Enhanced Seroconversion to West Nile Virus Proteins in Mice by West Nile Kunjin Replicon Virus-like Particles Expressing Glycoproteins from Crimean–Congo Hemorrhagic Fever Virus
Abstract
:1. Introduction
2. Results
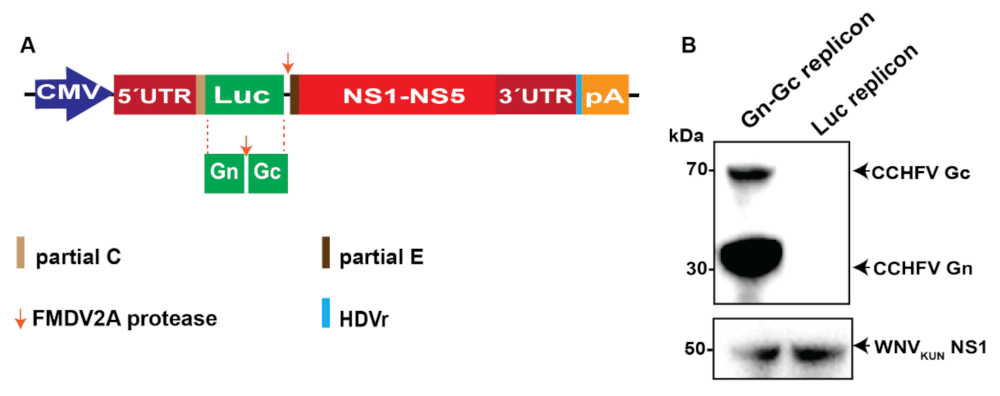
2.1. CCHFV Gn–Gc Expression by the WNVKUN Replicon
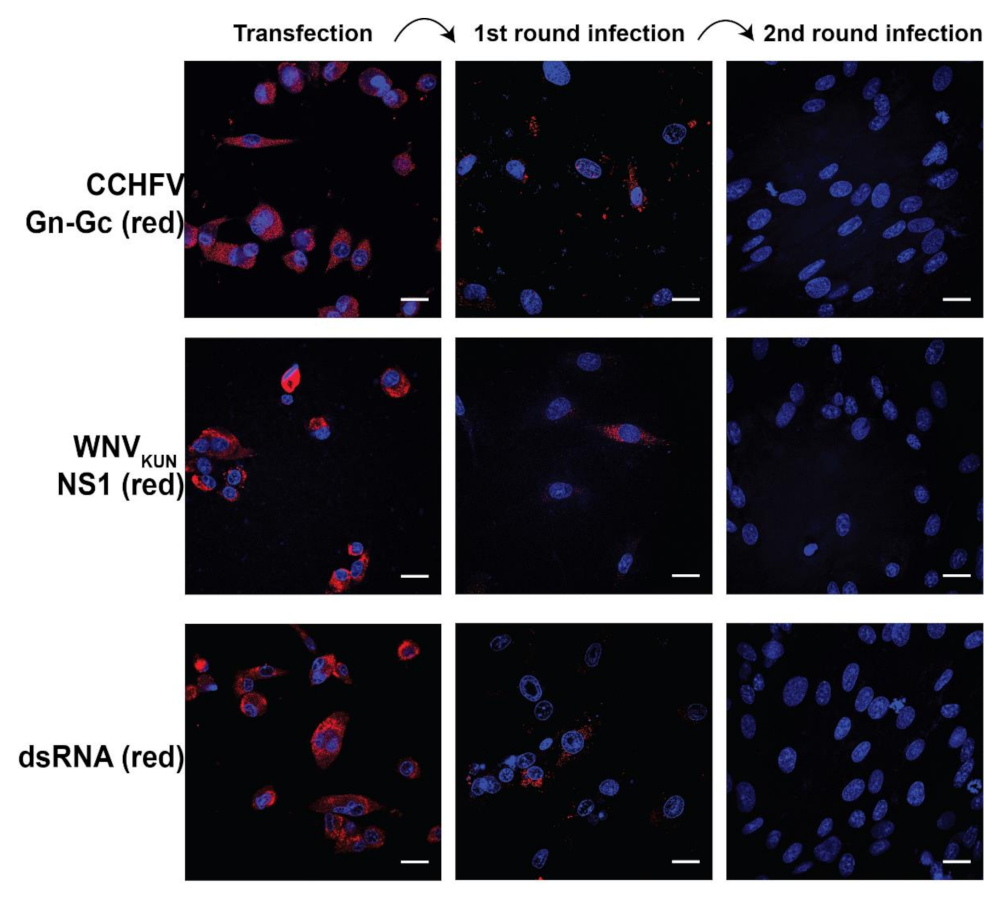
2.2. WNVKUN RVPs Transduced Their Polyprotein Gene and CCHFV Gn–Gc Gene in A Single Cycle
2.3. CCHFV Gn–Gc RVPs Induced Seroconversion to CCHFV Gn and Gc Proteins and Enhanced Seroconversion to WNVNY99 NS1 and E Proteins
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. Preparation of Gene Constructs
4.3. Proteins and Antibodies
4.4. Protein Electrophoresis and Immunoblotting
4.5. Immunofluorescence Assay
4.6. RVP Purification and RVP Concentration Measurement
4.7. Animal Immunizations
4.8. Sample Collection
4.9. Enzyme-Linked Immunosorbent Assays (ELISA)
4.10. WNVKUN and CCHFV Neutralization Assays
4.11. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lanciotti, R.S.; Ebel, G.D.; Deubelc, V.; Kerst, A.J.; Murric, S.; Meyerd, R.; Bowend, M.; Mc Kinneyd, N.; Morrill, W.E.; Crabtree, M.B.; et al. Complete Genome Sequences and Phylogenetic Analysis of West Nile Virus Strains Isolated from the United States, Europe, and the Middle East. Virology 2002, 298, 96–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American CDC. Available online: https://www.cdc.gov/westnile/index.html (accessed on 24 June 2021).
- Scherret, J.H.; Poidinger, M.; Mackenzie, J.S.; Broom, A.K.; Deubel, V.; Lipkin, W.I.; Briese, T.; Gould, E.A.; Hall, R.A. The relationships between West Nile and Kunjin viruses. Emerg. Infect. Dis. 2001, 7, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Hall, R.A.; Broom, A.K.; Smith, D.W.; Mackenzie, J.S. The Ecology and Epidemiology of Kunjin Virus. In Japanese Encephalitis and West Nile Viruses; Mackenzie, J.S., Barrett, A.D.T., Deubel, V., Eds.; Springer: Berlin/Heidelberg, Germany, 2002; pp. 253–269. [Google Scholar]
- Kellman, E.M.; Offerdahl, D.K.; Melik, W.; Bloom, M.E. Viral Determinants of Virulence in Tick-Borne Flaviviruses. Viruses 2018, 10, 329. [Google Scholar] [CrossRef]
- Barrows, N.J.; Campos, R.K.; Liao, K.-C.; Prasanth, K.R.; Soto-Acosta, R.; Yeh, S.-C.; Schott-Lerner, G.; Pompon, J.; Sessions, O.M.; Bradrick, S.S.; et al. Biochemistry and Molecular Biology of Flaviviruses. Chem. Rev. 2018, 118, 4448–4482. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xie, X.; Xia, H.; Zou, J.; Huang, L.; Popov, V.L.; Chen, X.; Shi, P.-Y. Zika Virus NS2A-Mediated Virion Assembly. mBio 2019, 10, e02375-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, X.; Zou, J.; Zhang, X.; Zhou, Y.; Routh, A.; Kang, C.; Popov, V.L.; Chen, X.; Wang, Q.-Y.; Dong, H.; et al. Dengue NS2A Protein Orchestrates Virus Assembly. Cell Host Microbe 2019, 26, 606–622.e8. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.-Y.; Tilgnera, M.; Lo, M. Construction and Characterization of Subgenomic Replicons of New York Strain of West Nile Virus. Virology 2002, 296, 219–233. [Google Scholar] [CrossRef]
