Improved Tribological Performance of Nitride-Reinforced Biocompatible Titanium–Niobium–Zirconium–Tantalum (TNZT) Alloys for Advanced Orthopedic Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Material Synthesis and Characterization
2.2. Biocompatibility Tests of the Alloys
2.2.1. Materials
2.2.2. MG-63 Cell Culture
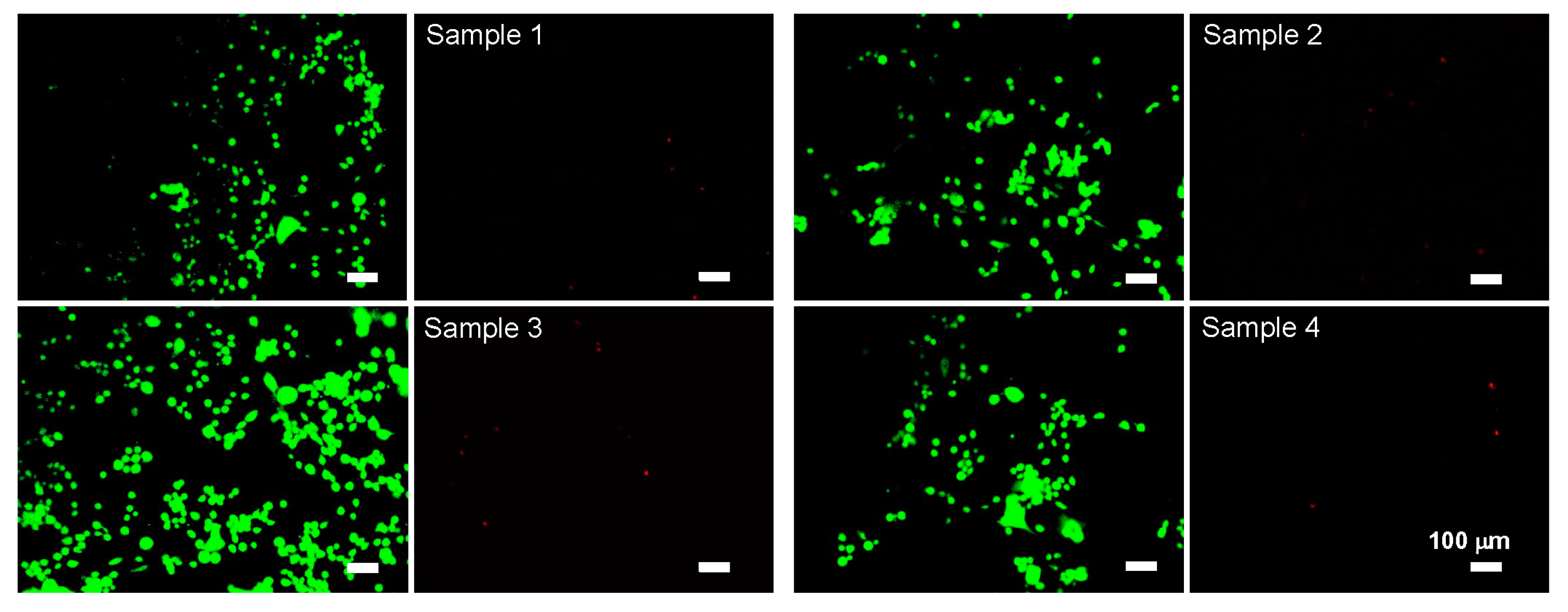
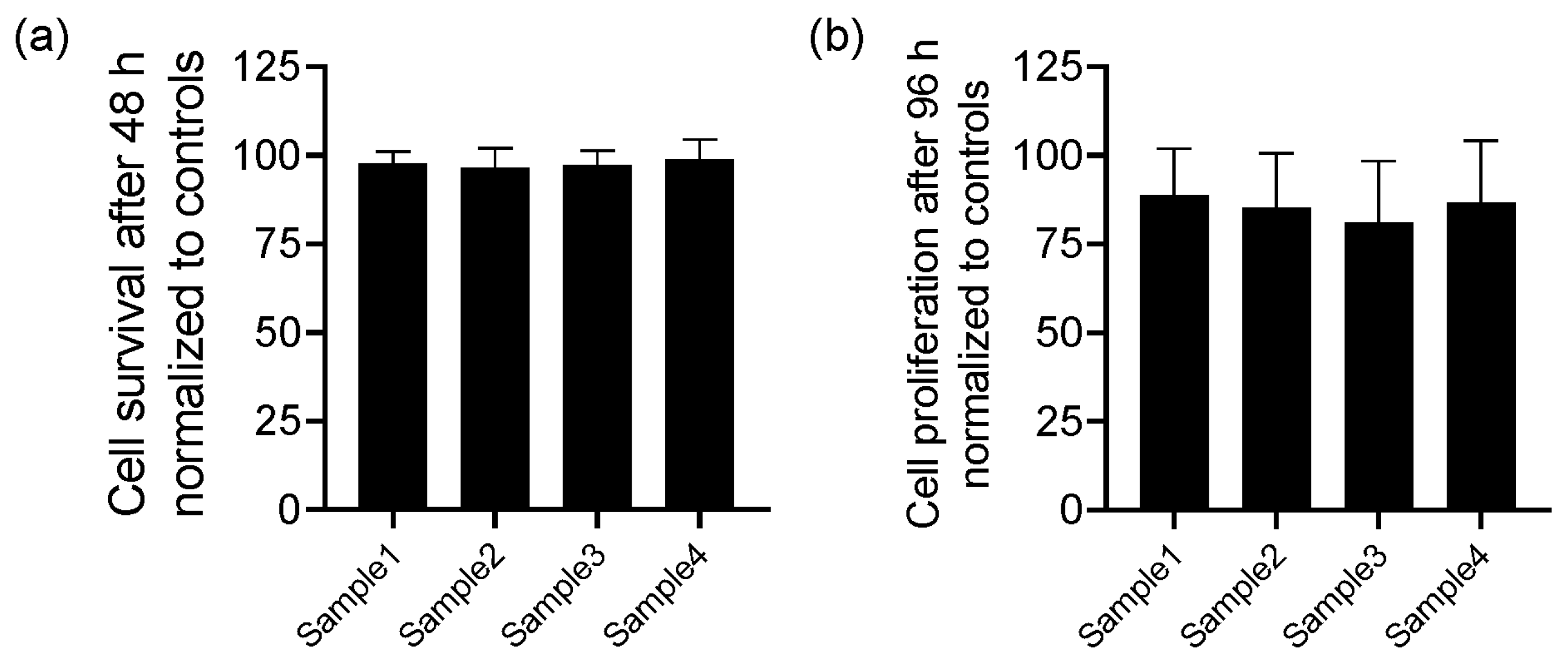
2.2.3. Cell Viability Test
2.2.4. MTT Assay
