Wan, Q.; Guo, L.; Sean, X.C. Effects of adapted physical exercise intervention on visual working memory in children with autism spectrum disorder. China Sport Sci. Technol. 2017, 53, 55–62. [Google Scholar]
- Policastro, F.; Accardo, A.; Marcovich, R.; Pelamatti, G.; Zoia, S. Correlations between motor and cognitive skills in young basketball players: A bivariate regression analysis. Phys. Med. Rehabil. Res. 2019, 4, 1–6. [Google Scholar] [CrossRef]
- Ke, L.; Lanlan, Z.; Jian, Z.; Jianing, W. Protocol: Comparison of open-skill and closed-skill exercises in improving the response inhibitory ability of the elderly: A protocol for a randomised controlled clinical trial. BMJ Open 2021, 11, e051966. [Google Scholar] [CrossRef] [PubMed]
- Ángel Latorre-Román, P.; Berrios-Aguayo, B.; Aragón-Vela, J.; Pantoja-Vallejo, A. Effects of a 10-week active recess program in school setting on physical fitness, school aptitudes, creativity and cognitive flexibility in elementary school children. A randomised-controlled trial. J. Sports Sci. 2021, 39, 1277–1286. [Google Scholar] [CrossRef]
- Rösch, D.; Schultz, F.; Höner, O. Decision-making skills in youth basketball players: Diagnostic and external validation of a video-based assessment. Int. J. Environ. Res. Public Health 2021, 18, 2331. [Google Scholar] [CrossRef] [PubMed]
- Zolghadr, H.; Sedaghati, P.; Daneshmandi, H.; Sokhangoe, Y. Effects of mini-basketball training on improving the motor coordination of children with intellectual disabilities and developmental coordination disorders: A randomizedcontrolled trial. BMC Sports Sci. Med. Rehabil. 2024, 16, 250. [Google Scholar] [CrossRef] [PubMed]
- Cairney, J.; Hay, J.; Faught, B.; Mandigo, J.; Flouris, A. Developmental coordination disorder, self-efficacy toward physical activity, and play: Does gender matter? Adapt. Phys. Act. Q. 2005, 22, 67–82. [Google Scholar] [CrossRef]
- Bart, O.; Jarus, T.; Erez, Y.; Rosenberg, L. How do young children with DCD participate and enjoy daily activities? Res. Dev. Disabil. 2011, 32, 1317–1322. [Google Scholar] [CrossRef] [PubMed]
- Adams, I.L.; Broekkamp, W.; Wilson, P.H.; Imms, C.; Overvelde, A.; Steenbergen, B. Role of pediatric physical therapists in promoting sports participation in developmental coordination disorder. Pediatr. Phys. Ther. 2018, 30, 106–111. [Google Scholar] [CrossRef]
- Lucas, B.R.; Elliott, E.J.; Coggan, S.; Pinto, R.Z.; Jirikowic, T.; McCoy, S.W.; Latimer, J. Interventions to improve gross motor performance in children with neurodevelopmental disorders: A meta-analysis. BMC Pediatr. 2016, 16, 193. [Google Scholar] [CrossRef] [PubMed]
- van der Linde, B.W.; van Netten, J.J.; Otten, B.E.; Postema, K.; Geuze, R.H.; Schoemaker, M.M. Psychometric properties of the DCDDaily-Q: A new parental questionnaire on children’s performance in activities of daily living. Res. Dev. Disabil. 2014, 35, 1711–1719. [Google Scholar] [CrossRef]
- Cavalcante-Neto, J.L.; Jelsma, D.; Draghi, T.T.G.; Tudella, E.; Smits-Engelsman, B. Active Video Games Performance and Heart Rate on the Wii or Kinect in Children with and without Developmental Coordination Disorder. Children 2022, 9, 1823. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.E.; Sugden, D.; Barnett, A.L. Movement assessment battery for children-2. Res. Dev. Disabil. 2007, 28, 361–373. [Google Scholar]
- Smits-Engelsman, B.; Schoemaker, M.; Delabastita, T.; Hoskens, J.; Geuze, R. Diagnostic criteria for DCD: Past and future. Hum. Mov. Sci. 2015, 42, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Doe-Asinyo, R.X.; Smits-Engelsman, B.C. Ecological validity of the PERF-FIT: Correlates of active play, motor performance and motor skill-related physical fitness. Heliyon 2021, 7, e07901. [Google Scholar] [CrossRef] [PubMed]
