Molecular Detection and Identification of Piroplasm in Cattle from Kathmandu Valley, Nepal
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Blood Sample Collection
2.3. Microscopic Examination
2.4. Molecular Analysis
2.4.1. DNA Extraction
2.4.2. Nested PCR
2.4.3. Sequencing
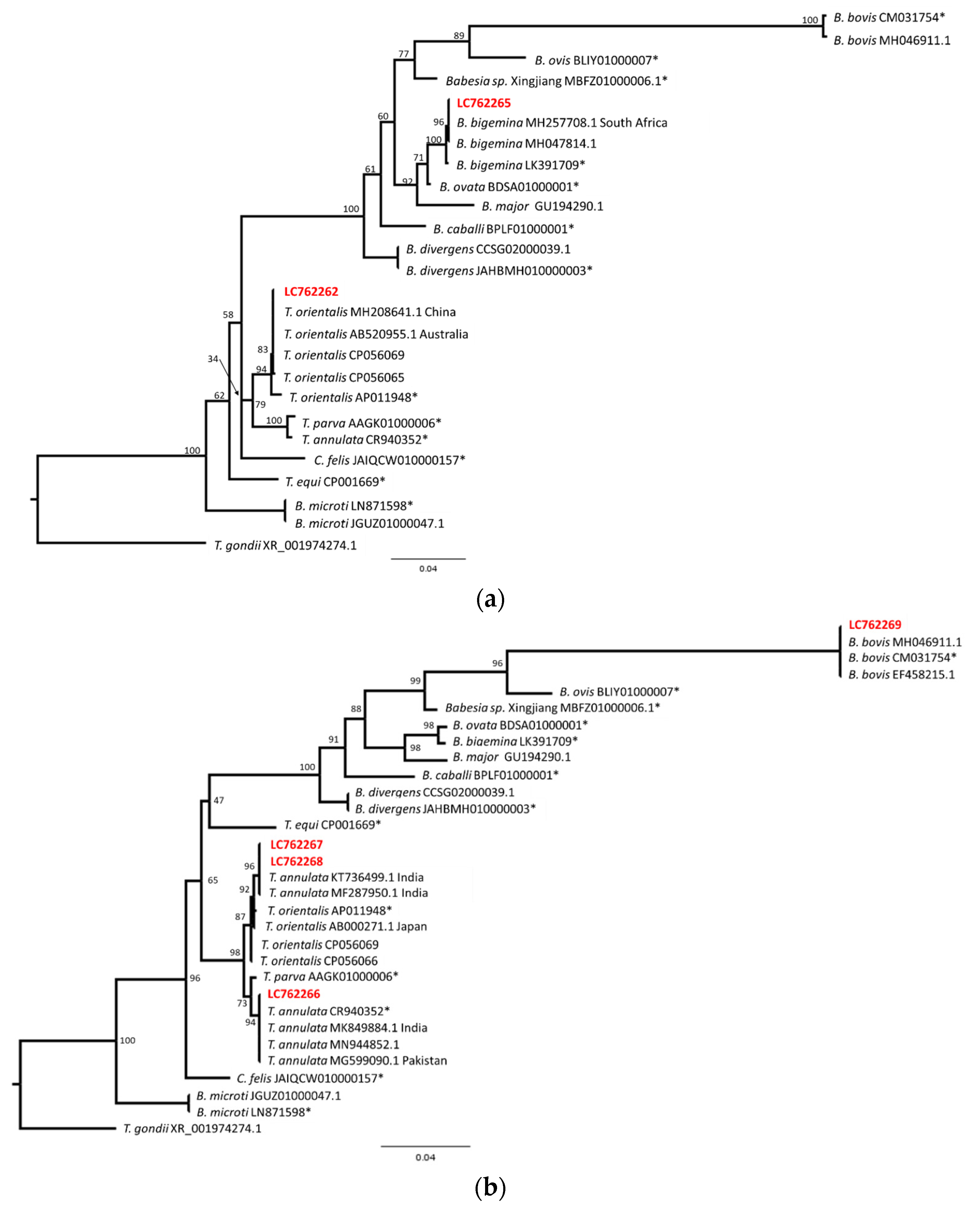