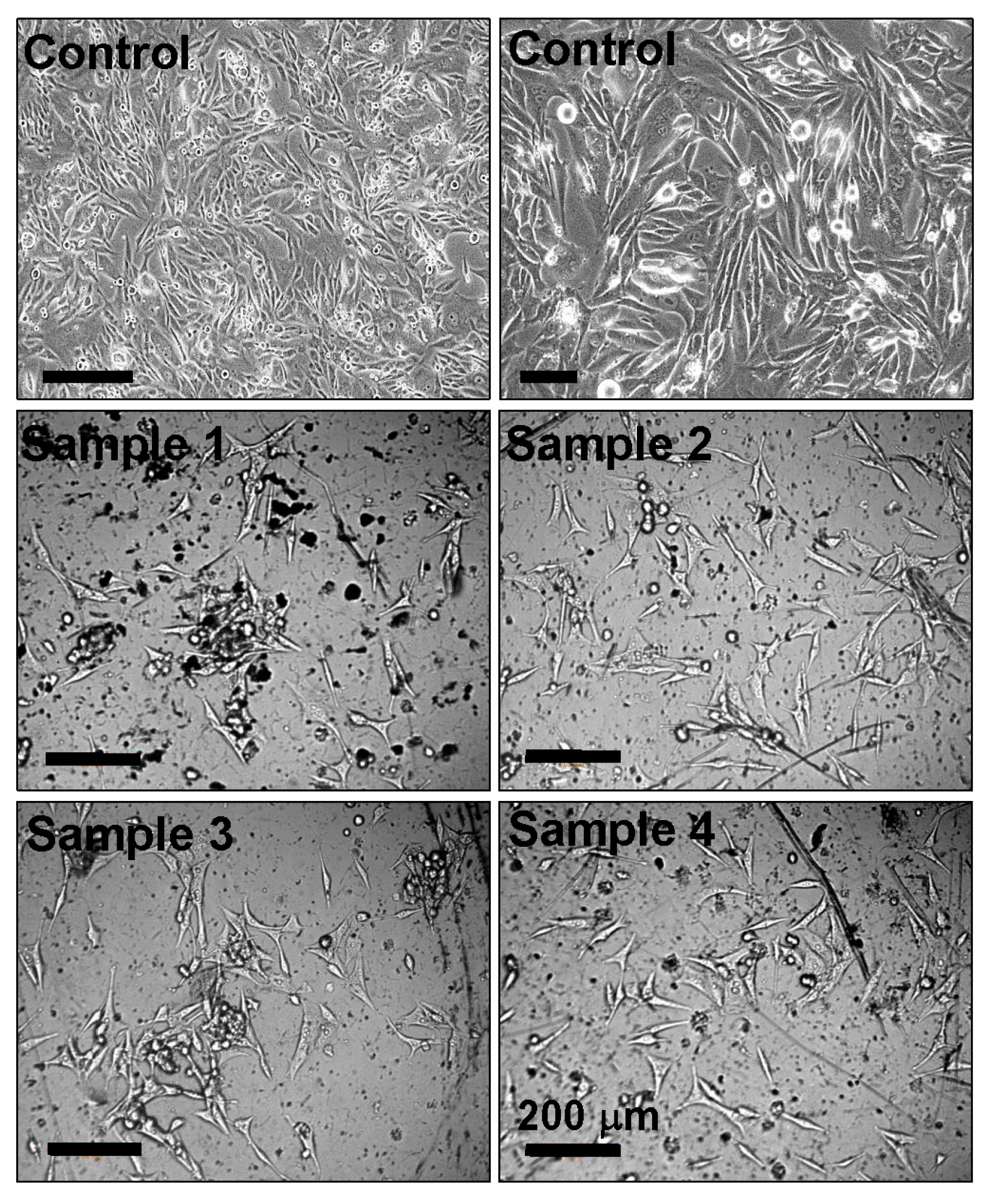
2.2.5. Cell Adhesion
3. Results
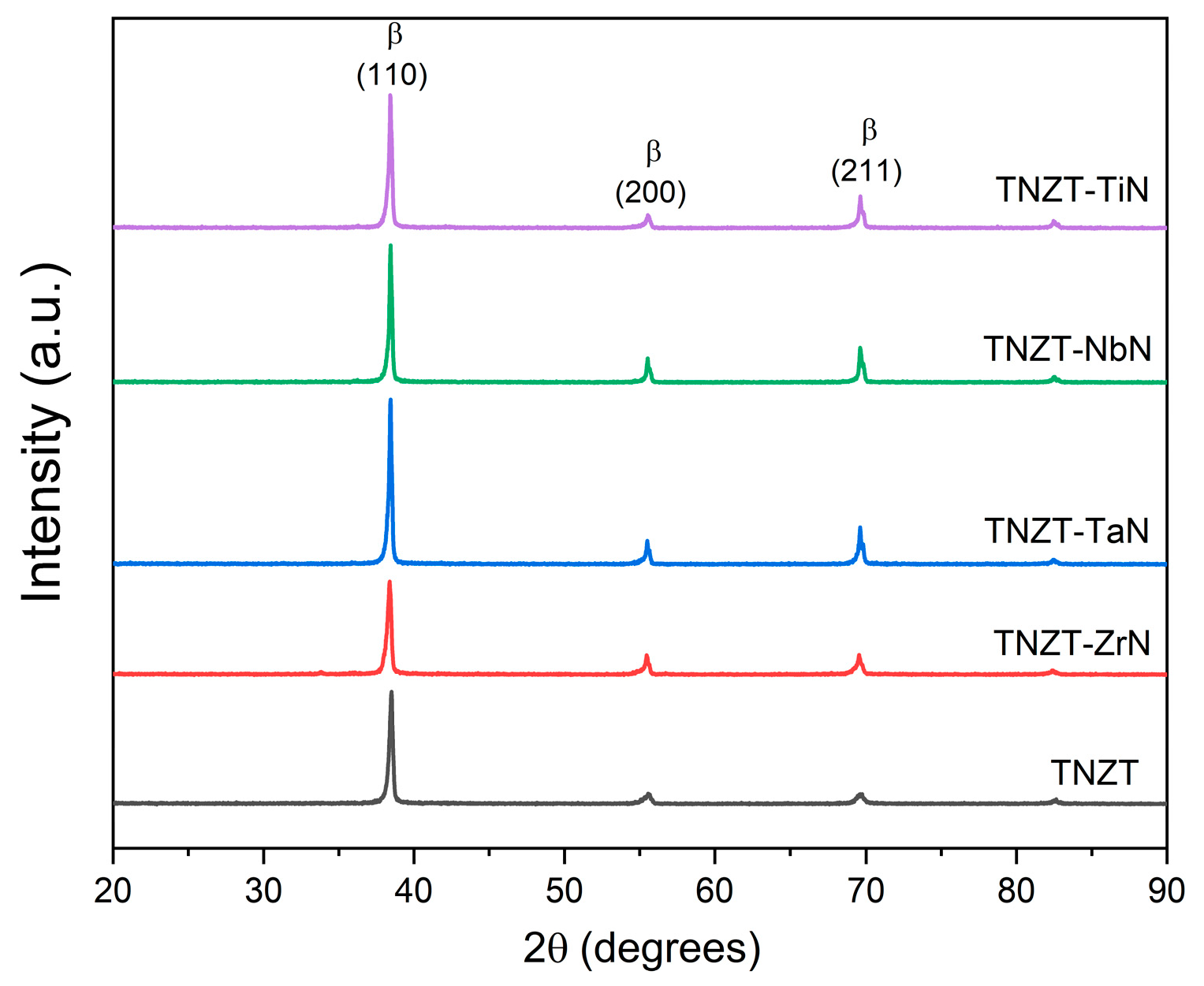
3.1. X-ray Diffraction
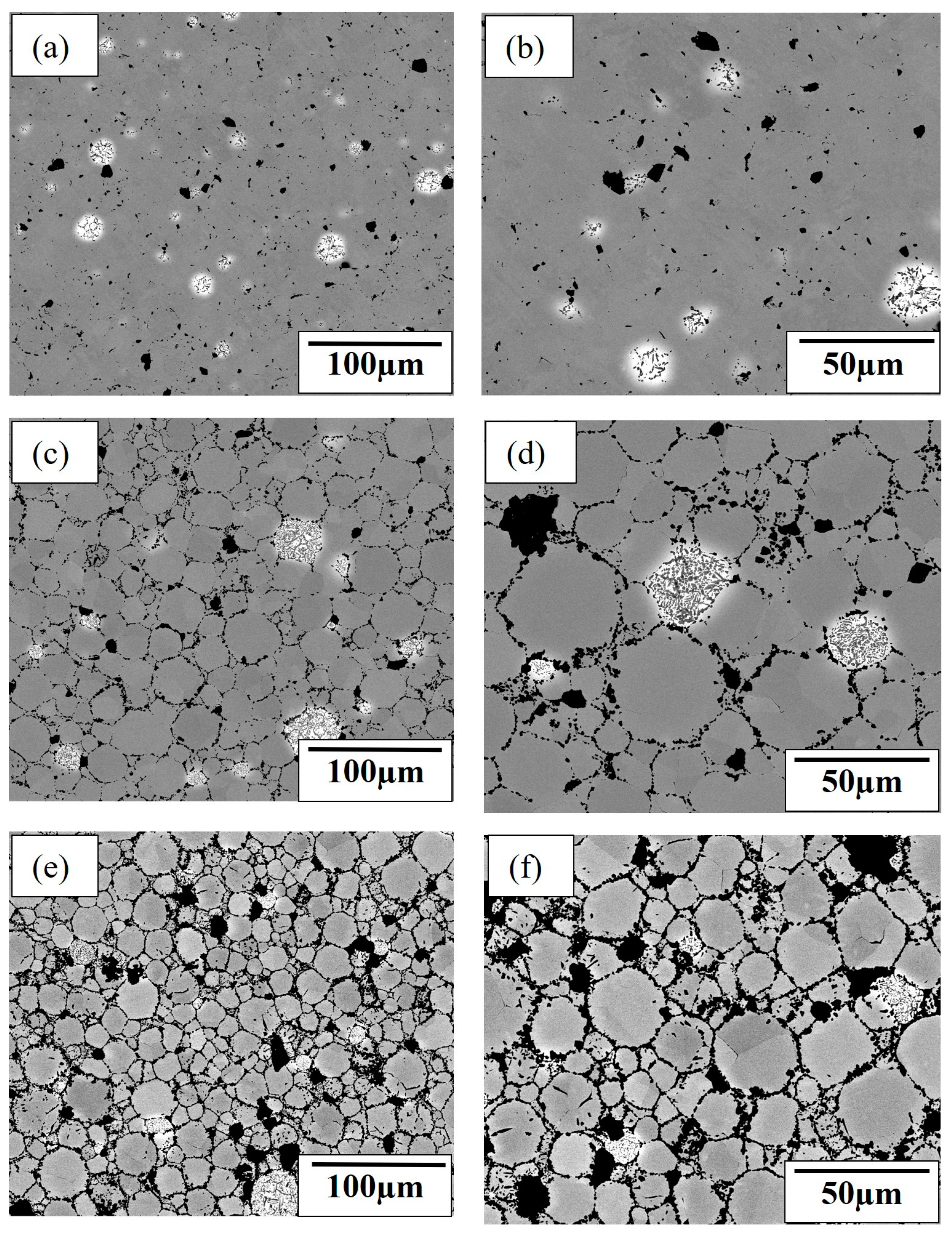
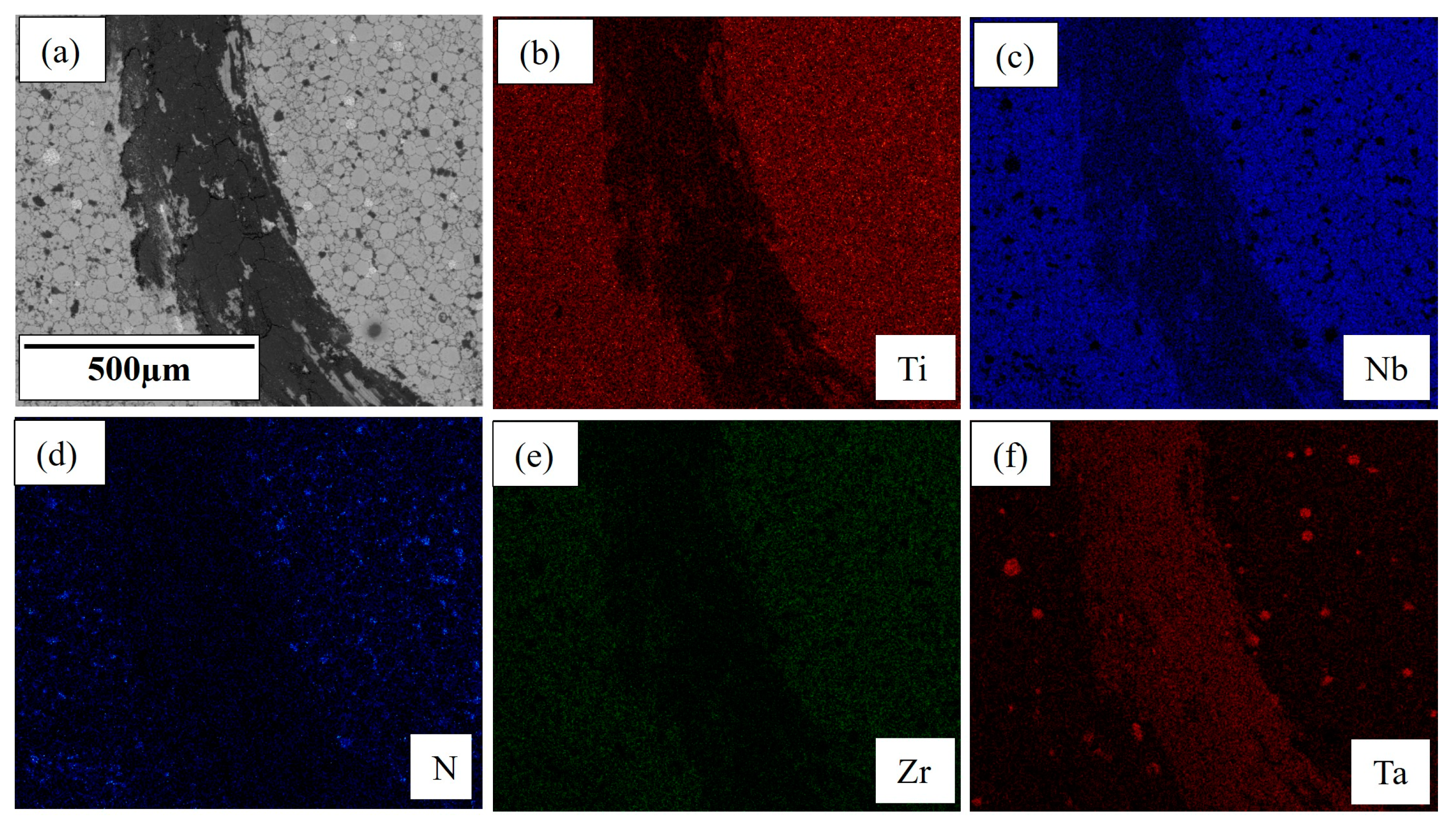
