Ocular Manifestations of Chikungunya Infection: A Systematic Review
Abstract
:1. Introduction
2. Results
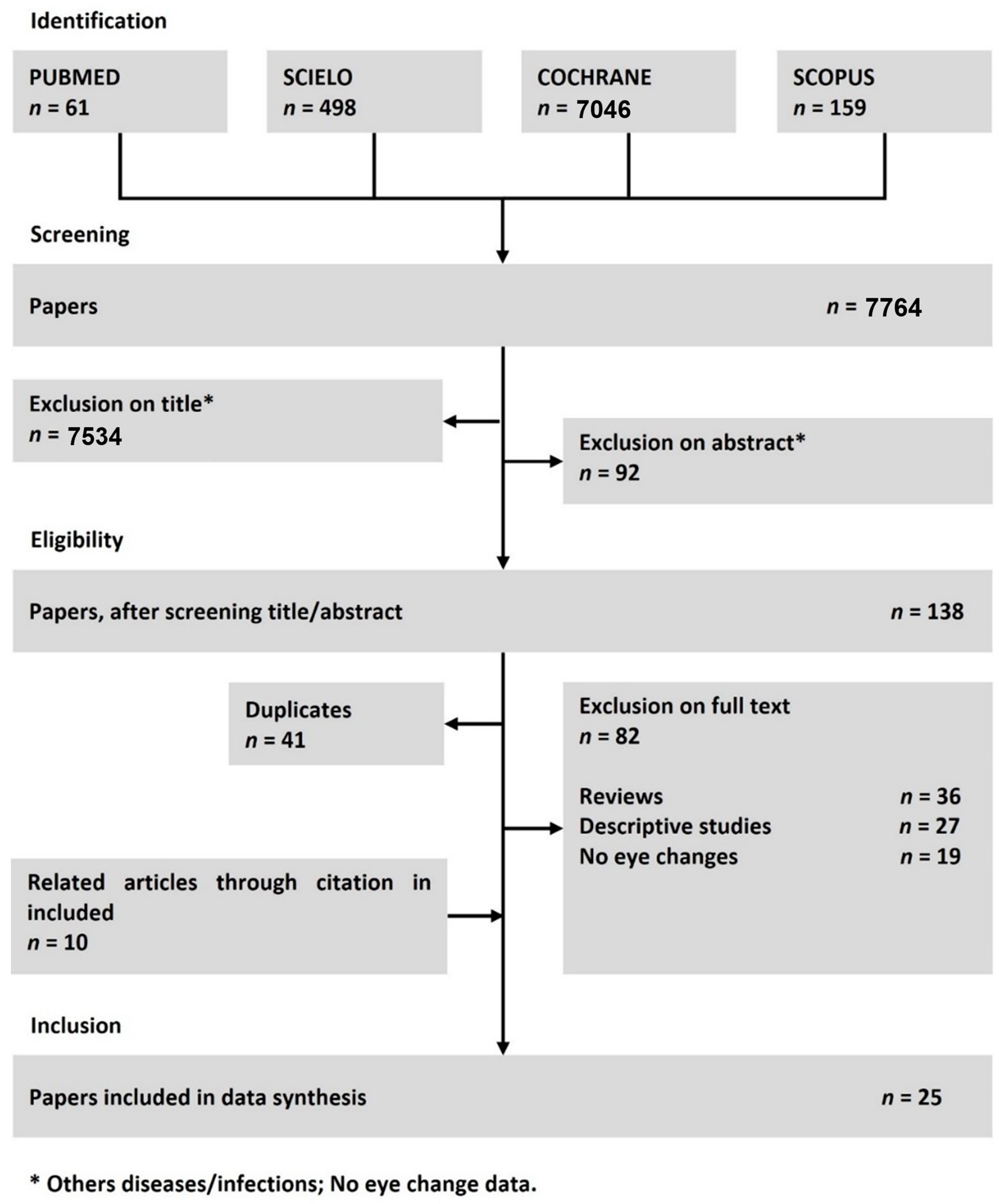
2.1. Selection of Studies
2.2. Geographical, Age and Gender Distribution
2.3. Ocular Alterations
2.4. Analysis of Risk of Bias
3. Discussion
4. Methods
4.1. Search Strategy
4.2. Study Selection
4.3. Data Extraction
4.4. Risk of Bias
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

Appendix B
| Sample Representativeness | Sample Size | Non-Respondents | Ascertainment of Exposure | Comparability | Assessment of Outcome | Statistical Analysis | Follow-Up Time |
|---|---|---|---|---|---|---|---|
| (a) Truly representative of the average population * (b) Somewhat representative of the average the average population* (c) No description | (a) Justified and satisfactory * (b) Not justified | (a) Comparability between respondents and non-responders’ characteristics is established, and the response rate is satisfactory. * (b) The response rate is unsatisfactory, or the comparability between respondents and non-respondents is unsatisfactory. (c) No description of the response rate or the characteristics of the responders and the non-responders | (a) Validated measurement tool * (b) Non-validated measurement tool, but the tool is available or described. * (c) No description of the measurement tool | (a) The study controls for the most important factor (select one). * (b) The study control for any additional factor | (a) Independent blind assessment * (b) Record linkage * (c) Self report (d) No description | (a) The statistical test used to analyse the data is clearly described * (b) The statistical test is described or incomplete | (a) The follow up time was long for the outcome to occur * (b) The follow up time was not long for the outcome to occur |
References
- Vairo, F.; Haider, N.; Kock, R.; Ntoumi, F.; Ippolito, G.; Zumla, A. Chikungunya: Epidemiology, Pathogenesis, Clinical Features, Management, and Prevention. Infect. Dis. Clin. N. Am. 2019, 33, 1003–1025. [Google Scholar] [CrossRef] [PubMed]
- Vu, D.M.; Jungkind, D.; LaBeaud, A.D. Chikungunya virus. Clin. Lab. Med. 2017, 37, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Cunha, M.S.; Costa, P.A.G.; Correa, I.A.; de Souza, M.R.M.; Calil, P.T.; da Silva, G.P.D.; Costa, S.M.; Fonseca, V.W.P.; da Costa, L.J. Chikungunya Virus: An Emergent Arbovirus to the South American Continent and a Continuous Threat to the World. Front. Microbiol. 2020, 11, 1297. [Google Scholar] [CrossRef] [PubMed]
- Petersen, L.R.; Powers, A.M. Chikungunya: Epidemiology. F1000Research 2016, 5, 1–8. [Google Scholar] [CrossRef] [Green Version]
- European Centre for Disease Prevention and Control (Webpage). Chikungunya Worldwide Overview. Available online: https://www.ecdc.europa.eu/en/chikungunya-monthly (accessed on 30 July 2021).
- Paixão, E.S.; Teixeira, M.G.; Rodrigues, L.C. Zika, Chikungunya and Dengue: The Causes and Threats of New and Reemerging Arboviral Diseases. BMJ Glob. Health 2018, 3, e000530. [Google Scholar] [CrossRef] [Green Version]
