Epidemic, Urban Planning and Health Impact Assessment: A Linking and Analyzing Framework
Abstract
:1. Introduction
2. Urban Planning, Public Health, and HIA
2.1. Urban Planning and Public Health
2.2. HIA and Its Application in Urban Planning
3. Epidemic and Built Environment’s Influence
3.1. Characteristics of Epidemic
3.2. The Influence of Built Environment on The Epidemic
4. A Comprehensive Framework of HIA for Urban Planning and Epidemic (HIA4UPE)
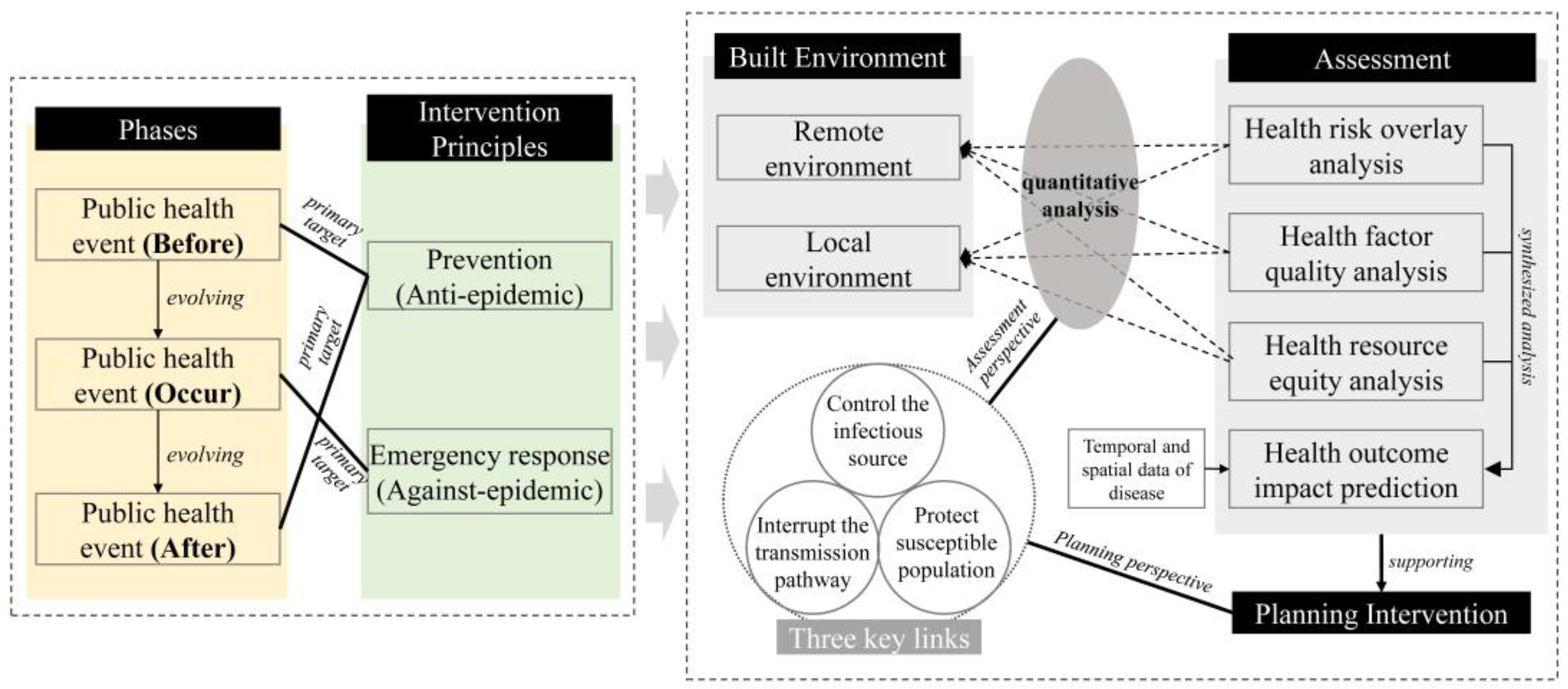
4.1. Establishment and Composition of HIA4UPE
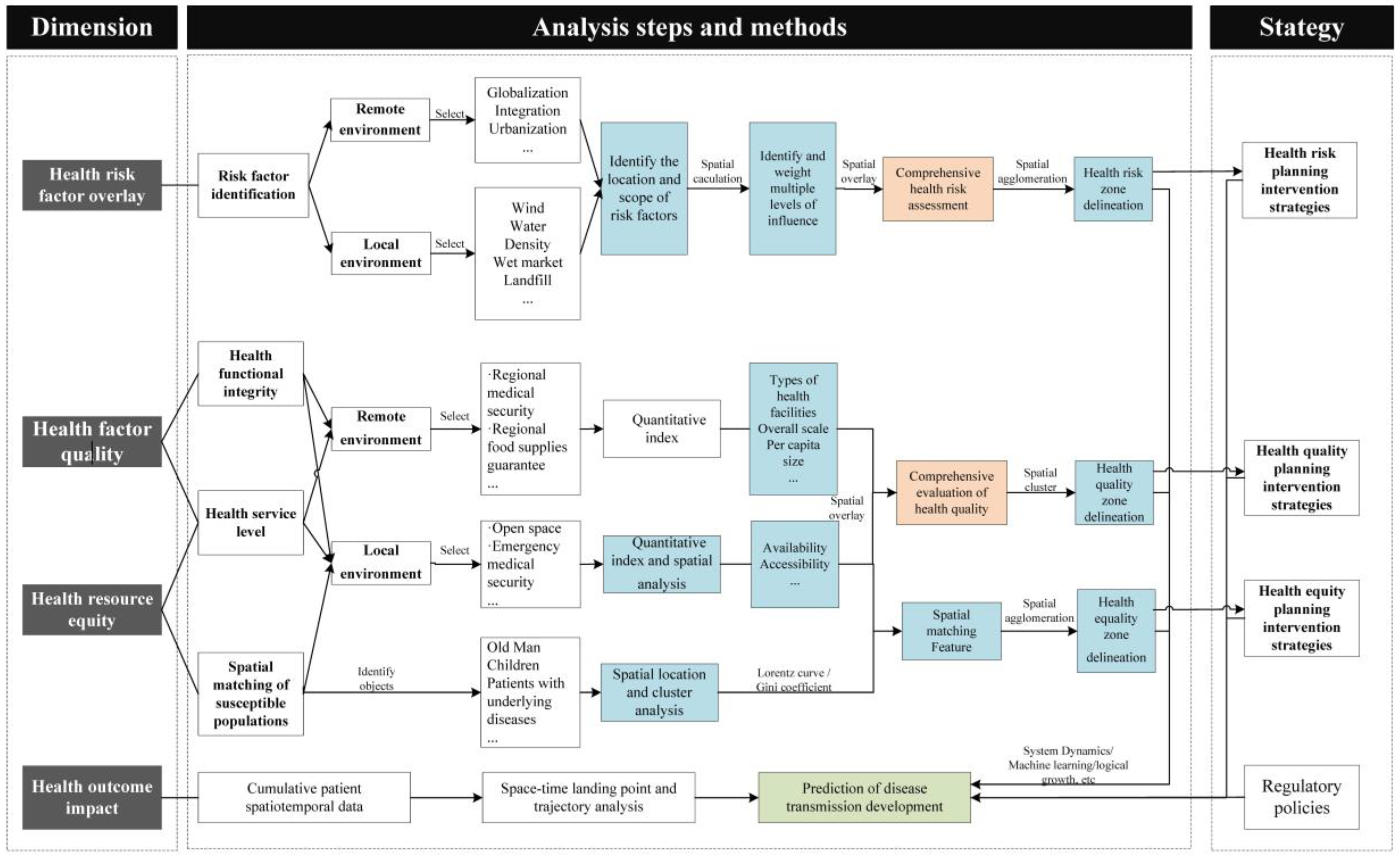
4.2. Assessment Modules of HIA4UPE
4.2.1. Health Risk-Overlay Analysis
4.2.2. Health Factor-Quality Analysis
4.2.3. Health Resource Equity Analysis
4.2.4. Health Outcome-Impact Prediction
5. Analyzing Methods of HIA4UPE
5.1. Spatial Analysis and Computational Technology (SACT)
5.2. Comprehensive Assessment Technology (CAT)
5.3. Prediction Analyzing Technology (PAT)
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Neiderud, C.-J. How urbanization affects the epidemiology of emerging infectious diseases. Infect. Ecol. Epidemiol. 2015, 5, 27060. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wei, Y.D.; Liu, M. Urban Form and Spatiotemporal Vulnerability of Local Communities to COVID-19. Geogr. Rev. 2023, 13, 482–501. [Google Scholar] [CrossRef]
- Wang, F.; Fang, Y.; Deng, H.; Wei, F. How community medical facilities can promote resilient community constructions under the background of pandemics. Indoor Built Environ. 2022, 31, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Jiang, Z.; Hou, Y.; Wang, H.; Wang, Z. Healthy City Community Space-Oriented Structural Planning and Management Optimization under COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 3863. [Google Scholar] [CrossRef] [PubMed]
- Green, G.; Tsouros, A. City Leadership for Health: Summary Evaluation of Phase IV of the WHO European Healthy Cities Network; World Health Organization. Regional Office for Europe: Copenhagen, Denmark, 2008. [Google Scholar]
- Corburn, J.; Bhatia, R. Health impact assessment in San Francisco: Incorporating the social determinants of health into environmental planning. J. Environ. Plan. Manag. 2007, 50, 323–341. [Google Scholar] [CrossRef]
- Fischer, T.B.; Muthoora, T.; Chang, M.; Sharpe, C. Health impact assessment in spatial planning in England–types of application and quality of documentation. Environ. Impact Assess. Rev. 2021, 90, 106631. [Google Scholar] [CrossRef]
