Mutations in Animal SARS-CoV-2 Induce Mismatches with the Diagnostic PCR Assays
Abstract
:1. Introduction
2. Materials and Methods
2.1. Selection of SARS-CoV-2 Genomes
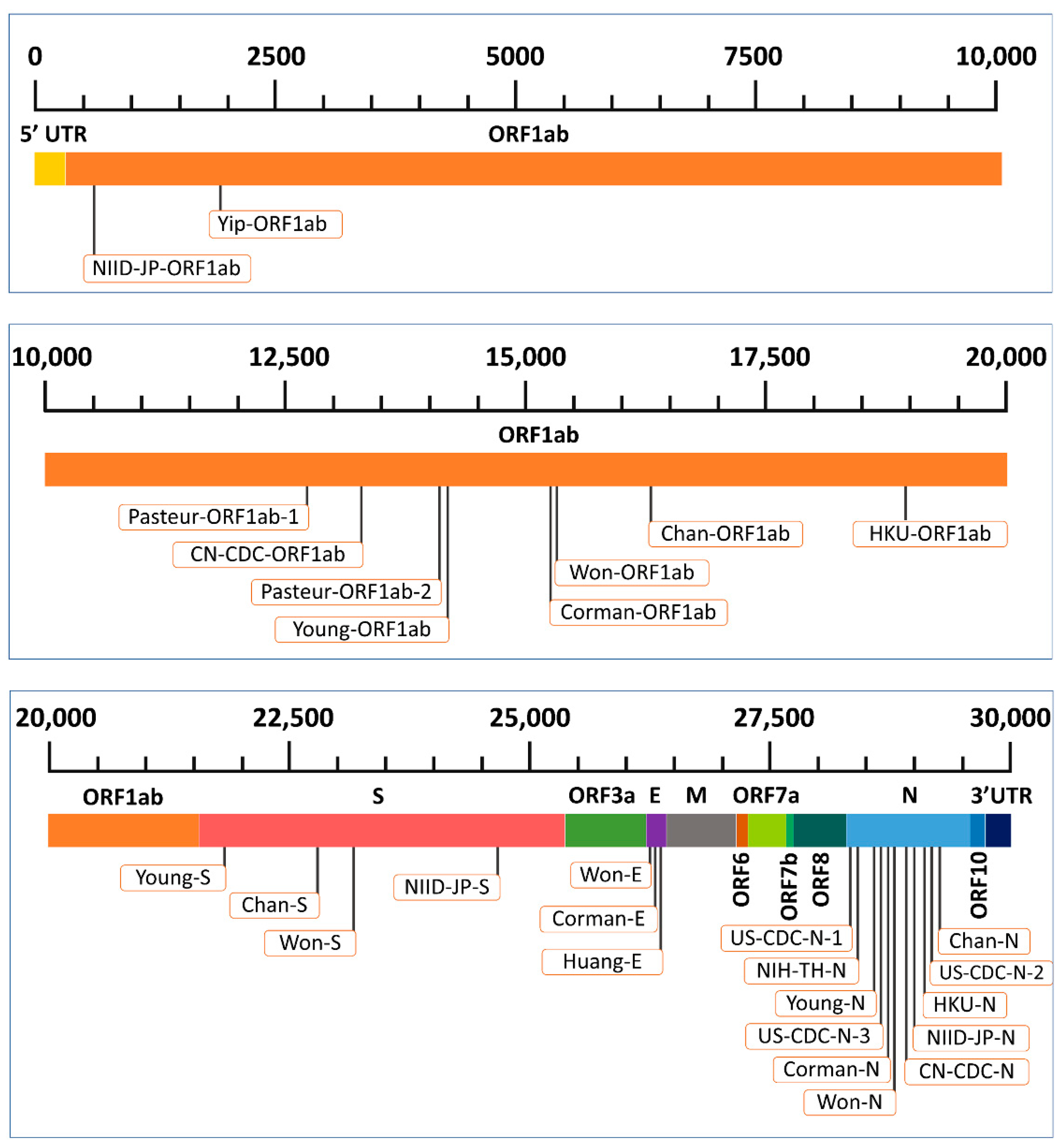
2.2. Selection of Diagnostic PCR Assays
2.3. Multiple-Sequence Alignment
2.4. Identification of Nucleotide Changes at the Primer-Probe Binding Sites
3. Results
3.1. Mismatches in Diagnostic PCR Assays Targeting the ORF1ab Gene

3.2. Mismatches in Diagnostic PCR Assays Targeting the S Gene
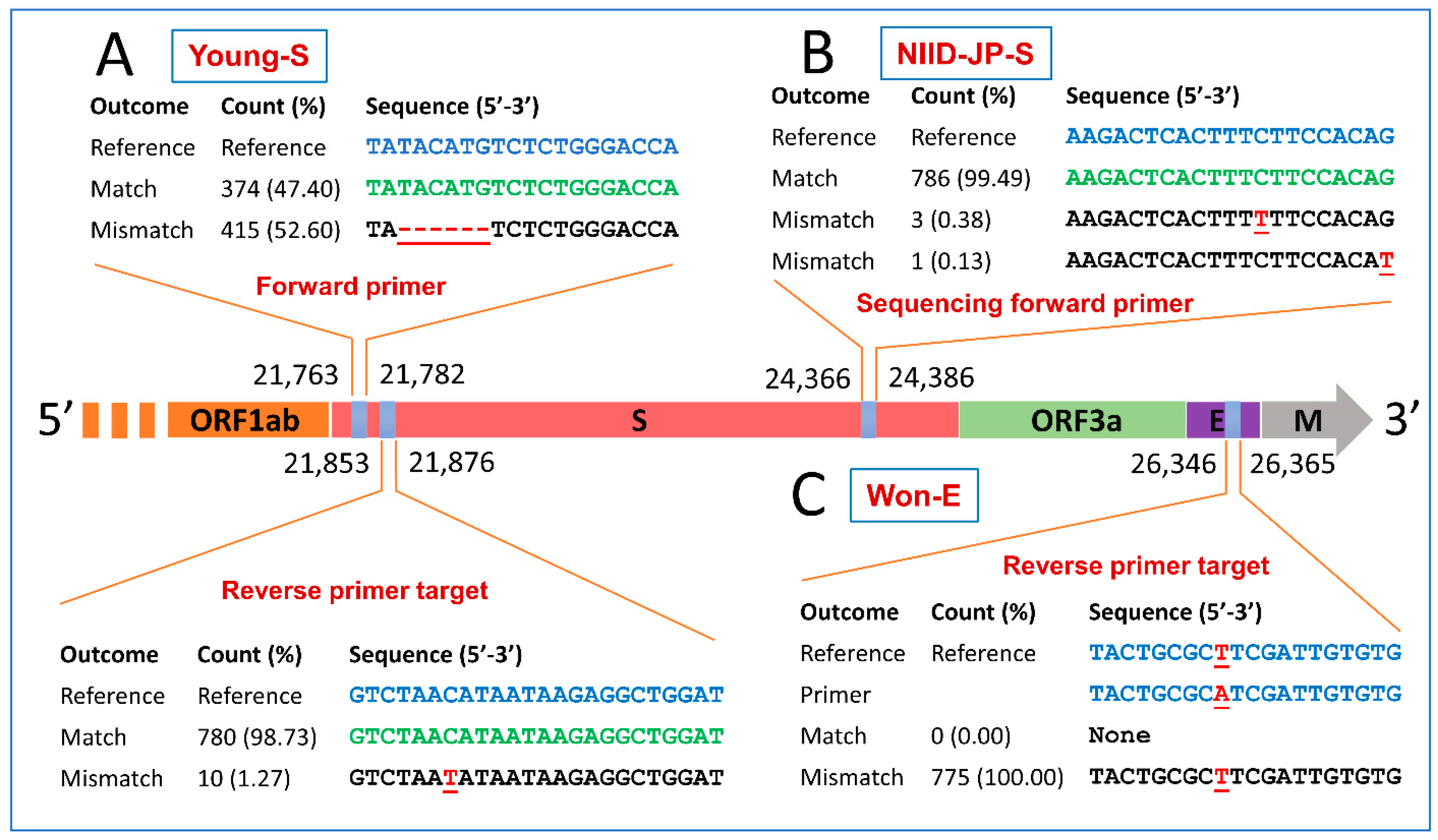
3.3. Mismatches in Diagnostic PCR Assays Targeting the E Gene
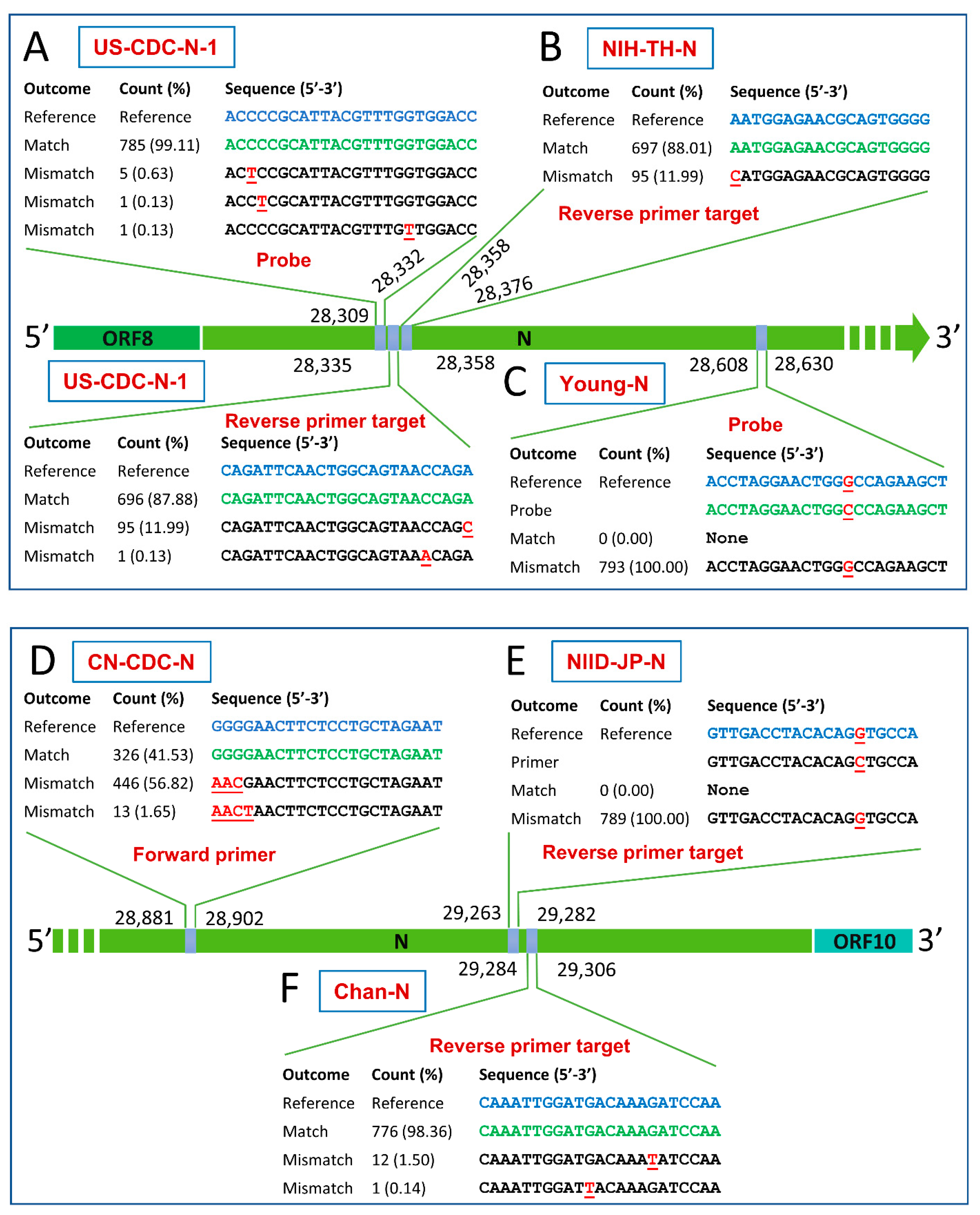
3.4. Mismatches in Diagnostic PCR Assays Targeting the N Gene
3.5. Suggested Modifications of Primer-Probe Sets
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [Green Version]
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef] [Green Version]
- Tazerji, S.S.; Duarte, P.M.; Rahimi, P.; Shahabinejad, F.; Dhakal, S.; Malik, Y.S.; Shehata, A.A.; Lama, J.; Klein, J.; Safdar, M. Transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to animals: An updated review. J. Transl. Med. 2020, 18, 358. [Google Scholar] [CrossRef]
- Chan, J.F.-W.; Kok, K.-H.; Zhu, Z.; Chu, H.; To, K.K.-W.; Yuan, S.; Yuen, K.-Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes & Infect. 2020, 9, 221–236. [Google Scholar] [CrossRef] [Green Version]
- Helmy, Y.A.; Fawzy, M.; Elaswad, A.; Sobieh, A.; Kenney, S.P.; Shehata, A.A. The COVID-19 pandemic: A comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. J. Clin. Med. 2020, 9, 1225. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, S.; Carrà, G.; Bottino, P.; Zanotto, E.; De Santis, M.C.; Margaria, J.P.; Giorgio, A.; Mandili, G.; Martini, M.; Cavallo, R. A novel multiplex qRT-PCR assay to detect SARS-CoV-2 infection: High sensitivity and increased testing capacity. Microorganisms 2020, 8, 1064. [Google Scholar] [CrossRef]
- Falzone, L.; Musso, N.; Gattuso, G.; Bongiorno, D.; Palermo, C.I.; Scalia, G.; Libra, M.; Stefani, S. Sensitivity assessment of droplet digital PCR for SARS-CoV-2 detection. Int. J. Mol. Med. 2020, 46, 957–964. [Google Scholar] [CrossRef] [PubMed]
- CDC. Research Use Only 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Primers and Probes. Available online: https://www.cdc.gov/coronavirus/2019-ncov/lab/rt-pcr-panel-primer-probes.html (accessed on 20 January 2020).
- Chan, J.F.-W.; Yip, C.C.-Y.; To, K.K.-W.; Tang, T.H.-C.; Wong, S.C.-Y.; Leung, K.-H.; Fung, A.Y.-F.; Ng, A.C.-K.; Zou, Z.; Tsoi, H.-W. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-PCR assay validated in vitro and with clinical specimens. J. Clin. Microbiol. 2020, 58, e00310-20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, D.K.; Pan, Y.; Cheng, S.M.; Hui, K.P.; Krishnan, P.; Liu, Y.; Ng, D.Y.; Wan, C.K.; Yang, P.; Wang, Q. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin. Chem. 2020, 66, 549–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.; Bleicker, T.; Brünink, S.; Schneider, J.; Schmidt, M.L. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro. Surveill. 2020, 25, 2000045. [Google Scholar] [CrossRef] [Green Version]
- Niu, P.; Lu, R.; Zhao, L.; Wang, H.; Huang, B.; Ye, F.; Wang, W.; Tan, W. Three novel real-time RT-PCR assays for detection of COVID-19 virus. China CDC Weekly 2020, 2, 453–457. [Google Scholar] [CrossRef]
