Opportunistic Features of Non-Clostridium botulinum Strains Containing bont Gene Cluster
Abstract
:1. Introduction
2. Saprophytic and Pathogenic Clostridium sporogenes
2.1. General Clostridium sporogenes Description
2.2. Pathogenic Strains of Clostridium sporogenes
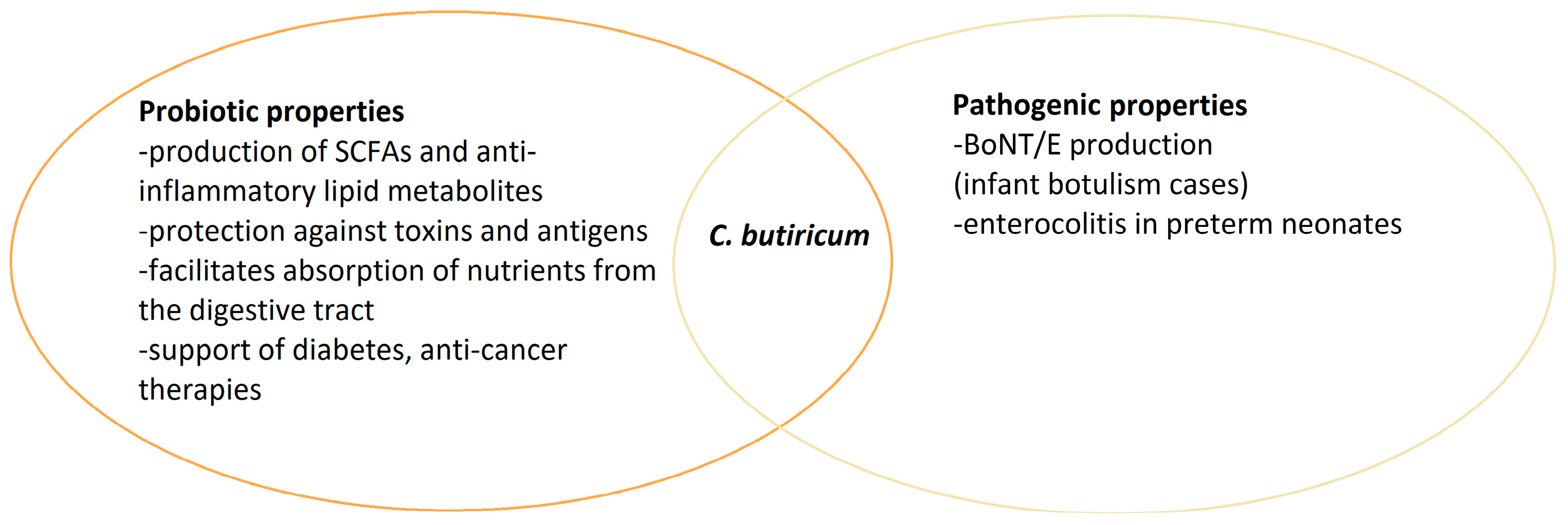
3. Double Nature of Clostridium butyricum
3.1. Clostridium butyricum as a Probiotic
3.2. Role of Clostridium butyricum in Health Promotion
| Clostridium botulinum as a Health Support | Source |
|---|---|
| With oral administration, the composition of the normal gastrointestinal microflora is regulated by increasing the beneficial microflora and reducing harmful strains of microorganisms; improves digestion and the functioning of the digestive system. | [39] |
| Creates an unfavourable environment for pathogenic organisms mainly by producing butyric acid and adhering to human epithelial cells, creating a protective mucosal barrier. | [39] |
| Prevents post-antibiotic diarrhea. | [39] |
| LAB could synergistically enhance the probiotic functions of C. butyricum. | [40] |
| Administration of C. butyricum effectively restores the intestinal microbial balance after colonoscopy and contributes to faster recovery. | [41] |
| Negative correlation between C. butyricum content and the predisposition to the development of obesity, and potential effective use as supplements in inhibiting the development of obesity. | [45,46] |
| Effectively balances blood glucose, alleviates vascular changes, and improves the intestinal microbiome, suggesting support of type 2 diabetes treatment. | [47,48] |
| Improves the effectiveness of HSCT and maintains the balance of the intestinal microflora. | [49] |
| In non-small cell lung cancer patients, supports the effectiveness of treatment that uses inhibitors of immunological control points. | [56] |
| Supports polypectomy treatment. | [57] |
3.3. Pathogenicity and Threats of Clostridium butyricum
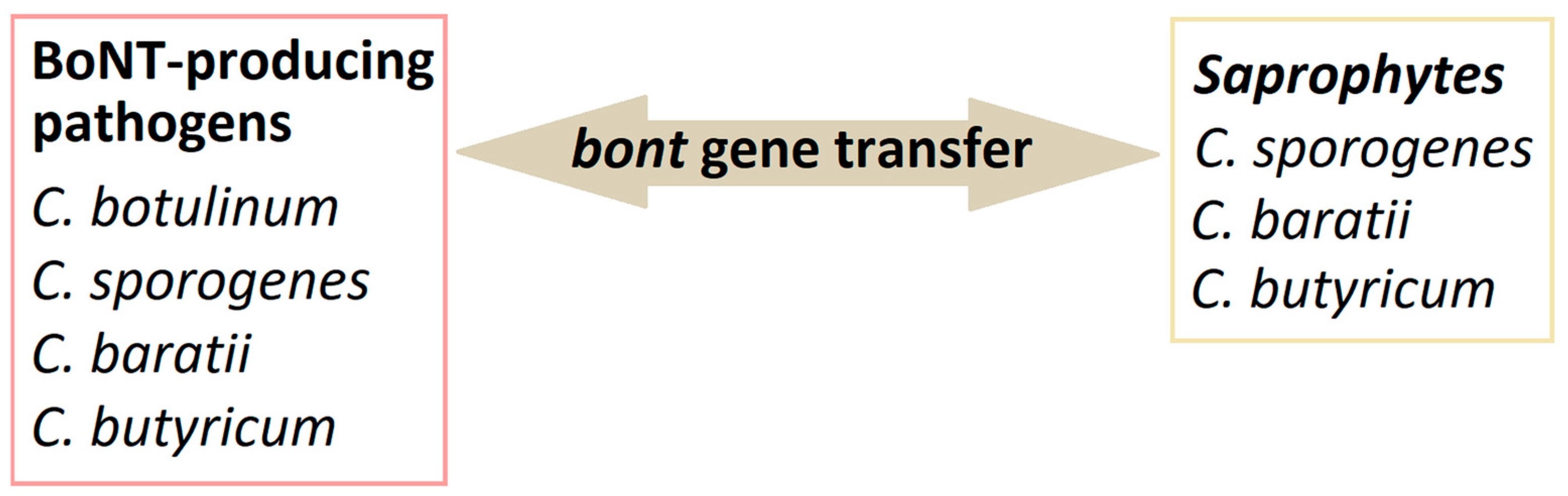
4. Genetic Mechanism of bont Genes Expression in Non-C. botulinum Strains
5. Non-Clostridium BoNT-like Producing Strains
6. Problem with Classifications and Taxonomy
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Samul, D.; Worsztynowicz, P.; Leja, K.; Grajek, W. Beneficial and harmful roles of bacteria from the Clostridium genus. Acta Biochim. Pol. 2013, 60, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Guo, P.; Zhang, K.; Ma, X.; He, P. Clostridium species as probiotics: Potentials and challenges. J. Anim. Sci. Biotechnol. 2020, 11, 24. [Google Scholar] [CrossRef]
- Erbguth, F.J. From poison to remedy: The chequered history of botulinum toxin. J. Neural Transm. 2008, 115, 559–565. [Google Scholar] [CrossRef]
- Ciccarelli, A.S.; Giménez, D.F. Cryoprotein produced by Clostridium botulinum type G. Infect. Immun. 1972, 5, 985–986. [Google Scholar] [CrossRef] [PubMed]