- Zaid, A.; Gérardin, P.; Taylor, A.; Mostafavi, H.; Malvy, D.; Mahalingam, S. Chikungunya Arthritis: Implications of Acute and Chronic Inflammation Mechanisms on Disease Management. Arthritis Rheumatol. 2018, 70, 484–495. [Google Scholar] [CrossRef] [Green Version]
- Burt, F.J.; Chen, W.; Miner, J.J.; Lenschow, D.J.; Merits, A.; Schnettler, E.; Kohl, A.; Rudd, P.A.; Taylor, A.; Herrero, L.J.; et al. Chikungunya Virus: An Update on the Biology and Pathogenesis of This Emerging Pathogen. Lancet Infect. Dis. 2017, 17, e107–e117. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Villamil-Gomez, W.; Paniz-Mondolfi, A.E. How many patients with post-chikungunya chronic inflammatory rheumatism can we expect in the new endemic areas of Latin America? Rheumatol. Int. 2015, 35, 2091–2094. [Google Scholar] [CrossRef]
- Silva, J.V.J., Jr.; Ludwig-Begall, L.F.; de Oliveira-Filho, E.F.; Oliveira, R.A.S.; Durães-Carvalho, R.; Lopes, T.R.R.; Silva, D.E.A.; Gil, L.H.V.G. A scoping review of Chikungunya virus infection: Epidemiology, clinical characteristics, viral co-circulation complications, and control. Acta Trop. 2018, 188, 213–224. [Google Scholar] [CrossRef]
- da Cunha, R.V.; Trinta, K.S. Chikungunya Virus: Clinical Aspects and Treatment. Mem. Inst. Oswaldo Cruz. 2017, 112, 523–531. [Google Scholar] [CrossRef]
- Barradas Barata, R. Epidemiology and Public Policies Epidemiologia e Políticas Públicas. Rev. Bras. Epidemiol. 2013, 16, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Kannan, M.; Rajendran, R.; Sunish, I.P.; Balasubramaniam, R.; Arunachalam, N.; Paramasivan, R.; Tewari, S.C.; Samuel, P.P.; Tyagi, B.K. A Study on Chikungunya Outbreak during 2007 in Kerala, South India. Indian J. Med. Res. 2009, 129, 311–315. [Google Scholar] [PubMed]
- Rose, N.; Anoop, T.M.; John, A.P.; Jabbar, P.K.; George, K.C. Acute Optic Neuritis Following Infection with Chikungunya Virus in Southern Rural India. Int. J. Infect. Dis. 2011, 15, e147–e150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perret, C.; Vizcaya, C.; Weitzel, T.; Rosas, R.; Dabanch, J.; Martínez, C. Chikungunya, Enfermedad Emergente En América Latina. Descripción de Los Primeros Casos En Chile. Rev. Chil. Infectol. 2018, 35, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Arroyo-Ávila, M.; Cabán, A.; García-Rivera, E.J.; Irizarry-Pérez, M.; Torres, H.; Gorbea, H.; Vilá, L.M. Clinical Manifestations Associated with Peripheral Joint Involvement in Patients with Acute Chikungunya Virus Infection. Am. J. Trop. Med. Hyg. 2017, 96, 916–921. [Google Scholar] [CrossRef] [Green Version]
- Vijayakumar, K.P.; Nair Anish, T.S.; George, B.; Lawrence, T.; Muthukkutty, S.C.; Ramachandran, R. Clinical Profile of Chikungunya Patients during the Epidemic of 2007 in Kerala, India. J. Glob. Infect. Dis. 2011, 3, 221–226. [Google Scholar] [CrossRef]
- Babu, K.; Kini, R.; Philips, M.; Subbakrishna, D.K. Clinical Profile of Isolated Viral Anterior Uveitis in a South Indian Patient Population. Ocul. Immunol. Inflamm. 2014, 22, 356–359. [Google Scholar] [CrossRef]
- Kawali, A.; Mahendradas, P.; Mohan, A.; Mallavarapu, M.; Shetty, B. Epidemic Retinitis. Ocul. Immunol. Inflamm. 2019, 27, 571–577. [Google Scholar] [CrossRef]
