Prevalence of Non-SARS-CoV-2 Respiratory Pathogens and Co-Infection with SARS-CoV-2 in the Early Stage of COVID-19 Epidemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Nucleic Acid Extraction and Preservation
2.4. Respiratory Pathogen Multiplex Detection
2.5. SARS-CoV-2 Nucleic Acid Detection
2.6. Statistics Analyses
2.7. Ethics Approval Statement
3. Results
3.1. Baseline Characteristics
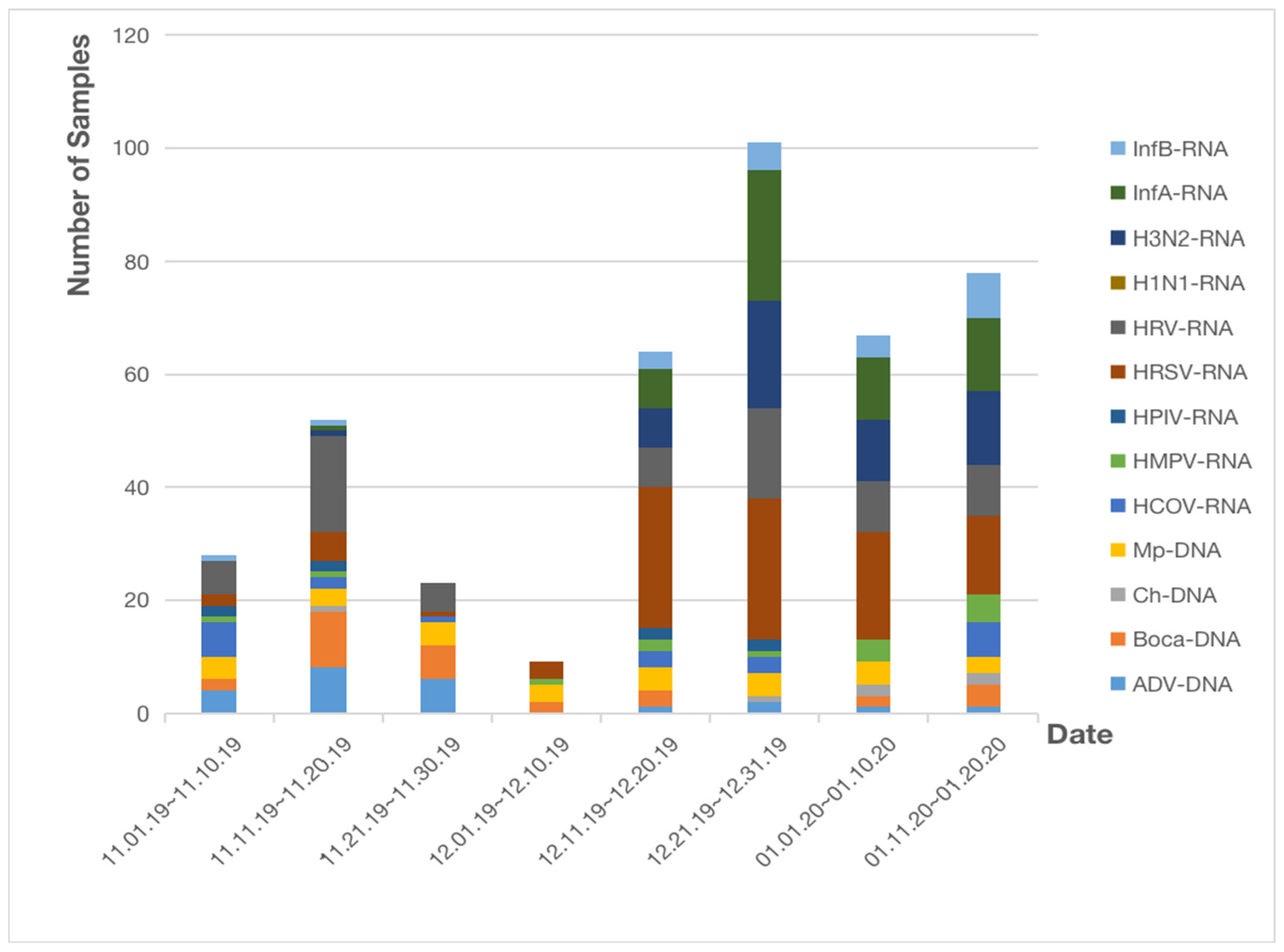