- Cato, E.P.; Stackebrandt, E. Taxonomy and Phylogeny. In Clostridia; Minton, N.P., Clarke, D.J., Eds.; Springer: Boston, MA, USA, 1989; pp. 1–26. ISBN 978-1-4757-9718-3. [Google Scholar]
- Carter, A.T.; Peck, M.W. Genomes, neurotoxins and biology of Clostridium botulinum Group I and Group II. Res. Microbiol. 2015, 166, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Collins, M.D.; East, A.K. Phylogeny and taxonomy of the food-borne pathogen Clostridium botulinum and its neurotoxins. J. Appl. Microbiol. 1998, 84, 5–17. [Google Scholar] [CrossRef]
- Scalfaro, C.; Iacobino, A.; Grande, L.; Morabito, S.; Franciosa, G. Effects of megaplasmid loss on growth of neurotoxigenic Clostridium butyricum strains and botulinum neurotoxin type E expression. Front. Microbiol. 2016, 7, 217. [Google Scholar] [CrossRef]
- Brunt, J.; Carter, A.T.; Stringer, S.C.; Peck, M.W. Identification of a novel botulinum neurotoxin gene cluster in Enterococcus. FEBS Lett. 2018, 592, 310–317. [Google Scholar] [CrossRef]
- Truong, R.D.; Do, V.A.; Njaravelil, K.A.; Ayesu, K.; Madruga, M.; Carlan, S.J. Unusual Case of Ludwig Angina Caused by Clostridium sporogenes in an Immunocompromised HIV-Positive Patient with Alcoholism and Dental Abscess. Am. J. Case Rep. 2023, 24, e941731. [Google Scholar] [CrossRef]
- Lorenzo, J.M.; Munekata, P.E.; Dominguez, R.; Pateiro, M.; Saraiva, J.A.; Franco, D. Main Groups of Microorganisms of Relevance for Food Safety and Stability: General Aspects and Overall Description; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 9780128110324. [Google Scholar]
- Alataby, H.A.; Krishnamoorthy, V.; Ndzelen, L.; Kenne, F.M.; Valenti, K.; Savermuttu, J.; Nfonoyim, J. Clostridium Sporogenes Causing Bacteremia Originated from the Skin and Soft Tissue Infection in an Immunocompetent Patient—Case Report and Literature Review. Int. J. Crit. Care Emerg. Med. 2020, 6, 95. [Google Scholar] [CrossRef]
- Vecchio, M.J.; Jankowich, M.; Qadir, H.; Gaitanis, M.; Menon, A. Cognitive Biases in the Era of COVID-19: A Case of Clostridium sporogenes Bacteremia in a Patient with Small Bowel Obstruction. Case Rep. Infect. Dis. 2020, 2020, 8812635. [Google Scholar] [CrossRef] [PubMed]
- Bodey, G.P.; Rodriguez, S.; Fainstein, V.; Elting, L.S. Clostridial bacteremia in cancer patients. A 12-year experience. Cancer 1991, 67, 1928–1942. [Google Scholar] [CrossRef] [PubMed]
- Abusnina, W.; Shehata, M.; Karem, E.; Koc, Z.; Khalil, E. Clostridium sporogenes bacteremia in an immunocompetent patient. IDCases 2019, 15, e00481. [Google Scholar] [CrossRef] [PubMed]
- Rechner, P.M.; Agger, W.A.; Mruz, K.; Cogbill, T.H. Clinical features of clostridial bacteremia: A review from a rural area. Clin. Infect. Dis. 2001, 33, 349–353. [Google Scholar] [CrossRef]