- Boshuizen, H.C.; Lhachimi, S.K.; van Baal, P.H.; Hoogenveen, R.T.; Smit, H.A.; Mackenbach, J.P.; Nusselder, W.J. The DYNAMO-HIA model: An efficient implementation of a risk factor/chronic disease Markov model for use in Health Impact Assessment (HIA). Demography 2012, 49, 1259–1283. [Google Scholar] [CrossRef] [PubMed]
- Adam, B.; Molnar, A.; Gulis, G.; Adany, R. Integrating a quantitative risk appraisal in a health impact assessment: Analysis of the novel smoke-free policy in Hungary. Eur. J. Public Health 2013, 23, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Rueda, D.; de Nazelle, A.; Teixidó, O.; Nieuwenhuijsen, M.J. Health impact assessment of increasing public transport and cycling use in Barcelona: A morbidity and burden of disease approach. Prev. Med. 2013, 57, 573–579. [Google Scholar] [CrossRef]
- Thondoo, M.; Goel, R.; Tatah, L.; Naraynen, N.; Woodcock, J.; Nieuwenhuijsen, M. The built environment and health in low-and middle-income countries: A review on quantitative health impact assessments. Curr. Environ. Health Rep. 2022, 9, 90–103. [Google Scholar] [CrossRef]
- Perdue, L.; Michael, Y.; Harris, C.; Heller, J.; Livingston, C.; Rader, M.; Goff, N. Rapid health impact assessment of policies to reduce vehicle miles traveled in Oregon. Public Health 2012, 126, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, T.J.; MacDonald Gibson, J. Health impacts of increased physical activity from changes in transportation infrastructure: Quantitative estimates for three communities. BioMed Res. Int. 2015, 2015, 812325. [Google Scholar] [CrossRef] [PubMed]
- Cook, W.K.; Heller, J.; Bhatia, R.; Farhang, L. A Health Impact Assessment of the Healthy Families Act of 2009; Human Impact Partners and San Francisco Department of Public Health: Oakland, CA, USA, 2009. [Google Scholar]
- Litt, J.S.; Tran, N.L.; Burke, T.A. Examining urban brownfields through the public health “macroscope”. Environ. Health Perspect. 2002, 110, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Lau, C.; Jagals, P. A framework for assessing and predicting the environmental health impact of infectious diseases: A case study of leptospirosis. Rev. Environ. Health 2012, 27, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Littman, R.J. The plague of Athens: Epidemiology and paleopathology. Mt. Sinai J. Med. 2009, 76, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Michael, J. Byzantine town planning analysis of its form, nature and extent. Ekistics 1964, 17, 251–258. [Google Scholar]
