Invasive Candida Infections in Neonates after Major Surgery: Current Evidence and New Directions
Abstract
:1. Introduction
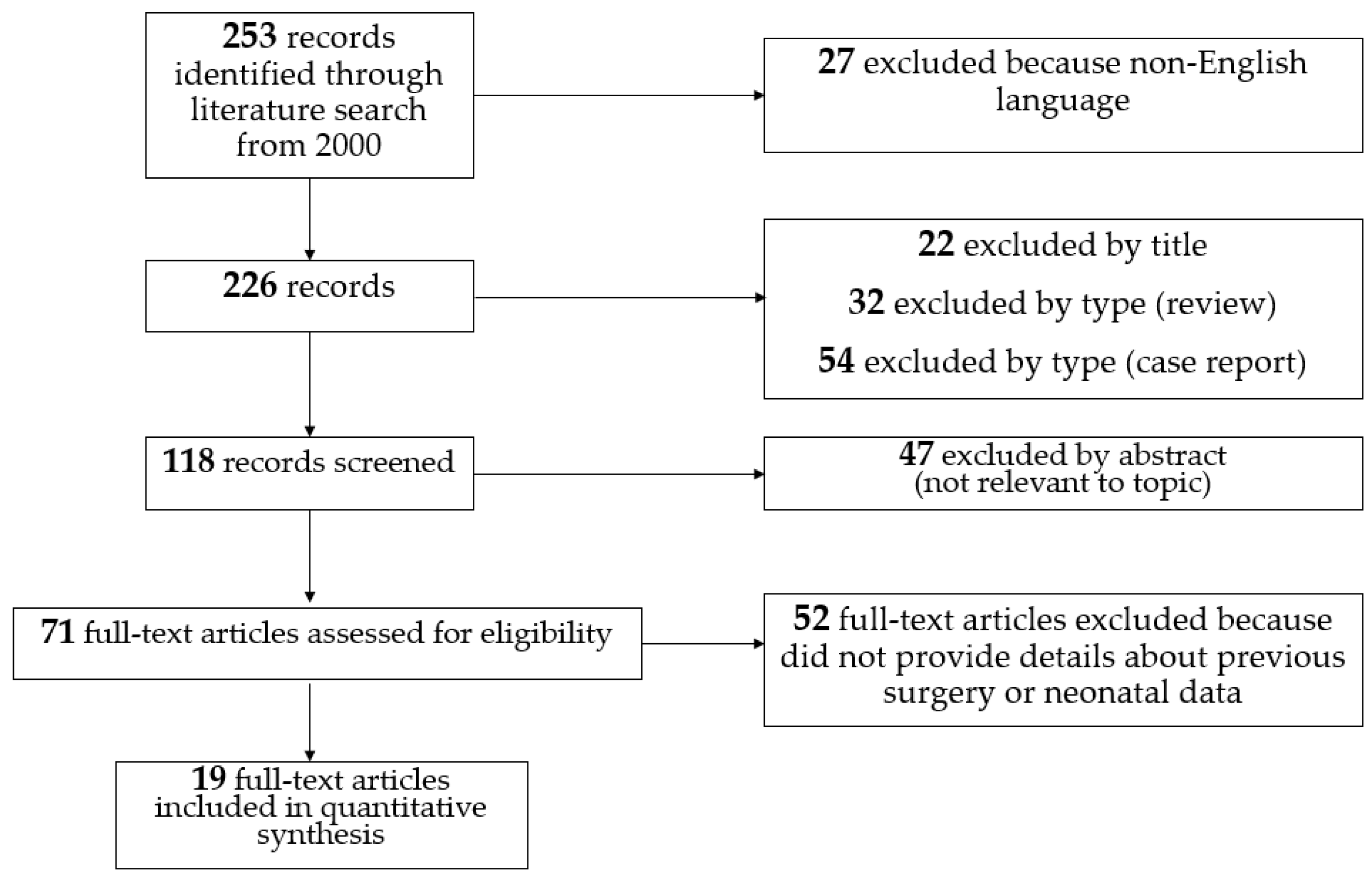
2. Methods
3. Results
4. Risk Factors for Invasive Candida Infections after Major Surgery
- Prematurity: Prematurity was recognized as the most common underlying condition (78%) among newborns with candidemia, with a median gestational age at birth of 25 weeks (IQR: 24–26) according to the United States’ Centers for Disease Control and Prevention’s (CDC’s) active population-based surveillance [22]. Most preterm neonates had a very low birth weight (VLBW, 1000–1500 g) or extremely low birth weight (ELBW, <1000 g) [22]. Mortality is high in ELBW infants with ICIs: Benjamin et al. reported an overall mortality of 34% for ELBW infants with ICIs compared with 14% for ELBW infants without ICIs [34].
- Site of surgery: Surgery in the 90 days before diagnosis was the most common (38%) underlying condition among infants with ICIs. The abdomen was the most common site of surgery, according to data from four US CDCs [22]. Gastrointestinal diseases, including congenital anomalies (i.e., gastroschisis, omphalocele, duodenal or ileocolic atresia/stenosis, necrotizing enterocolitis with intestinal perforation, stoma carriers in any location) predispose patients to candidemia, as a result of a compromised intestinal barrier that promotes translocation of Candida colonizing the gastrointestinal tract [35].
- Candida colonization: Candida colonization is the most important risk factor for ICIs and is further discussed below; it can involve from 10% to 60% of preterm babies during their hospital stay in NICU [36].
