Initial Risk Assessment in Patients with Alveolar Echinococcosis—Results from a Retrospective Cohort Study
Abstract
:1. Introduction
2. Results
2.1. Demographic and Descriptive Results
2.2. Univariate Analysis
2.3. Multivariate Analysis
3. Discussion
4. Methods
4.1. Sample Size Calculation and Data Collection
4.2. Variables of Interest
4.2.1. Demographic Variables, Medical History and Clinical Presentation
4.2.2. Laboratory Examinations
4.2.3. Imaging, Staging and AE-Related Complications
4.2.4. Treatment and Outcome
4.3. Statistical Analysis
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moro, P.; Schantz, P.M. Echinococcosis: A review. Int. J. Infect. Dis. 2009, 13, 125–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torgerson, P.R.; Keller, K.; Magnotta, M.; Ragland, N. The global burden of alveolar echinococcosis. PLoS Negl. Trop. Dis. 2010, 4, e722. [Google Scholar] [CrossRef] [PubMed]
- Gottstein, B. Echinococcus spp. and echinococcosis. Acta Vet. Scand. 2010, 52, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Romig, T.; Kratzer, W.; Kimmig, P.; Frosch, M.; Gaus, W.; Flegel, W.A.; Gottstein, B.; Lucius, R.; Beckh, K.; Kern, P. An epidemiologic survey of human alveolar echinococcosis in southwestern Germany. Am. J. Trop. Med. Hyg. 1999, 61, 566–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eckert, J.; Deplazes, P.; Kern, P. Alveolar Echinococcosis (Echinococcus Multilocularis) and Neotropical Forms of Echinococcosis; Oxford University Press: Oxford, UK, 2011. [Google Scholar] [CrossRef]
- Ammann, R.W.; Eckert, J. Parasitic diseases of the liver and intestines-Echinococcus. Gastroenterol. Clin. N. Am. 1996, 25, 655–689. [Google Scholar] [CrossRef]
- Grüner, B.; Kern, P.; Mayer, B.; Gräter, T.; Hillenbrand, A.; Barth, T.E.F.; Muche, R.; Henne-Bruns, D.; Kratzer, W.; Kern, P. Comprehensive diagnosis and treatment of alveolar echinococcosis: A single-center, long-term observational study of 312 patients in Germany. GMS Infect. Dis. 2017, 5. [Google Scholar] [CrossRef]
- Bresson-Hadni, S.; Vuitton, D.A.; Bartholomot, B.; Heyd, B.; Godart, D.; Meyer, J.P.; Hrusovsky, S.; Becker, M.C.; Mantion, G.; Lenys, D.; et al. A twenty-year history of alveolar echinococcosis: Analysis of a series of 117 patients from eastern France. Eur. J. Gastroenterol. Hepatol. 2000, 12, 327–336. [Google Scholar] [CrossRef]
- Torgerson, P.R.; Schweiger, A.; Deplazes, P.; Pohar, M.; Reichen, J.; Ammann, R.W.; Tarr, P.E.; Halkik, N.; Müllhaupt, B. Alveolar echinococcosis: From a deadly disease to a well-controlled infection. Relative survival and economic analysis in Switzerland over the last 35 years. J. Hepatol. 2008, 49, 72–77. [Google Scholar] [CrossRef]
- Kern, P. Clinical features and treatment of alveolar echinococcosis. Curr. Opin. Infect. Dis. 2010, 23, 505–512. [Google Scholar] [CrossRef]