- Fayzulin, R.; Scholle, F.; Petrakova, O.; Frolov, I.; Mason, P.W. Evaluation of replicative capacity and genetic stability of West Nile virus replicons using highly efficient packaging cell lines. Virology 2006, 351, 196–209. [Google Scholar] [CrossRef] [Green Version]
- Alcaraz-Estrada, S.L.; del Angel, R.; Padmanabhan, R. Construction of Self-Replicating Subgenomic Dengue Virus 4 (DENV4) Replicon. Program. Necrosis 2014, 1138, 131–150. [Google Scholar] [CrossRef]
- Manokaran, G.; Sujatmoko; McPherson, K.G.; Simmons, C.P. Attenuation of a dengue virus replicon by codon deoptimization of nonstructural genes. Vaccine 2019, 37, 2857–2863. [Google Scholar] [CrossRef]
- Khromykh, A.A.; Westaway, E.G. Subgenomic replicons of the flavivirus Kunjin: Construction and applications. J. Virol. 1997, 71, 1497–1505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamanaka, A.; Suzuki, R.; Konishi, E. Evaluation of single-round infectious, chimeric dengue type 1 virus as an antigen for dengue functional antibody assays. Vaccine 2014, 32, 4289–4295. [Google Scholar] [CrossRef] [PubMed]
- Li, S.-H.; Li, X.-F.; Zhao, H.; Deng, Y.-Q.; Yu, X.-D.; Zhu, S.-Y.; Jiang, T.; Ye, Q.; Qin, E.-D.; Qin, C.-F. Development and characterization of the replicon system of Japanese encephalitis live vaccine virus SA14-14-2. Virol. J. 2013, 10, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, W.; Ma, L.; Guo, L.-P.; Wang, X.-L.; Zhang, J.-W.; Bu, Z.-G.; Hua, R.-H. West Nile virus infectious replicon particles generated using a packaging-restricted cell line is a safe reporter system. Sci. Rep. 2017, 7, 3286. [Google Scholar] [CrossRef]
- Reynard, O.; Mokhonov, V.; Mokhonova, E.; Leung, J.; Page, A.; Mateo, M.; Pyankova, O.; Georges-Courbot, M.C.; Raoul, H.; Khromykh, A.A.; et al. Kunjin Virus Replicon-Based Vaccines Expressing Ebola Virus Glycoprotein GP Protect the Guinea Pig Against Lethal Ebola Virus Infection. J. Infect. Dis. 2011, 204 (Suppl. 3), S1060–S1065. [Google Scholar] [CrossRef] [Green Version]
- Bente, D.A.; Forrester, N.L.; Watts, D.M.; McAuley, A.J.; Whitehouse, C.A.; Bray, M. Crimean-Congo hemorrhagic fever: History, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antivir. Res. 2013, 100, 159–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Available online: https://www.who.int/health-topics/crimean-congo-haemorrhagic-fever/#tab=tab_1 (accessed on 24 June 2021).