- Shirato, K.; Nao, N.; Katano, H.; Takayama, I.; Saito, S.; Kato, F.; Katoh, H.; Sakata, M.; Nakatsu, Y.; Mori, Y. Development of genetic diagnostic methods for novel coronavirus 2019 (nCoV-2019) in Japan. Jpn. J. Infect. Dis. 2020, 73, 304–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Molecular Assays to Diagnose COVID-19: Summary Table of Available Protocols. Available online: https://www.who.int/publications/m/item/molecular-assays-to-diagnose-covid-19-summary-table-of-available-protocols (accessed on 20 January 2021).
- Won, J.; Lee, S.; Park, M.; Kim, T.Y.; Park, M.G.; Choi, B.Y.; Kim, D.; Chang, H.; Kim, V.N.; Lee, C.J. Development of a laboratory-safe and low-cost detection protocol for SARS-CoV-2 of the coronavirus disease 2019 (COVID-19). Exp. Neurobiol. 2020, 29, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.C.-Y.; Ho, C.-C.; Chan, J.F.-W.; To, K.K.-W.; Chan, H.S.-Y.; Wong, S.C.-Y.; Leung, K.-H.; Fung, A.Y.-F.; Ng, A.C.-K.; Zou, Z. Development of a novel, genome subtraction-derived, SARS-CoV-2-specific COVID-19-nsp2 real-time RT-PCR assay and its evaluation using clinical specimens. Int. J. Mol. Sci. 2020, 21, 2574. [Google Scholar] [CrossRef] [Green Version]
- Young, B.E.; Ong, S.W.X.; Kalimuddin, S.; Low, J.G.; Tan, S.Y.; Loh, J.; Ng, O.-T.; Marimuthu, K.; Ang, L.W.; Mak, T.M. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 2020, 323, 1488–1494. [Google Scholar] [CrossRef] [Green Version]
- Khan, K.A.; Cheung, P. Presence of mismatches between diagnostic PCR assays and coronavirus SARS-CoV-2 genome. R. Soc. Open Sci. 2020, 7, 200636. [Google Scholar] [CrossRef]
- Lippi, G.; Simundic, A.-M.; Plebani, M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19). Clin. Chem. Lab. Med. 2020, 58, 1070–1076. [Google Scholar] [CrossRef] [Green Version]
- Li, D.; Zhang, J.; Li, J. Primer design for quantitative real-time PCR for the emerging Coronavirus SARS-CoV-2. Theranostics 2020, 10, 7150. [Google Scholar] [CrossRef]
- Wernike, K.; Keller, M.; Conraths, F.J.; Mettenleiter, T.C.; Groschup, M.H.; Beer, M. Pitfalls in SARS-CoV-2 PCR diagnostics. Transbound. Emerg. Dis. 2020. [Google Scholar] [CrossRef]
- Suo, T.; Liu, X.; Feng, J.; Guo, M.; Hu, W.; Guo, D.; Ullah, H.; Yang, Y.; Zhang, Q.; Wang, X. ddPCR: A more accurate tool for SARS-CoV-2 detection in low viral load specimens. Emerg. Microbes & Infect. 2020, 9, 1259–1268. [Google Scholar] [CrossRef]
- Mitsuhashi, M. Technical report: Part 1. Basic requirements for designing optimal oligonucleotide probe sequences. J. Clin. Lab. Anal. 1996, 10, 277–284. [Google Scholar] [CrossRef]
- Gribble, J.; Stevens, L.J.; Agostini, M.L.; Anderson-Daniels, J.; Chappell, J.D.; Lu, X.; Pruijssers, A.J.; Routh, A.L.; Denison, M. The coronavirus proofreading exoribonuclease mediates extensive viral recombination. PLoS Pathog. 2021, 17, e1009226. [Google Scholar] [CrossRef] [PubMed]
- Elaswad, A.; Fawzy, M.; Basiouni, S.; Shehata, A. Mutational spectra of SARS-CoV-2 isolated from animals. PeerJ 2020, 8, e10609. [Google Scholar] [CrossRef]
- Ogando, N.S.; Ferron, F.; Decroly, E.; Canard, B.; Posthuma, C.C.; Snijder, E.J. The curious case of the nidovirus exoribonuclease: Its role in RNA synthesis and replication fidelity. Front. Microbiol. 2019, 10, 1813. [Google Scholar] [CrossRef]