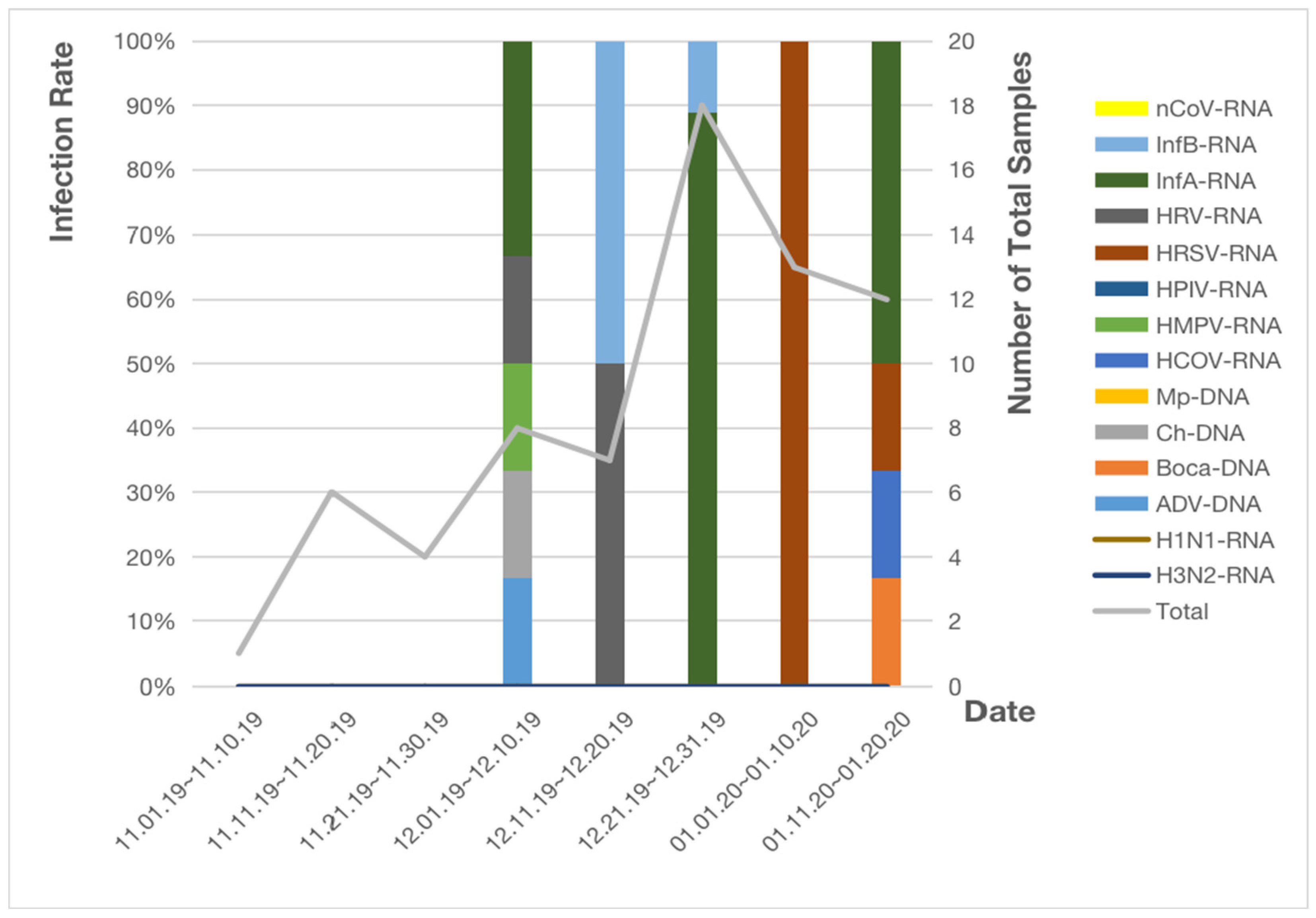
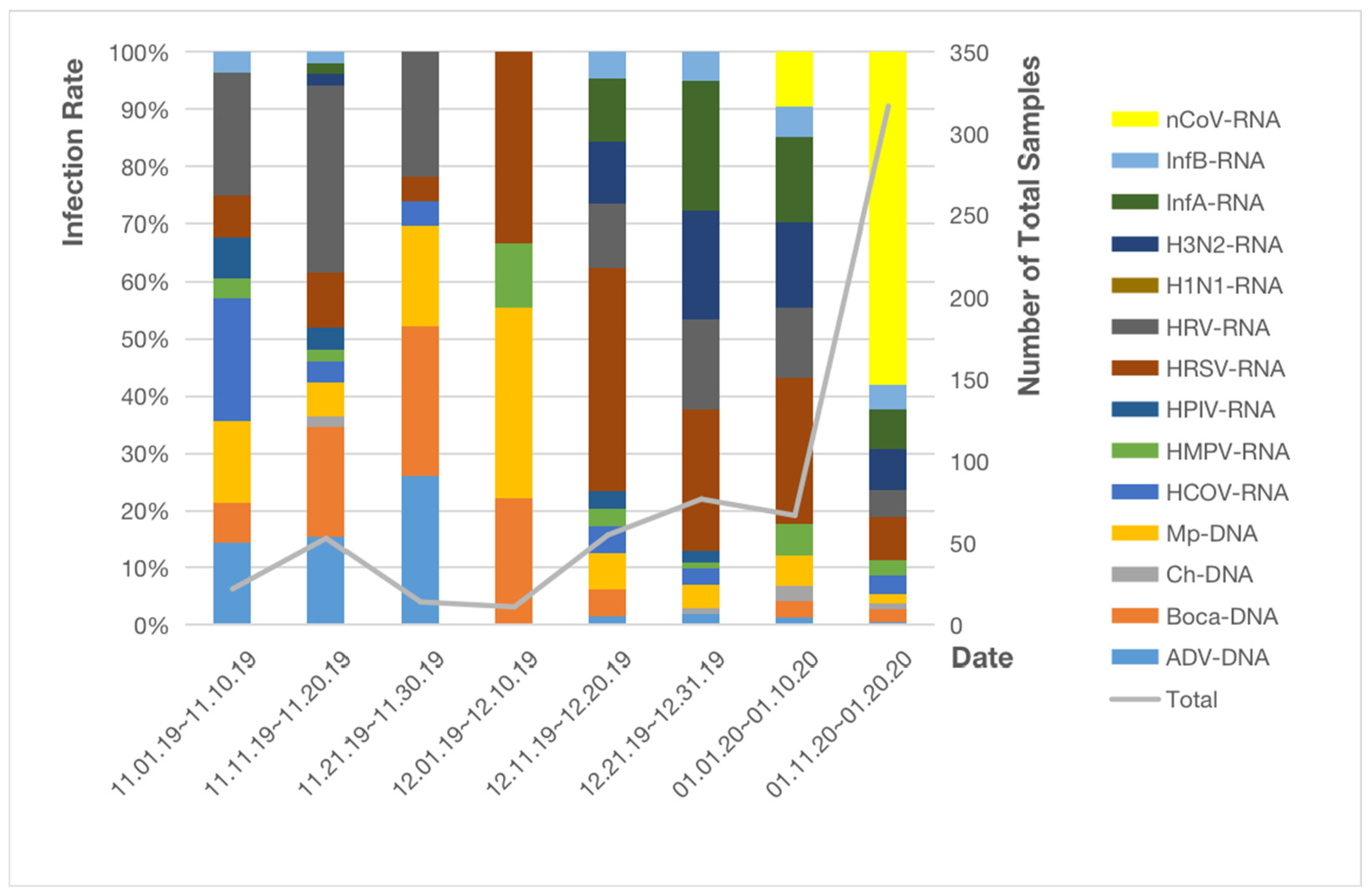
3.2. Distribution of Non-SARS-CoV-2 Respiratory Pathogens
3.3. Infection of SARS-CoV-2 and Characteristics of COVID-19 Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Hui, D.S.; Azhar, E.I. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.; Liu, J.; Zhao, X.; Liu, C.; Wang, W.; Wang, D.; Xu, W.; Zhang, C.; Yu, J.; Jiang, B.; et al. Clinical Characteristics of Imported Cases of Coronavirus Disease 2019 (COVID-19) in Jiangsu Province: A Multicenter Descriptive Study. Clin. Infect. Dis. 2020, 71, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. SARS-CoV That Caused the 2002–2003 Pandemic—5 July 2003. Available online: https://www.who.int/news/item/05-07-2003-sars-outbreak-contained-worldwide (accessed on 10 August 2021).