3.2. Scanning Electron Microscopy
3.3. Microhardness
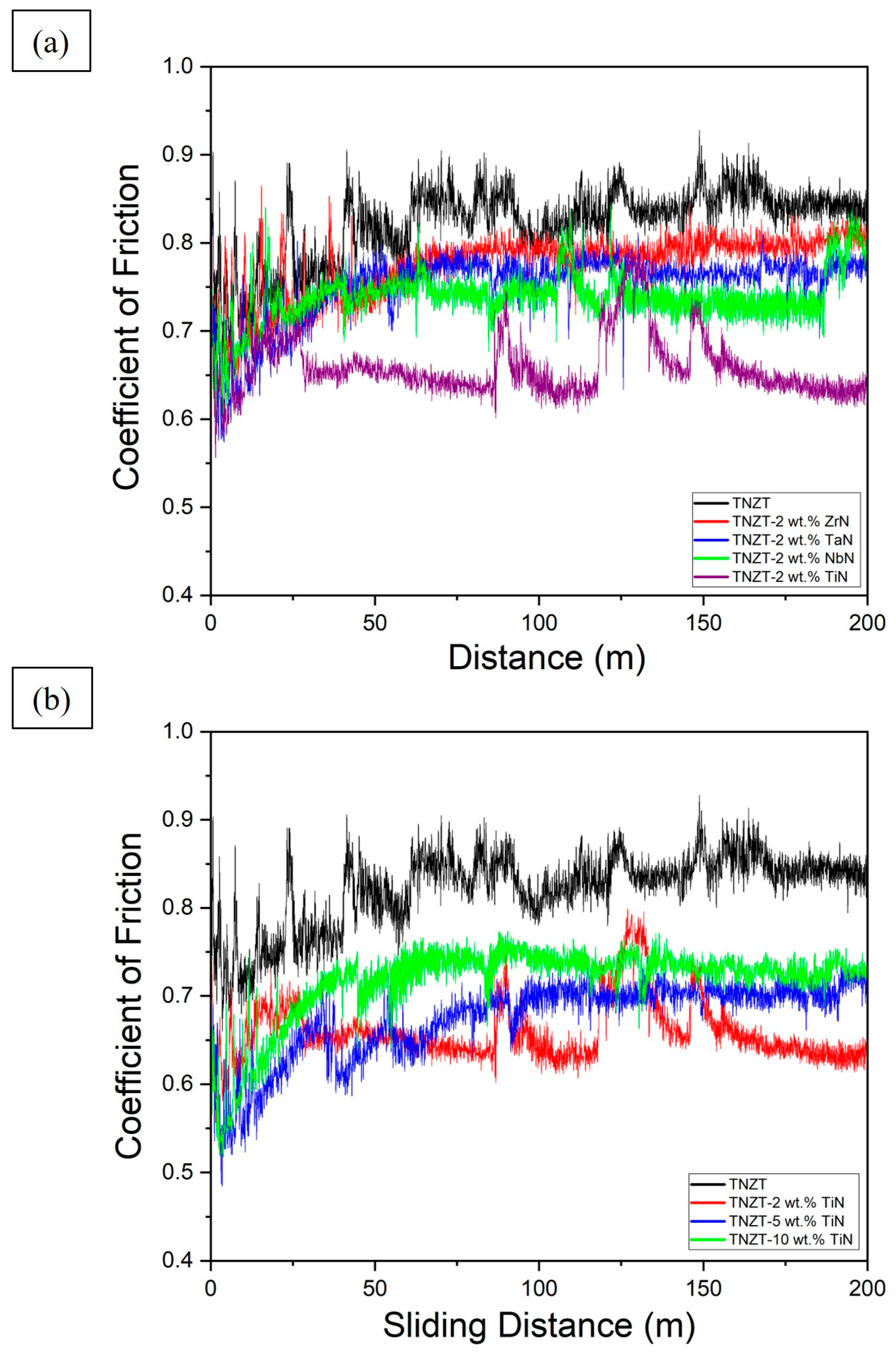
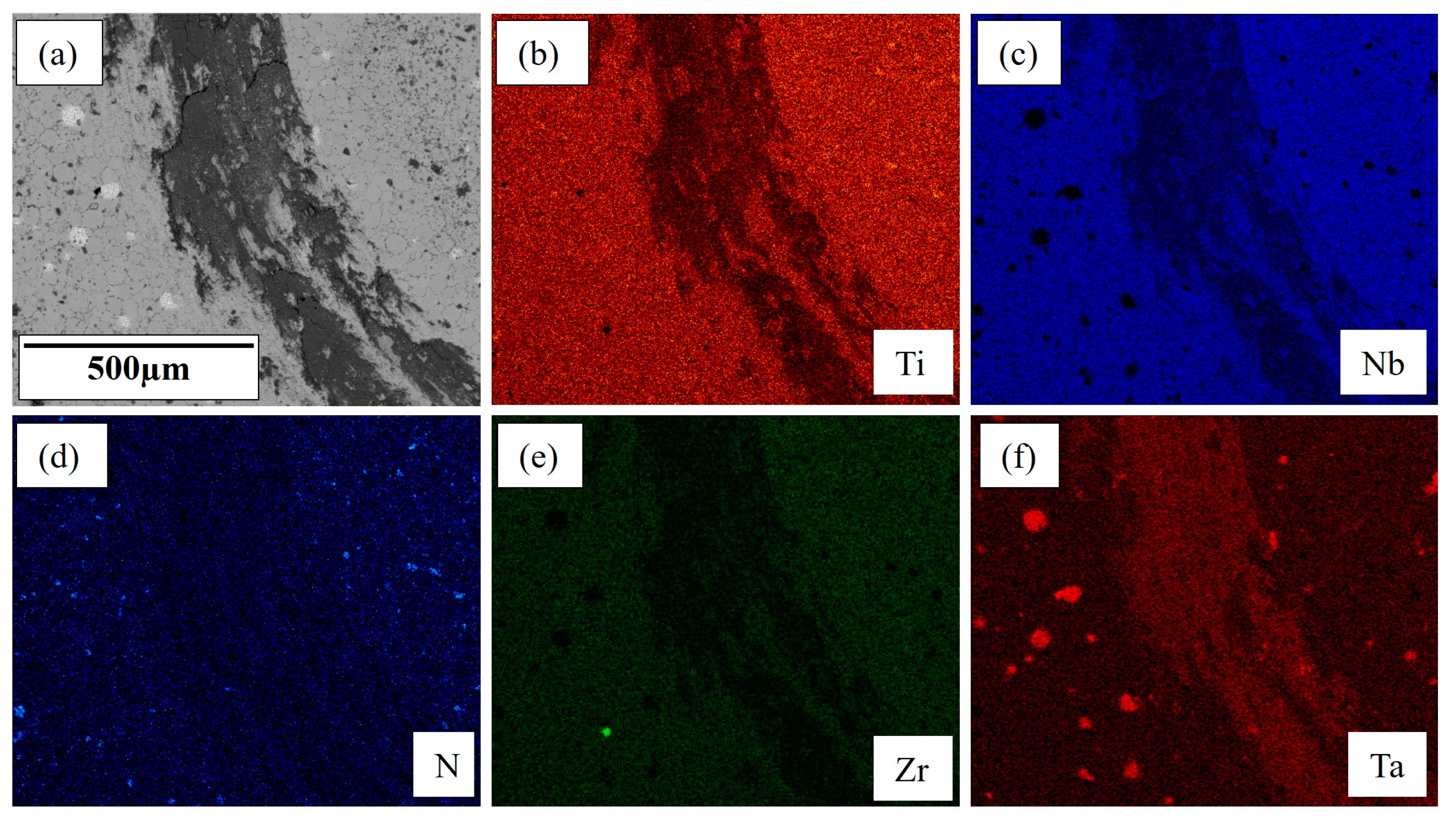
3.4. Wear Behavior
3.5. Cytotoxicity Studies
4. Conclusions
- All nitride-reinforced TNZT composites demonstrated superior tribological performance over pure TNZT alloys while retaining a single-phase BCC structure and excellent biocompatibility. This was attributed to the presence of very hard and strong nitrides in the β-Ti matrix.
