Transfection Models to Investigate Plasmodium vivax-Type Dormant Liver Stage Parasites
Abstract
1. Introduction
2. Liver Stage Models for P. vivax
2.1. P. vivax In Vivo Liver Stage Models
2.2. P. vivax In Vitro Liver Stage Platforms
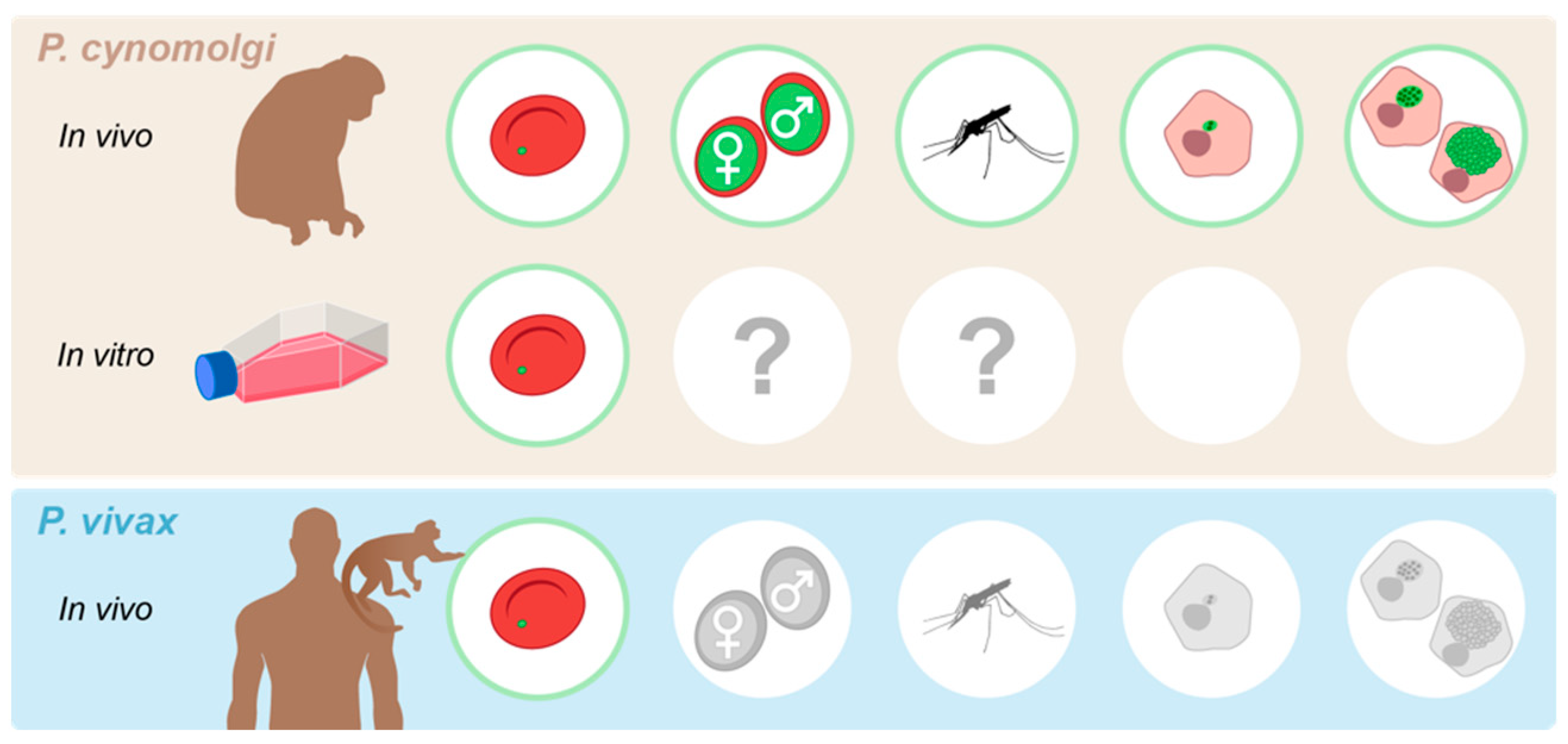
2.3. P. cynomolgi Liver Stage Research Platforms
3. Transfection Technology to Study Hypnozoite Biology
3.1. P. vivax Genetic Engineering Technology
3.2. P. vivax Hypnozoite Research Benefits and Limitations
3.3. P. cynomolgi Genetic Engineering Technology
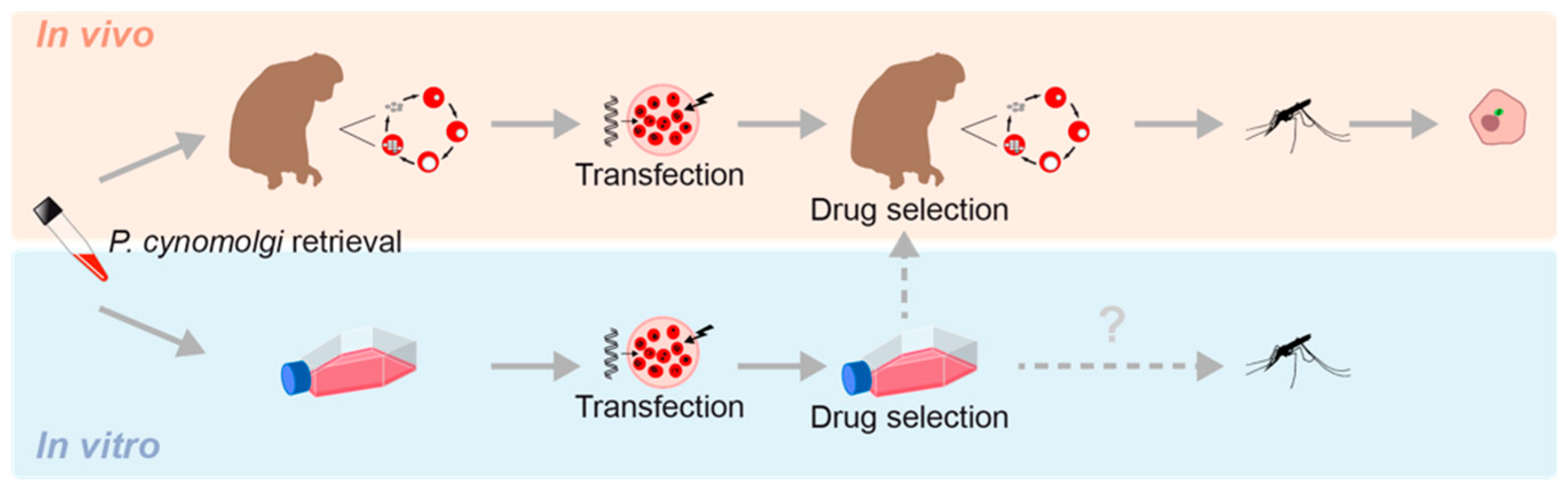
3.3.1. P. cynomolgi In Vivo Genetic Engineering Technology
3.3.2. Application of P. cynomolgi Vivo-Derived Transgenic Parasites to the Study of Hypnozoite Biology
3.3.3. P. cynomolgi Vitro Genetic Engineering Technology
3.4. P. cynomolgi Hypnozoite Research Benefits and Limitations
4. Conclusions and Outlook
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). World Malaria Report 2022. Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2022 (accessed on 17 July 2023).