- The National Health Commission of the People’s Republic of China. Available online: http://www.nhc.gov.cn/xcs/yqtb/202001/930c021cdd1f46dc832fc27e0cc465c8.shtml (accessed on 12 October 2022).
- Weekly, C.C. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)—China, 2020. China CDC Wkly. 2020, 2, 113–122. [Google Scholar] [CrossRef]
- Khan, M.; Adil, S.F.; Alkhathlan, H.Z.; Tahir, M.N.; Saif, S.; Khan, M.; Khan, S.T. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules 2020, 26, 39. [Google Scholar] [CrossRef] [PubMed]
- Nature. Available online: https://doi.org/10.1038/d41586-020-01538-8 (accessed on 12 October 2022).
- Adlhoch, C.; Sneiderman, M.; Martinuka, O.; Melidou, A.; Bundle, N.; Fielding, J.; Olsen, S.J.; Penttinen, P.; Pastore, L.; Pebody, R.; et al. Spotlight influenza: The 2019/20 influenza season and the impact of COVID-19 on influenza surveillance in the WHO European Region. Eurosurveillance 2021, 26, 2100077. [Google Scholar] [CrossRef] [PubMed]
- Itaya, T.; Furuse, Y.; Jindai, K. Does COVID-19 infection impact on the trend of seasonal influenza infection? 11 countries and regions, from 2014 to 2020. Int. J. Infect. Dis. 2020, 97, 78–80. [Google Scholar] [CrossRef] [PubMed]
- The National Institute of Infectious Diseases. Available online: https://www.niid.go.jp/niid/en/865-iasr/10759-489te.html (accessed on 12 October 2022).
- Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm (accessed on 10 August 2021).
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Nowak, M.D.; Sordillo, E.M.; Gitman, M.R.; Mondolfi, A.E.P. Coinfection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J. Med. Virol. 2020, 92, 1699–1700. [Google Scholar] [CrossRef] [PubMed]
- Si, Y.; Zhao, Z.; Chen, R.; Zhong, H.; Liu, T.; Wang, M.; Song, X.; Li, W.; Ying, B. Epidemiological surveillance of common respiratory viruses in patients with suspected COVID-19 in Southwest China. BMC Infect. Dis. 2020, 20, 688. [Google Scholar] [CrossRef]
- Wu, J.; Li, W.; Shi, X.; Chen, Z.; Jiang, B.; Liu, J.; Wang, D.; Liu, C.; Meng, Y.; Cui, L.; et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J. Intern. Med. 2020, 288, 128–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.; Cai, Y.; Huang, X.; Yu, X.; Zhao, L.; Wang, F.; Li, Q.; Gu, S.; Xu, T.; Li, Y.; et al. Co-infection with SARS-CoV-2 and Influenza A Virus in Patient with Pneumonia, China. Emerg. Infect. Dis. 2020, 26, 1324–1326. [Google Scholar] [CrossRef] [PubMed]
- Touzard-Romo, F.; Tapé, C. Co-infection with SARS-CoV-2 and Human Metapneumovirus. Rhode Isl. Med. J. 2020, 103, 75–76. [Google Scholar]