- TNZT-2 wt.% TiN exhibited the optimum hardness (311.8 HV) and lowest CoF (0.659), showcasing the highest efficiency of TiN among other nitrides in improving the tribological performance of TNZT alloys.
- TNZT composites with 5 wt.% TiN and 10 wt.% TiN showed a higher hardness (388.5 HV and 444.3 HV, respectively) but also showed a higher CoF (0.674 and 0.715, respectively). This was attributed to the higher but nonuniform presence of TiN.
- This work will aid in producing superior β-Ti alloys for advanced orthopedic applications.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Scholz, M.S.; Blanchfield, J.P.; Bloom, L.D.; Coburn, B.H.; Elkington, M.; Fuller, J.D.; Bond, I.P. The use of composite materials in modern orthopedic medicine and prosthetic devices: A review. Compos. Sci. Technol. 2011, 71, 1791–1803. [Google Scholar] [CrossRef]
- Filip, N.; Radu, I.; Veliceasa, B.; Filip, C.; Pertea, M.; Clim, A.; Pinzariu, A.C.; Drochioi, L.C.; Hilitanu, R.L.; Serban, I.L. Biomaterials in Orthopedic Devices: Current Issues and Future Perspectives. Coatings 2022, 12, 1544. [Google Scholar] [CrossRef]
- Intravaia, J.T.; Graham, T.; Kim, H.S.; Nanda, H.S.; Kumbar, S.G.; Nukavarapu, S.P. Smart orthopedic biomaterials and implants. Curr. Opin. Biomed. Eng. 2023, 25, 100439. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.R.; Kwon, J.W.; Suk, K.S.; Kim, H.S.; Moon, S.H.; Park, S.Y.; Lee, B.H. The Clinical Use of Osteobiologic and Metallic Biomaterials in Orthopedic Surgery: The Present and the Future. Materials 2023, 16, 3633. [Google Scholar] [CrossRef]
- Liang, W.; Zhou, C.; Zhang, H.; Bai, J.; Jiang, B.; Jiang, C.; Ming, W.; Zhang, H.; Long, H.; Huang, X.; et al. Recent advances in 3D printing of biodegradable metals for orthopaedic applications. J. Biol. Eng. 2023, 17, 56. [Google Scholar] [CrossRef] [PubMed]
- Affatato, S.; Ruggiero, A.; Merola, M. Advanced biomaterials in hip joint arthroplasty. A review on polymer and ceramics composites as alternative bearings. Compos. B Eng. 2015, 83, 276–283. [Google Scholar] [CrossRef]
- Niinomi, M.; Nakai, M.; Hieda, J. Development of new metallic alloys for biomedical applications. Acta Biomater. 2012, 8, 3888–3903. [Google Scholar] [CrossRef] [PubMed]
- Prakasam, M.; Locs, J.; Salma-Ancane, K.; Loca, D.; Largeteau, A.; Berzina-Cimdina, L. Biodegradable materials and metallic implants—A review. J. Funct. Biomater. 2017, 8, 44. [Google Scholar] [CrossRef]
- Kulkarni, M.; Mazare, A.; Gongadze, E.; Perutkova, Š.; Kralj-Iglič, V.; Milošev, I.; Schmuki, P.; Iglič, A.; Mozetič, M. Titanium nanostructures for biomedical applications. Nanotechnology 2015, 26, 062002. [Google Scholar] [CrossRef]
- Minagar, S.; Berndt, C.C.; Wang, J.; Ivanova, E.; Wen, C. A review of the application of anodization for the fabrication of nanotubes on metal implant surfaces. Acta Biomater. 2012, 8, 2875–2888. [Google Scholar] [CrossRef]
- Amaravathy, P.; Sowndarya, S.; Sathyanarayanan, S.; Rajendran, N. Novel sol gel coating of Nb2O5 on magnesium alloy for biomedical applications. Surf. Coat. Technol. 2014, 244, 131–141. [Google Scholar] [CrossRef]
- Mazur, M.; Kalisz, M.; Wojcieszak, D.; Grobelny, M.; Mazur, P.; Kaczmarek, D.; Domaradzki, J. Determination of structural, mechanical and corrosion properties of Nb2O5 and (NbyCu1−y) Ox thin films deposited on Ti6Al4V alloy substrates for dental implant applications. Mater. Sci. Eng. C 2015, 47, 211–221. [Google Scholar] [CrossRef]
- Li, Q.; Liu, T.; Li, J.; Cheng, C.; Niinomi, M.; Yamanaka, K.; Chiba, A.; Nakano, T. Microstructure, mechanical properties, and cytotoxicity of low Young’s modulus Ti–Nb–Fe–Sn alloys. J. Mater. Sci. 2022, 57, 5634–5644. [Google Scholar] [CrossRef]
- Bahl, S.; Suwas, S.; Chatterjee, K. Comprehensive review on alloy design, processing, and performance of β Titanium alloys as biomedical materials. Int. Mater. Rev. 2021, 66, 114–139. [Google Scholar] [CrossRef]
- Song, X.; Wang, L.; Niinomi, M.; Nakai, M.; Liu, Y. Fatigue characteristics of a biomedical β-type titanium alloy with titanium boride. Mater. Sci. Eng. A 2015, 640, 154–164. [Google Scholar] [CrossRef]
- Chirico, C.; Romero, A.V.; Gordo, E.; Tsipas, S.A. Improvement of wear resistance of low-cost powder metallurgy β-titanium alloys for biomedical applications. Surf. Coat. Technol. 2022, 434, 128207. [Google Scholar] [CrossRef]
- Biesiekierski, A.; Ping, D.; Li, Y.; Lin, J.; Munir, K.S.; Yamabe-Mitarai, Y.; Wen, C. Extraordinary high strength Ti-Zr-Ta alloys through nanoscaled, dual-cubic spinodal reinforcement. Acta Biomater. 2017, 53, 549–558. [Google Scholar] [CrossRef]