- WHO. West Nile Virus. Available online: https://www.who.int/news-room/fact-sheets/detail/west-nile-virus (accessed on 24 June 2021).
- Spengler, J.R.; Bergeron, É.; Spiropoulou, C.F. Crimean-Congo hemorrhagic fever and expansion from endemic regions. Curr. Opin. Virol. 2019, 34, 70–78. [Google Scholar] [CrossRef]
- American CDC. Available online: https://www.cdc.gov/westnile/statsmaps/cumMapsData.html (accessed on 24 June 2021).
- Shahhosseini, N.; Jafarbekloo, A.; Telmadarraiy, Z.; Chinikar, S.; Haeri, A.; Nowotny, N.; Groschup, M.H.; Fooks, A.R.; Faghihi, F. Co-circulation of Crimean-Congo Hemorrhagic Fever virus strains Asia 1 and 2 between the border of Iran and Pakistan. Heliyon 2017, 3, e00439. [Google Scholar] [CrossRef]
- Tran, P.-T.-H.; Asghar, N.; Höglund, U.; Larsson, O.; Haag, L.; Mirazimi, A.; Johansson, M.; Melik, W. Development of a Multivalent Kunjin Virus Reporter Virus-Like Particle System Inducing Seroconversion for Ebola and West Nile Virus Proteins in Mice. Microorganisms 2020, 8, 1890. [Google Scholar] [CrossRef]
- Zaayman, D.; Venter, M. West Nile Virus Neurologic Disease in Humans, South Africa, September 2008–May 2009. Emerg. Infect. Dis. 2012, 18, 2051–2054. [Google Scholar] [CrossRef]
- Hall, R.A.; Nisbet, D.J.; Pham, K.B.; Pyke, A.; Smith, G.A.; Khromykh, A. DNA vaccine coding for the full-length infectious Kunjin virus RNA protects mice against the New York strain of West Nile virus. Proc. Natl. Acad. Sci. USA 2003, 100, 10460–10464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paz, S.; Semenza, J.C. Environmental Drivers of West Nile Fever Epidemiology in Europe and Western Asia—A Review. Int. J. Environ. Res. Public Health 2013, 10, 3543–3562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaiser, J.A.; Barrett, A.D. Twenty Years of Progress Toward West Nile Virus Vaccine Development. Viruses 2019, 11, 823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulbert, S. West Nile virus vaccines—Current situation and future directions. Hum. Vaccines Immunother. 2019, 15, 2337–2342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rios, M.; Zhang, M.J.; Grinev, A.; Srinivasan, K.; Daniel, S.; Wood, O.; Hewlett, I.K.; Dayton, A.I. Monocytes-macrophages are a potential target in human infection with West Nile virus through blood transfusion. Transfusion 2006, 46, 659–667. [Google Scholar] [CrossRef]
- García-Nicolás, O.; Lewandowska, M.; Ricklin, M.E.; Summerfield, A. Monocyte-Derived Dendritic Cells as Model to Evaluate Species Tropism of Mosquito-Borne Flaviviruses. Front. Cell. Infect. Microbiol. 2019, 9, 5. [Google Scholar] [CrossRef] [Green Version]