- Warton, K.; Xu, Y.; Ford, C.E. Target sequence heterogeneity causes the ‘hook effect’in fluorescent dye-based quantitative PCR. BioTechniques 2020, 69, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Vogels, C.B.; Brito, A.F.; Wyllie, A.L.; Fauver, J.R.; Ott, I.M.; Kalinich, C.C.; Petrone, M.E.; Casanovas-Massana, A.; Muenker, M.C.; Moore, A. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT–qPCR primer–probe sets. Nat. Microbiol. 2020, 5, 1299–1305. [Google Scholar] [CrossRef] [PubMed]
- Koo, C.; Kaur, S.; Teh, Z.-Y.; Xu, H.; Nasir, A.; Lai, Y.-L.; Khan, E.; Ng, L.-C.; Hapuarachchi, H. Genetic variability in probe binding regions explains false negative results of a molecular assay for the detection of dengue virus. Vector Borne Zoonotic Dis. 2016, 16, 489–495. [Google Scholar] [CrossRef]
- Abdel-Maksoud, N.H.; El-Shamy, A.; Fawzy, M.; Gomaa, H.; Eltarabilli, M. Hepatitis B variants among Egyptian patients undergoing hemodialysis. Microbiol. Immunol. 2019, 63, 77–84. [Google Scholar] [CrossRef]
- Chow, C.-K.; Qin, K.; Lau, L.-T.; Yu, A.C.-H. Significance of a single-nucleotide primer mismatch in hepatitis B virus real-time PCR diagnostic assays. J. Clin. Microbiol. 2011, 49, 4418–4419. [Google Scholar] [CrossRef] [Green Version]
- Christopherson, C.; Sninsky, J.; Kwok, S. The effects of internal primer-template mismatches on RT-PCR: HIV-1 model studies. Nucleic Acids Res. 1997, 25, 654–658. [Google Scholar] [CrossRef] [Green Version]
- Mai, P.H.V.; Hong, T.U.T.; Le Khanh, H.N.; Thanh, T.N.; Le Thi, T.; Vu, S.N.; Phuong, A.N.; Thu, H.T.T.; Duc, C.V.; Le Quynh, M. Missed detections of influenza A (H1) pdm09 by real-time RT–PCR assay due to haemagglutinin sequence mutation, December 2017 to March 2018, northern Viet Nam. Western Pac. Surveill. Response J. 2019, 10, 32–38. [Google Scholar] [CrossRef]
- Hughes, G.; Smith, J.; Hanlon, C.; Rupprecht, C. Evaluation of a TaqMan PCR assay to detect rabies virus RNA: Influence of sequence variation and application to quantification of viral loads. J. Clin. Microbiol. 2004, 42, 299–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamau, E.; Agoti, C.N.; Lewa, C.S.; Oketch, J.; Owor, B.E.; Otieno, G.P.; Bett, A.; Cane, P.A.; Nokes, D.J. Recent sequence variation in probe binding site affected detection of respiratory syncytial virus group B by real-time RT-PCR. J. Clin. Virol. 2017, 88, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Wen, Z.; Zhong, G.; Yang, H.; Wang, C.; Huang, B.; Liu, R.; He, X.; Shuai, L.; Sun, Z. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science 2020, 368, 1016–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sit, T.H.; Brackman, C.J.; Ip, S.M.; Tam, K.W.; Law, P.Y.; To, E.M.; Veronica, Y.; Sims, L.D.; Tsang, D.N.; Chu, D.K. Infection of dogs with SARS-CoV-2. Nature 2020, 586, 776–778. [Google Scholar] [CrossRef] [PubMed]
- Hamer, S.A.; Pauvolid-Corrêa, A.; Zecca, I.B.; Davila, E.; Auckland, L.D.; Roundy, C.M.; Tang, W.; Torchetti, M.; Killian, M.L.; Jenkins-Moore, M. Natural SARS-CoV-2 infections, including virus isolation, among serially tested cats and dogs in households with confirmed human COVID-19 cases in Texas, USA. bioRxiv 2020. [Google Scholar] [CrossRef]
- Neira, V.; Brito, B.; Agüero, B.; Berrios, F.; Valdés, V.; Gutierrez, A.; Ariyama, N.; Espinoza, P.; Retamal, P.; Holmes, E. A household case evidences shorter shedding of SARS-CoV-2 in naturally infected cats compared to their human owners. Emerg. Microbes & Infect. 2020, 10, 376–383. [Google Scholar] [CrossRef]