- Battle, K.E.; Lucas, T.C.D.; Nguyen, M.; Howes, R.E.; Nandi, A.K.; Twohig, K.A.; Pfeffer, D.A.; Cameron, E.; Rao, P.C.; Casey, D.; et al. Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000–17: A spatial and temporal modelling study. Lancet 2019, 394, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Baird, J.K. African Plasmodium vivax malaria improbably rare or benign. Trends Parasitol. 2022, 38, 683–696. [Google Scholar] [CrossRef] [PubMed]
- Quaye, I.K.; Aleksenko, L.; Oeuvray, C.; Yewhalaw, D.; Duah, N.; Gyan, B.; Haiyambo, D.H.; Dongho, G.B.D.; Torgby, R.A.; Amoah, L.; et al. The Pan African Vivax and Ovale Network (PAVON): Refocusing on Plasmodium vivax, ovale and asymptomatic malaria in sub-Saharan Africa. Parasitol. Int. 2021, 84, 102415. [Google Scholar] [CrossRef]
- Zimmerman, P.A. Plasmodium vivax Infection in Duffy-Negative People in Africa. Am. J. Trop. Med. Hyg. 2017, 97, 636–638. [Google Scholar] [CrossRef]
- Baird, J.K. Evidence and implications of mortality associated with acute Plasmodium vivax malaria. Clin. Microbiol. Rev. 2013, 26, 36–57. [Google Scholar] [CrossRef] [PubMed]
- Price, R.N.; Tjitra, E.; Guerra, C.A.; Yeung, S.; White, N.J.; Anstey, N.M. Vivax malaria: Neglected and not benign. Am. J. Trop. Med. Hyg. 2007, 77, 79–87. [Google Scholar] [CrossRef]
- Phyo, A.P.; Dahal, P.; Mayxay, M.; Ashley, E.A. Clinical impact of vivax malaria: A collection review. PLoS Med. 2022, 19, e1003890. [Google Scholar] [CrossRef]
- Bantuchai, S.; Imad, H.; Nguitragool, W. Plasmodium vivax gametocytes and transmission. Parasitol. Int. 2022, 87, 102497. [Google Scholar] [CrossRef]
- Krotoski, W.A.; Collins, W.E.; Bray, R.S.; Garnham, P.C.; Cogswell, F.B.; Gwadz, R.W.; Killick-Kendrick, R.; Wolf, R.; Sinden, R.; Koontz, L.C.; et al. Demonstration of hypnozoites in sporozoite-transmitted Plasmodium vivax infection. Am. J. Trop. Med. Hyg. 1982, 31, 1291–1293. [Google Scholar] [CrossRef]
- Hemmer, C.J.; Holst, F.G.; Kern, P.; Chiwakata, C.B.; Dietrich, M.; Reisinger, E.C. Stronger host response per parasitized erythrocyte in Plasmodium vivax or ovale than in Plasmodium falciparum malaria. Trop. Med. Int. Health 2006, 11, 817–823. [Google Scholar] [CrossRef]
- Moreno-Perez, D.A.; Ruiz, J.A.; Patarroyo, M.A. Reticulocytes: Plasmodium vivax target cells. Biol. Cell 2013, 105, 251–260. [Google Scholar] [CrossRef]
- White, N.J. Why Do Some Primate Malarias Relapse? Trends Parasitol. 2016, 32, 918–920. [Google Scholar] [CrossRef] [PubMed]
- White, N.J. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar. J. 2011, 10, 297. [Google Scholar] [CrossRef] [PubMed]
- Kho, S.; Qotrunnada, L.; Leonardo, L.; Andries, B.; Wardani, P.A.I.; Fricot, A.; Henry, B.; Hardy, D.; Margyaningsih, N.I.; Apriyanti, D.; et al. Hidden Biomass of Intact Malaria Parasites in the Human Spleen. N. Engl. J. Med. 2021, 384, 2067–2069. [Google Scholar] [CrossRef]
- Obaldia, N., 3rd; Meibalan, E.; Sa, J.M.; Ma, S.; Clark, M.A.; Mejia, P.; Moraes Barros, R.R.; Otero, W.; Ferreira, M.U.; Mitchell, J.R.; et al. Bone Marrow Is a Major Parasite Reservoir in Plasmodium vivax Infection. mBio 2018, 9, e00625-18. [Google Scholar] [CrossRef] [PubMed]
- Markus, M.B. How does primaquine prevent Plasmodium vivax malarial recurrences? Trends Parasitol. 2022, 38, 924–925. [Google Scholar] [CrossRef] [PubMed]
- Markus, M.B. Putative Contribution of 8-Aminoquinolines to Preventing Recrudescence of Malaria. Trop. Med. Infect Dis. 2023, 8, 278. [Google Scholar] [CrossRef]
- Burgoine, K.L.; Bancone, G.; Nosten, F. The reality of using primaquine. Malar. J. 2010, 9, 376. [Google Scholar] [CrossRef][Green Version]
- Douglas, N.M.; Piera, K.A.; Rumaseb, A.; Ley, B.; Anstey, N.M.; Price, R.N. Primaquine-induced Severe Hemolysis in the Absence of Concomitant Malaria: Effects on G6PD Activity and Renal Function. Am. J. Trop. Med. Hyg. 2023, 108, 76–80. [Google Scholar] [CrossRef]
- Howes, R.E.; Battle, K.E.; Satyagraha, A.W.; Baird, J.K.; Hay, S.I. G6PD deficiency: Global distribution, genetic variants and primaquine therapy. Adv. Parasitol. 2013, 81, 133–201. [Google Scholar] [CrossRef]
- Howes, R.E.; Piel, F.B.; Patil, A.P.; Nyangiri, O.A.; Gething, P.W.; Dewi, M.; Hogg, M.M.; Battle, K.E.; Padilla, C.D.; Baird, J.K.; et al. G6PD deficiency prevalence and estimates of affected populations in malaria endemic countries: A geostatistical model-based map. PLoS Med. 2012, 9, e1001339. [Google Scholar] [CrossRef] [PubMed]
- Baird, J.K.; Battle, K.E.; Howes, R.E. Primaquine ineligibility in anti-relapse therapy of Plasmodium vivax malaria: The problem of G6PD deficiency and cytochrome P-450 2D6 polymorphisms. Malar. J. 2018, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Cox, F.E. History of the discovery of the malaria parasites and their vectors. Parasit. Vectors 2010, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Cogswell, F.B.; Krotoski, W.A.; Hollingdale, M.R.; Gwadz, R.W. Identification of hypnozoites and tissue schizonts of Plasmodium vivax and P. cynomolgi by the immunoperoxidase method. Am. J. Trop. Med. Hyg. 1983, 32, 1454–1455. [Google Scholar] [CrossRef]
- Lover, A.A.; Baird, J.K.; Gosling, R.; Price, R.N. Malaria Elimination: Time to Target All Species. Am. J. Trop. Med. Hyg. 2018, 99, 17–23. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Technical Strategy for Malaria 2016–2030. 2015. Available online: https://www.who.int/docs/default-source/documents/global-technical-strategy-for-malaria-2016-2030.pdf (accessed on 23 July 2023).