- Shen, D.X.; Babady, N.E.; Chen, R.; Gilhuley, K.; Tang, Y.W. Septicaemia caused by Clostridium sporogenes: Two case reports and a literature review. Rev. Res. Med. Microbiol. 2013, 24, 81–83. [Google Scholar] [CrossRef]
- Cobo, F.; Pérez-Carrasco, V.; García-Salcedo, J.A.; Navarro-Marí, J.M. Bacteremia caused by Clostridium sporogenes in an oncological patient. Rev. Esp. Quimioter. 2023, 36, 217–219. [Google Scholar] [CrossRef]
- Stabler, S.; Titécat, M.; Duployez, C.; Kipnis, E.; Dessein, R.; Le Guern, R. Clinical relevance of Clostridium bacteremia: An 8-year retrospective study. Anaerobe 2020, 63, 102202. [Google Scholar] [CrossRef]
- Corbett, C.E.; Wall, B.M.; Cohen, M. Empyema With Hydropneumothorax and Bacteremia Caused by Clostridium sporogenes. Am. J. Med. Sci. 1996, 312, 242–245. [Google Scholar] [CrossRef]
- Malmborg, A.S.; Rylander, M.; Selander, H. Case report: Primary thoracic empyema caused by clostridium sporogenes. Scand. J. Infect. Dis. 1970, 2, 155–156. [Google Scholar] [CrossRef]
- Inkster, T.; Cordina, C.; Siegmeth, A. Septic arthritis following anterior cruciate ligament reconstruction secondary to Clostridium sporogenes; a rare clinical pathogen. J. Clin. Pathol. 2011, 64, 820–821. [Google Scholar] [CrossRef] [PubMed]
- Hitchcock, C.R.; Demello, F.J.; Haglin, J.J. Gangrene infection: New approaches to an old disease. Surg. Clin. N. Am. 1975, 55, 1403–1410. [Google Scholar] [CrossRef] [PubMed]
- Kanaujia, R.; Dahiya, D.; Banda, A.R.; Ray, P.; Angrup, A. Non-traumatic gas gangrene due to Clostridium sporogenes. Lancet Infect. Dis. 2020, 20, 754. [Google Scholar] [CrossRef] [PubMed]
- Sárvári, K.P.; Schoblocher, D. The antibiotic susceptibility pattern of gas gangrene-forming Clostridium spp. clinical isolates from South-Eastern Hungary. Infect. Dis. 2020, 52, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Hara-Kudo, Y.; Yamakawa, Y.; Kumagai, S. Purification and some properties of Clostridium sporogenes hemorrhagic toxin. Biochem. Biophys. Res. Commun. 1996, 227, 413–418. [Google Scholar] [CrossRef]
- Brunt, J.; van Vliet, A.H.M.; Carter, A.T.; Stringer, S.C.; Amar, C.; Grant, K.A.; Godbole, G.; Peck, M.W. Diversity of the Genomes and Neurotoxins of Strains of Clostridium botulinum Group I and Clostridium sporogenes Associated with Foodborne, Infant and Wound Botulism. Toxins 2020, 12, 586. [Google Scholar] [CrossRef]
- Williamson, C.H.D.; Sahl, J.W.; Smith, T.J.; Xie, G.; Foley, B.T.; Smith, L.A.; Fernández, R.A.; Lindström, M.; Korkeala, H.; Keim, P.; et al. Comparative genomic analyses reveal broad diversity in botulinum-toxinproducing Clostridia. BMC Genom. 2016, 17, 180. [Google Scholar] [CrossRef]
- Mazuet, C.; Legeay, C.; Sautereau, J.; Ma, L.; Bouchier, C.; Bouvet, P.; Popoff, M.R. Diversity of group i and II clostridium botulinum strains from France including recently identified subtypes. Genome Biol. Evol. 2016, 8, 1643–1660. [Google Scholar] [CrossRef]