- Kratzer, W.; Gruener, B.; Kaltenbach, T.E.; Ansari-Bitzenberger, S.; Kern, P.; Fuchs, M.; Mason, R.A.; Barth, T.F.E.; Haenle, M.M.; Hillenbrand, A.; et al. Proposal of an ultrasonographic classification for hepatic alveolar echinococcosis: Echinococcosis multilocularis Ulm classification-ultrasound. World J. Gastroenterol. 2015, 21, 12392. [Google Scholar] [CrossRef]
- Kern, P.; Wen, H.; Sato, N.; Vuitton, D.A.; Gruener, B.; Shao, Y.; Delabrousse, E.; Kratzer, W.; Bresson-Hadni, S. WHO classification of alveolar echinococcosis: Principles and application. Parasitol. Int. 2006, 55, S283–S287. [Google Scholar] [CrossRef] [PubMed]
- Newgard, C.D.; Haukoos, J.S. Advanced Statistics: Missing Data in Clinical Research—Part 2: Multiple Imputation. Acad. Emerg. Med. 2007, 14, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, E.; Kern, P.; Vuitton, D.A. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010, 114, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.; Pawlowski, Z.S.; Dixon, H. Multicentre clinical trials of benzimidazolecarbamates in human echinococcosis. Bull. World Health Organ. 1986, 64, 383–388. [Google Scholar] [PubMed]
- Piarroux, M.; Piarroux, R.; Giorgi, R.; Knapp, J.; Bardonnet, K.; Sudre, B.; Watelet, J.; Dumortier, J.; Gérard, A.; Beytout, J.; et al. Clinical features and evolution of alveolar echinococcosis in France from 1982 to 2007: Results of a survey in 387 patients. J. Hepatol. 2011, 55, 1025–1033. [Google Scholar] [CrossRef] [PubMed]
- Reuter, S.; Jensen, B.; Buttenschoen, K.; Kratzer, W.; Kern, P. Benzimidazoles in the treatment of alveolar echinococcosis: A comparative study and review of the literature. J. Antimicrob. Chemother. 2000, 46, 451–456. [Google Scholar] [CrossRef] [Green Version]
- Vuitton, D.A.; Bresson-Hadni, S. Alveolar echinococcosis: Evaluation of therapeutic strategies. Expert Opin. Orphan Drugs 2013, 2, 67–86. [Google Scholar] [CrossRef]
- Kern, P.; Bardonnet, K.; Renner, E.; Auer, H.; Pawlowski, Z.; Ammann, R.W.; Vuitton, D.A.; Registry, T.E.E. European Echinococcosis Registry: Human Alveolar Echinococcosis, Europe, 1982–2000. Emerg. Infect. Dis. 2003, 9, 343. [Google Scholar] [CrossRef]
- Kadry, Z.; Renner, E.C.; Bachmann, L.M.; Attigah, N.; Ammann, R.W.; Clavien, P. Evaluation of treatment and long-term follow-up in patients with hepatic alveolar echinococcosis. Br. J. Surg. 2005, 92, 1110–1116. [Google Scholar] [CrossRef]
- Schuhbaur, J.; Schweizer, M.; Philipp, J.; Schmidberger, J.; Schlingeloff, P.; Kratzer, W. Long-term follow-up of liver alveolar echinococcosis using Echinococcosis multilocularis ultrasound classification. World J. Gastroenterol. 2021, 27, 6939–6950. [Google Scholar] [CrossRef]