- Hussein, H.A.A. Investigating the role of the urban environment in controlling pandemics transmission: Lessons from history. Ain Shams Eng. J. 2022, 13, 101785. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, J. Discussion on Urban Epidemic Prevention and Control in Chang’an City in Tang Dynasty; SPSD Press: Ishikawa, Japan, 2021; pp. 483–499. [Google Scholar]
- Ross, C.L.; Orenstein, M.; Botchwey, N. Health Impact Assessment in the United States; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Barton, H.; Tsourou, C. Healthy Urban Planning; Routledge: London, UK, 2013. [Google Scholar]
- Go, F.C.; World Health Organization. Environmental Impact Assessment: An Analysis of the Methodological and Substantive Issues Affecting Human Health Considerations; Monitoring and Assessment Research Centre: London, UK, 1987. [Google Scholar]
- Bhatia, R. A guide for health impact assessment. CDPH 2010, 10, 17–20. [Google Scholar]
- Schoner, J.; Chapman, J.; Brookes, A.; MacLeod, K.E.; Fox, E.H.; Iroz-Elardo, N.; Frank, L.D. Bringing health into transportation and land use scenario planning: Creating a National Public Health Assessment Model (N-PHAM). J. Transp. Health 2018, 10, 401–418. [Google Scholar] [CrossRef]
- Lhachimi, S.K.; Nusselder, W.J.; Smit, H.A.; van Baal, P.; Baili, P.; Bennett, K.; Fernández, E.; Kulik, M.C.; Lobstein, T.; Pomerleau, J. DYNAMO-HIA–a dynamic modeling tool for generic health impact assessments. PLoS ONE 2012, 7, e33317. [Google Scholar] [CrossRef]
- Kuo, T.; Jarosz, C.J.; Simon, P.; Fielding, J.E. Menu labeling as a potential strategy for combating the obesity epidemic: A health impact assessment. Am. J. Public Health 2009, 99, 1680–1686. [Google Scholar] [CrossRef] [PubMed]
- Gabet, S.; Lemarchand, C.; Guénel, P.; Slama, R. Breast cancer risk in association with atmospheric pollution exposure: A meta-analysis of effect estimates followed by a health impact assessment. Environ. Health Perspect. 2021, 129, 057012. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, A.; Slotterback, C.S.; Krizek, K.J. Health impact assessment in planning: Development of the design for health HIA tools. Environ. Impact Assess. Rev. 2010, 30, 42–51. [Google Scholar] [CrossRef]
- Brighton & Hove City Council. A-Z of Services. Available online: www.brighton-hove.gov.uk (accessed on 20 August 2023).