- Newman, A.; Smith, D.; Ghai, R.R.; Wallace, R.M.; Torchetti, M.K.; Loiacono, C.; Murrell, L.S.; Carpenter, A.; Moroff, S.; Rooney, J.A. First reported cases of SARS-CoV-2 infection in companion animals—New York, March–April 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Sailleau, C.; Dumarest, M.; Vanhomwegen, J.; Delaplace, M.; Caro, V.; Kwasiborski, A.; Hourdel, V.; Chevaillier, P.; Barbarino, A.; Comtet, L. First detection and genome sequencing of SARS-CoV-2 in an infected cat in France. Transbound. Emerg. Dis. 2020, 67, 2324–2328. [Google Scholar] [CrossRef]
- Segalés, J.; Puig, M.; Rodon, J.; Avila-Nieto, C.; Carrillo, J.; Cantero, G.; Terrón, M.T.; Cruz, S.; Parera, M.; Noguera-Julián, M. Detection of SARS-CoV-2 in a cat owned by a COVID-19− affected patient in Spain. Proc. Natl. Acad. Sci. USA. 2020, 117, 24790–24793. [Google Scholar] [CrossRef] [PubMed]
- McAloose, D.; Laverack, M.; Wang, L.; Killian, M.L.; Caserta, L.C.; Yuan, F.; Mitchell, P.K.; Queen, K.; Mauldin, M.R.; Cronk, B.D. From people to Panthera: Natural SARS-CoV-2 infection in tigers and lions at the Bronx Zoo. mBio 2020, 11, e02220-20. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.C.-Y.; Zhang, A.J.; Chan, J.F.-W.; Li, C.; Fan, Z.; Liu, F.; Chen, Y.; Liang, R.; Sridhar, S.; Cai, J.-P. Oral SARS-CoV-2 inoculation establishes subclinical respiratory infection with virus shedding in golden Syrian hamsters. Cell Rep. Med. 2020, 1, 100121. [Google Scholar] [CrossRef] [PubMed]
- Molenaar, R.J.; Vreman, S.; Hakze-van der Honing, R.W.; Zwart, R.; de Rond, J.; Weesendorp, E.; Smit, L.A.; Koopmans, M.; Bouwstra, R.; Stegeman, A. Clinical and pathological findings in SARS-CoV-2 disease outbreaks in farmed mink (Neovison vison). Vet. Pathol. 2020, 57, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Munnink, B.B.O.; Sikkema, R.S.; Nieuwenhuijse, D.F.; Molenaar, R.J.; Munger, E.; Molenkamp, R.; Van Der Spek, A.; Tolsma, P.; Rietveld, A.; Brouwer, M. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science 2021, 371, 172–177. [Google Scholar] [CrossRef]
- Oreshkova, N.; Molenaar, R.J.; Vreman, S.; Harders, F.; Munnink, B.B.O.; Hakze-van Der Honing, R.W.; Gerhards, N.; Tolsma, P.; Bouwstra, R.; Sikkema, R. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Euro. Surveill. 2020, 25, 2001005. [Google Scholar] [CrossRef]
- Parrish, C.R.; Holmes, E.C.; Morens, D.M.; Park, E.-C.; Burke, D.S.; Calisher, C.H.; Laughlin, C.A.; Saif, L.J.; Daszak, P. Cross-species virus transmission and the emergence of new epidemic diseases. Microbiol. Mol. Biol. Rev. 2008, 72, 457–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edgar, R.C. MUSCLE: A multiple sequence alignment method with reduced time and space complexity. BMC Bioinformatics 2004, 5, 113. [Google Scholar] [CrossRef] [Green Version]
- Larsson, A. AliView: A fast and lightweight alignment viewer and editor for large datasets. Bioinformatics 2014, 30, 3276–3278. [Google Scholar] [CrossRef] [PubMed]
- Sanjuán, R.; Domingo-Calap, P. Mechanisms of viral mutation. Cell. Mol. Life Sci. 2016, 73, 4433–4448. [Google Scholar] [CrossRef] [Green Version]
- Callaway, E. The coronavirus is mutating-does it matter? Nature 2020, 585, 174–177. [Google Scholar] [CrossRef]
- Velazquez-Salinas, L.; Zarate, S.; Eberl, S.; Gladue, D.P.; Novella, I.; Borca, M. Positive selection of ORF1ab, ORF3a, and ORF8 genes drives the early evolutionary trends of SARS-CoV-2 during the 2020 COVID-19 pandemic. Front. Microbiol. 2020, 11, 550674. [Google Scholar] [CrossRef]