- Smits-Engelsman, B.; Smit, E.; Doe-Asinyo, R.X.; Lawerteh, S.E.; Aertssen, W.; Ferguson, G.; Jelsma, D.L. Inter-rater reliability and test-retest reliability of the Performance and Fitness (PERF-FIT) test battery for children: A test for motor skill related fitness. BMC Pediatr. 2021, 21, 119. [Google Scholar] [CrossRef] [PubMed]
- Jane, J.Y.; Burnett, A.F.; Sit, C.H. Motor skill interventions in children with developmental coordination disorder: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2018, 99, 2076–2099. [Google Scholar]
- Wuang, Y.P.; Su, J.H.; Su, C.Y. Reliability and responsiveness of the Movement Assessment Battery for Children–Second Edition Test in children with developmental coordination disorder. Dev. Med. Child Neurol. 2012, 54, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, J.G.; Lee, E.J. Early intervention for children with/at risk of developmental coordination disorder: A scoping review. Dev. Med. Child Neurol. 2021, 63, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Hulteen, R.M.; Morgan, P.J.; Barnett, L.M.; Stodden, D.F.; Lubans, D.R. Development of foundational movement skills: A conceptual model for physical activity across the lifespan. Sports Med. 2018, 48, 1533–1540. [Google Scholar] [CrossRef]
- Werner, P.H.; Williams, L.H.; Hall, T.J. Teaching Children Gymnastics: Human Kinetics; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Bonney, E.; Ferguson, G.; Smits-Engelsman, B. The efficacy of two activity-based interventions in adolescents with developmental coordination disorder. Res. Dev. Disabil. 2017, 71, 223–236. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, G.; Jelsma, D.; Jelsma, J.; Smits-Engelsman, B. The efficacy of two task-orientated interventions for children with Developmental Coordination Disorder: Neuromotor Task Training and Nintendo Wii Fit training. Res. Dev. Disabil. 2013, 34, 2449–2461. [Google Scholar] [PubMed]
- Hung, W.W.; Pang, M.Y. Effects of group-based versus individual-based exercise training on motor performance in children with developmental coordination disorder: A randomized controlled study. J. Rehabil. Med. 2010, 42, 122–128. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, I.S.; da Silva Oliveira, D.; de Azevedo Guendler, J.; Rocha, B.M.; Sarinho, S.W. Effectiveness of motor intervention on children with Developmental Coordination Disorder (DCD): A systematic review. J. Phys. Educ. Sport Manag. 2017, 8, 32–40. [Google Scholar]
- Thornton, A.; Licari, M.; Reid, S.; Armstrong, J.; Fallows, R.; Elliott, C. Cognitive orientation to (daily) occupational performance intervention leads to improvements in impairments, activity and participation in children with Developmental Coordination Disorder. Disabil. Rehabil. 2016, 38, 979–986. [Google Scholar] [CrossRef]
- Caçola, P.; Romero, M.; Ibana, M.; Chuang, J. Effects of two distinct group motor skill interventions in psychological and motor skills of children with developmental coordination disorder: A pilot study. Disabil. Health J. 2016, 9, 172–178. [Google Scholar] [CrossRef]
- Zwicker, J.G.; Missiuna, C.; Harris, S.R.; Boyd, L.A. Developmental coordination disorder: A review and update. Eur. J. Paediatr. Neurol. 2012, 16, 573–581. [Google Scholar] [CrossRef]