- Manukau City Council. Wiri Spatial Structure Plan HIA. Available online: www.apho.org.uk/resource/item.aspx?RID=101558 (accessed on 20 August 2023).
- Farhang, L.; Bhatia, R.; Scully, C.C.; Corburn, J.; Gaydos, M.; Malekafzali, S. Creating tools for healthy development: Case study of San Francisco’s eastern neighborhoods community health impact assessment. J. Public Health Manag. Pract. 2008, 14, 255–265. [Google Scholar] [CrossRef] [PubMed]
- De Nazelle, A.; Nieuwenhuijsen, M.J.; Antó, J.M.; Brauer, M.; Briggs, D.; Braun-Fahrlander, C.; Cavill, N.; Cooper, A.R.; Desqueyroux, H.; Fruin, S. Improving health through policies that promote active travel: A review of evidence to support integrated health impact assessment. Environ. Int. 2011, 37, 766–777. [Google Scholar] [CrossRef] [PubMed]
- Holm, A.L.; Glümer, C.; Diderichsen, F. Health Impact Assessment of increased cycling to place of work or education in Copenhagen. BMJ Open 2012, 2, e001135. [Google Scholar] [CrossRef] [PubMed]
- Thornton, R.L.J.; Greiner, A.; Fichtenberg, C.M.; Feingold, B.J.; Ellen, J.M.; Jennings, J.M. Achieving a Healthy Zoning Policy in Baltimore: Results of a Health Impact Assessment of the Trans Form Baltimore Zoning Code Rewrite. Public Health Rep. 2013, 128, 87–103. [Google Scholar] [CrossRef] [PubMed]
- Serrano, E.; Larrañaga, I.; Morteruel, M.; Baixas de Ros, M.D.; Basterrechea, M.; Martinez, D.; Aldasoro, E.; Bacigalupe, A. Urban regeneration as population health intervention: A health impact assessment in the Bay of Pasaia (Spain). Int. J. Equity Health 2016, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.L.; de Nie, K.L.; Dannenberg, A.L.; Beck, L.F.; Marcus, M.J.; Barringer, J. Health impact assessment of the Atlanta BeltLine. Am. J. Prev. Med. 2012, 42, 203–213. [Google Scholar] [CrossRef]
- WHO Africa. Communicable Diseases. Available online: https://www.afro.who.int/node/5557 (accessed on 20 December 2023).
- Centers for Disease Control and Prevention. Infection Control Basics. Available online: https://www.cdc.gov/infection-control/about/?CDC_AAref_Val=https://www.cdc.gov/infectioncontrol/spread/index.html (accessed on 15 April 2024).