- Lefever, S.; Pattyn, F.; Hellemans, J.; Vandesompele, J. Single-nucleotide polymorphisms and other mismatches reduce performance of quantitative PCR assays. Clin. Chem. 2013, 59, 1470–1480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stadhouders, R.; Pas, S.D.; Anber, J.; Voermans, J.; Mes, T.H.; Schutten, M. The effect of primer-template mismatches on the detection and quantification of nucleic acids using the 5′ nuclease assay. J. Mol. Diagn. 2010, 12, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Whiley, D.M.; Sloots, T.P. Sequence variation in primer targets affects the accuracy of viral quantitative PCR. J. Clin. Virol. 2005, 34, 104–107. [Google Scholar] [CrossRef]
- Brault, A.; Fang, Y.; Dannen, M.; Anishchenko, M.; Reisen, W. A naturally occurring mutation within the probe-binding region compromises a molecular-based West Nile virus surveillance assay for mosquito pools (Diptera: Culicidae). J. Med. Entomol. 2012, 49, 939–941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garson, J.; Ferns, R.B.; Grant, P.R.; Ijaz, S.; Nastouli, E.; Szypulska, R.; Tedder, R. Minor groove binder modification of widely used TaqMan probe for hepatitis E virus reduces risk of false negative real-time PCR results. J. Virol. Methods 2012, 186, 157–160. [Google Scholar] [CrossRef]
- Dramé, M.; Tabue Teguo, M.; Proye, E.; Hequet, F.; Hentzien, M.; Kanagaratnam, L.; Godaert, L. Should RT-PCR be considered a gold standard in the diagnosis of Covid-19? J. Med. Virol. 2020, 92, 2312–2313. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Montori, V.M.; Sampathkumar, P. COVID-19 testing: The threat of false-negative results. Mayo Clin. Proc. 2020, 95, 1127–1129. [Google Scholar] [CrossRef] [PubMed]
- Paraskevis, D.; Kostaki, E.G.; Magiorkinis, G.; Panayiotakopoulos, G.; Sourvinos, G.; Tsiodras, S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect. Genet. Evol. 2020, 79, 104212. [Google Scholar] [CrossRef]
- Presti, A.L.; Rezza, G.; Stefanelli, P. Selective pressure on SARS-CoV-2 protein coding genes and glycosylation site prediction. Heliyon 2020, 6, e05001. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020, 181, 271–280.e278. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, H.; Pyrc, K.; Van Der Hoek, L.; Geier, M.; Berkhout, B.; Pöhlmann, S. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proc. Natl. Acad. Sci. USA 2005, 102, 7988–7993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berrio, A.; Gartner, V.; Wray, G. Positive selection within the genomes of SARS-CoV-2 and other Coronaviruses independent of impact on protein function. PeerJ 2020, 8, e10234. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Dong, W.; Milewska, A.; Golda, A.; Qi, Y.; Zhu, Q.K.; Marasco, W.A.; Baric, R.S.; Sims, A.C.; Pyrc, K. Human coronavirus HKU1 spike protein uses O-acetylated sialic acid as an attachment receptor determinant and employs hemagglutinin-esterase protein as a receptor-destroying enzyme. J. Virol. 2015, 89, 7202–7213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damas, J.; Hughes, G.M.; Keough, K.C.; Painter, C.A.; Persky, N.S.; Corbo, M.; Hiller, M.; Koepfli, K.-P.; Pfenning, A.R.; Zhao, H. Broad host range of SARS-CoV-2 predicted by comparative and structural analysis of ACE2 in vertebrates. Proc. Natl. Acad. Sci. USA 2020, 117, 22311–22322. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Chen, D.; Szabla, R.; Zheng, M.; Li, G.; Du, P.; Zheng, S.; Li, X.; Song, C.; Li, R. Broad and differential animal angiotensin-converting enzyme 2 receptor usage by SARS-CoV-2. J. Virol. 2020, 94, e00940-20. [Google Scholar] [CrossRef]