- Rausch, R.L.; Wilson, J.F.; Schantz, P.M.; McMahon, B.J. Spontaneous death of Echinococcus multilocularis: Cases diagnosed serologically (by Em2 ELISA) and clinical significance. Am. J. Trop. Med. Hyg. 1987, 36, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Bresson-Hadni, S.; Gottstein, B.; Laplante, J.-J.; Meyer, J.-P.; Miguet, J.-P.; Jacquier, P.; Lenys, D.; Vuitton, D.-A.; Mercet, P.; Rohmer, P. Seroepidemiologic screening of Echinococcus multilocularis infection in a European area endemic for alveolar echinococcosis. Am. J. Trop. Med. Hyg. 1994, 51, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Ammann, R.W.; Stumpe, K.D.M.; Grimm, F.; Deplazes, P.; Huber, S.; Bertogg, K.; Fischer, D.R.; Müllhaupt, B. Outcome after Discontinuing Long-Term Benzimidazole Treatment in 11 Patients with Non-resectable Alveolar Echinococcosis with Negative FDG-PET/CT and Anti-EmII/3-10 Serology. PLoS Negl. Trop. Dis. 2015, 9, e0003964. [Google Scholar] [CrossRef] [PubMed]
- Ammann, R.W.; Renner, E.C.; Gottstein, B.; Grimm, F.; Eckert, J.; Renner, E.L. Immunosurveillance of alveolar echinococcosis by specific humoral and cellular immune tests: Long-term analysis of the Swiss chemotherapy trial (1976–2001). J. Hepatol. 2004, 41, 551–559. [Google Scholar] [CrossRef]
- Tappe, D.; Kern, P.; Itoh, S.; Ito, A.; Sako, Y.; Nakao, M.; Frosch, M.; Reuter, S.; Grüner, B. Close Relationship between Clinical Regression and Specific Serology in the Follow-up of Patients with Alveolar Echinococcosis in Different Clinical Stages. Am. J. Trop. Med. Hyg. 2009, 80, 792–797. [Google Scholar] [CrossRef]
- Tappe, D.; Sako, Y.; Itoh, S.; Frosch, M.; Grüner, B.; Kern, P.; Ito, A. Immunoglobulin G subclass responses to recombinant Em18 in the follow-up of patients with alveolar echinococcosis in different clinical stages. Clin. Vaccine Immunol. 2010, 17, 944–948. [Google Scholar] [CrossRef] [Green Version]
- Chauchet, A.; Grenouillet, F.; Knapp, J.; Richou, C.; Delabrousse, E.; Dentan, C.; Millon, L.; Di Martino, V.; Contreras, R.; Deconinck, E.; et al. Increased incidence and characteristics of alveolar echinococcosis in patients with immunosuppression-associated conditions. Clin. Infect. Dis. 2014, 59, 1095–1104. [Google Scholar] [CrossRef] [Green Version]
- Lachenmayer, A.; Gebbers, D.; Gottstein, B.; Candinas, D.; Beldi, G. Elevated incidence of alveolar echinococcosis in immunocompromised patients. Food Waterborne Parasitol. 2019, 16, e00060. [Google Scholar] [CrossRef]


| Variable | Result |
|---|---|
| Gender | Female 57.5%, Male 42.5% |
| Mean age | 53 years (SD = 17.9 years, 11–89 years) |
| Symptoms | No symptoms 32.3%, abdominal discomfort 48.8%, abdominal pain 40.3%, loss of weight 16.7%, fatigue 15.6%, jaundice 10.5%, fever 6.2% |
| WHO definition [13] * | possible 3.6%, probable 36.4%, confirmed 59.6% |
| PNM classification [14] | P: P0 0.4%, P1 2.9%, P2 33.1%, P3 20.1%, P4 42.7%, Px 0.8% |
| N: N0 60.9%, N1 33.3%, Nx 5.8% | |
| M: M0 87.1%, M1 9.3%, Mx 3.6% | |
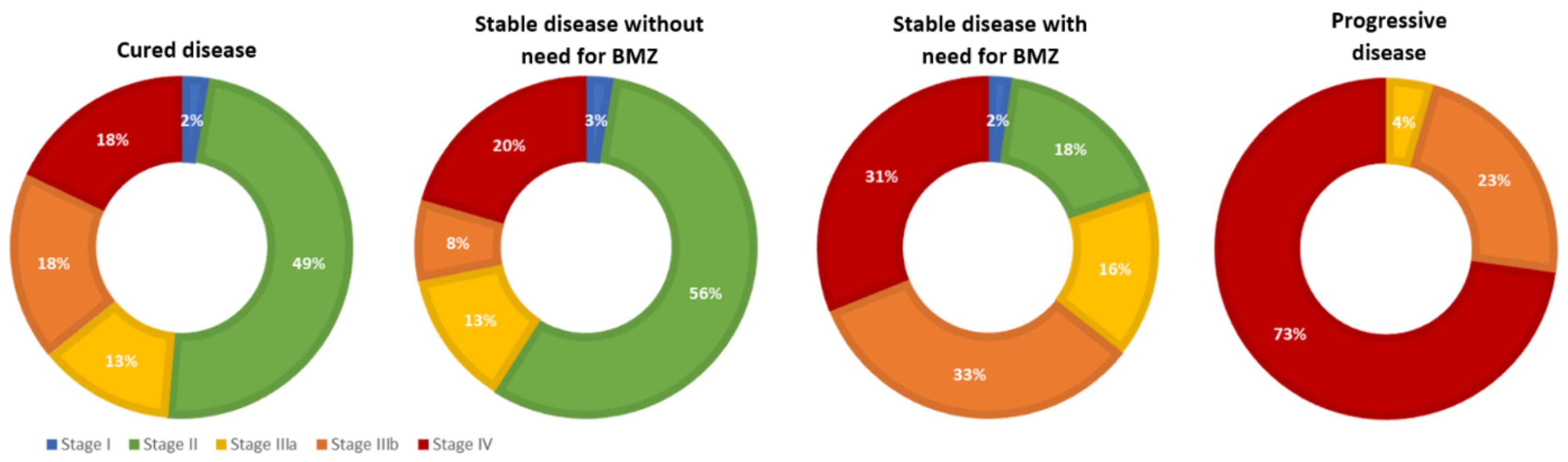
| Disease stage [14] | stage I 2.8%, stage II 26.3%, stage IIIa 14.7%, stage IIIb 23.9%, stage IV 30.9% |
| Outcome | cured 14.4%, stable disease 62.2% (47.8% with BMZ, 14.4% without BMZ for M = 45.6 months, SD = 25.8), progressive disease 5.2% |