2.5. Phylogenetic Analysis
2.6. Hematological Analysis
2.7. Statistical Analysis
3. Results
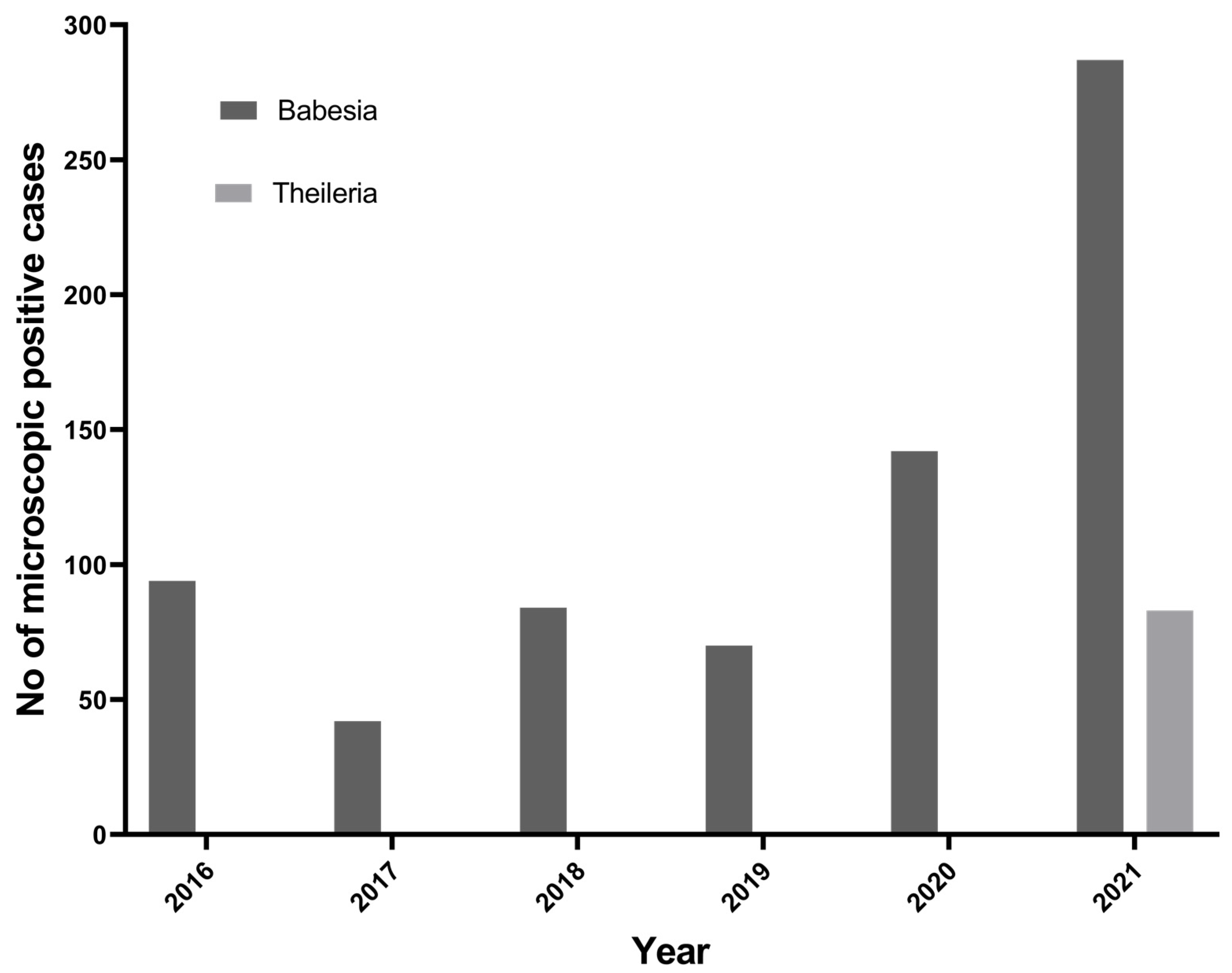
3.1. Microscopic Analysis
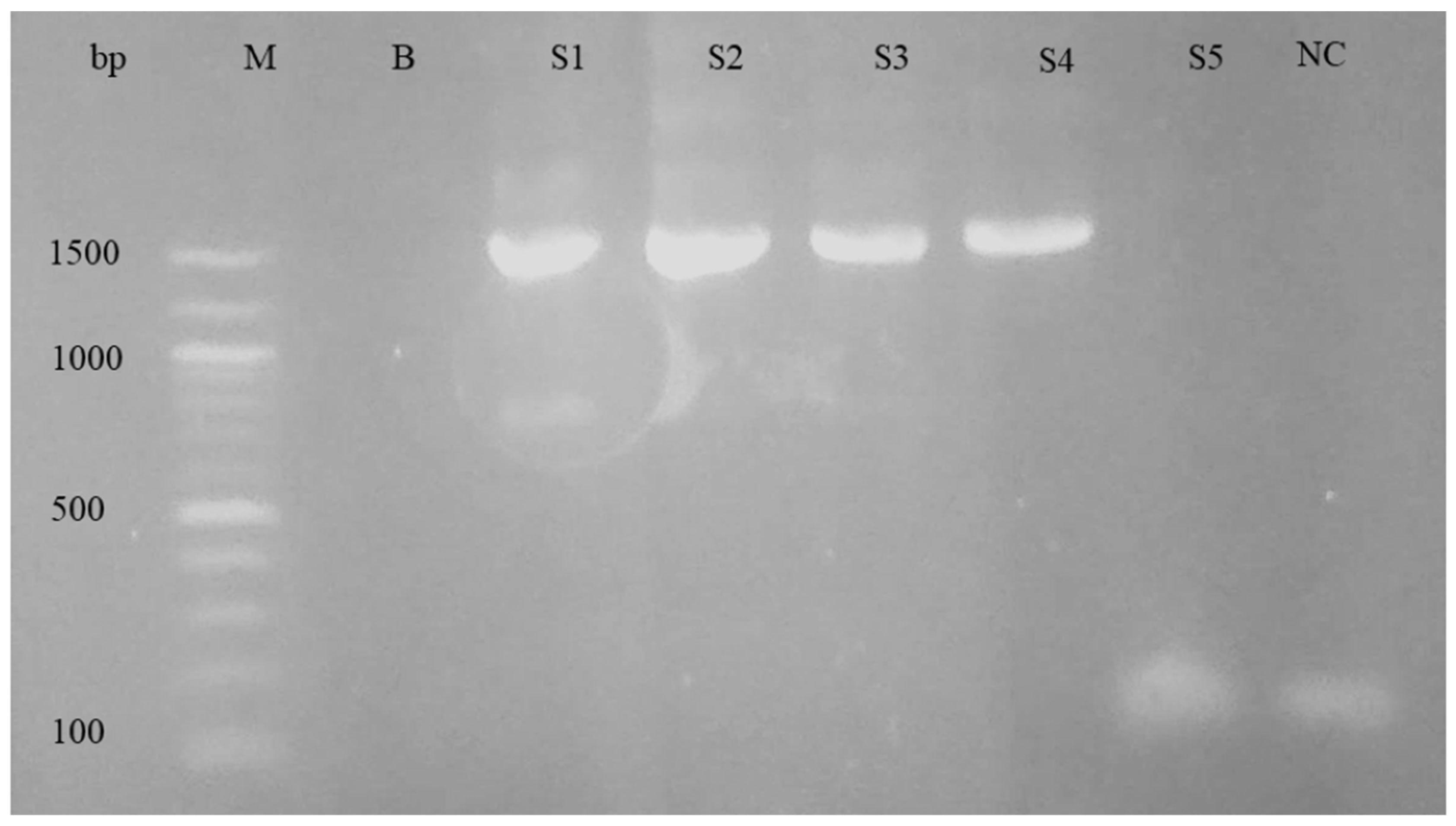
3.2. Molecular Analysis
3.3. Hematological Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GoN. Government of Nepal, Ministry of Agriculture and Livestock Development, Department of Livestock Services. Livestock Statics of Nepal, Lalitpur, Nepal, 2020/21. Available online: https://www.dls.gov.np/downloadfiles/Livestock_Statistics_of_Nepal_2077_78_1659524236-1669717523.pdf (accessed on 1 May 2023).