- Maity, T.; Balcı, Ö.; Gammer, C.; Ivanov, E.; Eckert, J.; Prashanth, K.G. High pressure torsion induced lowering of Young’s modulus in high strength TNZT alloy for bio-implant applications. J. Mech. Behav. Biomed. Mater. 2020, 108, 103839. [Google Scholar] [CrossRef]
- Liu, J.; Chang, L.; Liu, H.; Li, Y.; Yang, H.; Ruan, J. Microstructure, mechanical behavior and biocompatibility of powder metallurgy Nb-Ti-Ta alloys as biomedical material. Mater. Sci. Eng. C 2017, 71, 512–519. [Google Scholar] [CrossRef]
- Morais, L.S.; Serra, G.G.; Muller, C.A.; Andrade, L.R.; Palermo, E.F.; Elias, C.N.; Meyers, M. Titanium alloy mini-implants for orthodontic anchorage: Immediate loading and metal ion release. Acta Biomater. 2007, 3, 331–339. [Google Scholar] [CrossRef]
- Li, H.F.; Huang, J.Y.; Lin, G.C.; Wang, P.Y. Recent advances in tribological and wear properties of biomedical metallic materials. Rare Met. 2021, 40, 3091–3106. [Google Scholar] [CrossRef]
- Marin, E.; Lanzutti, A. Biomedical Applications of Titanium Alloys: A Comprehensive Review. Materials 2024, 17, 114. [Google Scholar] [CrossRef]
- Li, C.; Zhan, Y.; Jiang, W. β-Type Ti–Mo–Si ternary alloys designed for biomedical applications. Mater. Des. 2012, 34, 479–482. [Google Scholar] [CrossRef]
- Taddei, E.B.; Henriques, V.A.R.; Silva, C.R.M.; Cairo, C.A.A. Production of new titanium alloy for orthopedic implants. Mater. Sci. Eng. C 2004, 24, 683–687. [Google Scholar] [CrossRef]
- Hager Jr, C.H.; Sanders, J.; Sharma, S.; Voevodin, A. Gross slip fretting wear of CrCN, TiAlN, Ni, and CuNiIn coatings on Ti6Al4V interfaces. Wear 2007, 263, 430–443. [Google Scholar] [CrossRef]
- Gupta, M.K.; Etri, H.E.; Korkmaz, M.E.; Ross, N.S.; Krolczyk, G.M.; Gawlik, J.; Yasar, N.; Pimenov, D.Y. Tribological and surface morphological characteristics of titanium alloys: A review. Arch. Civ. Mech. Eng. 2022, 22, 72. [Google Scholar] [CrossRef]
- Samuel, S.; Nag, S.; Scharf, T.W.; Banerjee, R. Wear resistance of laser-deposited boride reinforced Ti-Nb–Zr–Ta alloy composites for orthopedic implants. Mater. Sci. Eng. C 2008, 28, 414–420. [Google Scholar] [CrossRef]
- Chan, C.W.; Lee, S.; Smith, G.; Sarri, G.; Ng, C.H.; Sharba, A.; Man, H.C. Enhancement of wear and corrosion resistance of beta titanium alloy by laser gas alloying with nitrogen. Appl. Surf. Sci. 2016, 367, 80–90. [Google Scholar] [CrossRef]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Raveh, A.; Hansen, P.L.; Avni, R.; Grill, A. Microstructure and composition of plasma-nitrided Ti-6Al-4V layers. Surf. Coat. Technol. 1989, 38, 339–351. [Google Scholar] [CrossRef]
- Matsuura, K.; Kudoh, M. Surface modification of titanium by a diffusional carbo-nitriding method. Acta Mater. 2002, 50, 2693–2700. [Google Scholar] [CrossRef]
- Sathish, S.; Geetha, M.; Pandey, N.D.; Richard, C.; Asokamani, R. Studies on the corrosion and wear behavior of the laser nitrided biomedical titanium and its alloys. Mater. Sci. Eng. C 2010, 30, 376–382. [Google Scholar] [CrossRef]
- Cui, Z.D.; Zhu, S.L.; Man, H.C.; Yang, X.J. Microstructure and wear performance of gradient Ti/TiN metal matrix composite coating synthesized using a gas nitriding technology. Surf. Coat. Technol. 2005, 190, 309–313. [Google Scholar] [CrossRef]
- Borkar, T.; Nag, S.; Ren, Y.; Tiley, J.; Banerjee, R. Reactive spark plasma sintering (SPS) of nitride reinforced titanium alloy composites. J. Alloys Compd. 2014, 617, 933–945. [Google Scholar] [CrossRef]
- Tjong, S.C.; Ma, Z.Y. Microstructural and mechanical characteristics of in situ metal matrix composites. Mater. Sci. Eng. R Rep. 2000, 29, 49–113. [Google Scholar] [CrossRef]
- Ma, Z.Y.; Ning, X.G.; Lu, Y.X.; Bi, J.; Wen, L.S.; Wu, S.J.; Jangg, G.; Daninger, H. In-situ Al4C3 dispersoid and SiC particle mixture-reinforced aluminium composite. Scr. Met. Mater. 1994, 31, 131–135. [Google Scholar] [CrossRef]
- Attar, H.; Ehtemam-Haghighi, S.; Kent, D.; Dargusch, M.S. Recent developments and opportunities in additive manufacturing of titanium-based matrix composites: A review. Int. J. Mach. Tools Manuf. 2018, 133, 85–102. [Google Scholar] [CrossRef]
- Mohseni, H.; Nandwana, P.; Tsoi, A.; Banerjee, R.; Scharf, T.W. In situ nitrided titanium alloys: Microstructural evolution during solidification and wear. Acta Mater. 2015, 83, 61–74. [Google Scholar] [CrossRef]
- Benjamin, J.S.; Volin, T.E. The mechanism of mechanical alloying. Metall. Trans. 1974, 5, 1929–1934. [Google Scholar] [CrossRef]
- Gilman, P.S.; Benjamin, J.S. Mechanical alloying. Annu. Rev. Mater. Sci. 1983, 13, 279–300. [Google Scholar] [CrossRef]
- Zhou, D.; Qiu, F.; Wang, H.; Jiang, Q. Manufacture of nano-sized particle-reinforced metal matrix composites: A review. Acta Metall. Sin-Engl. 2014, 27, 798–805. [Google Scholar] [CrossRef]