- Panato, C.S.; Figueredo, E.D.; Bassi, D.; Felipe, I.M.A.; Firmo, W.; da Cunha Araújo Firmo, W.; Sousa Rêgo, A.; de Maria Araújo Mendonça Silva, F. Evaluation of Functional Disability after Chikungunya Infection. Rev. Soc. Bras. Med. Trop. 2019, 52, e20190112. [Google Scholar] [CrossRef]
- Deeba, I.M.; Hasan, M.M.; Al Mosabbir, A.; Siam, M.H.B.; Islam, M.S.; Raheem, E.; Hossain, M.S. Manifestations of Atypical Symptoms of Chikungunya during the Dhaka Outbreak (2017) in Bangladesh. Am. J. Trop. Med. Hyg. 2019, 100, 1545–1548. [Google Scholar] [CrossRef]
- Lalitha, P.; Rathinam, S.; Banushree, K.; Maheshkumar, S.; Vijayakumar, R.; Sathe, P. Ocular Involvement Associated with an Epidemic Outbreak of Chikungunya Virus Infection. Am. J. Ophthalmol. 2007, 144, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Mahendradas, P.; Ranganna, S.K.; Shetty, R.; Balu, R.; Narayana, K.M.; Babu, R.B.; Shetty, B.K. Ocular Manifestations Associated with Chikungunya. Ophthalmology 2008, 115, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Ulloa-Padilla, J.P.; Dávila, P.J.; Izquierdo, N.J.; García-Rodríguez, O.; Jiménez, I.Z. Ocular Symptoms and Signs of Chikungunya Fever in Puerto Rico. P. R. Health Sci. J. 2018, 37, 83–87. [Google Scholar] [PubMed]
- Del Carpio-Orantes, L.; Contreras-Sánchez, E.R.; Luna-Ceballos, R.I. Ophthalmic Manifestations of Arbovirus Infections in Adults. Arch. la Soc. Española Oftalmol. 2020, 95, 71–74. [Google Scholar] [CrossRef]
- Mittal, A.; Mittal, S.; Bharati, J.; Ramakrishnan, R.; Saravanan, S.; Sathe, P.S. Optic Neuritis Associated with Chikungunya Virus Infection in South India. Arch. Ophthalmol. 2007, 125, 1381–1386. [Google Scholar] [CrossRef] [Green Version]
- Kharel, R.; Janani, M.K.; Madhavan, H.N.; Biswas, J. Outcome of Polymerase Chain Reaction (PCR) Analysis in 100 Suspected Cases of Infectious Uveitis. J. Ophthalmic. Inflamm. Infect. 2018, 8, 2. [Google Scholar] [CrossRef] [Green Version]
- Rezza, G.; Nicoletti, L.; Angelini, R.; Romi, R.; Finarelli, A.; Panning, M.; Cordioli, P.; Fortuna, C.; Boros, S.; Magurano, F.; et al. Infection with Chikungunya Virus in Italy: An Outbreak in a Temperate Region. Lancet 2007, 370, 1840–1846. [Google Scholar] [CrossRef]
- Hochedez, P.; Jaureguiberry, S.; Debruyne, M.; Bossi, P.; Hausfater, P.; Brucker, G.; Bricaire, F.; Caumes, E. Chikungunya Infection in Travelers. Emerg. Infect. Dis. 2006, 12, 1565–1567. [Google Scholar] [CrossRef]
- Paul, B.J.; Pannarkady, G.; Moni, S.P.; Thachil, E.J. Clinical Profile and Long-Term Sequelae of Chikungunya Fever. Indian J. Rheumatol. 2011, 6 (Suppl. S1), 12–19. [Google Scholar] [CrossRef]
- Staikowsky, F.; Le Roux, K.; Schuffenecker, I.; Laurent, P.; Grivard, P.; Develay, A.; Michault, A. Retrospective Survey of Chikungunya Disease in Réunion Island Hospital Staff. Epidemiol. Infect. 2008, 136, 196–206. [Google Scholar] [CrossRef]
- Manimunda, S.P.; Vijayachari, P.; Uppoor, R.; Sugunan, A.P.; Singh, S.S.; Rai, S.K.; Sudeep, A.B.; Muruganandam, N.; Chaitanya, I.K.; Guruprasad, D.R. Clinical Progression of Chikungunya Fever during Acute and Chronic Arthritic Stages and the Changes in Joint Morphology as Revealed by Imaging. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Chopra, A.; Anuradha, V.; Ghorpade, R.; Saluja, M. Acute Chikungunya and Persistent Musculoskeletal Pain Following the 2006 Indian Epidemic: A 2-Year Prospective Rural Community Study. Epidemiol. Infect. 2012, 140, 842–850. [Google Scholar] [CrossRef]