- van Dijk, M.R.; Waters, A.P.; Janse, C.J. Stable transfection of malaria parasite blood stages. Science 1995, 268, 1358–1362. [Google Scholar] [CrossRef]
- Wu, Y.; Sifri, C.D.; Lei, H.H.; Su, X.Z.; Wellems, T.E. Transfection of Plasmodium falciparum within human red blood cells. Proc. Natl. Acad. Sci. USA 1995, 92, 973–977. [Google Scholar] [CrossRef]
- Kafsack, B.F.; Rovira-Graells, N.; Clark, T.G.; Bancells, C.; Crowley, V.M.; Campino, S.G.; Williams, A.E.; Drought, L.G.; Kwiatkowski, D.P.; Baker, D.A.; et al. A transcriptional switch underlies commitment to sexual development in malaria parasites. Nature 2014, 507, 248–252. [Google Scholar] [CrossRef]
- Sinha, A.; Hughes, K.R.; Modrzynska, K.K.; Otto, T.D.; Pfander, C.; Dickens, N.J.; Religa, A.A.; Bushell, E.; Graham, A.L.; Cameron, R.; et al. A cascade of DNA-binding proteins for sexual commitment and development in Plasmodium. Nature 2014, 507, 253–257. [Google Scholar] [CrossRef]
- Cowman, A.F.; Baldi, D.L.; Healer, J.; Mills, K.E.; O’Donnell, R.A.; Reed, M.B.; Triglia, T.; Wickham, M.E.; Crabb, B.S. Functional analysis of proteins involved in Plasmodium falciparum merozoite invasion of red blood cells. FEBS Lett. 2000, 476, 84–88. [Google Scholar] [CrossRef]
- Murphy, S.C.; Vaughan, A.M.; Kublin, J.G.; Fishbauger, M.; Seilie, A.M.; Cruz, K.P.; Mankowski, T.; Firat, M.; Magee, S.; Betz, W.; et al. A genetically engineered Plasmodium falciparum parasite vaccine provides protection from controlled human malaria infection. Sci. Transl. Med. 2022, 14, eabn9709. [Google Scholar] [CrossRef] [PubMed]
- Roestenberg, M.; Walk, J.; van der Boor, S.C.; Langenberg, M.C.C.; Hoogerwerf, M.A.; Janse, J.J.; Manurung, M.; Yap, X.Z.; Garcia, A.F.; Koopman, J.P.R.; et al. A double-blind, placebo-controlled phase 1/2a trial of the genetically attenuated malaria vaccine PfSPZ-GA1. Sci. Transl. Med. 2020, 12, eaaz5629. [Google Scholar] [CrossRef] [PubMed]
- Swann, J.; Corey, V.; Scherer, C.A.; Kato, N.; Comer, E.; Maetani, M.; Antonova-Koch, Y.; Reimer, C.; Gagaring, K.; Ibanez, M.; et al. High-Throughput Luciferase-Based Assay for the Discovery of Therapeutics That Prevent Malaria. ACS Infect. Dis. 2016, 2, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Jongco, A.M.; Ting, L.M.; Thathy, V.; Mota, M.M.; Kim, K. Improved transfection and new selectable markers for the rodent malaria parasite Plasmodium yoelii. Mol. Biochem. Parasitol. 2006, 146, 242–250. [Google Scholar] [CrossRef]
- Kocken, C.H.; van der Wel, A.; Thomas, A.W. Plasmodium cynomolgi: Transfection of blood-stage parasites using heterologous DNA constructs. Exp. Parasitol. 1999, 93, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Reece, S.E.; Thompson, J. Transformation of the rodent malaria parasite Plasmodium chabaudi and generation of a stable fluorescent line PcGFPCON. Malar. J. 2008, 7, 183. [Google Scholar] [CrossRef]
- van der Wel, A.M.; Tomas, A.M.; Kocken, C.H.; Malhotra, P.; Janse, C.J.; Waters, A.P.; Thomas, A.W. Transfection of the primate malaria parasite Plasmodium knowlesi using entirely heterologous constructs. J. Exp. Med. 1997, 185, 1499–1503. [Google Scholar] [CrossRef]
- Moraes Barros, R.R.; Straimer, J.; Sa, J.M.; Salzman, R.E.; Melendez-Muniz, V.A.; Mu, J.; Fidock, D.A.; Wellems, T.E. Editing the Plasmodium vivax genome, using zinc-finger nucleases. J. Infect. Dis. 2015, 211, 125–129. [Google Scholar] [CrossRef]
- Pfahler, J.M.; Galinski, M.R.; Barnwell, J.W.; Lanzer, M. Transient transfection of Plasmodium vivax blood stage parasites. Mol. Biochem. Parasitol. 2006, 149, 99–101. [Google Scholar] [CrossRef]
- Kocken, C.H.; Ozwara, H.; van der Wel, A.; Beetsma, A.L.; Mwenda, J.M.; Thomas, A.W. Plasmodium knowlesi provides a rapid in vitro and in vivo transfection system that enables double-crossover gene knockout studies. Infect. Immun. 2002, 70, 655–660. [Google Scholar] [CrossRef]
- Ward, K.E.; Christensen, P.; Racklyeft, A.; Dhingra, S.K.; Chua, A.C.Y.; Remmert, C.; Suwanarusk, R.; Matheson, J.; Blackman, M.J.; Kaneko, O.; et al. Integrative genetic manipulation of Plasmodium cynomolgi reveals MultiDrug Resistance-1 Y976F associated with increased in vitro susceptibility to mefloquine. J. Infect. Dis. 2022, 227, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Ngotho, P.; Soares, A.B.; Hentzschel, F.; Achcar, F.; Bertuccini, L.; Marti, M. Revisiting gametocyte biology in malaria parasites. FEMS Microbiol. Rev. 2019, 43, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Bertschi, N.L.; Voorberg-van der Wel, A.; Zeeman, A.M.; Schuierer, S.; Nigsch, F.; Carbone, W.; Knehr, J.; Gupta, D.K.; Hofman, S.O.; van der Werff, N.; et al. Transcriptomic analysis reveals reduced transcriptional activity in the malaria parasite Plasmodium cynomolgi during progression into dormancy. Elife 2018, 7, e41081. [Google Scholar] [CrossRef] [PubMed]