| Continent | Country | Host Species | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| American Mink | Cat | Dog | European Mink | Golden Hamster | Lion | Mouse | Tiger | Total | ||
| Asia | China | - | - | - | - | - | - | 1 | - | 1 |
| Hong Kong | - | 1 | 2 | - | 5 | - | - | - | 8 | |
| Europe | Belgium | - | 1 | - | - | - | - | - | - | 1 |
| Denmark | 454 | 3 | - | - | - | - | - | - | 457 | |
| England | - | 1 | - | - | - | - | - | - | 1 | |
| France | - | 3 | - | - | - | - | - | - | 3 | |
| Greece | - | 1 | - | - | - | - | - | - | 1 | |
| Italy | - | - | 1 | - | - | - | - | - | 1 | |
| Netherlands | 270 | 1 | 1 | 13 | - | - | - | - | 285 | |
| Poland | 12 | - | - | - | - | - | - | - | 12 | |
| Spain | - | 1 | - | - | - | - | - | - | 1 | |
| North America | Canada | 4 | - | - | - | - | - | - | - | 4 |
| USA | - | 3 | 1 | - | - | 4 | - | 6 | 14 | |
| South America | Chile | - | 4 | - | - | - | - | - | - | 4 |
| Total | Total | 740 | 19 | 5 | 13 | 5 | 4 | 1 | 6 | 793 |
| Assay | Country | Oligo | Sequence (5’-3’) | Genome Position | Reference |
|---|---|---|---|---|---|
| ORF1ab | |||||
| NIID-JP-ORF1ab | Japan | F1 | TTCGGATGCTCGAACTGCACC | 484–504 | [14,15] |
| F2 | CTCGAACTGCACCTCATGG | 492–510 | |||
| R1 | CTTTACCAGCACGTGCTAGAAGG | 896–874 | |||
| R2 | CAGAAGTTGTTATCGACATAGC | 837–816 | |||
| FS | ACCTCATGGTCATGTTATGG | 502–521 | |||
| RS | GACATAGCGAGTGTATGCC | 823–805 | |||
| Yip-ORF1ab | China | F | ATGCATTTGCATCAGAGGCT | 1866–1885 | [17] |
| R | TTGTTATAGCGGCCTTCTGT | 1970–1951 | |||
| Pasteur-ORF1ab-1 | France | F | ATGAGCTTAGTCCTGTTG | 12,690–12,707 | [15] |
| P | AGATGTCTTGTGCTGCCGGTA | 12,717–12,737 | |||
| R | CTCCCTTTGTTGTGTTGT | 12,797–12,780 | |||
| CN-CDC-ORF1ab | China | F | CCCTGTGGGTTTTACACTTAA | 13,342–13,362 | [13,15] |
| P | CCGTCTGCGGTATGTGGAAAGGTTATGG | 13,377–13,404 | |||
| R | ACGATTGTGCATCAGCTGA | 13,460–13,442 | |||
| Pasteur-ORF1ab-2 | France | F | GGTAACTGGTATGATTTCG | 14,080–14,098 | [15] |
| P | TCATACAAACCACGCCAGG | 14,123–14,105 | |||
| R | CTGGTCAAGGTTAATATAGG | 14,186–14,167 | |||
| Young-ORF1ab | Singapore | F | TCATTGTTAATGCCTATATTAACC | 14,155–14,178 | [18] |
| P | AACTGCAGAGTCACATGTTGACA | 14,193–14,215 | |||
| R | CACTTAATGTAAGGCTTTGTTAAG | 14,243–14,220 | |||
| Corman-ORF1ab | Germany | F | GTGARATGGTCATGTGTGGCGG | 15,431–15,452 | [12] |
| P1 | CAGGTGGAACCTCATCAGGAGATGC | 15,470–15,494 | |||
| P2 | CCAGGTGGWACRTCATCMGGTGATGC | 15,469–15,494 | |||
| R | CARATGTTAAASACACTATTAGCATA | 15,530–15,505 | |||
| Won-ORF1ab | South Korea | F | CATGTGTGGCGGTTCACTAT | 15,441–15,460 | [16] |
| R | TGCATTAACATTGGCCGTGA | 15,558–15,539 | |||
| Chan-ORF1ab | China | F | CGCATACAGTCTTRCAGGCT | 16,220–16,239 | [10] |
| P | TTAAGATGTGGTGCTTGCATACGTAGAC | 16,272–16,303 | |||
| R | GTGTGATGTTGAWATGACATGGTC | 16,353–16,330 | |||
| HKU-ORF1ab | Hong Kong | F | TGGGGYTTTACRGGTAACCT | 18,778–18,797 | [11,15] |
| P | TAGTTGTGATGCWATCATGACTAG | 18,849–18,872 | |||
| R | AACRCGCTTAACAAAGCACTC | 18,909–18,889 | |||
| S | |||||
| Young-S | Singapore | F | TATACATGTCTCTGGGACCA | 21,763–21,782 | [18] |
| P | CTAAGAGGTTTGATAACCCTGTCCTACC | 21,789–21,816 | |||
| R | ATCCAGCCTCTTATTATGTTAGAC | 21,876–21,853 | |||