- Chen, S.; Zhang, Z.; Yang, J.; Wang, J.; Zhai, X.; Bärnighausen, T.; Wang, C. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet 2020, 395, 1305–1314. [Google Scholar] [CrossRef]
- Jin, S.; Gao, Y.; Xiao, S. Corporate governance structure and performance in the tourism industry in the COVID-19 pandemic: An empirical study of Chinese listed companies in China. Sustainability 2021, 13, 11722. [Google Scholar] [CrossRef]
- Eisenberg, J.N.; Desai, M.A.; Levy, K.; Bates, S.J.; Liang, S.; Naumoff, K.; Scott, J.C. Environmental determinants of infectious disease: A framework for tracking causal links and guiding public health research. Environ. Health Perspect. 2007, 115, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Gittins, H.; Dandy, N.; Wynne-Jones, S.; Morrison, V. “It’s opened my eyes to what’s out there”: How do nature-based interventions influence access to and perceptions of the natural environment? Wellbeing Space Soc. 2023, 4, 100125. [Google Scholar] [CrossRef]
- de Hollander, A.E.; Staatsen, B.A. Health, environment and quality of life: An epidemiological perspective on urban development. Landsc. Urban Plan. 2003, 65, 53–62. [Google Scholar] [CrossRef]
- Shah, V. The Politics and Perceptibility of Breath during the COVID-19 Pandemic; Massachusetts Institute of Technology: Cambridge, MA, USA, 2021. [Google Scholar]
- von Schirnding, Y. Health and sustainable development: Can we rise to the challenge? Lancet 2002, 360, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.D. Responding to global infectious disease outbreaks: Lessons from SARS on the role of risk perception, communication and management. Soc. Sci. Med. 2006, 63, 3113–3123. [Google Scholar] [CrossRef] [PubMed]
- Alirol, E.; Getaz, L.; Stoll, B.; Chappuis, F.; Loutan, L. Urbanisation and infectious diseases in a globalised world. Lancet Infect. Dis. 2011, 11, 131–141. [Google Scholar] [CrossRef]
- Patz, J.A.; Daszak, P.; Tabor, G.M.; Aguirre, A.A.; Pearl, M.; Epstein, J.; Wolfe, N.D.; Kilpatrick, A.M.; Foufopoulos, J.; Molyneux, D. Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence. Environ. Health Perspect. 2004, 112, 1092–1098. [Google Scholar] [CrossRef]
- Patz, J.A.; Graczyk, T.K.; Geller, N.; Vittor, A.Y. Effects of environmental change on emerging parasitic diseases. Int. J. Parasitol. 2000, 30, 1395–1405. [Google Scholar] [CrossRef]
- Connolly, J. Global crisis leadership for disease-induced threats: One Health and urbanisation. Glob. Policy 2020, 11, 283–292. [Google Scholar] [CrossRef]
- Chia, M.L.; Him Chau, D.H.; Lim, K.S.; Yang Liu, C.W.; Tan, H.K.; Tan, Y.R. Managing COVID-19 in a novel, rapidly deployable community isolation quarantine facility. Ann. Intern. Med. 2021, 174, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.-C.; Leung, M.; Tong, D.W.-K.; Lee, L.L.-Y.; Leung, W.L.-H.; Chan, F.W.-K.; Chen, J.H.-K.; Hung, I.F.-N.; Yuen, K.-Y.; Yeung, D.T.-K. Infection control challenges in setting up community isolation and treatment facilities for patients with coronavirus disease 2019 (COVID-19): Implementation of directly observed environmental disinfection. Infect. Control Hosp. Epidemiol. 2021, 42, 1037–1045. [Google Scholar] [CrossRef] [PubMed]
- Muley, D.; Shahin, M.; Dias, C.; Abdullah, M. Role of transport during outbreak of infectious diseases: Evidence from the past. Sustainability 2020, 12, 7367. [Google Scholar] [CrossRef]
- Matthew, R.A.; McDonald, B. Cities under siege: Urban planning and the threat of infectious disease. J. Am. Plan. Assoc. 2006, 72, 109–117. [Google Scholar] [CrossRef]
- Loske, D. The impact of COVID-19 on transport volume and freight capacity dynamics: An empirical analysis in German food retail logistics. Transp. Res. Interdiscip. Perspect. 2020, 6, 100165. [Google Scholar] [CrossRef] [PubMed]
- Liu, L. Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: Evidence from China. Cities 2020, 103, 102759. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.A.; Grace, D.; Kock, R.; Alonso, S.; Rushton, J.; Said, M.Y.; McKeever, D.; Mutua, F.; Young, J.; McDermott, J. Zoonosis emergence linked to agricultural intensification and environmental change. Proc. Natl. Acad. Sci. 2013, 110, 8399–8404. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.R.; Sun, T.; Li, Z.; Zhang, J.; Teng, J.; Liu, X.; Liu, R.; Zhao, R.; Jones, M.K.; Wang, Y. Community surveys and risk factor analysis of human alveolar and cystic echinococcosis in Ningxia Hui Autonomous Region, China. Bull. World Health Organ. 2006, 84, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Hua, L.; Ran, R.; Ni, Z. Are the epidemic prevention facilities effective? How cities should choose epidemic prevention facilities: Taking Wuhan as an example. Front. Public Health 2023, 11, 1125301. [Google Scholar] [CrossRef]