- Use of central lines: Despite numerous efforts in recent decades to reduce the incidence of central line associated sepsis (CLABSI) and central lines related sepsis (CRBSI) in NICUs, such infections still represent a major complication of health care assistance in those critically ill infants. Central-line-associated blood-stream infections (CLABSIs) arise from at least 48 h after CVC insertion to 48 h after CVC removal. Catheter-related blood-stream infections (CRBSIs) are bacteremias with positivity of CVC blood cultures developing at least 2 h earlier compared to peripheral blood cultures, or when the same organism is recovered from percutaneous blood culture and catheter lumen blood culture, with 3-fold greater colony count in the latter [37]. In particular, newborns undergoing major surgery in most cases have a central vascular catheter and are most susceptible to these infections. Among the germs involved in the genesis of CLABSIs, Candida spp. represented the third most common pathogens (13%), after Coagulase-Negative Staphylococci (28%), and Staphylococcus aureus (19%) in a study in 304 NICUs [38]. The length of stay of indwelling catheters is a strong risk factor for CLABSI and CRBSI, while no differences have been reported between the CLABSI incidence in femoral vein catheters, peripherally inserted catheters, and umbilical venous catheters [38]. Catheter removal is recommended if a CRBSI caused by coagulase-negative Staphylococci, gram-negative bacilli (Pseudomonas aeruginosa and Klebsiella pneumoniae), and fungi occurs, due to the particular ability of these germs to form an intraluminal biofilm, resistant to antibiotics and/or antifungals. Biofilms on indwelling catheters may be composed of gram-positive or gram-negative bacteria or yeasts. It consists of microbial cells surrounded by a self-secreting polymer matrix, that is released into the extracellular space [39]. The matrix is composed of water, polysaccharides, proteins, lipids, and extracellular DNA. This matrix provides a protective barrier from the surrounding environment and is able to hinder the penetration of antimicrobial drugs, while also providing protection against the host’s immune defense mechanisms. From this biofilm, germs are progressively released, causing the infection to persist and favoring the dissemination of microbes to additional sites in the body. The biofilm is very difficult to eradicate from the catheter, due to the difficult penetration of antimicrobial drugs into the matrix. Therefore, CVC removal is the gold standard approach in cases of CRBSI that do not respond to systemic treatment [37,40]. The best timing of central venous catheter removal in the presence of an associated and/or catheter-related Candida infection has been studied by many authors [40,41], which demonstrated that early catheter removal in candidemia is associated with better outcomes in terms of shorter duration of infection, reduced mortality, and reduced long-term neurologic disabilities. When catheter removal is not recommended for the patient’s condition, the lock therapy with antimicrobials may be an option. This rescue therapy has shown promise as a strategy for the treatment of CRBSI due to several Candida species. The most promising strategies of antifungal lock therapy include the use of amphotericin B, ethanol, or echinocandins [42,43].
- Use of corticosteroids: Treatment with corticosteroids is a risk factors for invasive fungal infections in the neonatal period. However, data are controversial. The addition of steroids to the antibiotic therapy in animal models increases the intestinal colonization, with an increase in the incidence of invasive infections [44]. Yu et al. reported no significant differences between neonates with ICI and their control peers reviewing medical charts of 5135 NICU admissions [17]. Length and dosage of steroid treatment may play a role in altering the risk in these infants.
- Use of prolonged broad-spectrum antibiotics: Longer duration of antibiotic treatment, in particular third-generation cephalosporins, vancomycin, or carbapenems, increases the risk of ICIs [17]. One of the hypotheses for the role of cephalosporins is that their concentration within the biliary system would cause intestinal dysmicrobism, favoring the proliferation of opportunistic germs, in particular fungi. Considering the antibiotic and other drugs exposure and the risk of infection by species of Candida, the third generation of cephalosporins seems to be a risk factor for Candida albicans infection, while parenteral nutrition, lipidic emulsion, and H2 antagonists are risk factors for Candida parapsilosis infections [11].
- Use of antacids: Inhibitors of gastric acidity such as proton-pump inhibitors (PPIs, e.g., omeprazole) are widely used to prevent and manage feeding intolerance and gastroesophageal reflux, although few data on safety and efficacy are available. However, PPIs potentially increase the risk of systemic infections and necrotizing enterocolitis (NEC), especially in preterm infants [45]. In a multicenter cohort of 743 infants, the main pathogens causing infections in infants exposed to inhibitors of gastric acidity were gram-negative-bacilli and Candida spp. [46].
- Use of parenteral nutrition: Parenteral nutrition (PN) is often considered an ideal microbial growth medium, and lipid administration in particular poses a specific risk for microbial growth [47]. PN given without the use of appropriate filters could contribute to potentially important extrinsic mechanism of infection in NICU patients [11]. Patients with species other than C. albicans were more likely to have PN than those with C. albicans (96.3% versus 71.4%, p = 0.039) [48].
- Endotracheal intubation and invasive devices: Surgical and mechanical devices such as endotracheal tubes, drains, or urinary catheters may be also responsible for the nosocomial spread of pathogens. According to an epidemiologic surveillance study, two devices increased the relative risk for nosocomial infections by 2.6 times and three devices by 3.6 times [49].
- Others: A length of stay in NICU >7 days was reported as one of the main potential risk factors by a multicenter IFI surveillance project (the AURORA project) [50]. Lack of, or inadequate, hand hygiene of healthcare workers has been also reported as one of the main reasons for horizontal transmission of virulent Candida spp. responsible for the invasive infections in critical patients, such as neonates [51]. Neutropenia, defined as neutrophil count <1500/mm3, was found as an independent predictor of candidemia in NICUs [52,53]. Extracorporeal membrane oxygenation (ECMO) procedures and locations may contribute to acquired infection risk and the most common organisms identified were coagulase-negative Staphylococci, followed by Candida, and Pseudomonas species at eight children’s hospitals [54].
5. Candida Colonization
6. Innate Defense Mechanisms against Candida and Surgery
7. Population Microdiversity and Role of Different Species of Candida
8. Epidemiology of Fungal Infections in NICUs
9. Prophylaxis of Fungal Infections
10. Diagnosis of Invasive Candida Infections
- (a)
- the T2 Magnetic Resonance Candida Panel (T2 Candida, T2 Biosystems, Lexington, MA, USA) can detect five major Candida species (C. albicans/C. tropicalis, C. parapsilosis, and C. krusei/C. glabrata) directly in blood and it does not require viable organisms, with a lower time to positivity (lower than 3 h) [93,94]. T2 Candida can be used to efficiently diagnose or rule out candidemia even using low-volume blood specimens from pediatric patients: this could result in improved time to appropriate antifungal therapy or reduction in unnecessary empirical antifungal therapy [95].
- (b)
- the indirect immunofluorescence assay (IFA) for C. albicans germ tube antibody (CAGTA) IgG is a method that enables the detection of specific IgG antibodies against antigens located on the cell wall surface of the mycelium of Candida spp. in human serum/plasma. Vircell Kit (Granada, Spain) and VirClia IgG Monotest (Granada, Spain) are the routine detection ways with widespread use in Europe. According to a systematic review, the diagnostic accuracy of the CAGTA assays is moderate for ICIs, and CAGTA findings should be interpreted in parallel with other biomarkers [96].