- Toenhake, C.G.; Voorberg-van der Wel, A.; Wu, H.; Kanyal, A.; Nieuwenhuis, I.G.; van der Werff, N.M.; Hofman, S.O.; Zeeman, A.M.; Kocken, C.H.M.; Bartfai, R. Epigenetically regulated RNA-binding proteins signify malaria hypnozoite dormancy. Cell Rep. 2023, 42, 112727. [Google Scholar] [CrossRef] [PubMed]
- Voorberg-van der Wel, A.; Roma, G.; Gupta, D.K.; Schuierer, S.; Nigsch, F.; Carbone, W.; Zeeman, A.M.; Lee, B.H.; Hofman, S.O.; Faber, B.W.; et al. A comparative transcriptomic analysis of replicating and dormant liver stages of the relapsing malaria parasite Plasmodium cynomolgi. Elife 2017, 6, e29605. [Google Scholar] [CrossRef] [PubMed]
- Voorberg-van der Wel, A.; Zeeman, A.M.; van Amsterdam, S.M.; van den Berg, A.; Klooster, E.J.; Iwanaga, S.; Janse, C.J.; van Gemert, G.J.; Sauerwein, R.; Beenhakker, N.; et al. Transgenic fluorescent Plasmodium cynomolgi liver stages enable live imaging and purification of Malaria hypnozoite-forms. PLoS ONE 2013, 8, e54888. [Google Scholar] [CrossRef]
- Voorberg-van der Wel, A.M.; Zeeman, A.M.; Nieuwenhuis, I.G.; van der Werff, N.M.; Klooster, E.J.; Klop, O.; Vermaat, L.C.; Kumar Gupta, D.; Dembele, L.; Diagana, T.T.; et al. A dual fluorescent Plasmodium cynomolgi reporter line reveals in vitro malaria hypnozoite reactivation. Commun. Biol. 2020, 3, 7. [Google Scholar] [CrossRef]
- Voorberg-van der Wel, A.M.; Zeeman, A.M.; Nieuwenhuis, I.G.; van der Werff, N.M.; Kocken, C.H.M. Dual-Luciferase-Based Fast and Sensitive Detection of Malaria Hypnozoites for the Discovery of Anti-relapse Compounds. Methods Mol. Biol. 2022, 2524, 397–408. [Google Scholar] [CrossRef]
- Coatney, G.R.; Collins, W.E.; Warren, M.; Contacos, P.G. The Primate Malarias; US National Institute of Allergy and Infectious Diseases: Rockville, MD, USA, 1971. [Google Scholar]
- Joyner, C.; Barnwell, J.W.; Galinski, M.R. No more monkeying around: Primate malaria model systems are key to understanding Plasmodium vivax liver-stage biology, hypnozoites, and relapses. Front. Microbiol. 2015, 6, 145. [Google Scholar] [CrossRef]
- Mikolajczak, S.A.; Vaughan, A.M.; Kangwanrangsan, N.; Roobsoong, W.; Fishbaugher, M.; Yimamnuaychok, N.; Rezakhani, N.; Lakshmanan, V.; Singh, N.; Kaushansky, A.; et al. Plasmodium vivax liver stage development and hypnozoite persistence in human liver-chimeric mice. Cell Host Microbe 2015, 17, 526–535. [Google Scholar] [CrossRef]
- Schafer, C.; Dambrauskas, N.; Reynolds, L.M.; Trakhimets, O.; Raappana, A.; Flannery, E.L.; Roobsoong, W.; Sattabongkot, J.; Mikolajczak, S.A.; Kappe, S.H.I.; et al. Partial protection against P. vivax infection diminishes hypnozoite burden and blood-stage relapses. Cell Host Microbe 2021, 29, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Flannery, E.L.; Kangwanrangsan, N.; Chuenchob, V.; Roobsoong, W.; Fishbaugher, M.; Zhou, K.; Billman, Z.P.; Martinson, T.; Olsen, T.M.; Schafer, C.; et al. Plasmodium vivax latent liver infection is characterized by persistent hypnozoites, hypnozoite-derived schizonts, and time-dependent efficacy of primaquine. Mol. Ther. Methods Clin. Dev. 2022, 26, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Bermudez, M.; Moreno-Perez, D.A.; Arevalo-Pinzon, G.; Curtidor, H.; Patarroyo, M.A. Plasmodium vivax in vitro continuous culture: The spoke in the wheel. Malar. J. 2018, 17, 301. [Google Scholar] [CrossRef] [PubMed]
- Thomson-Luque, R.; Adams, J.H.; Kocken, C.H.M.; Pasini, E.M. From marginal to essential: The golden thread between nutrient sensing, medium composition and Plasmodium vivax maturation in in vitro culture. Malar. J. 2019, 18, 344. [Google Scholar] [CrossRef]
- Valenciano, A.L.; Gomez-Lorenzo, M.G.; Vega-Rodriguez, J.; Adams, J.H.; Roth, A. In vitro models for human malaria: Targeting the liver stage. Trends Parasitol. 2022, 38, 758–774. [Google Scholar] [CrossRef]
- Chattopadhyay, R.; Velmurugan, S.; Chakiath, C.; Andrews Donkor, L.; Milhous, W.; Barnwell, J.W.; Collins, W.E.; Hoffman, S.L. Establishment of an in vitro assay for assessing the effects of drugs on the liver stages of Plasmodium vivax malaria. PLoS ONE 2010, 5, e14275. [Google Scholar] [CrossRef]
- Hollingdale, M.R.; Collins, W.E.; Campbell, C.C.; Schwartz, A.L. In vitro culture of two populations (dividing and nondividing) of exoerythrocytic parasites of Plasmodium vivax. Am. J. Trop. Med. Hyg. 1985, 34, 216–222. [Google Scholar] [CrossRef]
- Sattabongkot, J.; Yimamnuaychoke, N.; Leelaudomlipi, S.; Rasameesoraj, M.; Jenwithisuk, R.; Coleman, R.E.; Udomsangpetch, R.; Cui, L.; Brewer, T.G. Establishment of a human hepatocyte line that supports in vitro development of the exo-erythrocytic stages of the malaria parasites Plasmodium falciparum and P. vivax. Am. J. Trop. Med. Hyg. 2006, 74, 708–715. [Google Scholar] [CrossRef]