- Hick, J.L.; Hanfling, D.; Burstein, J.L.; DeAtley, C.; Barbisch, D.; Bogdan, G.M.; Cantrill, S. Health care facility and community strategies for patient care surge capacity. Ann. Emerg. Med. 2004, 44, 253–261. [Google Scholar] [CrossRef]
- United Nations Environment Programme and International Livestock Research Institute. Preventing the next pandemic–Zoonotic diseases and how to break the chain of transmission; UNEP: Nairobi, Kenya, 2020. [Google Scholar]
- Wang, L.; Jiang, X.; Li, X. Healthy city and its planning. Urban Climate Science for Planning Healthy Cities; Springer: Cham, Switzerland, 2021; pp. 17–41. [Google Scholar]
- McMichael, A.J. Environmental and social influences on emerging infectious diseases: Past, present and future. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2004, 359, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Xiang, T.; He, L. Modeling epidemic spread in transportation networks: A review. J. Traffic Transp. Eng. 2021, 8, 139–152. [Google Scholar] [CrossRef]
- Boss, L.P. Epidemic hysteria: A review of the published literature. Epidemiol. Rev. 1997, 19, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Shi, B.; Shi, Y.; Marvin, S.; Zheng, Y.; Xia, G. Air pollution dispersal in high density urban areas: Research on the triadic relation of wind, air pollution, and urban form. Sustain. Cities Soc. 2020, 54, 101941. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, Z. Industrial water pollution, water environment treatment, and health risks in China. Environ. Pollut. 2016, 218, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Wang, Z.; An, Y. How to Optimize the Allocation of Anti-epidemic Materials in Public Health Emergencies From the Perspective of Public Economics. Front. Psychol. 2022, 13, 851286. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.Q.; Zheng, B.H.; Yu, H.; Peng, X. Green space layout optimization based on microclimate environment features. Int. J. Sustain. Dev. Plan. 2019, 14, 9–19. [Google Scholar] [CrossRef]
- Toorn, M.v.d. Public space and public health related to green space in urban landscape architecture. In Proceedings of the Fábos Conference on Landscape and Greenway Planning, Budapest, Hungary, 30 June–3 July 2022; p. 69. [Google Scholar]
- Li, S.; Wu, Z.; Tang, J.; Wang, S.; Wang, P. Research on urban country parks based on emergency medical facilities for public health emergencies—A case study of Guangzhou, China. Environ. Sci. Pollut. Res. 2023, 30, 81019–81037. [Google Scholar] [CrossRef] [PubMed]
- van Lunzen, J.; Altfeld, M. Sex differences in infectious diseases–common but neglected. J. Infect. Dis. 2014, 209, S79–S80. [Google Scholar] [CrossRef]
- Zhang, X.; Xia, Q.; Lai, Y.; Wu, B.; Tian, W.; Miao, W.; Feng, X.; Xin, L.; Miao, J.; Wang, N. Spatial effects of air pollution on the economic burden of disease: Implications of health and environment crisis in a post-COVID-19 world. Int. J. Equity Health 2022, 21, 1–16. [Google Scholar] [CrossRef]
- Watson, T. Public health investments and the infant mortality gap: Evidence from federal sanitation interventions on US Indian reservations. J. Public Econ. 2006, 90, 1537–1560. [Google Scholar] [CrossRef]
- Indriyani, W.; Yudhistira, M.H.; Sastiono, P.; Hartono, D. The relationship between the built environment and respiratory health: Evidence from a longitudinal study in Indonesia. SSM-Popul. Health 2022, 19, 101193. [Google Scholar] [CrossRef]
- Hu, Y.; Lin, Z.; Jiao, S.; Zhang, R. High-Density Communities and Infectious Disease Vulnerability: A Built Environment Perspective for Sustainable Health Development. Buildings 2024, 14, 103. [Google Scholar] [CrossRef]
- Liu, C.; Liu, Z.; Guan, C. The impacts of the built environment on the incidence rate of COVID-19: A case study of King County, Washington. Sustain. Cities Soc. 2021, 74, 103144. [Google Scholar] [CrossRef]
- Santangelo, O.E.; Gentile, V.; Pizzo, S.; Giordano, D.; Cedrone, F. Machine learning and prediction of infectious diseases: A systematic review. Mach. Learn. Knowl. Extr. 2023, 5, 175–198. [Google Scholar] [CrossRef]