11. Treatment of Invasive Candida Infections
12. Future Research Considerations
13. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hoyer, L.L.; Cota, E. Candida albicans Agglutinin-Like Sequence (Als) Family Vignettes: A Review of Als Protein Structure and Function. Front. Microbiol. 2016, 7, 280. [Google Scholar] [CrossRef] [Green Version]
- Filler, S.G.; Sheppard, D.C. Fungal invasion of normally non-phagocytic host cells. PLoS Pathog. 2006, 2, e129. [Google Scholar] [CrossRef]
- Staniszewska, M. Virulence Factors in Candida species. Curr. Protein Pept. Sci. 2020, 21, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, E.; Smith, P.B.; Jacqz-Aigrain, E.; Kaguelidou, F.; Cohen-Wolkowiez, M.; Manzoni, P.; Benjamin, D.K., Jr. Neonatal fungal infections: When to treat? Early Hum. Dev. 2012, 88, S6–S10. [Google Scholar] [CrossRef] [Green Version]
- Benjamin, D.K.; Stoll, B.J.; Gantz, M.G.; Walsh, M.C.; Sánchez, P.J.; Das, A.; Shankaran, S.; Higgins, R.D.; Auten, K.J.; Miller, N.A.; et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal candidiasis: Epidemiology, risk factors, and clinical judgment. Pediatrics 2010, 126, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Hope, W.W.; Castagnola, E.; Groll, A.H.; Roilides, E.; Akova, M.; Arendrup, M.C.; Arikan-Akdagli, S.; Bassetti, M.; Bille, J.; Cornely, O.A.; et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: Prevention and management of invasive infections in neonates and children caused by Candida spp. Clin. Microbiol. Infect. 2012, 18, 38–52. [Google Scholar] [CrossRef] [Green Version]
- Autmizguine, J.; Smith, P.B.; Prather, K.; Bendel, C.; Natarajan, G.; Bidegain, M.; Kaufman, D.A.; Burchfield, D.J.; Ross, A.S.; Pandit, P.; et al. Fluconazole Prophylaxis Study Team. Effect of fluconazole prophylaxis on Candida fluconazole susceptibility in premature infants. J. Antimicrob. Chemother. 2018, 73, 3482–3487. [Google Scholar] [CrossRef] [PubMed]
- Auriti, C.; Goffredo, B.M.; Ronchetti, M.P.; Piersigilli, F.; Cairoli, S.; Bersani, I.; Dotta, A.; Bagolan, P.; Pai, M.P. High-dose micafungin in neonates and young infants with invasive candidiasis: Results of a phase 2 study. Antimicrob. Agents Chemother. 2021, AAC.02494-20. [Google Scholar] [CrossRef]
- Chapman, R.L.; Faix, R.G. Persistently positive cultures and outcome in invasive neonatal candidiasis. Pediatric Infect. Dis. J. 2000, 19, 822–827. [Google Scholar] [CrossRef]
- Mokaddas, E.; Ramadan, S.; Abo el Maaty, S.; Sanyal, S. Candidemia in Pediatric Surgery Patients. J. Chemother. 2000, 12, 332–338. [Google Scholar] [CrossRef]
- Saiman, L.; Ludington, E.; Pfaller, M.; Rangel-Frausto, S.; Wiblin, R.T.; Dawson, J.; Blumberg, H.M.; Patterson, J.E.; Rinaldi, M.; Edwards, J.E.; et al. Risk factors for candidemia in Neonatal Intensive Care Unit patients. Pediatric Infect. Dis. J. 2000, 19, 319–324. [Google Scholar] [CrossRef]
- Roilides, E.; Farmaki, E.; Evdoridou, J.; Dotis, J.; Hatziioannidis, E.; Tsivitanidou, M.; Bibashi, E.; Filioti, I.; Sofianou, D.; Gil-Lamaignere, C.; et al. Neonatal candidiasis: Analysis of epidemiology, drug susceptibility, and molecular typing of causative isolates. Eur. J. Clin. Microbiol. Infect. Dis. 2004, 23, 745–750. [Google Scholar] [CrossRef]
- Avila-Aguero, M.L.; Canas-Coto, A.; Ulloa-Gutierrez, R.; Caro, M.A.; Alfaro, B.; Paris, M.M. Risk factors for Candida infections in a neonatal intensive care unit in Costa Rica. Int. J. Infect. Dis. 2005, 9, 90–95. [Google Scholar] [CrossRef] [Green Version]
- Shetty, S.S.; Harrison, L.H.; Hajjeh, R.A.; Taylor, T.; Mirza, S.A.; Schmidt, A.B.; Sanza, L.T.; Shutt, K.A.; Fridkin, S.K. Determining Risk Factors for Candidemia Among Newborn Infants from Population-Based Surveillance: Baltimore, Maryland, 1998–2000. Pediatric Infect. Dis. J. 2005, 24, 601–604. [Google Scholar] [CrossRef] [PubMed]
- Badran, E.F.; Al Baramki, J.H.; Al Shamyleh, A.; Shehabi, A.; Khuri-Bulos, N. Epidemiology and clinical outcome of candidaemia among Jordanian newborns over a 10-year period. Scand. J. Infect. Dis. 2008, 40, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Blyth, C.C.; Chen, S.C.; Slavin, M.A.; Serena, C.; Nguyen, Q.; Marriott, D.; Ellis, D.; Meyer, W.; Sorrell, T.C. Australian Candidemia Study. Not Just Little Adults: Candidemia Epidemiology, Molecular Characterization, and Antifungal Susceptibility in Neonatal and Pediatric Patients. Pediatrics 2009, 123, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Du, L.; Yuan, T.; Zheng, J.; Chen, A.; Chen, L.; Shi, L. Risk factors and clinical analysis for invasive fungal infection in neonatal intensive care unit patients. Am. J. Perinatol. 2013, 30, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Baptista, M.I.; Nona, J.; Ferreira, M.; Sampaio, I.; Abrantes, M.; Tomé, M.T.; Neto, M.T.; Barroso, R.; Serelha, M.; Virella, D. Invasive fungal infection in neonatal intensive care units: A multicenter survey. J. Chemother. 2016, 28, 37–43. [Google Scholar] [CrossRef]