- Vishwanath, S.; Badami, K.; Sriprakash, K.S.; Sujatha, B.L.; Shashidhar, S.D.; Shilpa, Y.D. Post-Fever Retinitis: A Single Center Experience from South India. Int. Ophthalmol. 2014, 34, 851–857. [Google Scholar] [CrossRef]
- Babu, K.; Adiga, M.; Govekar, S.R.; Ravi Kumar, B.V.; Murthy, K.R. Associations of Fuchs Heterochromic Iridocyclitis in a South Indian Patient Population. J. Ophthalmic. Inflamm. Infect. 2013, 3, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahendradas, P.; Shetty, R.; Narayana, K.M.; Shetty, B.K. In Vivo Confocal Microscopy of Keratic Precipitates in Infectious Versus Noninfectious Uveitis. Ophthalmology 2010, 117, 373–380. [Google Scholar] [CrossRef]
- Kawali, A.; Srinivasan, S.; Mahendradas, P.; Shetty, B. Epidemic retinitis and community outbreaks. Indian J. Ophthalmol. 2020, 68, 1916. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, A.; Patel, R.; Goyal, S.; Rajaratnam, T.; Sharma, A.; Hossain, P. Ocular Manifestations of Emerging Viral Diseases. Eye 2021, 35, 1117–1139. [Google Scholar] [CrossRef] [PubMed]
- Matusali, G.; Colavita, F.; Bordi, L.; Lalle, E.; Ippolito, G.; Capobianchi, M.R.; Castilletti, C. Tropism of the Chikungunya Virus. Viruses 2019, 11, 175. [Google Scholar] [CrossRef] [Green Version]
- Mahendradas, P.; Avadhani, K.; Shetty, R. Chikungunya and the Eye: A Review. J. Ophthalmic. Inflamm. Infect. 2013, 3, 35. [Google Scholar] [CrossRef] [Green Version]
- de Andrade, G.C.; Ventura, C.V.; Filho, P.A.; de Arruda Mello Filho, P.A.; Maia, M.; Vianello, S.; Rodrigues, E.B. Arboviruses and the Eye. Int. J. Retin. Vitr. 2017, 3, 4. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Pulgarín, D.F.; Chowdhury, F.R.; Villamil-Gomez, W.E.; Rodriguez-Morales, A.J.; Blohm, G.M.; Paniz-Mondolfi, A.E. Ophthalmologic Aspects of Chikungunya Infection. Travel Med. Infect. Dis. 2016, 14, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Pulgarín, D.F.; Muñoz-Urbano, D.M.; De la Cruz, D.Z. The eye and the chikungunya virus. In Current Topics in Chikungunya; Rodriguez-Morales, A.J., Ed.; IntechOpen: London, UK, 2016. [Google Scholar]
- McMonnies, C.W. Inflammation and Keratoconus. Optom. Vis. Sci. 2015, 92, e35–e41. [Google Scholar] [CrossRef] [PubMed]
- Cronau, H.; Kankanala, R.R.; Mauger, T. Diagnosis and Management of Red Eye in Primary Care. Am. Fam. Physician 2010, 81, 137–144. [Google Scholar]
- Efron, N. Contact Lens Wear Is Intrinsically Inflammatory. Clin. Exp. Optom. 2017, 100, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Merle, H.; Donnio, A.; Jean-Charles, A.; Guyomarch, J.; Hage, R.; Najioullah, F.; Césaire, R.; Cabié, A. Ocular Manifestations of Emerging Arboviruses: Dengue Fever, Chikungunya, Zika Virus, West Nile Virus, and Yellow Fever. J. Fr. Ophtalmol. 2018, 41, e235–e243. [Google Scholar] [CrossRef]