- Smith, T.J.; Hill, K.K.; Raphael, B.H. Historical and current perspectives on Clostridium botulinum diversity. Res. Microbiol. 2015, 166, 290–302. [Google Scholar] [CrossRef]
- Giordani, F.; Fillo, S.; Anselmo, A.; Palozzi, A.M.; Fortunato, A.; Gentile, B.; Azarnia Tehran, D.; Ciammaruconi, A.; Spagnolo, F.; Pittiglio, V.; et al. Genomic characterization of Italian Clostridium botulinum group I strains. Infect. Genet. Evol. 2015, 36, 62–71. [Google Scholar] [CrossRef]
- McLauchlin, J.; Grant, K.A.; Little, C.L. Food-borne botulism in the United Kingdom. J. Public Health 2006, 28, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Franciosa, G.; Maugliani, A.; Scalfaro, C.; Aureli, P. Evidence that plasmid-borne botulinum neurotoxin type B genes are widespread among Clostridium botulinum serotype B strains. PLoS ONE 2009, 4, e4829. [Google Scholar] [CrossRef]
- Liberato, V.; Benevenuti, C.; Coelho, F.; Botelho, A.; Amaral, P.; Pereira, N.; Ferreira, T. Clostridium sp. as Bio-Catalyst for Fuels and Chemicals Production in a Biorefinery Context. Catalysts 2019, 9, 962. [Google Scholar] [CrossRef]
- Moțățăianu, A.; Șerban, G.; Andone, S. The Role of Short-Chain Fatty Acids in Microbiota-Gut-Brain Cross-Talk with a Focus on Amyotrophic Lateral Sclerosis: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 15094. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Liu, X.; Wang, Y.; Wang, T.; Fang, D.; Hu, K. Effects of Clostridium butyricum on Intestinal Microflora and Metabolism of Eriocheir sinensis. Int. J. Mol. Sci. 2023, 24, 13784. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Commission Implementing Decision of 10 March 2014. Off. J. Eur. Union 2014, 588, 30–33. [Google Scholar]
- Ariyoshi, T.; Hagihara, M.; Takahashi, M.; Mikamo, H. Effect of Clostridium butyricum on Gastrointestinal Infections. Biomedicines 2022, 10, 483. [Google Scholar] [CrossRef]
- Seki, H.; Shiohara, M.; Matsumura, T.; Miyagawa, N.; Tanaka, M.; Komiyama, A.; Kurata, S. Prevention of antibiotic-associated diarrhea in children by Clostridium butyricum MIYAIRI. Pediatr. Int. 2003, 45, 86–90. [Google Scholar] [CrossRef]
- Hagihara, M.; Kuroki, Y.; Ariyoshi, T.; Higashi, S.; Fukuda, K.; Yamashita, R.; Matsumoto, A.; Mori, T.; Mimura, K.; Yamaguchi, N.; et al. Clostridium butyricum Modulates the Microbiome to Protect Intestinal Barrier Function in Mice with Antibiotic-Induced Dysbiosis. iScience 2020, 23, 100772. [Google Scholar] [CrossRef]
- So, J.S.; Oh, K.; Shin, Y. Growth stimulation of Clostridium butyricum in the presence of Lactobacillus brevis JL16 and Lactobacillus parabuchneri MH44. Food Sci. Technol. Braz. 2022, 42, 1–8. [Google Scholar] [CrossRef]