- Bhatta, B.R.; Kaphle, K.; Yadav, K.K. Situation of Livestock, Production and its Products in Nepal. Arch. Vet. Sci. Med. 2018, 1, 1–8. [Google Scholar]
- Poudel, U.; Dahal, U.; Upadhyaya, N.; Chaudhari, S.; Dhakal, S. Livestock and poultry production in Nepal and current status of vaccine development. Vaccines 2020, 8, 332. [Google Scholar] [CrossRef]
- Dhital, B.; Shrestha, S.; Kaphle, K.; Pudasaini, R. Distribution of the cattle ticks from mid hills to plains of Nepal. J. Agric. Nat. Resour. 2018, 1, 197–205. [Google Scholar] [CrossRef]
- Bohara, T.; Shrestha, S. A Study on Cattle Tick and Tick Borne Pathogens of Midwestern Nepal. Nepal. Vet. J 2016, 33, 23–27. [Google Scholar]
- Johansson, M.; Mysterud, A.; Flykt, A. Livestock owners’ worry and fear of tick-borne diseases. Parasites Vectors 2020, 13, 331. [Google Scholar] [CrossRef] [PubMed]
- MoALD. 2021 Statistical Information On Nepalese Agriculture (2077/78). Publ. Nepal. Data Portal 2021, 73, 274. [Google Scholar]
- Słodki, J.; Jasik, K.P.; Kepa, M.; Idzik, D.; Wojtyczka, R.D. Tick-transmitted diseases caused by apicomplexa. Acta Protozool. 2011, 50, 155–161. [Google Scholar]
- Andersson, M.O.; Tolf, C.; Tamba, P.; Stefanache, M.; Radbea, G.; Rubel, F.; Waldenström, J.; Dobler, G.; Chițimia-Dobler, L. Babesia, Theileria, and Hepatozoon species in ticks infesting animal hosts in Romania. Parasitol. Res. 2017, 116, 2291–2297. [Google Scholar] [CrossRef]
- Patterson, C. Veterinary Medicine: A Textbook of the Diseases of Cattle, Horses, Sheep, Pigs, and Goats, Volumes 1 and 2. Can. Vet. J. 2017, 58, 1116. [Google Scholar]
- Ijaz, M.; Khan, M.S.; Avais, M.; Ashraf, K.; Ali, M.M.; Khan, M.Z.U. Infection rate and chemotherapy of various helminthes in diarrhoeic sheep in and around Lahore. J. Anim. Plant Sci. 2009, 28, 167–170. [Google Scholar]
- Mishra, K. Impediments in the Agriculture Sector of Nepal; Nepal Economic Forum: Lalitpur, Nepal, 2023. [Google Scholar]
- Thapa, R.B.; Murayama, Y. Scenario based urban growth allocation in Kathmandu Valley, Nepal. Landsc. Urban Plan. 2012, 105, 140–148. [Google Scholar] [CrossRef]
- Masatani, T.; Hayashi, K.; Andoh, M.; Tateno, M.; Endo, Y.; Asada, M.; Kusakisako, K.; Tanaka, T.; Gokuden, M.; Hozumi, N.; et al. Detection and molecular characterization of Babesia, Theileria, and Hepatozoon species in hard ticks collected from Kagoshima, the southern region in Japan. Ticks Tick-Borne Dis. 2017, 8, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, M.; Khatri-Chhetri, M.; Poudel, R.C.; Maharjan, J.; Prakash Dumre, S.; Das Manandhar, K.; Pandey, B.D.; Pun, S.B.; Pandey, K. Molecular evidence supports the expansion of visceral leishmaniasis towards non-program districts of Nepal. BMC Infect. Dis. 2019, 19, 444. [Google Scholar] [CrossRef] [PubMed]