- Mahesh, G.; Giridhar, A.; Shedbele, A.; Kumar, R.; Saikumar, S.J. A Case of Bilateral Presumed Chikungunya Neuroretinitis. Indian J. Ophthalmol. 2009, 57, 148–150. [Google Scholar] [CrossRef]
- Portnoi Baran, L.C.; Fernades da Costa, M.; Summer Vidal, K.; Damico, F.M.; Telles Salgueiro Barboni, M.; da Silva Lima, D.; de Cássia Rodrigues de Matos França, V.; Gomes Martins, C.M.; Segundo Tabares, H.; Leonardo Dias, S.; et al. Alterations in Visual Acuity and Visual Development in Infants 1–24 Months Old Either Exposed to or Infected by Zika Virus during Gestation, with and without Microcephaly. J. AAPOS 2019, 23, 215.e1–215.e7. [Google Scholar] [CrossRef]
- Yudhishdran, J.; Liyanage, I.K.; Navinan, M.R.; Herath, S.; Withanage, D.; Jeyalakshmy, S.; Kulatunga, A. The Eye in Dengue Fever, a Rarely Appreciated Aspect of Dengue Expanded Syndrome: A Case Report. J. Med. Case Rep. 2019, 13, 574–580. [Google Scholar] [CrossRef] [Green Version]
- Khairallah, M.; Kahloun, R. Ocular Manifestations of Emerging Infectious Diseases. Curr. Opin. Ophthalmol. 2013, 24, 574–580. [Google Scholar] [CrossRef]
- Karesh, J.W.; Mazzoli, R.A.; Heintz, S.K. Ocular Manifestations of Mosquito-Transmitted Diseases. Mil. Med. 2018, 183, 450–458. [Google Scholar] [CrossRef] [Green Version]
- Couderc, T.; Gangneux, N.; Chrétien, F.; Caro, V.; Le Luong, T.; Ducloux, B.; Tolou, H.; Lecuit, M.; Grandadam, M. Chikungunya Virus Infection of Corneal Grafts. J. Infect. Dis. 2012, 206, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Korzeniewski, K. Eye diseases in travelers. Int. Marit. Health 2020, 71, 78–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salceanu, S.O.; Raman, V. Recurrent chikungunya retinitis. BMJ Case. Rep. 2018, 2018, bcr2017222864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliver, G.F.; Carr, J.M.; Smith, J.R. Emerging infectious uveitis: Chikungunya, dengue, Zika and Ebola: A review. Clin Exp. Ophthalmol. 2019, 47, 372–380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuthya, S.; Anthony, C.L.; Fashina, T.; Yeh, S.; Shantha, J.G. World Health Organization High Priority Pathogens: Ophthalmic Disease Findings and Vision Health Perspectives. Pathogens 2021, 10, 442. [Google Scholar] [CrossRef] [PubMed]
- Kahloun, R.; Abroug, N.; Anis, K.; Zeghidi, M.H.; Zaouali, S.; Khairallah, M. Dovepress Infectious Optic Neuropathies: A Clinical Update. Eye Brain 2015, 7, 59–81. [Google Scholar]
- Rajapakse, S.; Rodrigo, C.; Rajapakse, A. Atypical Manifestations of Chikungunya Infection. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 89–96. [Google Scholar] [CrossRef]
- Khairallah, M.; Chee, S.P.; Rathinam, S.R.; Attia, S.; Nadella, V. Novel Infectious Agents Causing Uveitis. Int. Ophthalmol. 2010, 30, 465–483. [Google Scholar] [CrossRef]
- Scripsema, N.K.; Sharifi, E.; Samson, C.M.; Kedhar, S.; Rosen, R.B. Chikungunya-Associated Uveitis and Exudative Retinal Detachment: A Case Report. Retin. Cases Br. Reports 2015, 9, 352–356. [Google Scholar] [CrossRef]
- Lee, J.H.; Agarwal, A.; Mahendradas, P.; Lee, C.S.; Gupta, V.; Pavesio, C.E.; Agrawal, R. Viral Posterior Uveitis. Surv. Ophthalmol. 2017, 62, 404–445. [Google Scholar] [CrossRef]