- Lin, D.; Liu, L.; Zhang, M.; Hu, Y.; Yang, Q.; Guo, J.; Guo, Y.; Dai, Y.; Xu, Y.; Cai, Y.; et al. Co-infections of SARS-CoV-2 with multiple common respiratory pathogens in infected patients. Sci. China Life Sci. 2020, 63, 606–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.; Quinn, J.; Pinsky, B.; Shah, N.H.; Brown, I. Rates of Co-infection Between SARS-CoV-2 and Other Respiratory Pathogens. JAMA 2020, 323, 2085–2086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Wang, H.; Wang, F.; Lu, X.; Du, H.; Xu, J.; Han, F.; Zhang, L.; Zhang, M. Co-infections of SARS-CoV-2 with multiple common respiratory pathogens in infected children: A retrospective study. Medicine 2021, 100, e24315. [Google Scholar] [CrossRef] [PubMed]
- Pigny, F.; Wagner, N.; Rohr, M.; Mamin, A.; Cherpillod, P.; Posfay-Barbe, K.M.; Kaiser, L.; Eckerle, I.; L’Huillier, A.G. Viral co-infections among SARS-CoV-2-infected children and infected adult household contacts. Eur. J. Pediatr. 2021, 180, 1991–1995. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Xing, Y.; Shi, L.; Li, W.; Gao, Y.; Pan, S.; Wang, Y.; Wang, W.; Xing, Q. Coinfection and Other Clinical Characteristics of COVID-19 in Children. Pediatrics 2020, 146, e20200961. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Zhang, S.; Zhang, R.; Chen, X.; Wang, Y.; Zhu, C. Epidemiological and Clinical Characteristics of COVID-19 in Children: A Systematic Review and Meta-Analysis. Front. Pediatr. 2020, 8, 591132. [Google Scholar] [CrossRef] [PubMed]
| Cities | Age | P25 | P50 | P75 | Mean | Deviation | Min | Max |
|---|---|---|---|---|---|---|---|---|
| Wuhan | Male (N = 326) | 1.00 | 6.00 | 55.00 | 25.66 | 28.53 | 1 | 92 |
| Female (N = 290) | 3.00 | 26.50 | 56.00 | 29.94 | 27.79 | 1 | 88 | |
| Taiyuan | Male (N = 39) | 45.00 | 62.00 | 71.00 | 58.62 | 19.47 | 17 | 93 |
| Female (N = 30) | 27.00 | 56.00 | 77.00 | 51.03 | 26.79 | 2 | 86 |
| City | Month | Infection a | Total b | Percentage (%) | X2 | p Value |
|---|---|---|---|---|---|---|
| Wuhan | November | 103 | 422 | 24.41 | 137 | <0.01 |
| December | 174 | 41.23 | ||||
| January | 145 | 34.36 | ||||
| Taiyuan | November | 0 | 24 | 0 | 10.64 | 0.096 |
| December | 17 | 70.83 | ||||
| January | 7 | 29.17 |
| City | Date | N a | N b | Percentage (%) | X2 | p |
|---|---|---|---|---|---|---|
| Wuhan | 1 January 2020–10 January 2020 | 67 | 7 | 10.45 | 14.71 | <0.01 |
| 11 January 2020–20 January 2020 | 317 | 108 | 34.07 |
| Sex, n (%) | |
|---|---|
| Male | 1 (16.7) |
| Female | 5 (83.3) |
| Clinical symptoms, n (%) | |
| Fever | 6 (100) |
| Cough | 5 (83.3) |
| Emesis | 1 (16.7) |
| Chills | 2 (33.3) |
| Headache | 1 (16.7) |