| Chan-S | China | F | CCTACTAAATTAAATGATCTCTGCTTTACT | 22,712–22,741 | [10] |
| P | CGCTCCAGGGCAAACTGGAAAG | 22,792–22,813 | |||
| R | CAAGCTATAACGCAGCCTGTA | 22,869–22,849 | |||
| Won-S | South Korea | F | CTACATGCACCAGCAACTGT | 23,114–23,133 | [16] |
| R | CACCTGTGCCTGTTAAACCA | 23,213–23,194 | |||
| NIID-JP-S | Japan | F1 | TTGGCAAAATTCAAGACTCACTTT | 24,354–24,377 | [14,15] |
| F2 | TCAAGACTCACTTTCTTCCAC | 24,364–24,384 | |||
| R1 | TGTGGTTCATAAAAATTCCTTTGTG | 24,900–24,876 | |||
| R2 | ATTTGAAACAAAGACACCTTCAC | 24,856–24,834 | |||
| FS | AAGACTCACTTTCTTCCACAG | 24,366–24,386 | |||
| RS | CAAAGACACCTTCACGAGG | 24,848–24,830 | |||
| E | |||||
| Won-E | South Korea | F | TTCGGAAGAGACAGGTACGTT | 26,259–26,279 | [16] |
| R | CACACAATCGATGCGCAGTA | 26,365–26,346 | |||
| Corman-E | Germany | F | ACAGGTACGTTAATAGTTAATAGCGT | 26,269–26,294 | [12] |
| P | ACACTAGCCATCCTTACTGCGCTTCG | 26,332–26,357 | |||
| R | ATATTGCAGCAGTACGCACACA | 26,381–26,360 | |||
| Huang-E | China | F | ACTTCTTTTTCTTGCTTTCGTGGT | 26,295–26,318 | [1] |
| P | CTAGTTACACTAGCCATCCTTACTGC | 26,326–26,351 | |||
| R | GCAGCAGTACGCACACAATC | 26,376–26,357 | |||
| N | |||||
| US-CDC-N-1 | United States | F | GACCCCAAAATCAGCGAAAT | 28,287–28,306 | [9,15] |
| P | ACCCCGCATTACGTTTGGTGGACC | 28,309–28,332 | |||
| R | TCTGGTTACTGCCAGTTGAATCTG | 28,358–28,335 | |||
| NIH-TH-N | Thailand | F | CGTTTGGTGGACCCTCAGAT | 28,320–28,339 | [15] |
| P | CAACTGGCAGTAACCA | 28,341–28,356 | |||
| R | CCCCACTGCGTTCTCCATT | 28,376–28,358 | |||
| Young-N | Singapore | F | CTCAGTCCAAGATGGTATTTCT | 28,583–28,604 | [18] |
| P | ACCTAGGAACTGGCCCAGAAGCT | 28,608–28,630 | |||
| R | AGCACCATAGGGAAGTCC | 28,648–28,631 | |||
| US-CDC-N-3 | United States | F | GGGAGCCTTGAATACACCAAAA | 28,681–28,702 | [9,15] |
| P | AYCACATTGGCACCCGCAATCCTG | 28,704–28,727 | |||
| R | TGTAGCACGATTGCAGCATTG | 28,752–28,732 | |||
| Corman-N | Germany | F | CACATTGGCACCCGCAATC | 28,706–28,724 | [12] |
| P | ACTTCCTCAAGGAACAACATTGCCA | 28,753–28,777 | |||
| R | GAGGAACGAGAAGAGGCTTG | 28,833–28,814 | |||
| Won-N | South Korea | F | CAATGCTGCAATCGTGCTAC | 28,732–28,751 | [16] |
| R | GTTGCGACTACGTGATGAGG | 28,849–28,830 | |||
| CN-CDC-N | China | F | GGGGAACTTCTCCTGCTAGAAT | 28,881–28,902 | [13,15] |
| P | TTGCTGCTGCTTGACAGATT | 28,934–28,953 | |||
| R | CAGACATTTTGCTCTCAAGCTG | 28,979–28,958 | |||
| NIID-JP-N | Japan | F | AAATTTTGGGGACCAGGAAC | 29,125–29,144 | [14,15] |
| P | ATGTCGCGCATTGGCATGGA | 29,222–29,241 | |||
| R | TGGCAGCTGTGTAGGTCAAC | 29,282–29,263 | |||
| R-v3 | TGGCACCTGTGTAGGTCAAC | 29,282–29,263 | |||
| HKU-N | Hong Kong | F | TAATCAGACAAGGAACTGATTA | 29,145–29,166 | [11,15] |
| P | GCAAATTGTGCAATTTGCGG | 29,196–29,177 | |||
| R | CGAAGGTGTGACTTCCATG | 29,254–29,236 | |||
| US-CDC-N-2 | United States | F | TTACAAACATTGGCCGCAAA | 29,164–29,183 | [9,15] |
| P | ACAATTTGCCCCCAGCGCTTCAG | 29,188–29,210 | |||
| R | GCGCGACATTCCGAAGAA | 29,230–29,213 | |||
| Chan-N | China | F | GCGTTCTTCGGAATGTCG | 29,210–29,227 | [10] |
| P | AACGTGGTTGACCTACACAGST | 29,257–29,278 | |||
| R | TTGGATCTTTGTCATCCAATTTG | 29,306–29,284 | |||
| Assay | Oligo | Sequence (5’-3’) | Mismatch Sequence(s) and Frequency | Mismatch Genomic Position | Suggested Modifications |
| NIID-JP-ORF1ab | FS | ACCTCATGGTCATGTTATGG | ACCTCATGGTCATG TGG (409/787) ACCTCATGGTCAGTTATGG (40/787) ACCTCATGGTCACGTTATAG (1/787) | 516–518 514 514, 520 | Design new primers outside this region. |