- de SousaRodrigues, C.F.; de Lima, F.J.C.; Barbosa, F.T. Importance of Using Basic Statistics Adequately in Clinical Research. Braz. J. Anesthesiol. 2017, 67, 619–625. [Google Scholar] [CrossRef]
- Nasci, R.S. Movement of Chikungunya Virus into the Western Hemisphere. Emerg. Infect. Dis. 2014, 20, 1394–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Silva, N.M.; Teixeira, R.A.G.; Cardoso, C.G.; Siqueira, J.B.; Coelho, G.E.; De Oliveira, E.S.F. Vigilância de Chikungunya No Brasil: Desafios No Contexto Da Saúde Pública. Epidemiol. Serv. Saude. 2018, 27, e2017127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo, C.K.L.; Mertz, D.; Loeb, M. Newcastle-Ottawa Scale: Comparing Reviewers’ to Authors’ Assessments. BMC Med. Res. Methodol. 2014, 14, 45. [Google Scholar] [CrossRef] [Green Version]
- Alshabanat, A.; Zafari, Z.; Albanyan, O.; Dairi, M.; FitzGerald, J.M. Asthma and COPD Overlap Syndrome (ACOS): A Systematic Review and Meta Analysis. PLoS ONE 2015, 10, e0136065. [Google Scholar] [CrossRef] [Green Version]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G.; Agostoni, P.; Barros, H.; et al. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef] [Green Version]

| Reference | Origin | Type of Study | Patients | Method of CHIKV Diagnosis | Patients with CHIKV (n) | Patients Presenting Ocular Symptoms/Manifestations (n) | % of Patients Presenting Ocular Symptoms/Manifestations |
|---|---|---|---|---|---|---|---|
| KANNAN et al. [13] | India | Cross sectional | All age groups, men and women | Laboratory test/clinical symptoms | 354 | 41 | 11.6% |
| ROSE et al. [14] | India | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 10 | 10 | 100% |
| PERRET et al. [15] | Chile | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 16 | 8 | 50% |
| ARROYO-ÁVILA et al. [16] | Puerto Rico | Cross sectional | Teens and adults, men and women | Laboratory test/clinical symptoms | 172 | 75 | 43.6% |
| VIJAYAKUMAR et al. [17] | India | Cross sectional | All age groups, men and women | Clinical symptoms | 1913 | 419 | 21.9% |
| BABU et al. [18] | India | Cross sectional | All age groups, men and women | Laboratory test | 2 | 2 | 100% |
| KAWALI et al. [19] | India | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 6 | 2 | 33.3% |
| PANATO et al. [20] | Brazil | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 130 | 32 | 24.6% |
| DEEBA et al. [21] | Bangladesh | Cross sectional | All age groups, men and women | Clinical symptoms | 1326 | 817 | 61.7% |
| LALITHA et al. [22] | India | Cross sectional | Adults, men and women | Laboratory test | 37 | 37 | 100% |
| MAHENDRADAS et al. [23] | India | Cross sectional | Adults, men and women | Laboratory test | 9 | 9 | 100% |
| ULLOA-PADILLA et al. [24] | Puerto Rico | Cross sectional | Adults, men and women | Laboratory test | 139 | 42 | 30.2% |
| DEL CARPIO-ORANTES et al. [25] | Mexico | Cross sectional | Adults, men and women | Clinical symptoms | 1410 | 151 | 10.7% |
| MITTAL et al. [26] | India | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 14 | 4 | 28.6% |
| KHAREL (SITAULA) et al. [27] | India | Cross sectional | * | Laboratory test | 1 | 1 | 100% |
| REZZA et al. [28] | Italy | Cross sectional | All age groups, men and women | Clinical symptoms | 205 | 31 | 15.1% |