- Oeser, C.; Vergnano, S.; Naidoo, R.; Anthony, M.; Chang, J.; Chow, P.; Clarke, P.; Embleton, N.; Kennea, N.; Pattnayak, S.; et al. Neonatal Infection Surveillance Network (neonIN). Neonatal invasive fungal infection in England 2004–2010. Clin. Microbiol. Infect. 2014, 20, 936–941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, M.; Huang, S.; Guo, L.; Li, H.; Wang, F.; Zhang, Q.I.; Song, G. Clinical features and risk factors for blood stream infections of Candida in neonates. Exp. Ther. Med. 2015, 10, 1139–1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mesini, A.; Bandettini, R.; Caviglia, I.; Fioredda, F.; Amoroso, L.; Faraci, M.; Mattioli, G.; Piaggio, G.; Risso, F.M.; Moscatelli, A.; et al. Candida infections in paediatrics: Results from a prospective centre study in a tertiary care children’ s hospital. Mycoses 2016, 1–6. [Google Scholar] [CrossRef]
- Benedict, K.; Roy, M.; Kabbani, S.; Anderson, E.J.; Farley, M.M.; Harb, S.; Harrison, L.H.; Bonner, L.; Wadu, V.L.; Marceaux, K.; et al. Neonatal and Pediatric Candidemia: Results from Population-Based Active Laboratory Surveillance in Four US Locations, 2009–2015. J. Pediatric Infect. Dis. Soc. 2018, 7, e78–e85. [Google Scholar] [CrossRef]
- Charsizadeh, A.; Mirhendi, H.; Nikmanesh, B.; Eshaghi, H.; Makimura, K. Microbial epidemiology of candidaemia in neonatal and paediatric intensive care units at the Children’s Medical Center, Tehran. Mycoses 2018, 61, 22–29. [Google Scholar] [CrossRef]
- Fortmann, I.; Hartz, A.; Paul, P.; Pulzer, F.; Müller, A.; Böttger, R.; Proquitté, H.; Dawczynski, K.; Simon, A.; Rupp, J.; et al. German Neonatal Network. Antifungal Treatment and Outcome in Very Low Birth Weight Infants: A Population-based Observational Study of the German Neonatal Network. Pediatric Infect. Dis. J. 2018, 37, 1165–1171. [Google Scholar] [CrossRef]
- Tsai, M.H.; Hsu, J.F.; Yang, L.Y.; Pan, Y.B.; Lai, M.Y.; Chu, S.M.; Huang, H.R.; Chiang, M.C.; Fu, R.H.; Lu, J.J. Candidemia due to uncommon Candida species in children: New threat and impacts on outcomes. Sci. Rep. 2018, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Öncü, B.; Belet, N.; Emecen, A.N.; Birinci, A. Health care-associated invasive Candida infections in children. Med. Mycol. 2019, 57, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Leverger, G.; Timsit, J.F.; Milpied, N.; Gachot, B. Use of Micafungin for the Prevention and Treatment of Invasive Fungal Infections in Everyday Pediatric Care in France: Results of the MYRIADE Study. Pediatric Infect. Dis. J. 2019, 38, 716–721. [Google Scholar] [CrossRef]
- Ostrosky-Zeichner, L.; Sable, C.; Sobel, J.; Alexander, B.D.; Donowitz, G.; Kan, V.; Kauffman, C.A.; Kett, D.; Larsen, R.A.; Morrison, V.; et al. Multicenter retrospective development and validation of a clinical prediction rule for nosocomial invasive candidiasis in the intensive care setting. Eur. J. Clin. Microbiol. Infect. Dis. 2007, 26, 271–276. [Google Scholar] [CrossRef]
- Hermsen, E.D.; Zapapas, M.K.; Maiefski, M.; Rupp, M.E.; Freifeld, A.G.; Kalil, A.C. Validation and comparison of clinical prediction rules for invasive candidiasis in intensive care unit patients: A matched case-control study. Crit. Care 2011, 15, R198. [Google Scholar] [CrossRef] [Green Version]
- Bassetti, M.; Righi, E.; Ansaldi, F.; Merelli, M.; Scarparo, C.; Antonelli, M.; Garnacho-Montero, J.; Diaz-Martin, A.; Palacios-Garcia, I.; Luzzati, R.; et al. A multicenter multinational study of abdominal candidiasis: Epidemiology, outcomes and predictors of mortality. Intensive Care Med. 2015, 4, 1601–1610. [Google Scholar] [CrossRef]
- Kett, D.H.; Azoulay, E.; Echeverria, P.M.; Vincent, J.L. The EPIC II Group of Investigators. Candida bloodstream infections in intensive care units: Analysis of the extended prevalence of infection in intesive care unit study. Crit. Care Med. 2011, 39, 665–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kullberg, B.J.; Arendrup, M.C. Invasive Candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent, J.L.; Rello, J.; Marshall, J.; Silva, E.; Anzueto, A.; Martin, C.D.; Moreno, R.; Lipman, J.; Gomersall, C.; Sakr, Y.; et al. EPIC II Group of Investigators. International Study of the Prevalence and Outcomes of Infection in Intensive Care Units. JAMA 2009, 302, 2323–2329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Autmizguine, J.; Hornik, C.P.; Benjamin, D.K., Jr.; Brouwer, K.L.; Hupp, S.R.; Cohen-Wolkowiez, M.; Watt, K.M. Pharmacokinetics and Safety of Micafungin in Infants Supported with Extracorporeal Membrane Oxygenation. Pediatric Infect. Dis. J. 2016, 35, 1204–1210. [Google Scholar] [CrossRef] [Green Version]
- Yan, L.; Yang, C.; Tang, J. Disruption of the intestinal mucosal barrier in Candida albicans infections. Microbiol. Res. 2013, 168, 389–395. [Google Scholar] [CrossRef]
- Manzoni, P.; Mostert, M.; Jacqz-Aigrain, E.; Stronati, M.; Farina, D. Candida colonization in the nursery. J. Pediatric (Rio J.). 2012, 88, 187–190. [Google Scholar] [CrossRef] [Green Version]
- Mermel, L.A.; Allon, M.; Bouza, E.; Craven, D.E.; Flynn, P.; O’Grady, N.P.; Raad, I.I.; Rijnders, B.J.; Sherertz, R.J.; Warren, D.K. Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 49, 1–45. [Google Scholar] [CrossRef]