- Dohoo, I.; Martin, W.; Stryhn, H. Eterinary Epidemiologic Research; University of Prince Edward Island: Harlottetown, PE, Canada, 2003. [Google Scholar]
- Ratala, D.K.; Singh, U.M.; Manandhar, P. Babeiosis in cattle—A case Report. Bull. Vet. Sc. AH Nepal 1989, 17–18, 35–36. [Google Scholar]
- Shrestha, S.P.; Singh, U.M. Identification of ticks in relation to blood protozoan diseases in cattle. In Proceedings of the fourth National Workshop on Livestock and Fisheries Research, Khumaltar, Nepal, 24–26 April 2000; pp. 165–167. [Google Scholar]
- Khankhawash, G. Haemo-Protozoan Parasites of Cattle in Gorkha Municipality-7, Gorkha, Nepal. Master Thesis, Central Department of Zoology, Kirtipur, Nepal, 2018. [Google Scholar]
- Deo, S.N.; Neupane, M. Study on Some Epidemiological Aspects and Treatment of Bovine Piroplasmosis in Morang District. Ann. Tech. Rep. 2002, 7–21. [Google Scholar]
- Thakuri, K.; Mahato, S.; Thakur, R. Diseases of cattle and buffaloes in the Koshi hills of Nepal: A retrospective study. Vet. Rev. 1992, 7, 41–46. [Google Scholar]
- RVDL. Regional Veterinary Diagnostic Laboratory; Annual Report; RVDL: Biratnagar, Nepal, 1996. [Google Scholar]
- Acharya, K.; Pradhan, S.M. Study of blood protozoan diseases with special references to Theileriosis in eastern region of Nepal. Bull. Vet. Sc. AH Nepal. 1996, 24, 55–58. [Google Scholar]
- Yadav, S. Prevalence of Blood Protozoan Parasites of Cattle, Buffaloes and Goats of Three Vdcs of Siraha District, Nepal. Master Thesis, Central Department of Zoology, Kirtipur, Nepal, 2015. [Google Scholar]
- Debbarma, A.; Pandit, S.; Jas, R.; Baidya, S.; Chandra Mandal, S.; Sarathi Jana, P.; Das, M. Prevalence of tick-borne haemoparasitic diseases in cattle of West Bengal, India. Biol. Rhythm Res. 2020, 51, 310–317. [Google Scholar] [CrossRef]
- Pradeep, R.K.; Nimisha, M.; Sruthi, M.K.; Vidya, P.; Amrutha, B.M.; Kurbet, P.S.; Kumar, K.G.A.; Varghese, A.; Deepa, C.K.; Dinesh, C.N.; et al. Molecular characterization of South Indian field isolates of bovine Babesia spp. and Anaplasma spp. Parasitol. Res. 2019, 118, 617–630. [Google Scholar] [CrossRef]
- Mosqueda, J.; Olvera-Ramirez, A.; Aguilar-Tipacamu, G.; Canto, G.J. Current Advances in Detection and Treatment of Babesiosis. Curr. Med. Chem. 2012, 19, 1504–1518. [Google Scholar] [CrossRef]
- Nayel, M.; El-Dakhly, K.M.; Aboulaila, M.; Elsify, A.; Hassan, H.; Ibrahim, E.; Salama, A.; Yanai, T. The use of different diagnostic tools for Babesia and Theileria parasites in cattle in Menofia, Egypt. Parasitol. Res. 2012, 111, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Hüe, T.; Graille, M.; Mortelecque, A.; Desoutter, D.; Delathière, J.; Marchal, C.; Teurlai, M.; Barré, N. Diagnostic methods used to monitor an outbreak of babesiosis (Babesia bovis) in a herd of feral cattle in New Caledonia. Aust. Vet. J. 2013, 91, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Kolte, S.W.; Larcombe, S.D.; Jadhao, S.G.; Magar, S.P.; Warthi, G.; Kurkure, N.V.; Glass, E.J.; Shiels, B.R. PCR diagnosis of tick-borne pathogens in Maharashtra state, India indicates fitness cost associated with carrier infections is greater for crossbreed than native cattle breeds. PLoS ONE 2017, 12, e0174595. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.J.; Raut, S.; Singh, R.P.; Mishra, P.; Hossain, M.S.; Dey, A.R.; Kabir, A.; Anisuzzaman; Talukder, M.H.; Shahiduzzaman, M. Molecular detection of Babesia and Theileria from crossbred cattle in Sirajganj and Rangpur districts of Bangladesh. Vet. Med. Sci. 2022, 9, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Ashraf, K.; Anwar, N.; Jamal, M.A.; Naeem, H.; Ahmad, N.; Rahaman, A.U. Diagnosis of Babesia Bovis Infection in Indigenous and Crossbred Cattlewith Comparison Between Conventional and Molecular Diagnostic Techniques. J. Infect. Mol. Biol. 2017, 5, 1–6. [Google Scholar]
- Alam Tufani, N.; Ul Haq, A.; Tufani, I.N.; Malik, I.H.; Hussain, I.S.; Razaq Bhat, R.; Amin, I.U.; Nabi, I.S.; Tufani, N.; Malik, H.; et al. Cross sectional study on prevalence of ovine babesiosis in different breeds of Kashmir valley. J. Entomol. Zool. Stud. 2017, 5, 1492–1496. [Google Scholar]
- Muraleedharan, K. Babesia and Babesiosis in Livestock of Karnataka State, India—An Overview. Vet. Res. Int. 2015, 3, 81–88. [Google Scholar]
- Kakati, P.; Sarmah, P.C.; Ray, D.; Bhattacharjee, K.; Sharma, R.K.; Barkalita, L.M.; Sarma, D.K.; Baishya, B.C.; Borah, P.; Stanley, B. Emergence of oriental theileriosis in cattle and its transmission through Rhipicephalus (Boophilus) microplus in Assam, India. Vet. World 2015, 8, 1099–1104. [Google Scholar] [CrossRef]
- Agrawal, V.; Das, G.; Jaiswal, A.; Jayraw, A.K.; Jatav, G.P.; Shakya, M.; Jamara, N. First Report on Molecular Identification of Babesia bigemina in a Nervous Signs Evident Naturally Infected Holstein-Friesian Cattle from Central India. Indian J. Anim. Res. 2021, 57, 377–380. [Google Scholar] [CrossRef]
- Sivakumar, T.; Kothalawala, H.; Abeyratne, S.A.E.; Vimalakumar, S.C.; Meewewa, A.S.; Hadirampela, D.T.; Puvirajan, T.; Sukumar, S.; Kuleswarakumar, K.; Chandrasiri, A.D.N.; et al. A PCR-based survey of selected Babesia and Theileria parasites in cattle in Sri Lanka. Vet. Parasitol. 2012, 190, 263–267. [Google Scholar] [CrossRef]
- Selim, A.M.; Senapati, S.K.; Das, M.; Mishra, C.; Patra, R.C.; Panda, S.K. Molecular, epidemiological and haematological evaluation in Theileria orientalis infected cattle from an endemic region in India. Anim. Biotechnol. 2021, 32, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Parveen, A.; Ashraf, S.; Aktas, M.; Ozubek, S.; Iqbal, F. Molecular epidemiology of Theileria annulata infection of cattle in Layyah District, Pakistan. Exp. Appl. Acarol. 2021, 83, 461–473. [Google Scholar] [CrossRef]