- Chen, Z.; Yu, L.; Liu, J.; Kong, J.; Deng, X.; Guo, X.; Shan, J.; Zhou, D.; Li, W.; Lin, Y.; et al. Gut microbiota dynamics and fecal SCFAs after colonoscopy: Accelerating microbiome stabilization by Clostridium butyricum. J. Transl. Med. 2024, 22, 222. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhang, Z.; Zhang, X.; Lu, C.; Yang, W.; Xie, X.; Xin, H.; Lu, X.; Ni, M.; Yang, X.; et al. Effects of dietary Clostridium butyricum and rumen protected fat on meat quality, oxidative stability, and chemical composition of finishing goats. J. Anim. Sci. Biotechnol. 2024, 15, 3. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yun, Y.; Lai, Z.; Ji, S.; Yu, G.; Xie, Z.; Zhang, H.; Zhong, X.; Wang, T.; Zhang, L. Supplemental Clostridium butyricum modulates lipid metabolism by reshaping the gut microbiota composition and bile acid profile in IUGR suckling piglets. J. Anim. Sci. Biotechnol. 2023, 14, 36. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Ma, J.; Lin, H.; Zhou, S.; Long, Z.; Qin, H.; Lin, Y.; Liu, L.; Huang, Z.; Li, Z. Analyzing the influence of Clostridium butyricum on liver health in spotted sea bass (Lateolabrax maculatus) via transcriptomics and metabolomics. Aquac. Int. 2024, 32, 4717–4736. [Google Scholar] [CrossRef]
- Liao, J.; Liu, Y.; Pei, Z.; Wang, H.; Zhu, J.; Zhao, J.; Lu, W.; Chen, W. Clostridium butyricum Reduces Obesity in a Butyrate-Independent Way. Microorganisms 2023, 11, 1292. [Google Scholar] [CrossRef]
- Liao, J.; Liu, Y.; Yao, Y.; Zhang, J.; Wang, H.; Zhao, J.; Chen, W.; Lu, W. Clostridium butyricum Strain CCFM1299 Reduces Obesity via Increasing Energy Expenditure and Modulating Host Bile Acid Metabolism. Nutrients 2023, 15, 4339. [Google Scholar] [CrossRef]
- Tayyib, H.M.U.; Ali, A.; Jabeen, S.; Habib-ur-Rehman; Kamran, H.; Bajaber, M.A.; Usman, M.; Zhang, X. Restoration of gut dysbiosis through Clostridium butyricum and magnesium possibly balance blood glucose levels: An experimental study. BMC Microbiol. 2024, 24, 105. [Google Scholar] [CrossRef]
- Zhou, T.; Qiu, S.; Zhang, L.; Li, Y.; Zhang, J.; Shen, D.; Zhao, P.; Yuan, L.; Zhao, L.; Duan, Y.; et al. Supplementation of Clostridium butyricum Alleviates Vascular Inflammation in Diabetic Mice. Diabetes Metab. J. 2024, 48, 390–404. [Google Scholar] [CrossRef]
- Fukushima, K.; Kudo, H.; Oka, K.; Hayashi, A.; Onizuka, M.; Kusakabe, S.; Hino, A.; Takahashi, M.; Takeda, K.; Mori, M.; et al. Clostridium butyricum MIYAIRI 588 contributes to the maintenance of intestinal microbiota diversity early after haematopoietic cell transplantation. Bone Marrow Transplant. 2024, 59, 795–802. [Google Scholar] [CrossRef]
- West, H.; McCleod, M.; Hussein, M.; Morabito, A.; Rittmeyer, A.; Conter, H.J.; Kopp, H.-G.; Daniel, D.; McCune, S.; Mekhail, T.; et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019, 20, 924–937. [Google Scholar] [CrossRef]