- Dubbink-Verheij, G.H.; Bekker, V.; Pelsma, I.C.M.; van Zwet, E.W.; Smits-Wintjens, V.E.H.J.; Steggerda, S.J.; Te Pas, A.J.; Lopriore, E. Bloodstream infection incidence of Different central Venous Catheters in Neonates: A Descriptive Cohort Study. Front. Pediatrics 2017, 5, 1–7. [Google Scholar] [CrossRef]
- Gominet, M.; Compain, F.; Beloin, C.; Lebeaux, D. Central venous catheters and biofilms: Where do we stand in 2017? APMIS 2017, 125, 365–375. [Google Scholar] [CrossRef] [Green Version]
- Karlowicz, M.G.; Hashimoto, L.N.; Kelly, R.E.; Buescher, E.S. Should Central Venous Catheters Be Removed as Soon as Candidemia Is Detected in Neonates? Pediatrics 2000, 106, E63. [Google Scholar] [CrossRef] [Green Version]
- Benjamin, D.K.; Stoll, B.J.; Fanaroff, A.A.; McDonald, S.A.; Oh, W.; Higgins, R.D.; Duara, S.; Poole, K.; Laptook, A.; Goldberg, R.; et al. Neonatal Candidiasis Among Extremely Low Birth Weight Infants: Risk Factors, Mortality Rates, and Neurodevelopmental Outcomes at 18 to 22 Months. Pediatrics 2006, 117, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.E.; Tan, K.; Lai, N.M.; McDonald, S.J. Antibiotic lock for the prevention of catheter-related infection in neonates. Cochrane Database Syst. Rev. 2015, 6. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef]
- Bendel, C.M.; Wiesner, S.M.; Garni, R.M.; Cebelinski, E.; Wells, C.L. Cecal Colonization and Systemic Spread of Candida albicans in Mice Treated with Antibiotics and Dexamethasone. Pediatric Res. 2002, 51, 290–295. [Google Scholar] [CrossRef] [Green Version]
- Terrin, G.; Passariello, A.; De Curtis, M.; Manguso, F.; Salvia, G.; Lega, L.; Messina, F.; Paludetto, R.; Berni Canani, R. Ranitidine is associated with infections, necrotizing enterocolitis, and fatal outcome in newborns. Pediatrics 2012, 129, e40–e45. [Google Scholar] [CrossRef] [Green Version]
- Manzoni, P.; García Sánchez, R.; Meyer, M.; Stolfi, I.; Pugni, L.; Messner, H.; Cattani, S.; Betta, P.M.; Memo, L.; Decembrino, L.; et al. Exposure to Gastric Acid Inhibitors Increases the Risk of Infection in Preterm Very Low Birth Weight Infants but Concomitant Administration of Lactoferrin Counteracts This Effect. J. Pediatrics 2018, 193, 62–67.e1. [Google Scholar] [CrossRef] [Green Version]
- Austin, P.D.; Hand, K.S.; Elia, M. Systematic review and meta-analyses of the effect of lipid emulsion on microbial growth in parenteral nutrition. J. Hosp. Infect. 2016, 94, 307–319. [Google Scholar] [CrossRef]
- Caggiano, G.; Lovero, G.; De Giglio, O.; Barbuti, G.; Montagna, O.; Laforgia, N.; Montagna, M.T. Candidemia in the Neonatal Intensive Care Unit: A Retrospective, Observational Survey and Analysis of Literature Data. Biomed. Res. Int. 2017, 2017, 7901763. [Google Scholar] [CrossRef] [Green Version]
- Becerra, M.R.; Tantaleán, J.A.; Suárez, V.J.; Alvarado, M.C.; Candela, J.L.; Urcia, F.C. Epidemiologic surveillance of nosocomial infections in a Pediatric Intensive Care Unit of a developing country. BMC Pediatrics 2010, 10, 66. [Google Scholar] [CrossRef] [Green Version]
- Montagna, M.T.; Lovero, G.; De Giglio, O.; Iatta, R.; Caggiano, G.; Montagna, O.; Laforgia, N. AURORA Project Group. Invasive fungal infections in Neonatal Intensive Care Units of Southern Italy: A multicentre regional active surveillance (Aurora Project). J. Prev. Med. Hyg. 2010, 51, 125–130. [Google Scholar] [CrossRef]
- De Paula Menezes, R.; Silva, F.F.; Melo, S.; Alves, P.; Brito, M.O.; de Souza Bessa, M.A.; Amante Penatti, M.P.; Pedroso, R.S.; Abdallah, V.; Röder, D. Characterization of Candida species isolated from the hands of the healthcare workers in the neonatal intensive care unit. Med. Mycol. 2018, 57, 588–594. [Google Scholar] [CrossRef]
- Mahieu, L.M.; Van Gasse, N.; Wildemeersch, D.; Jansens, H.; Ieven, M. Number of sites of perinatal Candida colonization and neutropenia are associated with nosocomial candidemia in the neonatal intensive care unit patient. Pediatric Crit. Care Med. 2010, 11, 240–245. [Google Scholar] [CrossRef]
- Ramy, N.; Hashim, M.; Abou Hussein, H.; Sawires, H.; Gaafar, M.; El Maghraby, A. Role of early onset neutropenia in development of candidemia in premature infants. J. Trop. Pediatrics 2018, 64, 51–59. [Google Scholar] [CrossRef]
- Cashen, K.; Reeder, R.; Dalton, H.J.; Berg, R.A.; Shanley, T.P.; Newth, C.; Pollack, M.M.; Wessel, D.; Carcillo, J.; Harrison, R.; et al. Acquired infection during neonatal and pediatric extracorporeal membrane oxygenation. Perfusion 2018, 33, 472–482. [Google Scholar] [CrossRef]
- Manzoni, P.; Farina, D.; Leonessa, M.; Antonielli d’Oulx, E.; Galletto, P.; Mostert, M.; Miniero, R.; Gomirato, G. Risk Factors for Progression to Invasive Fungal Infection in Preterm Neonates With Fungal Colonization. Pediatrics 2006, 118, 2359–2364. [Google Scholar] [CrossRef]
- Kühbacher, A.; Burger-Kentischer, A.; Rupp, S. Interaction of Candida Species with the Skin. Microorganisms 2017, 5, 32. [Google Scholar] [CrossRef] [Green Version]
- Manzoni, P.; Farina, D.; Leonessa, M.; Priolo, C.; Arisio, R.; Gomirato, G. Type and number of sites colonized by fungi and risk of progression to invasive fungal infection in preterm neonates in neonatal intensive care unit. J. Perinat. Med. 2007, 35, 220–226. [Google Scholar] [CrossRef]