- Rawle, D.J.; Setoh, Y.X.; Edmonds, J.H.; Khromykh, A.A. Comparison of attenuated and virulent West Nile virus strains in human monocyte-derived dendritic cells as a model of initial human infection. Virol. J. 2015, 12, 46. [Google Scholar] [CrossRef] [Green Version]
- Ye, C.; Abraham, S.; Wu, H.; Shankar, P.; Manjunath, N. Silencing Early Viral Replication in Macrophages and Dendritic Cells Effectively Suppresses Flavivirus Encephalitis. PLoS ONE 2011, 6, e17889. [Google Scholar] [CrossRef] [Green Version]
- Khan, M.S.A.; Nain, Z.; Syed, S.B.; Abdulla, F.; Moni, M.A.; Sheam, M.M.; Karim, M.M.; Adhikari, U.K. Computational formulation and immune dynamics of a multi-peptide vaccine candidate against Crimean-Congo hemorrhagic fever virus. Mol. Cell. Probes 2021, 55, 101693. [Google Scholar] [CrossRef]
- Goedhals, D.; Paweska, J.T.; Burt, F.J. Long-lived CD8+ T cell responses following Crimean-Congo haemorrhagic fever virus infection. PLoS Neglected Trop. Dis. 2017, 11, e0006149. [Google Scholar] [CrossRef]
- Shepherd, A.J.; Swanepoel, R.; Leman, P.A. Antibody Response in Crimean-Congo Hemorrhagic Fever. Clin. Infect. Dis. 1989, 11, S801–S806. [Google Scholar] [CrossRef] [PubMed]
- Bertolotti-Ciarlet, A.; Smith, J.; Strecker, K.; Paragas, J.; Altamura, L.A.; McFalls, J.M.; Frias-Stäheli, N.; Garcia-Sastre, A.; Schmaljohn, C.S.; Doms, R.W. Cellular Localization and Antigenic Characterization of Crimean-Congo Hemorrhagic Fever Virus Glycoproteins. J. Virol. 2005, 79, 6152–6161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, P.-T.-H.; Asghar, N.; Johansson, M.; Melik, W. Roles of the Endogenous Lunapark Protein during Flavivirus Replication. Viruses 2021, 13, 1198. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, P.-T.-H.; Höglund, U.; Larsson, O.; Appelberg, S.; Mirazimi, A.; Johansson, M.; Melik, W. Enhanced Seroconversion to West Nile Virus Proteins in Mice by West Nile Kunjin Replicon Virus-like Particles Expressing Glycoproteins from Crimean–Congo Hemorrhagic Fever Virus. Pathogens 2022, 11, 233. https://doi.org/10.3390/pathogens11020233
Tran P-T-H, Höglund U, Larsson O, Appelberg S, Mirazimi A, Johansson M, Melik W. Enhanced Seroconversion to West Nile Virus Proteins in Mice by West Nile Kunjin Replicon Virus-like Particles Expressing Glycoproteins from Crimean–Congo Hemorrhagic Fever Virus. Pathogens. 2022; 11(2):233. https://doi.org/10.3390/pathogens11020233
Chicago/Turabian StyleTran, Pham-Tue-Hung, Urban Höglund, Olivia Larsson, Sofia Appelberg, Ali Mirazimi, Magnus Johansson, and Wessam Melik. 2022. "Enhanced Seroconversion to West Nile Virus Proteins in Mice by West Nile Kunjin Replicon Virus-like Particles Expressing Glycoproteins from Crimean–Congo Hemorrhagic Fever Virus" Pathogens 11, no. 2: 233. https://doi.org/10.3390/pathogens11020233