- Rameckers, E.A.; Crafford, R.; Ferguson, G.; Smits Engelsman, B.C. Efficacy of a Task-Oriented Intervention for Children with a Dual Diagnosis of Specific Learning Disabilities and Developmental Coordination Disorder: A Pilot Study. Children 2023, 10, 415. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.-L.; Wilson, P.H.; Wu, S.K. Role of visual–perceptual skills (non-motor) in children with developmental coordination disorder. Hum. Mov. Sci. 2008, 27, 649–664. [Google Scholar] [CrossRef] [PubMed]
- Macnab, J.J.; Miller, L.T.; Polatajko, H.J. The search for subtypes of DCD: Is cluster analysis the answer? Hum. Mov. Sci. 2001, 20, 49–72. [Google Scholar] [CrossRef] [PubMed]
- Vaivre-Douret, L.; Lalanne, C.; Ingster-Moati, I.; Boddaert, N.; Cabrol, D.; Dufier, J.-L.; Golse, B.; Falissard, B. Subtypes of developmental coordination disorder: Research on their nature and etiology. Dev. Neuropsychol. 2011, 36, 614–643. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, A.; Khodaverdi, Z.; Zamani, M.H. Effect of Wii Fit training on visual perception and executive function in boys with developmental coordination disorders: A randomized controlled trial. Res. Dev. Disabil. 2022, 124, 104196. [Google Scholar] [CrossRef] [PubMed]
- Jelsma, D.; Targino Gomes Draghi, T.; Cavalcante Neto, J.; Smits-Engelsman, B. Improved attentional abilities after playing five weeks of active video games in children with and without developmental coordination disorder. Appl. Neuropsychol. Child 2023, 13, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Hammond, J.; Jones, V.; Hill, E.L.; Green, D.; Male, I. An investigation of the impact of regular use of the W ii F it to improve motor and psychosocial outcomes in children with movement difficulties: A pilot study. Child Care Health Dev. 2014, 40, 165–175. [Google Scholar] [CrossRef]
- Diamond, A.; Ling, D.S. Conclusions about interventions, programs, and approaches for improving executive functions that appear justified and those that, despite much hype, do not. Dev. Cogn. Neurosci. 2016, 18, 34–48. [Google Scholar] [CrossRef]
- Amato, A.; Giustino, V.; Patti, A.; Proia, P.; Trivic, T.; Drid, P.; Obradovic, A.; Manojlovic, M.; Mondoni, M.; Paoli, A.; et al. Young basketball players have better manual dexterity performance than sportsmen and non-sportsmen of the same age: A cross-sectional study. Sci. Rep. 2023, 13, 20953. [Google Scholar] [CrossRef]
- Tsai, C.-L.; Wang, C.-H.; Tseng, Y.-T. Effects of exercise intervention on event-related potential and task performance indices of attention networks in children with developmental coordination disorder. Brain Cogn. 2012, 79, 12–22. [Google Scholar] [CrossRef]
- Giagazoglou, P.; Sidiropoulou, M.; Mitsiou, M.; Arabatzi, F.; Kellis, E. Can balance trampoline training promote motor coordination and balance performance in children with developmental coordination disorder? Res. Dev. Disabil. 2015, 36, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, M.; Baig, M.O.; Memon, S.I.; Ashraf, N.; Butt, P.; Afzal, K.; Iqbal, R. Effects of trampoline exercises in children with developmental coordination disorder: A randomized controlled trial. Phys. Med. Rehabil. Kurortmed. 2022, 32, 279–284. [Google Scholar] [CrossRef]
| Skills | Exercises | Materials |
|---|---|---|
| Week 1–2 | ||
| Coordination | Dribbling from standing, sitting down and getting up without losing the ball. | 18 balls |
| Pass and catch | Spiky ball, pass and catch against an elastic net. | 2 groups, 18 balls |
| Reaction speed | Running forward, backward, and sideways upon trainer’s signal. | 3 groups |
| Strength-coordination | American jumping on a ladder, dribbling in slalom, and pass the ball to their partner. | 2 ladders, 12 plastic sticks |