- Kaufman, D.A.; Gurka, M.J.; Hazen, K.C.; Boyle, R.; Robinson, M.; Grossman, L.B. Patterns of Fungal Colonization in Preterm Infants Weighing Less Than 1000 Grams at Birth. Pediatric Infect. Dis. J. 2006, 25, 733–737. [Google Scholar] [CrossRef]
- Robinson, J.L.; Davies, H.D.; Barton, M.; O’Brien, K.; Simpson, K.; Asztalos, E.; Synnes, A.; Rubin, E.; Le Saux, N.; Hui, C.; et al. Characteristics and outcome of infants with candiduria in neonatal intensive care—A Paediatric Investigators Collaborative Network on Infections in Canada (PICNIC) study. BMC Infect. Dis. 2009, 9, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Yu, J.C.; Khodadadi, H.; Malik, A.; Davidson, B.; Salles, É.; Bhatia, J.; Hale, V.L.; Baban, B. Innate Immunity of Neonates and Infants. Front. Immunol. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Tsafaras, G.P.; Ntontsi, P.; Xanthou, G. Advantages and Limitations of the Neonatal Immune System. Front. Pediatrics 2020, 8, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Netea, M.G.; Joosten, L.A.; van der Meer, J.W.; Kullberg, B.J.; van de Veerdonk, F.L. Immune defence against Candida fungal infections. Nat. Rev. Immunol. 2015, 15, 630–642. [Google Scholar] [CrossRef] [PubMed]
- Maródi, L.; Johnston, R.B. Invasive Candida species disease in infants and children: Occurrence, risk factors, management, and innate host defense mechanisms. Curr. Opin. Pediatrics 2007, 19, 693–697. [Google Scholar] [CrossRef]
- Maródi, L. Innate cellular immune responses in newborns. Clin. Immunol. 2006, 118, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Naglik, J.R.; König, A.; Hube, B.; Gaffen, S.L. Candida albicans—Epithelial interactions and induction of mucosal innate immunity. Curr. Opin. Microbiol. 2017, 40, 104–112. [Google Scholar] [CrossRef]
- Naglik, J.R.; Gaffen, S.L.; Hube, B. Candidalysin: Discovery and function in Candida albicans infections. Curr. Opin. Microbiol. 2019, 52, 100–109. [Google Scholar] [CrossRef]
- Tong, Y.; Tang, J. Candida albicans infection and intestinal immunity. Microbiol. Res. 2017, 198, 27–35. [Google Scholar] [CrossRef]
- Richardson, J.P.; Moyes, D.L.; Ho, J.; Naglik, J.R. Candida innate immunity at the mucosa. Semin. Cell Dev. Biol. 2018, 89, 58–70. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, D.; Fairchild, K.D. Clinical microbiology of bacterial and fungal sepsis in very-low-birth-weight infants. Clin. Microbiol. Rev. 2004, 17, 638–680. [Google Scholar] [CrossRef] [Green Version]
- Cleveland, A.A.; Farley, M.M.; Harrison, L.H.; Stein, B.; Hollick, R.; Lockhart, S.R.; Magill, S.S.; Derado, G.; Park, B.J.; Chiller, T.M. Changes in Incidence and Antifungal Drug Resistance in Candidemia: Results from Population-Based Laboratory Surveillance in Atlanta and Baltimore, 2008–2011. Clin. Infect. Dis. 2012, 55, 1352–1361. [Google Scholar] [CrossRef]
- Warris, A.; Pana, Z.D.; Oletto, A.; Lundin, R.; Castagnola, E.; Lehrnbecher, T.; Groll, A.H.; Roilides, E.; Andersen, C.T.; Arendrup, M.C.; et al. EUROCANDY study group. Etiology and Outcome of Candidemia in Neonates and Children in Europe: An 11-year Multinational Retrospective Study. Pediatric Infect. Dis J. 2020, 39, 114–120. [Google Scholar] [CrossRef]
- Steinbach, W.J.; Roilides, E.; Berman, D.; Hoffman, J.A.; Groll, A.H.; Bin-Hussain, I.; Palazzi, D.L.; Castagnola, E.; Halasa, N.; Velegraki, A.; et al. International Pediatric Fungal Network. Results from a prospective, international, epidemiologic study of invasive candidiasis in children and neonates. Pediatric Infect. Dis. J. 2012, 31, 1252–1257. [Google Scholar] [CrossRef]
- Hemedez, C.; Trail-Burns, E.; Mao, Q.; Chu, S.; Shaw, S.K.; Bliss, J.M.; De Paepe, M.E. Pathology of Neonatal Non- albicans Candidiasis: Autopsy Study and Literature Review. Pediatric Dev. Patbol. 2019, 22, 98–105. [Google Scholar] [CrossRef]
- Kaufman, D.A. “Getting to Zero”: Preventing invasive Candida infections and eliminating infection-related mortality and morbidity in extremely preterm infants. Early Hum. Dev. 2012, 88 (Suppl. 2), S45–S49. [Google Scholar] [CrossRef]
- Bassetti, M.; Marchetti, M.; Chakrabarti, A.; Colizza, S.; Garnacho-Montero, J.; Kett, D.H.; Munoz, P.; Cristini, F.; Andoniadou, A.; Viale, P.; et al. A research agenda on the management of intra-abdominal candidiasis: Results from a consensus of multinational experts. Intensive Care Med. 2013, 39, 2092–2106. [Google Scholar] [CrossRef]
- Baley, J. Neonatal Candidiasis: The Current Challenge. Clin. Perinatol. 1991, 18, 263–280. [Google Scholar] [CrossRef]
- Baley, J.; Kliegman, R.; Boxerbaum, B.; Fanaroff, A. Fungal Colonization in the Very Low Birth Weight Infant. Pediatrics 1986, 78, 225–232. [Google Scholar]
- Stoll, B.J.; Gordon, T.; Korones, S.B.; Shankaran, S.; Tyson, J.E.; Bauer, C.R.; Fanaroff, A.A.; Lemons, J.A.; Donovan, E.F.; Oh, W.; et al. Late-onset sepsis in very low birth weight neonates: A report from the National Institute of Child Health and Human Development Neonatal Research Network. J. Pediatrics 1996, 129, 63–71. [Google Scholar] [CrossRef]
- Dodds Ashley, E.; Drew, R.; Johnson, M.; Danna, R.; Dabrowski, D.; Walker, V.; Prasad, M.; Alexander, B.; Papadopoulos, G.; Perfect, J. Cost of Invasive Fungal Infections in the Era of New Diagnostics and Expanded Treatment Options. Pharmacotherapy 2012, 32, 890–901. [Google Scholar] [CrossRef]