| RS | GACATAGCGAGTGTATGCC | GGCATATACTCGCTATGTC (4/791) | 811 | GACATAGCGAGTTATGCC | |
| Yip-ORF1ab | R | TTGTTATAGCGGCCTTCTGT | ACRGAAGGCCGCTATAACAA (1/780) ACAGAAGGCCGCTGTAACAA (1/780) ACAAAGGCCGCTATAACAA (4/780) | 1954 1964 1955 | TTGTTATAGCGGCCTTTGT |
| Pasteur-ORF1ab-1 | R | CTCCCTTTGTTGTGTTGT | ACAACACAACAAAGGAG (149/792) ACAACACAACAAAGGAG (61/792) | 12,795 12,794 | CTCTTTGTTGTGTTGT |
| CN-CDC-ORF1ab | F | CCCTGTGGGTTTTACACTTAA | CCCTGTGGGTTTTAACTTAA (4/793) | 13,356 | CCCTGTGGGTTTTAACTTAA |
| Corman-ORF1ab | P2 | CCAGGTGGWACRTCATCMGGTGATGC | CCAGGTGGAACCTCATCAGGGATGC (793/793) | 15,480, 15,489 | P2 was designed to detect SARS-CoV-2, SARS-CoV, and bat-SARS-related CoVs. For perfect match, use the other probe (probe1) of Corman-ORF1ab assay [12]. |
| R | CARATGTTAAASACACTATTAGCATA | TATGCTAATAGTGTTTTAACATTTG (793/793) | 15,519 | CARATGTTAAAACACTATTAGCATA | |
| Chan-ORF1ab | R | GTGTGATGTTGAWATGACATGGTC | GACCATGTCATATCAACATCACA (792/792) | 16,353 | TGTGATGTTGAWATGACATGGTC |
| HKU-ORF1ab | P | TAGTTGTGATGCWATCATGACTAG | TAGTTGTGATCAATCATGACTAG (12/793) | 18,859 | TAGTTGTGATCWATCATGACTAG |
| Young-S | F | TATACATGTCTCTGGGACCA | TA TCTCTGGGACCA (415/789) | 21,765–21,770 | Design new primers outside this region. |
| R | ATCCAGCCTCTTATTATGTTAGAC | GTCTAAATAATAAGAGGCTGGAT (10/790) | 21,859 | GTCTAAATAATAAGAGGCTGGAT | |
| NIID-JP-S | FS | AAGACTCACTTTCTTCCACAG | AAGACTCACTTTTTTCCACAG (3/790) AAGACTCACTTTCTTCCACAT (1/790) | 24,378 24,386 | Individual mutations are below the threshold. No modifications are currently required. |
| Won-E | R | CACACAATCGATGCGCAGTA | TACTGCGCTCGATTGTGTG (775/775) | 26,354 | CACACAATCGAGCGCAGTA |
| US-CDC-N-1 | P | ACCCCGCATTACGTTTGGTGGACC | ACCTCGCATTACGTTTGGTGGACC (1/792) ACCCCGCATTACGTTTGTTGGACC (1/792) ACCCGCATTACGTTTGGTGGACC (5/792) | 28,312 28,326 28,311 | ACCCGCATTACGTTTGGTGGACC |
| R | TCTGGTTACTGCCAGTTGAATCTG | CAGATTCAACTGGCAGTAACCAG (95/792) CAGATTCAACTGGCAGTAAACAGA (1/792) | 28,358 28,354 | CTGGTTACTGCCAGTTGAATCTG | |
| NIH-TH-N | R | CCCCACTGCGTTCTCCATT | ATGGAGAACGCAGTGGGG (95/792) | 28,358 | CCCCACTGCGTTCTCCAT |
| Young-N | P | ACCTAGGAACTGGCCCAGAAGCT | ACCTAGGAACTGGCCAGAAGCT (793/793) | 28,621 | ACCTAGGAACTGGCCAGAAGCT |
| CN-CDC-N | F | GGGGAACTTCTCCTGCTAGAAT | GAACTTCTCCTGCTAGAAT (446/785) AACTTCTCCTGCTAGAAT (13/785) | 28,881–28,884 | AACTTCTCCTGCTAGAATor design new primer |
| NIID-JP-N | R | TGGCAGCTGTGTAGGTCAAC | GTTGACCTACACAGTGCCA (789/789) | 29,277 | This mismatch is already corrected in R-v3 primer of NIID-JP-N assay [14]. |
| Chan-N | R | TTGGATCTTTGTCATCCAATTTG | CAAATTGGATGACAAAATCCAA (12/789) CAAATTGGATTACAAAGATCCAA (1/789) | 29,300 29,294 | TTGGATTTTGTCATCCAATTTG |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elaswad, A.; Fawzy, M. Mutations in Animal SARS-CoV-2 Induce Mismatches with the Diagnostic PCR Assays. Pathogens 2021, 10, 371. https://doi.org/10.3390/pathogens10030371
Elaswad A, Fawzy M. Mutations in Animal SARS-CoV-2 Induce Mismatches with the Diagnostic PCR Assays. Pathogens. 2021; 10(3):371. https://doi.org/10.3390/pathogens10030371
Chicago/Turabian StyleElaswad, Ahmed, and Mohamed Fawzy. 2021. "Mutations in Animal SARS-CoV-2 Induce Mismatches with the Diagnostic PCR Assays" Pathogens 10, no. 3: 371. https://doi.org/10.3390/pathogens10030371
APA StyleElaswad, A., & Fawzy, M. (2021). Mutations in Animal SARS-CoV-2 Induce Mismatches with the Diagnostic PCR Assays. Pathogens, 10(3), 371. https://doi.org/10.3390/pathogens10030371