| IgE | Ech. IgG IHA | Ech. IgG EIA | Em2+ | |
|---|---|---|---|---|
| Ech. IgG IHA | s = 0.412; p < 0.001 | |||
| Ech. IgG EIA | r = 0.211; p = 0.030 | s = 0.542; p < 0.001 | ||
| Em2+ | s = 0.442; p < 0.001 | s = 0.472; p < 0.001 | s = 0.419; p < 0.001 | |
| Size of largest lesion | r = 0.438; p < 0.001 | s = 0.489; p < 0.001 | r = 0.431; p < 0.001 | s = 0.551; p < 0.001 |
| Variable | (A) Progressive Disease | (B) Controlled Disease | ||||
|---|---|---|---|---|---|---|
| OR | CI 95% | p = | OR | CI 95% | p = | |
| Age | 0.992 | 0.964–1.021 | 0.581 | 1.003 | 0.973–1.034 | 0.831 |
| Gender | 0.670 | 0.245–1.824 | 0.433 | 0.543 | 0.180–1.633 | 0.277 |
| P—Localisation of parasite | 1.886 | 0.824–4.313 | 0.133 | 0.668 | 0.335–1.330 | 0.251 |
| N—Involvement of neighbouring organs | 3.696 | 1.173–11.653 | 0.026 | 0.616 | 0.113–3.347 | 0.575 |
| Staging (I–IV) * | 2.860 | 1.384–5.911 | 0.005 | 0.670 | 0.389–1.154 | 0.149 |
| Largest diameter of lesion | 1.017 | 1.004–1.029 | 0.007 | 0.972 | 0.949–0.996 | 0.022 |
| Morphology of lesion | 0.979 | 0.848–1.132 | 0.778 | 1.029 | 0.933–1.134 | 0.571 |
| IgE levels at first presentation | 1.000 | 1.000–1.000 | 0.822 | 1.000 | 0.998–1.001 | 0.594 |
| Echinococcus IgG EIA | 1.007 | 0.998–1.015 | 0.131 | 0.997 | 0.979–1.014 | 0.704 |
| Echinococcus Em2+ ELISA | 1.611 | 0.174–14.925 | 0.675 | 0.245 | 0.072–0.835 | 0.024 |
| γGT at first presentation | 1.000 | 0.998–1.002 | 0.733 | 0.998 | 0.992–1.004 | 0.587 |
| Clinical Outcome | Definition |
|---|---|
| Cured (at the end of follow-up) | Curative surgery performed >2 years ago, no signs of recurrent or residual AE lesions at study endpoint |
| Stable disease with need for BMZ (at the end of follow-up) |
|
| Stable disease without need for BMZ (at the end of follow-up) |
|
| Progressive disease (at any point in time during follow-up) |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peters, L.; Burkert, S.; Hagemann, J.B.; Albes, R.; Klemptner, J.; Birkle, J.; Schwaibold, E.; Siefermann, S.; Grüner, B. Initial Risk Assessment in Patients with Alveolar Echinococcosis—Results from a Retrospective Cohort Study. Pathogens 2022, 11, 557. https://doi.org/10.3390/pathogens11050557
Peters L, Burkert S, Hagemann JB, Albes R, Klemptner J, Birkle J, Schwaibold E, Siefermann S, Grüner B. Initial Risk Assessment in Patients with Alveolar Echinococcosis—Results from a Retrospective Cohort Study. Pathogens. 2022; 11(5):557. https://doi.org/10.3390/pathogens11050557
Chicago/Turabian StylePeters, Lynn, Sanne Burkert, Jürgen Benjamin Hagemann, Rasmus Albes, Jonas Klemptner, Jessica Birkle, Elias Schwaibold, Sofia Siefermann, and Beate Grüner. 2022. "Initial Risk Assessment in Patients with Alveolar Echinococcosis—Results from a Retrospective Cohort Study" Pathogens 11, no. 5: 557. https://doi.org/10.3390/pathogens11050557