- Harrington, R.; Kindermann, S.L.; Hou, Q.; Taylor, R.J.; Azie, N.; Horn, D.L. Candidemia and invasive candidiasis among hospitalized neonates and pediatric patients. Curr. Med. Res. Opin. 2017, 33, 1803–1812. [Google Scholar] [CrossRef]
- Schwab, F.; Geffers, C.; Piening, B.; Haller, S.; Eckmanns, T.; Gastmeier, P. How many outbreaks of nosocomial infections occur in German neonatal intensive care units annually? Infection 2014, 42, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Qi, L.; Fan, W.; Xia, X.; Yao, L.; Liu, L.; Zhao, H.; Kong, X.; Liu, J. Nosocomial outbreak of Candida parapsilosis sensu stricto fungaemia in a neonatal intensive care unit in China. J. Hosp. Infect. 2018, 100, e246–e252. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Gu, H.F.; Zhang, H.G.; Chen, S.B.; Wang, J.Q.; Geng, S.X.; Li, L.; Liu, P.; Liu, X.; Ji, Y.R.; et al. An outbreak of Candida parapsilosis fungemia among preterm infants. Genet. Mol. Res. 2015, 14, 18259–18267. [Google Scholar] [CrossRef] [PubMed]
- Asadzadeh, M.; Ahmad, S.; Al-Sweih, N.; Hagen, F.; Meis, J.F.; Khan, Z. High-resolution fingerprinting of Candida parapsilosis isolates suggests persistence and transmission of infections among neonatal intensive care unit patients in Kuwait. Sci. Rep. 2019, 9, 1340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kollef, M.; Micek, S.; Hampton, N.; Doherty, J.A.; Kumar, A. Septic Shock Attributed to Candida Infection: Importance of Empiric Therapy and Source Control. Clin. Infect. Dis. 2012, 54, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Puig-Asensio, M.; Pemán, J.; Zaragoza, R.; Garnacho-Montero, J.; Martín-Mazuelos, E.; Cuenca-Estrella, M.; Almirante, B. Prospective Population Study on Candidemia in Spain (CANDIPOP) Project, Hospital Infection Study Group (GEIH), Medical Mycology Study Group (GEMICOMED) of the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC), & Spanish Network for Research in Infectious Diseases. Impact of therapeutic strategies on the prognosis of candidemia in the ICU. Crit. Care Med. 2014, 42, 1423–1432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaufman, D.; Boyle, R.; Hazen, K.C.; Patrie, J.T.; Robinson, M.; Donowitz, L.G. Fluconazole prophylaxis against fungal colonization and infection in preterm infants. N. Engl. J. Med. 2001, 345, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, P.; Stolfi, I.; Pugni, L.; Decembrino, L.; Magnani, C.; Vetrano, G.; Tridapalli, E.; Corona, G.; Giovannozzi, C.; Farina, D.; et al. Italian Task Force for the Study and Prevention of Neonatal Fungal Infections, & Italian Society of Neonatology. A Multicenter, Randomized Trial of Prophylactic Fluconazole in Preterm Neonates. N. Engl. J. Med. 2007, 356, 2483–2495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Healy, C.M.; Baker, C.J.; Zaccaria, E.; Campbell, J.R. Impact of Fluconazole prophylaxis on incidence and outcome of invasive Candidiasis in a Neonatal Intensive Care Unit. J. Pediatrics 2005, 147, 166–171. [Google Scholar] [CrossRef]
- Clerihew, L.; Austin, N.; McGuire, W. Prophylactic systemic antifungal agents to prevent mortality and morbidity in very low birth weight infants. Cochrane Database Syst. Rev. 2007, 4, CD003850. [Google Scholar] [CrossRef]
- Aliaga, S.; Clark, R.H.; Laughon, M.; Walsh, T.J.; Hope, W.W.; Benjamin, D.K.; Kaufman, D.; Arrieta, A.; Benjamin, D.K., Jr.; Smith, P.B. Changes in the Incidence of Candidiasis in Neonatal Intensive Care Units. Pediatrics 2014, 133, 236–242. [Google Scholar] [CrossRef] [Green Version]
- Adams-Chapman, I.; Bann, C.M.; Das, A.; Ronald, N.; Stoll, B.J.; Walsh, M.C.; Sánchez, P.J.; Higgins, R.D.; Shankaran, S.; Watterberg, K.L.; et al. Eunice Kennedy Shriver National Institutes of Child Health and Human Development Neonatal Research Network. Neurodevelopmental Outcome of Extremely Low Birth Weight Infants with Candida infection. J. Pediatrics 2013, 163, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Donnelly, J.P. New Concepts in Diagnostics for Invasive Mycoses: Non-Culture-Based Methodologies. J. Fungi. 2019, 5, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mylonakis, E.; Clancy, C.J.; Ostrosky-Zeichner, L.; Garey, K.W.; Alangaden, G.J.; Vazquez, J.A.; Groeger, J.S.; Judson, M.A.; Vinagre, Y.M.; Heard, S.O.; et al. T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: A clinical trial. Clin. Infect. Dis. 2015, 60, 892–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamula, C.L.; Hughes, K.; Fisher, B.T.; Zaoutis, T.E.; Singh, I.R.; Velegraki, A. T2Candida Provides Rapid and Accurate Species Identification in Pediatric Cases of Candidemia. Am. J. Clin. Pathol. 2016, 145, 858–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, S.; Wu, T.; Wu, Y.; Ming, D.; Zhu, X. Diagnostic accuracy of Candida albicans germ tube antibody for invasive candidiasis: Systematic review and meta-analysis. Diagn. Microbiol. Infect. Dis. 2019, 93, 339–345. [Google Scholar] [CrossRef]
- Pana, Z.-D.; Kougia, V.; Roilides, E. Therapeutic strategies for invasive fungal infections in neonatal and pediatric patients: An update. Expert Opin. Pharm. 2015, 16, 693–710. [Google Scholar] [CrossRef]