| HOCHEDEZ et al. [29] | Africa/France | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 22 | 1 | 4.5% |
| PAUL et al. [30] | India | Cross sectional | Adults, men and women | Laboratory test/clinical symptoms | 122 | 21 | 17.2% |
| STAIKOWSKY et al. [31] | France | Cross sectional | Adults, men and women | Clinical symptoms | 221 | 16 | 7.2% |
| MANIMUNDA et al. [32] | India | Cross sectional | All age groups, men and women | Laboratory test | 203 | 49 | 24.1% |
| CHOPRA et al. [33] | India | Cross sectional | All age groups, men and women | Laboratory test/clinical symptoms | 509 | 36 | 7.1% |
| VISHWANATH et al. [34] | India | Cross sectional | Adults, women | Laboratory test | 1 | 1 | 100% |
| BABU et al. [35] | India | Cross sectional | * | Laboratory test | 1 | 1 | 100% |
| MAHENDRADAS et al. [36] | Germany | Cross sectional | Teens and adults, men and women | Laboratory test/clinical symptoms | 3 | 3 | 100% |
| KAWALI et al. [37] | India | Cross sectional | * | Laboratory test/clinical symptoms | 5 | 5 | 100% |
| Reference | Origin | Patients with CHIKV (n) | Patients Presenting Eye Inflammation | |||
|---|---|---|---|---|---|---|
| Total of Patients (n) | Male (n) | Female (n) | Age (Mean) | |||
| KANNAN et al. [13] | India | 354 | 27 | * | * | * |
| VIJAYAKUMAR et al. [17] | India | 1913 | 419 | * | * | * |
| DEEBA et al. [21] | Bangladesh | 1326 | 749 | * | * | * |
| LALITHA et al. [22] | India | 37 | 37 | 16 | 21 | 44.2 |
| MAHENDRADAS et al. [36] | India | 9 | 2 | 2 | 0 | 61.5 |
| ULLOA-PADILLA et al. [24] | Puerto Rico | 139 | 55 | * | * | * |
| MITTAL et al. [26] | India | 14 | 1 | * | * | * |
| KHAREL (SITAULA) et al. [27] | India | 1 | 1 | * | * | * |
| MANIMUNDA et al. [32] | India | 203 | 38 | * | * | * |
| VISHWANATH et al. [34] | India | 1 | 1 | 1 | 0 | 27 |
| BABU et al. [35] | India | 1 | 1 | * | * | * |
| Total of patients: | 3998 | Patients with the symptom: | 1331 | % of patients with the symptom: | 33% | |
| Reference | Origin | Patients with CHIKV (n) | Patients Presenting Visual Defects | |||
|---|---|---|---|---|---|---|
| Total of Patients (n) | Men (n) | Women (n) | Age (Mean) | |||
| ROSE et al. [14] | India | 10 | 10 | 3 | 7 | 35.8 |
| BABU et al. [35] | India | 2 | 2 | 0 | 2 | 45 |
| KAWALI et al. [37] | India | 6 | 2 | * | * | * |
| DEEBA et al. [21] | Bangladesh | 1326 | 230 | * | * | * |
| LALITHA et al. [22] | India | 37 | 37 | * | * | * |
| MAHENDRADAS et al. [36] | India | 9 | 7 | 3 | 4 | 50.7 |
| ULLOA-PADILLA et al. [24] | Puerto Rico | 139 | 2 | * | * | * |
| MITTAL et al. [26] | India | 14 | 14 | 5 | 9 | 45.8 |
| VISHWANATH et al. [34] | India | 1 | 1 | 1 | 0 | 27 |
| BABU et al. [35] | India | 1 | 1 | * | * | * |
| Total of patients: | 575 | Patients with the symptom: | 137 | % of patients with the symptom: | 23% | |
| Reference | Origin | Patients with CHIKV (n) | Patients Presenting Eye Pain | |||
|---|---|---|---|---|---|---|
| Total of Patients (n) | Men (n) | Women (n) | Age (Mean) | |||
| KANNAN et al. [13] | India | 354 | 41 | * | * | * |
| ROSE et al. [14] | India | 10 | 10 | 3 | 7 | 35.8 |