- Topalian, S.L.; Hodi, F.S.; Brahmer, J.R.; Gettinger, S.N.; Smith, D.C.; McDermott, D.F.; Powderly, J.D.; Sosman, J.A.; Atkins, M.B.; Leming, P.D.; et al. Five-Year Survival and Correlates among Patients with Advanced Melanoma, Renal Cell Carcinoma, or Non-Small Cell Lung Cancer Treated with Nivolumab. JAMA Oncol. 2019, 5, 1411–1420. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, L.; Rodríguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. Pembrolizumab plus Chemotherapy in Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092. [Google Scholar] [CrossRef]
- Boyero, L.; Sánchez-Gastaldo, A.; Alonso, M.; Noguera-Uclés, J.F.; Molina-Pinelo, S.; Bernabé-Caro, R. Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy. Cancers 2020, 12, 3729. [Google Scholar] [CrossRef]
- Kovács, S.A.; Győrffy, B. Transcriptomic datasets of cancer patients treated with immune-checkpoint inhibitors: A systematic review. J. Transl. Med. 2022, 20, 249. [Google Scholar] [CrossRef] [PubMed]
- Vu, S.H.; Vetrivel, P.; Kim, J.; Lee, M.-S. Cancer Resistance to Immunotherapy: Molecular Mechanisms and Tackling Strategies. Int. J. Mol. Sci. 2022, 23, 10906. [Google Scholar] [CrossRef] [PubMed]
- Paz Del Socorro, T.; Oka, K.; Boulard, O.; Takahashi, M.; Poulin, L.F.; Hayashi, A.; Chamaillard, M. The biotherapeutic Clostridium butyricum MIYAIRI 588 strain potentiates enterotropism of Rorγt+Treg and PD-1 blockade efficacy. Gut Microbes 2024, 16, 2315631. [Google Scholar] [CrossRef]
- Saitsu, Y.; Yoneda, S.; Fukuta, K. Management of a pregnant woman with a large cervical polyp and moderate genital bleeding in the first trimester. BMJ Case Rep. 2024, 17, e258163. [Google Scholar] [CrossRef]
- Cassir, N.; Benamar, S.; La Scola, B. Clostridium butyricum: From beneficial to a new emerging pathogen. Clin. Microbiol. Infect. 2016, 22, 37–45. [Google Scholar] [CrossRef]
- Ferraris, L.; Balvay, A.; Bellet, D.; Delannoy, J.; Maudet, C.; Larcher, T.; Rozé, J.C.; Philippe, C.; Meylheuc, T.; Butel, M.J.; et al. Neonatal necrotizing enterocolitis: Clostridium butyricum and Clostridium neonatale fermentation metabolism and enteropathogenicity. Gut Microbes 2023, 15, 2172666. [Google Scholar] [CrossRef]
- Oguma, K.; Inoue, K.; Fujinaga, Y.; Yokota, K.; Watanabe, T.; Ohyama, T.; Takeshi, K.; Inoue, K. Structure and Function of Clostridium Botulinum Progenitor Toxin. J. Toxicol. Toxin Rev. 1999, 18, 17–34. [Google Scholar] [CrossRef]
- Gu, S.; Jin, R. Assembly and Function of the Botulinum Neurotoxin Progenitor Complex. Curr. Top. Microbiol. Immunol. 2013, 364, 21–44. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J.; Hill, K.K.; Foley, B.T.; Detter, J.C.; Munk, A.C.; Bruce, D.C.; Doggett, N.A.; Smith, L.A.; Marks, J.D.; Xie, G.; et al. Analysis of the Neurotoxin Complex Genes in Clostridium botulinum A1-A4 and B1 Strains: BoNT/A3, /Ba4 and /B1 Clusters Are Located within Plasmids. PLoS ONE 2007, 2, e1271. [Google Scholar] [CrossRef] [PubMed]