- Selim, A.M.; Das, M.; Senapati, S.K.; Jena, G.R.; Mishra, C.; Nath, I.; Senapati, S.; Sethi, M. Molecular detection of Theileria annulata infection in cattle by conventional PCR and quantitative real time PCR in India. J. Parasit. Dis. 2021, 45, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Magdy Selim, A.; Das, M.; Kumar Senapati, S.; Rani Jena, G.; Mishra, C.; Mohanty, B.; Kumar Panda, S.; Chandra Patra, R. Molecular detection of three genotypes of Theileria orientalis in crossbred jersey cattle in Odisha, India. J. Entomol. Zool. Stud. 2020, 8, 22–26. [Google Scholar]
- Lamichhane, U.; Sc, B.V.; Basnet, H.B. A study on cattle tick of Chitwan district of Nepal in different seasons. Int. J. Vet. Sci. Anim. Husb. 2020, 5, 36–38. [Google Scholar]
- Gupta, V.; Gupta, R.; Shrestha, S.P. Infectivity of Theileria annulata in Hyalomma ticks of Eastern Terai districts, Nepal. Nepal. J. Zool. 2013, 1, 15–23. [Google Scholar]
- Niu, Q.; Bonsergent, C.; Rogniaux, H.; Guan, G.; Malandrin, L.; Moreau, E. RAP-1a is the main rhoptry-associated-protein-1 (RAP-1) recognized during infection with Babesia sp. BQ1 (Lintan) (B. motasi-like phylogenetic group), a pathogen of sheep in China. Vet. Parasitol. 2016, 232, 48–57. [Google Scholar] [CrossRef]
- Maharana, B.R.; Kumar, B.; Prasad, A.; Patbandha, T.K.; Sudhakar, N.R.; Joseph, J.P.; Patel, B.R. Prevalence and assessment of risk factors for haemoprotozoan infections in cattle and buffaloes of South-West Fujarat, India. Indian J. Anim. Res. 2016, 50, 733–739. [Google Scholar]
- Ananda, K.J.; D’Souza, P.E.; Puttalakshmamma, G.C. Prevalence of haemoprotozoan diseases in crossbred cattle in Bangalore north. Vet. World 2009, 2, 15–16. [Google Scholar] [CrossRef]
- Zeb, J.; Song, B.; Aziz, M.U.; Hussain, S.; Zarin, R.; Sparagano, O. Diversity and Distribution of Theileria Species and Their Vectors in Ruminants from India, Pakistan and Bangladesh. Diversity 2022, 14, 82. [Google Scholar] [CrossRef]
- Muwel, N.; Verma, R.; Das, G.; Kumar, S.; Nath, S. Co-infection of Babesia sp. and Theileria sp. In a Holstein Friesian crossbred calf-A case report. J. Vet. Parasitol. 2021, 35, 137–139. [Google Scholar] [CrossRef]
- Zhou, M.; Cao, S.; Sevinc, F.; Sevinc, M.; Ceylan, O.; Ekici, S.; Jirapattharasate, C.; Moumouni, P.F.A.; Liu, M.; Wang, G.; et al. Molecular detection and genetic characterization of Babesia, Theileria and Anaplasma amongst apparently healthy sheep and goats in the central region of Turkey. Ticks Tick-Borne Dis. 2017, 8, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Kaur, R.; Yadav, A.; Rafiqi, S.I.; Godara, R.; Sudan, V.; Chakraborty, D.; Katoch, R. Epidemiology, haematology and molecular characterization of haemoprotozoon and rickettsial organisms causing infections in cattle of Jammu region, North India. BMC Vet. Res. 2021, 17, 219. [Google Scholar] [CrossRef]