| PERRET et al. [15] | Chile | 16 | 8 | * | * | * |
| ARROYO-ÁVILA et al. [16] | Puerto Rico | 172 | 75 | * | * | * |
| MAHENDRADAS et al. [36] | India | 9 | 2 | 1 | 1 | 59 |
| MITTAL et al. [26] | India | 14 | 1 | 1 | 0 | 25 |
| Total of patients: | 1545 | Patients with the symptom: | 306 | % of patients with the symptom: | 19% | |
| Reference | Patients with CHIKV (n) | Corneal Involvement | Conjunctivitis | Episcleritis | Optic Neuritis | Uveitis | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total of Patients (n) Papatiens (n) | Women (n) | Men (n) | Age (Mean) | Total of Patiens (n) | Women (n) | Men (n) | Age (Mean) | Total of Patiens (n) | Women (n) | Men (n) | Age (Mean) | Total of Patiens (n) | Women (n) | Men (n) | Age (Mean) | Total of Patiens (n) | Women (n) | Men (n) | Age (Mean) | ||
| ROSE et al. [14] | 10 | 10 | 3 | 7 | 35.8 | ||||||||||||||||
| BABU et al. [35] | 2 | 2 | 0 | 2 | 45 | ||||||||||||||||
| KAWALI et al. [37] | 6 | 2 | * | * | * | ||||||||||||||||
| LALITHA et al. [22] | 37 | 3 | * | * | * | 8 | * | * | * | 20 | * | * | * | ||||||||
| MAHENDRADAS et al. [36] | 9 | 1 | 1 | 0 | 63 | 8 | 3 | 5 | 51.2 | ||||||||||||
| ULLOA-PADILLA et al. [24] | 139 | 27 | * | * | * | 13 | |||||||||||||||
| DEL CARPIO-ORANTES et al. [25] | 1410 | 151 | * | * | * | ||||||||||||||||
| MITTAL et al. [26] | 14 | 12 | 5 | 7 | 46.5 | ||||||||||||||||
| KHAREL (SITAULA) et al. [27] | 1 | 1 | * | * | * | ||||||||||||||||
| REZZA et al. [28] | 205 | 7 | * | * | * | ||||||||||||||||
| STAIKOWSKY et al. [31] | 221 | 16 | * | * | * | ||||||||||||||||
| MANIMUNDA et al. [32] | 203 | 49 | * | * | * | ||||||||||||||||
| VISHWANATH et al. [34] | 1 | 1 | 1 | 0 | 27 | ||||||||||||||||
| BABU et al. [35] | 1 | 1 | * | * | * | ||||||||||||||||
| MAHENDRADAS et al. [36] | 3 | 3 | * | * | * | ||||||||||||||||
| KAWALI et al. [37] | 5 | 5 | * | * | * | ||||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, L.C.M.; da Silva Platner, F.; da Silva Fonseca, L.; Rossato, V.F.; de Andrade, D.C.P.; de Sousa Valente, J.; Brain, S.D.; Fernandes, E.S. Ocular Manifestations of Chikungunya Infection: A Systematic Review. Pathogens 2022, 11, 412. https://doi.org/10.3390/pathogens11040412
da Silva LCM, da Silva Platner F, da Silva Fonseca L, Rossato VF, de Andrade DCP, de Sousa Valente J, Brain SD, Fernandes ES. Ocular Manifestations of Chikungunya Infection: A Systematic Review. Pathogens. 2022; 11(4):412. https://doi.org/10.3390/pathogens11040412
Chicago/Turabian Styleda Silva, Liziane Cristine Malaquias, Fernanda da Silva Platner, Lauany da Silva Fonseca, Virgílio Frota Rossato, Dian Carlos Pereira de Andrade, João de Sousa Valente, Susan Diana Brain, and Elizabeth Soares Fernandes. 2022. "Ocular Manifestations of Chikungunya Infection: A Systematic Review" Pathogens 11, no. 4: 412. https://doi.org/10.3390/pathogens11040412
APA Styleda Silva, L. C. M., da Silva Platner, F., da Silva Fonseca, L., Rossato, V. F., de Andrade, D. C. P., de Sousa Valente, J., Brain, S. D., & Fernandes, E. S. (2022). Ocular Manifestations of Chikungunya Infection: A Systematic Review. Pathogens, 11(4), 412. https://doi.org/10.3390/pathogens11040412