- Pewkliang, Y.; Rungin, S.; Lerdpanyangam, K.; Duangmanee, A.; Kanjanasirirat, P.; Suthivanich, P.; Sa-Ngiamsuntorn, K.; Borwornpinyo, S.; Sattabongkot, J.; Patrapuvich, R.; et al. A novel immortalized hepatocyte-like cell line (imHC) supports in vitro liver stage development of the human malarial parasite Plasmodium vivax. Malar. J. 2018, 17, 50. [Google Scholar] [CrossRef]
- Ng, S.; Schwartz, R.E.; March, S.; Galstian, A.; Gural, N.; Shan, J.; Prabhu, M.; Mota, M.M.; Bhatia, S.N. Human iPSC-derived hepatocyte-like cells support Plasmodium liver-stage infection in vitro. Stem Cell Rep. 2015, 4, 348–359. [Google Scholar] [CrossRef]
- Gural, N.; Mancio-Silva, L.; Miller, A.B.; Galstian, A.; Butty, V.L.; Levine, S.S.; Patrapuvich, R.; Desai, S.P.; Mikolajczak, S.A.; Kappe, S.H.I.; et al. In Vitro Culture, Drug Sensitivity, and Transcriptome of Plasmodium vivax Hypnozoites. Cell Host Microbe 2018, 23, 395–406. [Google Scholar] [CrossRef] [PubMed]
- March, S.; Ng, S.; Velmurugan, S.; Galstian, A.; Shan, J.; Logan, D.J.; Carpenter, A.E.; Thomas, D.; Sim, B.K.; Mota, M.M.; et al. A microscale human liver platform that supports the hepatic stages of Plasmodium falciparum and vivax. Cell Host Microbe 2013, 14, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Chua, A.C.Y.; Ananthanarayanan, A.; Ong, J.J.Y.; Wong, J.Y.; Yip, A.; Singh, N.H.; Qu, Y.; Dembele, L.; McMillian, M.; Ubalee, R.; et al. Hepatic spheroids used as an in vitro model to study malaria relapse. Biomaterials 2019, 216, 119221. [Google Scholar] [CrossRef]
- Mazier, D.; Landau, I.; Druilhe, P.; Miltgen, F.; Guguen-Guillouzo, C.; Baccam, D.; Baxter, J.; Chigot, J.P.; Gentilini, M. Cultivation of the liver forms of Plasmodium vivax in human hepatocytes. Nature 1984, 307, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Roth, A.; Maher, S.P.; Conway, A.J.; Ubalee, R.; Chaumeau, V.; Andolina, C.; Kaba, S.A.; Vantaux, A.; Bakowski, M.A.; Thomson-Luque, R.; et al. A comprehensive model for assessment of liver stage therapies targeting Plasmodium vivax and Plasmodium falciparum. Nat. Commun. 2018, 9, 1837. [Google Scholar] [CrossRef] [PubMed]
- Carlton, J.M.; Adams, J.H.; Silva, J.C.; Bidwell, S.L.; Lorenzi, H.; Caler, E.; Crabtree, J.; Angiuoli, S.V.; Merino, E.F.; Amedeo, P.; et al. Comparative genomics of the neglected human malaria parasite Plasmodium vivax. Nature 2008, 455, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Nurk, S.; Koren, S.; Rhie, A.; Rautiainen, M.; Bzikadze, A.V.; Mikheenko, A.; Vollger, M.R.; Altemose, N.; Uralsky, L.; Gershman, A.; et al. The complete sequence of a human genome. Science 2022, 376, 44–53. [Google Scholar] [CrossRef]
- Zeeman, A.M.; Lakshminarayana, S.B.; van der Werff, N.; Klooster, E.J.; Voorberg-van der Wel, A.; Kondreddi, R.R.; Bodenreider, C.; Simon, O.; Sauerwein, R.; Yeung, B.K.; et al. PI4 Kinase Is a Prophylactic but Not Radical Curative Target in Plasmodium vivax-Type Malaria Parasites. Antimicrob. Agents Chemother. 2016, 60, 2858–2863. [Google Scholar] [CrossRef]
- Mancio-Silva, L.; Gural, N.; Real, E.; Wadsworth, M.H., 2nd; Butty, V.L.; March, S.; Nerurkar, N.; Hughes, T.K.; Roobsoong, W.; Fleming, H.E.; et al. A single-cell liver atlas of Plasmodium vivax infection. Cell Host Microbe 2022, 30, 1048–1060. [Google Scholar] [CrossRef]
- Ruberto, A.A.; Maher, S.P.; Vantaux, A.; Joyner, C.J.; Bourke, C.; Balan, B.; Jex, A.; Mueller, I.; Witkowski, B.; Kyle, D.E. Single-cell RNA profiling of Plasmodium vivax-infected hepatocytes reveals parasite- and host- specific transcriptomic signatures and therapeutic targets. Front. Cell. Infect. Microbiol. 2022, 12, 986314. [Google Scholar] [CrossRef]
- Krotoski, W.A.; Bray, R.S.; Garnham, P.C.; Gwadz, R.W.; Killick-Kendrick, R.; Draper, C.C.; Targett, G.A.; Krotoski, D.M.; Guy, M.W.; Koontz, L.C.; et al. Observations on early and late post-sporozoite tissue stages in primate malaria. II. The hypnozoite of Plasmodium cynomolgi bastianellii from 3 to 105 days after infection, and detection of 36- to 40-h pre-erythrocytic forms. Am. J. Trop. Med. Hyg. 1982, 31, 211–225. [Google Scholar] [CrossRef] [PubMed]
- Krotoski, W.A.; Garnham, P.C.; Bray, R.S.; Krotoski, D.M.; Killick-Kendrick, R.; Draper, C.C.; Targett, G.A.; Guy, M.W. Observations on early and late post-sporozoite tissue stages in primate malaria. I. Discovery of a new latent form of Plasmodium cynomolgi (the hypnozoite), and failure to detect hepatic forms within the first 24 h after infection. Am. J. Trop. Med. Hyg. 1982, 31, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Hawking, F.; Worms, M.J.; Gammage, K. 24- and 48-h cycles of malaria parasites in the blood; their purpose, production and control. Trans. R. Soc. Trop. Med. Hyg. 1968, 62, 731–765. [Google Scholar] [CrossRef] [PubMed]