- Skarin, H.; Segerman, B. Horizontal gene transfer of toxin genes in Clostridium botulinum. Mob. Genet. Elem. 2011, 1, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Nawrocki, E.M.; Bradshaw, M.; Johnson, E.A. Botulinum neurotoxin-encoding plasmids can be conjugatively transferred to diverse clostridial strains. Sci. Rep. 2018, 8, 3100. [Google Scholar] [CrossRef] [PubMed]
- Ng, V.; Lin, W.-J. Comparison of assembled Clostridium botulinum A1 genomes revealed their evolutionary relationship. Genomics 2014, 103, 94–106. [Google Scholar] [CrossRef]
- Hill, K.K.; Xie, G.; Foley, B.T.; Smith, T.J.; Munk, A.C.; Bruce, D.; Smith, L.A.; Brettin, T.S.; Detter, J.C. Recombination and insertion events involving the botulinum neurotoxin complex genes in Clostridium botulinum types A, B, E and F and Clostridium butyricum type E strains. BMC Biol. 2009, 7, 66. Available online: https://bmcbiol.biomedcentral.com/articles/10.1186/1741-7007-7-66 (accessed on 28 August 2024). [CrossRef]
- Paul, C.J.; Twine, S.M.; Tam, K.J.; Mullen, J.A.; Kelly, J.F.; Austin, J.W.; Logan, S.M. Flagellin Diversity in Clostridium botulinum Groups I and II: A New Strategy for Strain Identification. Appl. Environ. Microbiol. 2007, 73, 2963–2975. [Google Scholar] [CrossRef]
- Woudstra, C.; Lambert, D.; Anniballi, F.; De Medici, D.; Austin, J.; Fach, P. Genetic Diversity of the Flagellin Genes of Clostridium botulinum Groups I and II. Appl. Environ. Microbiol. 2013, 79, 3926–3932. [Google Scholar] [CrossRef]
- Valdezate, S.; Carrasco, G.; Medina, M.J.; Garrido, N.; Del Pino, S.; Valiente, M.; Pallarés, M.P.; Villalon, P. Exploring the genetic background of the botulism neurotoxin BoNT/B2 in Spain. Microbiol. Spectr. 2023, 11, e0238023. [Google Scholar] [CrossRef]
- Smith, T.J.; Tian, R.; Imanian, B.; Williamson, C.H.D.; Johnson, S.L.; Daligault, H.E.; Schill, K.M. Integration of Complete Plasmids Containing Bont Genes into Chromosomes of Clostridium parabotulinum, Clostridium sporogenes, and Clostridium argentinense. Toxins 2021, 13, 473. [Google Scholar] [CrossRef]
- Grenda, T.; Grenda, A.; Krawczyk, P.; Kwiatek, K. Botulinum toxin in cancer therapy—Current perspectives and limitations. Appl. Microbiol. Biotechnol. 2022, 106, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Lebreton, F.; Mansfield, M.J.; Miyashita, S.-I.; Zhang, J.; Schwartzman, J.A.; Tao, L.; Masuyer, G.; Martínez-Carranza, M.; Stenmark, P.; et al. Identification of a Botulinum Neurotoxin-like Toxin in a Commensal Strain of Enterococcus faecium. Cell Host Microbe 2018, 23, 169–176.e6. [Google Scholar] [CrossRef]
- Tehran, D.A.; Pirazzini, M. Novel Botulinum Neurotoxins: Exploring Underneath the Iceberg Tip. Toxins 2018, 10, 190. [Google Scholar] [CrossRef]
- Poulain, B.; Popoff, M.R. Why Are Botulinum Neurotoxin-Producing Bacteria So Diverse and Botulinum Neurotoxins So Toxic? Toxins 2019, 11, 34. [Google Scholar] [CrossRef]
- Grenda, T.; Jarosz, A.; Sapała, M.; Stasiak, K.; Grenda, A.; Domaradzki, P.; Kwiatek, K. Molecular Diversity of BoNT-Producing Clostridia—A Still-Emerging and Challenging Problem. Diversity 2023, 15, 392. [Google Scholar] [CrossRef]