| Shoot | Lineup behind the cone and shooting from different spots and distances. | 6 groups, 6 balls |
| Rule, defense-attack | Reduced game 3 against 3. | 3 mini grounds |
| Cool-down stretches | Active and passive flexibility. | Body only |
| Week 3–4 | ||
| Pass and catch | The child in front passes the ball alternately for 2 partners (moving along line). | 6 groups, 6 balls |
| Shoot-precision | Standing behind a cone, throw a tennis or basketball into a bucket from a 2–3 m distance. | 6 groups, 6 tennis balls, 6 basketballs |
| Pass and catch | Spiky ball, pass and catch against an elastic net at his partner’s chest level. | 2 groups, 18 balls |
| Strength-coordination | Jumping forwards, backward, left and right, sprinting upon trainer’s signal with and without dribbling. | 3 groups |
| Shoot | Line up behind the cone and shoot from different spots and distances. | 6 groups, 6 balls |
| Rule, defense-attack | Reduced game 3 against 3. | 3 mini grounds |
| Cool-down stretches | Active and passive flexibility. | Body only |
| Week 5–6 | ||
| Pass and catch | Throwing a tennis or basketball, walling and catching. | 18 tennis balls, 18 basketballs |
| Coordination | Dribbling in a ladder. | 2 ladders |
| Strength-coordination | Jumping the hurdles without losing the ball. | 12 hurdles, 2 groups |
| Strength | Running forward, touch the cone (color shown), and running backward. | 3 groups, 9 plastic sticks |
| Shoot-precision | Line up behind the cone and shoot from different spots and distances. | 6 groups, 6 balls |
| Rule, defense-attack | Reduced game 3 against 3. | 3 mini grounds |
| Cool-down stretches | Active and passive flexibility | Body only |
| Week 7–8 | ||
| Reaction speed | The teacher throws the ball up, on the rebound the child must catch it before his opponent. | One against one |
| Strength-coordination | Jumping the hurdles, skipping in the hoops with and without dribbling. | 12 hurdles, 12 hoops |
| Coordination | Face to face, dribbling a basketball with one hand, passing a tennis ball with the other hand. | 18 tennis balls, 18 basketballs |
| Coordination | Dribbling, putting the cone in the hoop and returning to starting position. | 18 balls, 6 cones, 6 hoops |
| Shoot-precision | Line up behind the cone and shoot from different spots and distances. | 6 groups, 6 balls |
| Rule, defense-attack | Reduced game 3 against 3. | 3 mini grounds |
| Cool-down stretches | Active and passive flexibility. | Body only |
| DCD Training Group (n = 18) | DCD Non-Training Group (n = 20) | |||||||
|---|---|---|---|---|---|---|---|---|
| Median | Minimum | Maximum | Median | Minimum | Maximum | z-Scores | p-Value | |
| Age (years) | 8.6 | 8 | 8.9 | 8.5 | 8.1 | 9.9 | −0.117 | 0.907 |
| Height (m) | 1.35 | 1.30 | 1.44 | 1.33 | 1.27 | 1.45 | −0.192 | 0.848 |
| Body mass (kg) | 33.50 | 30 | 40 | 31 | 27 | 38 | −2.108 | 0.035 |
| BMI (kg m−2) | 18.45 | 16 | 22 | 17.64 | 15 | 20 | −1.463 | 0.144 |
| z-Value | p-Value | |
|---|---|---|
| MABC-2 | ||
| Total Standard Scores | −5.256 | <0.001 |
| Manual Dexterity (SS) | −4.843 | <0.001 |
| Aiming and Catching (SS) | −4.071 | <0.001 |
| Balance (SS) | −3.029 | <0.01 |
| PERF-FIT | ||
| Jumping (#) | −5.252 | <0.001 |
| Hopping right (#) | −5.324 | <0.001 |
| Hopping left (#) | −5.239 | <0.001 |
| Bouncing and Catching (#) | −5.029 | <0.001 |
| Throwing and Catching (#) | −5.303 | <0.001 |
| Static Balance (s) | −4.825 | <0.001 |
| Dynamic Balance (#) | −4.654 | <0.001 |
| Running (s) | −5.007 | <0.001 |