- Ellwanger, J.H.; Chies, J.A. Wind: A neglected factor in the spread of infectious diseases. Lancet Planet. Health 2018, 2, e475. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; LeJeune, J.; Alsdorf, D.; Lu, B.; Shum, C.; Liang, S. Global distribution of outbreaks of water-associated infectious diseases. PLoS Neglected Trop. Dis. 2012, 6, e1483. [Google Scholar] [CrossRef] [PubMed]
- Li, Y. Computational fluid dynamics technology and its application in wind environment analysis. J. Urban Technol. 2010, 17, 67–81. [Google Scholar] [CrossRef]
- Blocken, B.; Stathopoulos, T.; Carmeliet, J.; Hensen, J.L. Application of computational fluid dynamics in building performance simulation for the outdoor environment: An overview. J. Build. Perform. Simul. 2011, 4, 157–184. [Google Scholar] [CrossRef]
- Nakamura, T.; Nakamura, A.; Mukuda, K.; Harada, M.; Kotani, K. Potential accessibility scores for hospital care in a province of Japan: GIS-based ecological study of the two-step floating catchment area method and the number of neighborhood hospitals. BMC Health Serv. Res. 2017, 17, 438. [Google Scholar] [CrossRef]
- Wang, F.; Luo, W. Assessing spatial and nonspatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health Place 2005, 11, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.; Cheng, Y.; Liu, J. Hierarchical two-step floating catchment area (2SFCA) method: Measuring the spatial accessibility to hierarchical healthcare facilities in Shenzhen, China. Int. J. Equity Health 2020, 19, 164. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Zeng, S.; Namaiti, A.; Zeng, J. Evaluation of Supply–Demand Matching of Public Health Resources Based on Ga2SFCA: A Case Study of the Central Urban Area of Tianjin. ISPRS Int. Geo-Inf. 2023, 12, 156. [Google Scholar] [CrossRef]
- Hajimaghsoudi, M.; Baghian, N.; Raadabadi, M. The Relationship between the Distribution of General Practitioners and the Mortality Rate of Children Based on the Gini Coefficient and Lorenz Curve. Evid. Based Health Policy Manag. Econ. 2018, 2, 109–114. [Google Scholar]
- Wang, Z.; Ye, W.; Chen, X.; Li, Y.; Zhang, L.; Li, F.; Yao, N.; Gao, C.; Wang, P.; Yi, D. Spatio-temporal pattern, matching level and prediction of ageing and medical resources in China. BMC Public Health 2023, 23, 1155. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Hu, Y.; Lai, L. Demography-oriented urban spatial matching of service facilities: Case study of changchun, China. Land-Basel 2022, 11, 1660. [Google Scholar] [CrossRef]
- Gong, X.; Liu, J.; Wu, L.; Bu, Z.; Zhu, Z. Development of a healthy assessment system for residential building epidemic prevention. Build. Environ. 2021, 202, 108038. [Google Scholar] [CrossRef]
- Luo, Z.; Zhou, Z.; Hao, Y.; Feng, J.; Gong, Y.; Li, Y.; Huang, Y.; Zhang, Y.; Li, S. Establishment of an indicator framework for the transmission risk of the mountain-type zoonotic visceral leishmaniasis based on the Delphi-entropy weight method. Infect. Dis. Poverty 2022, 11, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Lu, X.; Zeng, W.; Tao, L.; Li, Y. Research on the evaluation and optimization model of community public space during the epidemic prevention period based on TOPSIS. Environ. Dev. Sustain. 2024, 26, 9553–9576. [Google Scholar] [CrossRef]
- Abidin, N.Z.; Jaafar, I.A.; Wibowo, A.; Alwi, A. Prioritizing the Dengue Epidemic Mitigation Strategy Using Fuzzy TOPSIS Approach. Eur. J. Mol. Clin. Med. 2020, 7, 3833–3844. [Google Scholar]
- Peng, Z.; Su, P.; Chen, W. Indoor Air Quality Assessment of Metro Stations Based on the Optimal Combination Weight and Improved Fuzzy Comprehensive Evaluation. J. Environ. Eng. 2023, 149, 04023001. [Google Scholar] [CrossRef]
- Cui, L. Applying fuzzy comprehensive evaluation method to evaluate quality in crisis and emergency management. Commun. Stat.-Theory Methods 2012, 41, 3942–3959. [Google Scholar] [CrossRef]
- He, X.; Li, L.; Liu, X.; Wu, Y.; Mei, S.; Zhang, Z. Using grey relational analysis to analyze influential factor of hand, foot and mouth disease in Shenzhen. Grey Syst. Theory Appl. 2019, 9, 197–206. [Google Scholar] [CrossRef]
- Rehman, S.; Rehman, E.; Mumtaz, A.; Jianglin, Z. Cardiovascular disease mortality and potential risk factor in china: A multi-dimensional assessment by a grey relational approach. Int. J. Public Health 2022, 67, 1604599. [Google Scholar] [CrossRef] [PubMed]