- Krotoski, W.A.; Krotoski, D.M.; Garnham, P.C.; Bray, R.S.; Killick-Kendrick, R.; Draper, C.C.; Targett, G.A.; Guy, M.W. Relapses in primate malaria: Discovery of two populations of exoerythrocytic stages. Preliminary note. Br. Med. J. 1980, 280, 153–154. [Google Scholar] [CrossRef] [PubMed]
- Coatney, G.R. Reminiscences: My Forty-Year Romance with Malaria. Trans. Neb. Acad. Sci. Affil. Soc. 1985, 222, 5–11. [Google Scholar]
- Corcoran, K.D.; Hansukjariya, P.; Sattabongkot, J.; Ngampochjana, M.; Edstein, M.D.; Smith, C.D.; Shanks, G.D.; Milhous, W.K. Causal prophylactic and radical curative activity of WR182393 (a guanylhydrazone) against Plasmodium cynomolgi in Macaca mulatta. Am. J. Trop. Med. Hyg. 1993, 49, 473–477. [Google Scholar] [CrossRef]
- Davidson, D.E., Jr.; Ager, A.L.; Brown, J.L.; Chapple, F.E.; Whitmire, R.E.; Rossan, R.N. New tissue schizontocidal antimalarial drugs. Bull. World Health Organ. 1981, 59, 463–479. [Google Scholar]
- Deye, G.A.; Gettayacamin, M.; Hansukjariya, P.; Im-Erbsin, R.; Sattabongkot, J.; Rothstein, Y.; Macareo, L.; Fracisco, S.; Bennett, K.; Magill, A.J.; et al. Use of a rhesus Plasmodium cynomolgi model to screen for anti-hypnozoite activity of pharmaceutical substances. Am. J. Trop. Med. Hyg. 2012, 86, 931–935. [Google Scholar] [CrossRef]
- Dow, G.S.; Gettayacamin, M.; Hansukjariya, P.; Imerbsin, R.; Komcharoen, S.; Sattabongkot, J.; Kyle, D.; Milhous, W.; Cozens, S.; Kenworthy, D.; et al. Radical curative efficacy of tafenoquine combination regimens in Plasmodium cynomolgi-infected Rhesus monkeys (Macaca mulatta). Malar. J. 2011, 10, 212. [Google Scholar] [CrossRef]
- Dutta, G.P.; Puri, S.K.; Bhaduri, A.P.; Seth, M. Radical curative activity of a new 8-aminoquinoline derivative (CDRI 80/53) against Plasmodium cynomolgi B in monkeys. Am. J. Trop. Med. Hyg. 1989, 41, 635–637. [Google Scholar] [CrossRef]
- Schmidt, L.H. Appraisals of compounds of diverse chemical classes for capacities to cure infections with sporozoites of Plasmodium cynomolgi. Am. J. Trop. Med. Hyg. 1983, 32, 231–257. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, L.H.; Fradkin, R.; Genther, C.S.; Rossan, R.N.; Squires, W. Responses of Sporozoite-Induced and Trophozoite-Induced Infections to Standard Antimalarial Drugs. Am. J. Trop. Med. Hyg. 1982, 31, 646–665. [Google Scholar] [CrossRef] [PubMed]
- Sodeman, T.M.; Contacos, P.G.; Collins, W.E.; Smith, C.S.; Jumper, J.R. Studies on the prophylactic and radical curative activity of RC-12 against Plasmodium cynomolgi in Macaca mulatta. Bull. World Health Organ. 1972, 47, 425–428. [Google Scholar] [PubMed]
- Millet, P.; Fisk, T.L.; Collins, W.E.; Broderson, J.R.; Nguyen-Dinh, P. Cultivation of exoerythrocytic stages of Plasmodium cynomolgi, P. knowlesi, P. coatneyi, and P. inui in Macaca mulatta hepatocytes. Am. J. Trop. Med. Hyg. 1988, 39, 529–534. [Google Scholar] [CrossRef]
- Dembele, L.; Gego, A.; Zeeman, A.M.; Franetich, J.F.; Silvie, O.; Rametti, A.; Le Grand, R.; Dereuddre-Bosquet, N.; Sauerwein, R.; van Gemert, G.J.; et al. Towards an in vitro model of Plasmodium hypnozoites suitable for drug discovery. PLoS ONE 2011, 6, e18162. [Google Scholar] [CrossRef]
- Zeeman, A.M.; van Amsterdam, S.M.; McNamara, C.W.; Voorberg-van der Wel, A.; Klooster, E.J.; van den Berg, A.; Remarque, E.J.; Plouffe, D.M.; van Gemert, G.J.; Luty, A.; et al. KAI407, a potent non-8-aminoquinoline compound that kills Plasmodium cynomolgi early dormant liver stage parasites in vitro. Antimicrob. Agents Chemother. 2014, 58, 1586–1595. [Google Scholar] [CrossRef]
- Ashraf, K.; Tajeri, S.; Arnold, C.S.; Amanzougaghene, N.; Franetich, J.F.; Vantaux, A.; Soulard, V.; Bordessoulles, M.; Cazals, G.; Bousema, T.; et al. Artemisinin-independent inhibitory activity of Artemisia sp. infusions against different Plasmodium stages including relapse-causing hypnozoites. Life Sci. Alliance 2022, 5, e202101237. [Google Scholar] [CrossRef]
- Gupta, D.K.; Dembele, L.; Voorberg-van der Wel, A.; Roma, G.; Yip, A.; Chuenchob, V.; Kangwanrangsan, N.; Ishino, T.; Vaughan, A.M.; Kappe, S.H.; et al. The Plasmodium liver-specific protein 2 (LISP2) is an early marker of liver stage development. Elife 2019, 8, e43362. [Google Scholar] [CrossRef]
- Sutton, P.L.; Luo, Z.; Divis, P.C.S.; Friedrich, V.K.; Conway, D.J.; Singh, B.; Barnwell, J.W.; Carlton, J.M.; Sullivan, S.A. Characterizing the genetic diversity of the monkey malaria parasite Plasmodium cynomolgi. Infect. Genet. Evol. 2016, 40, 243–252. [Google Scholar] [CrossRef]
- Dembele, L.; Franetich, J.F.; Lorthiois, A.; Gego, A.; Zeeman, A.M.; Kocken, C.H.; Le Grand, R.; Dereuddre-Bosquet, N.; van Gemert, G.J.; Sauerwein, R.; et al. Persistence and activation of malaria hypnozoites in long-term primary hepatocyte cultures. Nat. Med. 2014, 20, 307–312. [Google Scholar] [CrossRef]