| Stepping (s) | −5.239 | <0.001 |
| Side Jump (#) | −5.042 | <0.001 |
| Long Jump (cm) | −5.196 | <0.001 |
| Overhand Throw (cm) | −4.876 | <0.001 |
| DCD Training Group (n = 18) | DCD Usual Care Group (n = 20) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median Pre | Median Post | Range Pre | Range Post | z-Score | p-Value | Effect size r | Median Pre | Median Post | Range Pre | Range Post | z-Score | p-Value | |
| MABC-2 | |||||||||||||
| Total Standard Scores | 5 | 8 | 3 | 4 | 3.755 | <0.001 | 0.89 | 4 | 4 | 4 | 4 | 0.816 | 0.414 |
| Manual Dexterity (SS) | 6 | 9 | 3 | 4 | 3.758 | <0.001 | 0.89 | 6 | 6 | 5 | 6 | −1.03 | 0.31 |
| Aiming and Catching (SS) | 6 | 8 | 5 | 4 | 3.647 | <0.001 | 0.86 | 6 | 6 | 6 | 4 | −0.319 | 0.749 |
| Balance (SS) | 6.50 | 8.50 | 4 | 5 | 3.384 | <0.001 | 0.80 | 5 | 6 | 6 | 5 | −0.183 | 0.855 |
| PERF-FIT | |||||||||||||
| Jumping (#) | 15 | 20 | 4 | 7 | 3.744 | <0.001 | 0.88 | 15 | 15 | 3 | 4 | 0.32 | 0.32 |
| Hopping right (#) | 9 | 17 | 3 | 7 | 3.745 | <0.001 | 0.88 | 9 | 9.50 | 4 | 4 | 0.471 | 0.637 |
| Hopping left (#) | 8 | 15 | 2 | 9 | 3.736 | <0.001 | 0.83 | 8.50 | 9 | 3 | 3 | 1.268 | 0.205 |
| Bouncing and Catching (#) | 37.50 | 43 | 4 | 5 | 3.738 | <0.001 | 0.88 | 37 | 38 | 4 | 7 | 0.784 | 0.433 |
| Throwing and Catching (#) | 34.50 | 43.50 | 4 | 8 | 3.742 | <0.001 | 0.88 | 35 | 35 | 6 | 10 | 0.599 | 0.61 |
| Static Balance (s) | 32.20 | 40.75 | 19 | 20 | 3.680 | <0.001 | 0.87 | 33.50 | 32.90 | 10 | 9 | −1.76 | 0.240 |
| Dynamic Balance (#) | 15.50 | 22 | 5 | 10 | 3.524 | <0.001 | 0.83 | 15 | 15 | 7 | 5 | −0.931 | 0.352 |
| Running (s) | 10.05 | 7.55 | 2 | 2 | −3.729 | <0.001 | 0.88 | 10.25 | 10 | 2 | 2 | −0.692 | 0.489 |
| Stepping (s) | 18.20 | 14.55 | 2 | 3 | −3.724 | <0.001 | 0.88 | 18.10 | 18.05 | 2 | 3 | −0.038 | 0.97 |
| Side Jump (#) | 15 | 21 | 3 | 7 | 3.755 | <0.001 | 0.88 | 14.50 | 15 | 4 | 4 | 0.707 | 0.479 |
| Long Jump (cm) | 90 | 125 | 23 | 35 | 3.724 | <0.001 | 0.88 | 89.50 | 95 | 20 | 25 | 1.361 | 0.173 |
| Overhand Throw (cm) | 200.50 | 235 | 22 | 45 | 3.520 | <0.001 | 0.83 | 200 | 200 | 39 | 40 | −1.55 | 0.121 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farhat, F.; Ammar, A.; Mezghani, N.; Kammoun, M.M.; Trabelsi, K.; Gharbi, A.; Sallemi, L.; Rebai, H.; Moalla, W.; Smits-Engelsman, B. The Effect of Task-Oriented Basketball Training on Motor Skill-Related Fitness in Children with Developmental Coordination Disorder. Sports 2025, 13, 62. https://doi.org/10.3390/sports13030062
Farhat F, Ammar A, Mezghani N, Kammoun MM, Trabelsi K, Gharbi A, Sallemi L, Rebai H, Moalla W, Smits-Engelsman B. The Effect of Task-Oriented Basketball Training on Motor Skill-Related Fitness in Children with Developmental Coordination Disorder. Sports. 2025; 13(3):62. https://doi.org/10.3390/sports13030062
Chicago/Turabian StyleFarhat, Faiçal, Achraf Ammar, Nourhen Mezghani, Mohamed Moncef Kammoun, Khaled Trabelsi, Adnene Gharbi, Lassad Sallemi, Haithem Rebai, Wassim Moalla, and Bouwien Smits-Engelsman. 2025. "The Effect of Task-Oriented Basketball Training on Motor Skill-Related Fitness in Children with Developmental Coordination Disorder" Sports 13, no. 3: 62. https://doi.org/10.3390/sports13030062
APA StyleFarhat, F., Ammar, A., Mezghani, N., Kammoun, M. M., Trabelsi, K., Gharbi, A., Sallemi, L., Rebai, H., Moalla, W., & Smits-Engelsman, B. (2025). The Effect of Task-Oriented Basketball Training on Motor Skill-Related Fitness in Children with Developmental Coordination Disorder. Sports, 13(3), 62. https://doi.org/10.3390/sports13030062