- Hezer, S.; Gelmez, E.; Özceylan, E. Comparative analysis of TOPSIS, VIKOR and COPRAS methods for the COVID-19 Regional Safety Assessment. J. Infect. Public Health 2021, 14, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Guo, Z.; Ai, L.; Liu, J.; Zhang, X.; Cao, C.; Xu, J.; Xia, S.; Zhou, X.-N.; Chen, J. Establishment of an indicator framework for global One Health Intrinsic Drivers index based on the grounded theory and fuzzy analytical hierarchy-entropy weight method. Infect. Dis. Poverty 2022, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Darko, A.; Chan, A.P.C.; Ameyaw, E.E.; Owusu, E.K.; Pärn, E.; Edwards, D.J. Review of application of analytic hierarchy process (AHP) in construction. Int. J. Constr. Manag. 2019, 19, 436–452. [Google Scholar] [CrossRef]
- Han, L.; Song, Y.; Duan, L.; Yuan, P. Risk assessment methodology for Shenyang Chemical Industrial Park based on fuzzy comprehensive evaluation. Environ. Earth Sci. 2015, 73, 5185–5192. [Google Scholar] [CrossRef]
- Munier, N.; Hontoria, E.; Munier, N.; Hontoria, E. Shortcomings of the AHP Method. In Uses and Limitations of the AHP Method: A Non-Mathematical and Rational Analysis; Springer: Cham, Switzerland, 2021; pp. 41–90. [Google Scholar]
- Yang, Y.; Atkinson, P.; Ettema, D. Individual space–time activity-based modelling of infectious disease transmission within a city. J. R. Soc. Interface 2008, 5, 759–772. [Google Scholar] [CrossRef]
- Qi, F.; Du, F. Tracking and visualization of space-time activities for a micro-scale flu transmission study. Int. J. Health Geogr. 2013, 12, 1–16. [Google Scholar] [CrossRef]
- Xiong, L.; Hu, P.; Wang, H. Establishment of epidemic early warning index system and optimization of infectious disease model: Analysis on monitoring data of public health emergencies. Int. J. Disaster Risk Reduct. 2021, 65, 102547. [Google Scholar] [CrossRef]
- Shen, C.Y. Logistic growth modelling of COVID-19 proliferation in China and its international implications. Int. J. Infect. Dis. 2020, 96, 582–589. [Google Scholar] [CrossRef]
- Gharakhanlou, N.M.; Hooshangi, N. Spatio-temporal simulation of the novel coronavirus (COVID-19) outbreak using the agent-based modeling approach (case study: Urmia, Iran). Inform. Med. Unlocked 2020, 20, 100403. [Google Scholar] [CrossRef]
- Wang, C.; Wang, F. GIS-automated delineation of hospital service areas in Florida: From Dartmouth method to network community detection methods. Ann. GIS 2022, 28, 93–109. [Google Scholar] [CrossRef]
| Built Environment | Public Health Event Development Phases | Intervention Principles | Key Links | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Dimension | Specific Factors | Before | Occurs | After | Prevention | Emergency Response | Controlling the Infectious Source | Interrupting the Transmission Pathway | Protecting Susceptible Populations |
| Remote environment | Globalization | △ | ● | △ | △ | ● | √ | ||
| Integration | △ | ● | △ | △ | ● | √ | |||
| Urbanization | △ | ● | △ | △ | ● | √ | √ | ||
| Site selection and construction of large-scale projects | ○ | ● | ○ | ○ | ● | √ | √ | ||
| Medical industry structure and layout | ○ | ● | ○ | ● | ● | √ | √ | ||
| Logistics transportation | △ | ● | △ | △ | ● | √ | |||
| Food production and processing | △ | ● | △ | △ | ● | ||||
| Local environment | Density | ● | △ | ○ | ● | △ | √ | ||
| Wind environment | ● | △ | ○ | ● | △ | √ | |||
| Water environment | ● | △ | ○ | ● | △ | √ | |||
| Public transportation | △ | ● | △ | △ | ● | √ | |||
| Open space | ● | △ | ○ | ● | △ | √ | √ | ||
| Classification and grading of medical facilities | ● | ● | ● | ● | ● | √ | √ | ||
| Community emergency services facilities | ● | ● | ● | ● | ● | √ | √ | ||
| Wet market | ○ | ● | ○ | ○ | ● | √ | √ | √ | |
| Refuse collection, transfer, and disposal station | ○ | ● | ○ | ○ | ● | √ | √ | √ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, X.; Ye, D.; Lan, W.; Luo, Y. Epidemic, Urban Planning and Health Impact Assessment: A Linking and Analyzing Framework. Buildings 2024, 14, 2141. https://doi.org/10.3390/buildings14072141
Jiang X, Ye D, Lan W, Luo Y. Epidemic, Urban Planning and Health Impact Assessment: A Linking and Analyzing Framework. Buildings. 2024; 14(7):2141. https://doi.org/10.3390/buildings14072141
Chicago/Turabian StyleJiang, Xiji, Dan Ye, Wenlong Lan, and Yinglu Luo. 2024. "Epidemic, Urban Planning and Health Impact Assessment: A Linking and Analyzing Framework" Buildings 14, no. 7: 2141. https://doi.org/10.3390/buildings14072141