- Cubi, R.; Vembar, S.S.; Biton, A.; Franetich, J.F.; Bordessoulles, M.; Sossau, D.; Zanghi, G.; Bosson-Vanga, H.; Benard, M.; Moreno, A.; et al. Laser capture microdissection enables transcriptomic analysis of dividing and quiescent liver stages of Plasmodium relapsing species. Cell. Microbiol. 2017, 19, e12735. [Google Scholar] [CrossRef] [PubMed]
- Tachibana, S.; Kawai, S.; Katakai, Y.; Takahashi, H.; Nakade, T.; Yasutomi, Y.; Horii, T.; Tanabe, K. Contrasting infection susceptibility of the Japanese macaques and cynomolgus macaques to closely related malaria parasites, Plasmodium vivax and Plasmodium cynomolgi. Parasitol. Int. 2015, 64, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Pasini, E.M.; Bohme, U.; Rutledge, G.G.; Voorberg-Van der Wel, A.; Sanders, M.; Berriman, M.; Kocken, C.H.; Otto, T.D. An improved Plasmodium cynomolgi genome assembly reveals an unexpected methyltransferase gene expansion. Wellcome Open Res. 2017, 2, 42. [Google Scholar] [CrossRef]
- Tachibana, S.; Sullivan, S.A.; Kawai, S.; Nakamura, S.; Kim, H.R.; Goto, N.; Arisue, N.; Palacpac, N.M.; Honma, H.; Yagi, M.; et al. Plasmodium cynomolgi genome sequences provide insight into Plasmodium vivax and the monkey malaria clade. Nat. Genet. 2012, 44, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Akinyi, S.; Hanssen, E.; Meyer, E.V.; Jiang, J.; Korir, C.C.; Singh, B.; Lapp, S.; Barnwell, J.W.; Tilley, L.; Galinski, M.R. A 95 kDa protein of Plasmodium vivax and P. cynomolgi visualized by three-dimensional tomography in the caveola-vesicle complexes (Schuffner’s dots) of infected erythrocytes is a member of the PHIST family. Mol. Microbiol. 2012, 84, 816–831. [Google Scholar] [CrossRef]
- Barale, J.C.; Menard, R. Centromeric plasmids and artificial chromosomes: New kids on the Plasmodium transfection block. Cell Host Microbe 2010, 7, 181–183. [Google Scholar] [CrossRef][Green Version]
- Manzoni, G.; Briquet, S.; Risco-Castillo, V.; Gaultier, C.; Topcu, S.; Ivanescu, M.L.; Franetich, J.F.; Hoareau-Coudert, B.; Mazier, D.; Silvie, O. A rapid and robust selection procedure for generating drug-selectable marker-free recombinant malaria parasites. Sci. Rep. 2014, 4, 4760. [Google Scholar] [CrossRef]
- van Schaijk, B.C.; van Dijk, M.R.; van de Vegte-Bolmer, M.; van Gemert, G.J.; van Dooren, M.W.; Eksi, S.; Roeffen, W.F.; Janse, C.J.; Waters, A.P.; Sauerwein, R.W. Pfs47, paralog of the male fertility factor Pfs48/45, is a female specific surface protein in Plasmodium falciparum. Mol. Biochem. Parasitol. 2006, 149, 216–222. [Google Scholar] [CrossRef]
- Iwanaga, S.; Kato, T.; Kaneko, I.; Yuda, M. Centromere plasmid: A new genetic tool for the study of Plasmodium falciparum. PLoS ONE 2012, 7, e33326. [Google Scholar] [CrossRef]
- Iwanaga, S.; Khan, S.M.; Kaneko, I.; Christodoulou, Z.; Newbold, C.; Yuda, M.; Janse, C.J.; Waters, A.P. Functional identification of the Plasmodium centromere and generation of a Plasmodium artificial chromosome. Cell Host Microbe 2010, 7, 245–255. [Google Scholar] [CrossRef]
- Mitchell, G.; Roma, G.; Voorberg-van der Wel, A.; Beibel, M.; Zeeman, A.M.; Schuierer, S.; Torres, L.; Flannery, E.L.; Kocken, C.H.M.; Mikolajczak, S.A.; et al. Transcriptional profiling of hepatocytes infected with the replicative form of the malaria parasite Plasmodium cynomolgi. Malar. J. 2022, 21, 393. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.P.; Unch, J.; Binkowski, B.F.; Valley, M.P.; Butler, B.L.; Wood, M.G.; Otto, P.; Zimmerman, K.; Vidugiris, G.; Machleidt, T.; et al. Engineered luciferase reporter from a deep-sea shrimp utilizing a novel imidazopyrazinone substrate. ACS Chem. Biol. 2012, 7, 1848–1857. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.R.; Das, S.; Wong, E.H.; Andenmatten, N.; Stallmach, R.; Hackett, F.; Herman, J.P.; Muller, S.; Meissner, M.; Blackman, M.J. Robust inducible Cre recombinase activity in the human malaria parasite Plasmodium falciparum enables efficient gene deletion within a single asexual erythrocytic growth cycle. Mol. Microbiol. 2013, 88, 687–701. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, P.; Briquet, S.; Patarot, D.; Loubens, M.; Hoareau-Coudert, B.; Silvie, O. The dimerisable Cre recombinase allows conditional genome editing in the mosquito stages of Plasmodium berghei. PLoS ONE 2020, 15, e0236616. [Google Scholar] [CrossRef]
- Knuepfer, E.; Napiorkowska, M.; van Ooij, C.; Holder, A.A. Generating conditional gene knockouts in Plasmodium—A toolkit to produce stable DiCre recombinase-expressing parasite lines using CRISPR/Cas9. Sci. Rep. 2017, 7, 3881. [Google Scholar] [CrossRef]
- Christensen, P.; Racklyeft, A.; Ward, K.E.; Matheson, J.; Suwanarusk, R.; Chua, A.C.Y.; Kaneko, O.; Aung, H.L.; Renia, L.; Amanzougaghene, N.; et al. Improving in vitro continuous cultivation of Plasmodium cynomolgi, a model for P. vivax. Parasitol. Int. 2022, 89, 102589. [Google Scholar] [CrossRef]