- Aulakh, G.S.; Singla, L.D.; Kaur, P.; Alka. Bovine babesiosis due to Babesia bigemina: Haematobiochemical and therapeutic studies. Indian J. Anim. Sci. 2005, 75, 617–622. [Google Scholar]


| Microscopic | PCR | ||
|---|---|---|---|
| Positive (n) | Negative (n) | Total, N (%) | |
| Positive | 32 | 13 | 45 (42.5%) |
| Negative | 24 | 17 | 61 (57.5%) |
| Total | 56 (52.8%) | 50 (47.2) | 106 |
| Accession No. | Sequence Length | Result of BLAST Search Species (Accession No, Identity (%)) | Indicated Species | |
|---|---|---|---|---|
| 1 | LC762262 | 990 | T. orientalis (MH208641.1, AB520955.1 and others, 990/990 (100)) | T. orientalis |
| 2 | LC762263 | 428 | T. orientalis/sergenti/buffeli (MH208641.1, MT355456.1, MH327775.1 and others, 427/428 (99.77%)) | T. orientalis |
| 3 | LC762264 | 464 | T. annulata (MF287950.1 and others, 462/464 (99.57%)), T. orientalis (LC576818.1 and others, 462/464 (99.57%)) | T. annulata or T. orientalis |
| 4 | LC762265 | 919 | B. bigemina (MH047814.1, 918/919 (99.89%) followed by LC645217.1 and others 917/919 (99.78%)) | B. bigemina |
| 5 | LC762266 | 918 | T. annulata (MT341858.1, MG599090.1 and others, 918/918 (100)) | T. annulata |
| 6 | LC762267 | 901 | T. annulata (MF287950.1 and others, 901/901 (100%)), T. orientalis (LC576818.1 and others, 901/901 (100%)) | T. annulata or T. orientalis |
| 7 | LC762268 | 901 | T. annulata (MF287950.1 and others, 901/901 (100%)), T. orientalis (LC576818.1 and others, 901/901 (100%)) | T. annulata or T. orientalis |
| 8 | LC762269 | 893 | B. bovis (MH046911.1, EF458215.1 and others, 893/893 (100%)) | B. bovis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhakal, M.; Gompo, T.R.; Devkota, P.; Kafle, S.C.; Subedi, J.R.; Gong, H.; Arima, H.; Culleton, R.; Asada, M.; Pandey, K. Molecular Detection and Identification of Piroplasm in Cattle from Kathmandu Valley, Nepal. Pathogens 2023, 12, 1045. https://doi.org/10.3390/pathogens12081045
Dhakal M, Gompo TR, Devkota P, Kafle SC, Subedi JR, Gong H, Arima H, Culleton R, Asada M, Pandey K. Molecular Detection and Identification of Piroplasm in Cattle from Kathmandu Valley, Nepal. Pathogens. 2023; 12(8):1045. https://doi.org/10.3390/pathogens12081045
Chicago/Turabian StyleDhakal, Medhavi, Tulsi Ram Gompo, Prakash Devkota, Sharmila Chapagain Kafle, Janak Raj Subedi, Haiyan Gong, Hiroaki Arima, Richard Culleton, Masahito Asada, and Kishor Pandey. 2023. "Molecular Detection and Identification of Piroplasm in Cattle from Kathmandu Valley, Nepal" Pathogens 12, no. 8: 1045. https://doi.org/10.3390/pathogens12081045
APA StyleDhakal, M., Gompo, T. R., Devkota, P., Kafle, S. C., Subedi, J. R., Gong, H., Arima, H., Culleton, R., Asada, M., & Pandey, K. (2023). Molecular Detection and Identification of Piroplasm in Cattle from Kathmandu Valley, Nepal. Pathogens, 12(8), 1045. https://doi.org/10.3390/pathogens12081045