| Radiological features, n (%) | |
| CT ground glass appearance | 2 (33.3) |
| Bilateral chest CT consolidation | 4 (66.7) |
| Co-infection, n (%) | |
| HMPV | 2 (33.3) |
| HRSV | 1 (16.7) |
| Mp | 1 (16.7) |
| Treatment, n (%) | |
| Antibiotics | 6 (100) |
| Steroid | 2 (33.3) |
| Immunoglobulin | 2(33.3) |
| Alveolar lavage | 2(33.3) |
| Admission Diagnosis, n (%) | |
| Fever of unknown | 1 (16.7) |
| Pulmonary infection | 3 (50) |
| Bronchitis | 2 (33.3) |
| pneumonia | 1 (16.7) |
| Discharge Diagnosis, n (%) | |
| Pneumonia | 3(50) |
| Pulmonary infection | 2(33.3) |
| Bronchitis | 2(33.3) |
| COVID-19 | 1(16.7) |
| Inspection Item | Mean ± SD | Reference Value |
|---|---|---|
| Erythrocyte count (×1012/L) | 3.80 ± 0.82 | 3.50–5.00 |
| Leukocyte count (×109/L) | 6.61 ± 5.52 | 4.00–10.00 |
| Neutrophils count (×109/L) | 6.77 ± 5.28 | 2.00–7.00 |
| Neutrophils% | 74.38 ± 10.78 | 50.00–75.00 |
| Monocytes count (×109/L) | 0.45 ± 0.31 | 0.20–1.00 |
| Monocytes% | 10.00 ± 5.40 | 3.00–8.00 |
| Lymphocytes count (×109/L) | 1.20 ± 0.93 | 1.00–4.40 |
| Lymphocytes% | 20.18 ± 9.55 | 20.00–40.00 |
| HGB (g/L) | 119.33 ± 10.88 | 110.00–150.00 |
| PLT (×109/L) | 356.25 ± 104.81 | 100.00–300.00 |
| APTT (s) | 35.05 ± 0.78 | 25.10–36.50 |
| PT% | 67.65 ± 8.84 | 80.00–160.00 |
| FIB (g/L) | 4.50 ± 0.34 | 2.38–4.98 |
| AST (IU/L) | 29.25 ± 22.72 | 0–40.00 |
| ALB (g/L) | 34.09 ± 2.99 | 38.00–60.00 |
| HDL-C (mmol/L) | 0.70 ± 0.16 | 0.80–1.80 |
| Creatinine (μmol/L) | 39.00 ± 12.36 | 53.00–106.00 |
| Potassium (K) (mmol/L) | 3.97 ± 1.33 | 3.50–5.50 |
| Sodium (Na) (mmol/L) | 139.67 ± 10.69 | 130.00–150.00 |
| Calcium (Ca) (mmol/L) | 1.95 ± 0.08 | 1.80–2.60 |
| PH | 7.46 ± 0.02 | 7.35–7.45 |
| PCT (ng/mL) | 0.09 ± 0.04 | 0–0.50 |
| IgG (g/L) | 11.37 ± 8.43 | 7.23–16.85 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, H.; Saed, Y.A.; Song, W.; Wang, M.; Li, Y. Prevalence of Non-SARS-CoV-2 Respiratory Pathogens and Co-Infection with SARS-CoV-2 in the Early Stage of COVID-19 Epidemic. Pathogens 2022, 11, 1292. https://doi.org/10.3390/pathogens11111292
Han H, Saed YA, Song W, Wang M, Li Y. Prevalence of Non-SARS-CoV-2 Respiratory Pathogens and Co-Infection with SARS-CoV-2 in the Early Stage of COVID-19 Epidemic. Pathogens. 2022; 11(11):1292. https://doi.org/10.3390/pathogens11111292
Chicago/Turabian StyleHan, Huimin, Yasin Abdi Saed, Wenzhu Song, Ming Wang, and Yafeng Li. 2022. "Prevalence of Non-SARS-CoV-2 Respiratory Pathogens and Co-Infection with SARS-CoV-2 in the Early Stage of COVID-19 Epidemic" Pathogens 11, no. 11: 1292. https://doi.org/10.3390/pathogens11111292