- Chua, A.C.Y.; Ong, J.J.Y.; Malleret, B.; Suwanarusk, R.; Kosaisavee, V.; Zeeman, A.M.; Cooper, C.A.; Tan, K.S.W.; Zhang, R.; Tan, B.H.; et al. Robust continuous in vitro culture of the Plasmodium cynomolgi erythrocytic stages. Nat. Commun. 2019, 10, 3635. [Google Scholar] [CrossRef]
- Ghorbal, M.; Gorman, M.; Macpherson, C.R.; Martins, R.M.; Scherf, A.; Lopez-Rubio, J.J. Genome editing in the human malaria parasite Plasmodium falciparum using the CRISPR-Cas9 system. Nat. Biotechnol. 2014, 32, 819–821. [Google Scholar] [CrossRef]
- Carrasquilla, M.; Adjalley, S.; Sanderson, T.; Marin-Menendez, A.; Coyle, R.; Montandon, R.; Rayner, J.C.; Pance, A.; Lee, M.C.S. Defining multiplicity of vector uptake in transfected Plasmodium parasites. Sci. Rep. 2020, 10, 10894. [Google Scholar] [CrossRef]
- Knuepfer, E.; Wright, K.E.; Kumar Prajapati, S.; Rawlinson, T.A.; Mohring, F.; Koch, M.; Lyth, O.R.; Howell, S.A.; Villasis, E.; Snijders, A.P.; et al. Divergent roles for the RH5 complex components, CyRPA and RIPR in human-infective malaria parasites. PLoS Pathog. 2019, 15, e1007809. [Google Scholar] [CrossRef]
- Kocken, C.H.; Zeeman, A.M.; Voorberg-van der Wel, A.; Thomas, A.W. Transgenic Plasmodium knowlesi: Relieving a bottleneck in malaria research? Trends Parasitol. 2009, 25, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Mohring, F.; Hart, M.N.; Patel, A.; Baker, D.A.; Moon, R.W. CRISPR-Cas9 Genome Editing of Plasmodium knowlesi. Bio Protoc. 2020, 10, e3522. [Google Scholar] [CrossRef] [PubMed]
- Mohring, F.; Hart, M.N.; Rawlinson, T.A.; Henrici, R.; Charleston, J.A.; Diez Benavente, E.; Patel, A.; Hall, J.; Almond, N.; Campino, S.; et al. Rapid and iterative genome editing in the malaria parasite Plasmodium knowlesi provides new tools for P. vivax research. Elife 2019, 8, e45829. [Google Scholar] [CrossRef] [PubMed]
- Moon, R.W.; Hall, J.; Rangkuti, F.; Ho, Y.S.; Almond, N.; Mitchell, G.H.; Pain, A.; Holder, A.A.; Blackman, M.J. Adaptation of the genetically tractable malaria pathogen Plasmodium knowlesi to continuous culture in human erythrocytes. Proc. Natl. Acad. Sci. USA 2013, 110, 531–536. [Google Scholar] [CrossRef]
- Moraes Barros, R.R.; Gibson, T.J.; Kite, W.A.; Sa, J.M.; Wellems, T.E. Comparison of two methods for transformation of Plasmodium knowlesi: Direct schizont electroporation and spontaneous plasmid uptake from plasmid-loaded red blood cells. Mol. Biochem. Parasitol. 2017, 218, 16–22. [Google Scholar] [CrossRef]
- Moraes Barros, R.R.; Thawnashom, K.; Gibson, T.J.; Armistead, J.S.; Caleon, R.L.; Kaneko, M.; Kite, W.A.; Mershon, J.P.; Brockhurst, J.K.; Engels, T.; et al. Activity of Plasmodium vivax promoter elements in Plasmodium knowlesi, and a centromere-containing plasmid that expresses NanoLuc throughout the parasite life cycle. Malar. J. 2021, 20, 247. [Google Scholar] [CrossRef]
- Verzier, L.H.; Coyle, R.; Singh, S.; Sanderson, T.; Rayner, J.C. Plasmodium knowlesi as a model system for characterising Plasmodium vivax drug resistance candidate genes. PLoS Negl. Trop. Dis. 2019, 13, e0007470. [Google Scholar] [CrossRef]
- Krotoski, W.A.; Collins, W.E. Failure to detect hypnozoites in hepatic tissue containing exoerythrocytic schizonts of Plasmodium knowlesi. Am. J. Trop. Med. Hyg. 1982, 31, 854–856. [Google Scholar] [CrossRef]
| Material Used for Transfection | Transfection Tools Available | Used to Investigate | Refs | |
|---|---|---|---|---|
| P. vivax vivo | In vivo-derived blood stages | Transient transfection, zinc-finger mediated recombination | Blood stages in vivo | [40,41] |
| P. cynomolgi vivo | In vivo-derived blood stages | Homology directed recombination, episomal, centromere | Blood stages in vivo; liver stage schizonts and hypnozoites in vitro | [37,45,46,47,48,49,50,98] |
| P. cynomolgi vitro | In vitro-derived blood stages | Episomal, Crispr/Cas9 | Blood stages in vitro | [43] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voorberg-van der Wel, A.; Zeeman, A.-M.; Kocken, C.H.M. Transfection Models to Investigate Plasmodium vivax-Type Dormant Liver Stage Parasites. Pathogens 2023, 12, 1070. https://doi.org/10.3390/pathogens12091070
Voorberg-van der Wel A, Zeeman A-M, Kocken CHM. Transfection Models to Investigate Plasmodium vivax-Type Dormant Liver Stage Parasites. Pathogens. 2023; 12(9):1070. https://doi.org/10.3390/pathogens12091070
Chicago/Turabian StyleVoorberg-van der Wel, Annemarie, Anne-Marie Zeeman, and Clemens H. M. Kocken. 2023. "Transfection Models to Investigate Plasmodium vivax-Type Dormant Liver Stage Parasites" Pathogens 12, no. 9: 1070. https://doi.org/10.3390/pathogens12091070
APA StyleVoorberg-van der Wel, A., Zeeman, A.-M., & Kocken, C. H. M. (2023). Transfection Models to Investigate Plasmodium vivax-Type Dormant Liver Stage Parasites. Pathogens, 12(9), 1070. https://doi.org/10.3390/pathogens12091070