- Mamedov, V. Spark plasma sintering as advanced PM sintering method. Powder Metall. 2002, 45, 322–328. [Google Scholar] [CrossRef]
- Walunj, G.; Desai, J.; Bohara, S.; Contieri, R.; Kothapalli, C.; Ivanov, E.; Borkar, T. Light Weight-Low Modulus Biocompatible Titanium Alloys Processed via Spark Plasma Sintering. J. Alloys Metall. Syst. 2023, 3, 100018. [Google Scholar] [CrossRef]
- Batalha, R.L.; Batalha, R.L.; Pinotti, V.E.; Pinotti, V.E.; Alnoaimy, O.O.S.; Alnoaimy, O.O.S.; Batalha, W.C.; Batalha, W.C.; Gustmann, T.; Gustmann, T.; et al. Microstructure and properties of TiB2-reinforced Ti–35Nb–7Zr–5Ta processed by laser-powder bed fusion. J. Mater. Res. 2022, 37, 259–271. [Google Scholar] [CrossRef]
- Facchini, D. Biomedical nanocrystalline metals and alloys: Structure, properties and applications. In Nanomedicine; Woodhead Publishing: Sawston, UK, 2012; pp. 36–67. [Google Scholar] [CrossRef]
- Li, Y.; Garabedian, N.; Schneider, J.; Greiner, C. Waviness affects friction and abrasive wear. Tribol. Lett. 2023, 71, 64. [Google Scholar] [CrossRef]
- Long, M.; Rack, H.J. Friction and surface behavior of selected titanium alloys during reciprocating-sliding motion. Wear 2001, 249, 157–167. [Google Scholar] [CrossRef]
- Li, Y.; Schreiber, P.; Schneider, J.; Greiner, C. Tribological mechanisms of slurry abrasive wear. Friction 2023, 11, 1079–1093. [Google Scholar] [CrossRef]
- Carreño, G.; Pereira, A.; Ávila-Salas, F.; Marican, A.; Andrade, F.; Roca-Melendres, M.M.; Valdes, O.; Vijayakumar, S.; Schwartz, S., Jr.; Abasolo, I.; et al. Development of “on-demand” thermo-responsive hydrogels for anti-cancer drugs sustained release: Rational design, in silico prediction and in vitro validation in colon cancer models. Mater. Sci. Eng. C 2021, 131, 112483. [Google Scholar] [CrossRef]
- Niinomi, M. Design and development of metallic biomaterials with biological and mechanical biocompatibility. J. Biomed. Mater. Res. A 2019, 107, 944–954. [Google Scholar] [CrossRef]
- Luo, J.P.; Sun, J.F.; Huang, Y.J.; Zhang, J.H.; Zhang, Y.D.; Zhao, D.P.; Yan, M. Low-modulus biomedical Ti–30Nb–5Ta–3Zr additively manufactured by Selective Laser Melting and its biocompatibility. Mater. Sci. Eng. C 2019, 97, 275–284. [Google Scholar] [CrossRef]
- Luo, J.P.; Huang, Y.J.; Xu, J.Y.; Sun, J.F.; Dargusch, M.S.; Hou, C.H.; Ren, L.; Wang, R.Z.; Ebel, T.; Yan, M. Additively manufactured biomedical Ti-Nb-Ta-Zr lattices with tunable Young’s modulus: Mechanical property, biocompatibility, and proteomics analysis. Mater. Sci. Eng. C 2020, 114, 110903. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.C.; Ventura, B.N.; Milián, L.; Escuder, A.V.; Amigó Borrás, V. Study of Electrochemical and Biological Characteristics of As-Cast Ti-Nb-Zr-Ta System Based on Its Microstructure. Metals 2022, 12, 476. [Google Scholar] [CrossRef]
- Luo, X.; Yang, C.; Li, R.Y.; Wang, H.; Lu, H.Z.; Song, T.; Ma, H.W.; Li, D.D.; Gebert, A.; Li, Y.Y. Effect of silicon content on the microstructure evolution, mechanical properties, and biocompatibility of β-type TiNbZrTa alloys fabricated by laser powder bed fusion. Biomater. Adv. 2022, 133, 112625. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Digole, S.; Desai, J.; Christopher, C.; Bohara, S.; Witharamage, C.S.; Kothapalli, C.; Gupta, R.K.; Borkar, T. Improved Tribological Performance of Nitride-Reinforced Biocompatible Titanium–Niobium–Zirconium–Tantalum (TNZT) Alloys for Advanced Orthopedic Applications. Metals 2024, 14, 122. https://doi.org/10.3390/met14010122
Digole S, Desai J, Christopher C, Bohara S, Witharamage CS, Kothapalli C, Gupta RK, Borkar T. Improved Tribological Performance of Nitride-Reinforced Biocompatible Titanium–Niobium–Zirconium–Tantalum (TNZT) Alloys for Advanced Orthopedic Applications. Metals. 2024; 14(1):122. https://doi.org/10.3390/met14010122
Chicago/Turabian StyleDigole, Satyavan, Jay Desai, Calvin Christopher, Smriti Bohara, Chathuranga Sandamal Witharamage, Chandra Kothapalli, Rajeev Kumar Gupta, and Tushar Borkar. 2024. "Improved Tribological Performance of Nitride-Reinforced Biocompatible Titanium–Niobium–Zirconium–Tantalum (TNZT) Alloys for Advanced Orthopedic Applications" Metals 14, no. 1: 122. https://doi.org/10.3390/met14010122
APA StyleDigole, S., Desai, J., Christopher, C., Bohara, S., Witharamage, C. S., Kothapalli, C., Gupta, R. K., & Borkar, T. (2024). Improved Tribological Performance of Nitride-Reinforced Biocompatible Titanium–Niobium–Zirconium–Tantalum (TNZT) Alloys for Advanced Orthopedic Applications. Metals, 14(1), 122. https://doi.org/10.3390/met14010122