- Hayashi, H.; Sakamoto, M.; Kitahara, M.; Benno, Y. Diversity of the Clostridium coccoides group in human fecal microbiota as determined by 16S rRNA gene library. FEMS Microbiol. Lett. 2006, 257, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Lawson, P.A.; Rainey, F.A. Proposal to restrict the genus Clostridium Prazmowski to Clostridium butyricum and related species. Int. J. Syst. Evol. Microbiol. 2016, 66, 1009–1016. [Google Scholar] [CrossRef]
- Smith, T.; Williamson, C.H.D.; Hill, K.; Sahl, J.; Keim, P. Botulinum Neurotoxin-Producing Bacteria. Isn’t It Time that We Called a Species a Species? mBio 2018, 9, e01469-18. [Google Scholar] [CrossRef]
- Peck, M.W. Biology and Genomic Analysis of Clostridium botulinum. In Advances in Microbial Physiology; Poole, R.K., Ed.; Academic Press: Cambridge, MA, USA, 2009; Volume 55, pp. 183–320. [Google Scholar]
- Suen, J.C.; Hatheway, C.L.; Steigerwalt, A.G.; Brenner, D.J. Genetic confirmation of identities of neurotoxigenic Clostridium baratii and Clostridium butyricum implicated as agents of infant botulism. J. Clin. Microbiol. 1988, 26, 2191–2192. [Google Scholar] [CrossRef]
| Group of C. botulinum Species | Other Genera of BoNT-like Producing Bacteria | ||||||
|---|---|---|---|---|---|---|---|
| Other BoNT-Producing Clostridia | Organisms Potentially Able to Produce BoNT-like Proteins (I/Wo/J/En/Cp1 Toxin) | ||||||
| I | II | III | IV | ||||
| C. botulinum A and proteolytic strains of C. botulinum B and F | C. botulinum E and glucidolytic strains of C. botulinum B and F | C. botulinum C and D | C. botulinum G, which was assigned to a new species C. argentinense. | C. baratii Type F | C. butyricum Type E | C. sporogenes Type B | E. faecalis Weisella oryzae Enterococcus faecium Chryseobacterium piperi |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grenda, T.; Grenda, A.; Jakubczyk, A.; Rybczyńska-Tkaczyk, K. Opportunistic Features of Non-Clostridium botulinum Strains Containing bont Gene Cluster. Pathogens 2024, 13, 780. https://doi.org/10.3390/pathogens13090780
Grenda T, Grenda A, Jakubczyk A, Rybczyńska-Tkaczyk K. Opportunistic Features of Non-Clostridium botulinum Strains Containing bont Gene Cluster. Pathogens. 2024; 13(9):780. https://doi.org/10.3390/pathogens13090780
Chicago/Turabian StyleGrenda, Tomasz, Anna Grenda, Anna Jakubczyk, and Kamila Rybczyńska-Tkaczyk. 2024. "Opportunistic Features of Non-Clostridium botulinum Strains Containing bont Gene Cluster" Pathogens 13, no. 9: 780. https://doi.org/10.3390/pathogens13090780
APA StyleGrenda, T., Grenda, A., Jakubczyk, A., & Rybczyńska-Tkaczyk, K. (2024). Opportunistic Features of Non-Clostridium botulinum Strains Containing bont Gene Cluster. Pathogens, 13(9), 780. https://doi.org/10.3390/pathogens13090780