- Bradley, J.S.; Barnett, E.D.; Cantey, J.B. (Eds.) Choosing Among Antifungal Agents: Polyenes, Azoles, and Echinocandins. In Nelson’s Pediatric Antimicrobial Therapy, 25th ed.; Chapter 2; American Academy of Pediatrics: Itasca, IL, USA, 2019. [Google Scholar]
- Scott, B.L.; Hornik, C.D.; Zimmerman, K. Pharmacokinetic, efficacy, and safety considerations for the use of antifungal drugs in the neonatal population. Expert Opin. Drug Metab. Toxicol. 2020, 16, 605–616. [Google Scholar] [CrossRef]
- Saxén, H.; Hoppu, K.; Pohjavuori, M. Pharmacokinetics of fluconazole in very low birth weight infants during the first two weeks of life. Clin. Pharmacol. Ther. 1993, 54, 269–277. [Google Scholar] [CrossRef]
- Larkin, E.L.; Dharmaiah, S.; Ghannoum, M.A. Biofilms and beyond: Expanding echinocandin utility. J. Antimicrob. Chemother. 2018, 73, i73–i81. [Google Scholar] [CrossRef]
- Cateau, E.; Rodier, M.H.; Imbert, C. In vitro efficacies of caspofungin or micafungin catheter lock solutions on Candida albicans biofilm growth. J. Antimicrob. Chemother. 2008, 62, 153–155. [Google Scholar] [CrossRef] [Green Version]
- Katragkou, A.; Roilides, E.; Walsh, T.J. Role of Echinocandins in Fungal Biofilm-Related Disease: Vascular Catheter-Related Infections, Immunomodulation, and Mucosal Surfaces. Clin. Infect. Dis. 2015, 61 (Suppl. 6), S622–S629. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Country and Year [Ref.] | Study Type | Study Period | Inclusion Criteria | Neonates (n) | Preterm (n, %) | Central Line (n, %) | Previous Surger (n, %) | Abdominal Surgery (n, %) | Non Abdominal Surgery (n, %) | In-Hospital Mortality (n, %) | Fungal Mortality (n, %) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| US, 2000 [9] | R, SC | 1981–1999 | ICI | 96 | 83 VLBW (86) | 63 (66) | 3 (12) | NA | NA | 31 (32) | 11 (11) |
| Kuwait, 2000 [10] | R, SC | 1994–1998 | Positive BC | 25 | 9 LBW (36) | NA | 25 (100) | 20 (80) | 5 (20) | 8 (25) | NA |
| US, 2000 [11] | P, MC | 1993–1995 | Positive BC | 35 | 29 VLBW (83) | NA | 13 (37) | NA | NA | 8 (23) | NA |
| Greece, 2004 [12] | P, SC | 1994–2000 | ICI | 59 | NA | NA | 23 (39) | NA | NA | 17 (29) | C. albicans: 15/38 (39); C. parapsilosis: 1/9 (11); others: NA |
| Costa Rica, 2005 [13] | R, SC | 1994–1998 | Positive BC | 110 | 46 (62) | 98 (89) | 79 (72) | 40 (36) | 39 (35) | 37 (34) | 29 (26) |
| US, 2005 [14] | P, MC | 1998–2000 | Positive BC | 35 | 30 VLBW (86) | 23 (66) | 13 (37) | 8 (23) | 5 (14) | 7 (20) | NA |
| Jordan, 2008 [15] | R, SC | 1995–2006 | Positive BC | 24 | 13 (54) | 19 (79) | 10 (42) | 10 (42) | 0 | 13 (54) | 4 (17) |
| Australia, 2009 [16] | P, MC | 2001–2004 | Positive BC | 33 | 33 (94) | 24 (89) | 5 (19) | NA | NA | 7 (22) | NA |
| China, 2013 [17] | R, SC | 2004–2010 | IFI | 45 | 29 VLBW (64) | 32 (71) | NA | 9 (20) | NA | 4 (9) | NA |
| Portugal, 2014 [18] | P, MC | 2005–2010 | IFI | 44 | 37 (84) | 44 (100) | 14 (32) | NA | NA | 5 (11) | 5 (11) |
| England, 2014 [19] | R and P, MC | R: 2004–2009; P: 2010 | IFI | 84 | 79 (94) | 71 (87) | NA | 11 (13) | NA | 26 (31) | 18 (21) |
| China, 2015 [20] | R, SC | 2006–2010 | Positive BC | 19 | NA | 16 (84) | NA | 9 (47) | NA | 3 (16) | NA |
| Italy, 2016 [21] | P, MC | 2005–2015 | ICI | 14 | 12 LBW (85) | NA | 2 (14) | 2 (14) | 0 | NA for neonates with ICI | NA for neonates with ICI |
| US, 2018 [22] | P, MC | 2008–2015 | Positive BC | 90 | 46 (78) | 70 (78) | 8 (9) | 2 (2) | 7 (7) | 14 (16) | NA |
| Iran, 2018 [23] | P, SC | 2014–2016 | Positive BC | 35 | 17 (49) | 33 (94) | 14 (40) | 10 (29) | 4 (11) | 15 (43) | NA for neonates with ICI |
| Germany, 2018 [24] | P, MC | 2009–2015 | Need for antifungal treatment | 724 | 724 (100) | 652 (90) | NA | 272 (38) | NA | 71 (10) | NA |
| Taiwan, 2018 [25] | R, SC | 2004–2015 | ICI | 113 | NA | 108 (96) | 31 (27) | NA | NA | 48 (43) | 32 (28) |
| Turkey, 2019 [26] | R, SC | 2007–2012 | ICI | 22 | 20 | 3 (6) | 5 (17) | NA | NA | 10 (46) | NA |
| France, 2019 [27] | P, MC | 2010–2012 | IFI treated with micafungin | 31 | 29 (97) | NA | NA | 4 (4) | NA | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Rose, D.U.; Santisi, A.; Ronchetti, M.P.; Martini, L.; Serafini, L.; Betta, P.; Maino, M.; Cavigioli, F.; Cocchi, I.; Pugni, L.; et al. Invasive Candida Infections in Neonates after Major Surgery: Current Evidence and New Directions. Pathogens 2021, 10, 319. https://doi.org/10.3390/pathogens10030319
De Rose DU, Santisi A, Ronchetti MP, Martini L, Serafini L, Betta P, Maino M, Cavigioli F, Cocchi I, Pugni L, et al. Invasive Candida Infections in Neonates after Major Surgery: Current Evidence and New Directions. Pathogens. 2021; 10(3):319. https://doi.org/10.3390/pathogens10030319
Chicago/Turabian StyleDe Rose, Domenico Umberto, Alessandra Santisi, Maria Paola Ronchetti, Ludovica Martini, Lisa Serafini, Pasqua Betta, Marzia Maino, Francesco Cavigioli, Ilaria Cocchi, Lorenza Pugni, and et al. 2021. "Invasive Candida Infections in Neonates after Major Surgery: Current Evidence and New Directions" Pathogens 10, no. 3: 319. https://doi.org/10.3390/pathogens10030319






