Low Rates of Immunity among Medical Students and Residents in the Era of the Resurgence of Measles
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Statement
References
- Lazar, M.; Stănescu, A.; Penedos, A.R.; Pistol, A. Characterisation of measles after the introduction of the combined measles-mumps-rubella (MMR) vaccine in 2004 with focus on the laboratory data, 2016 to 2019 outbreak, Romania. Euro Surveill. 2019, 24, 1900041. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention Control Measles. Annual Epidemiological Report for 2023; ECDC: Stockholm, Sweden, 2024. [Google Scholar]
- World Health Organization Regional Office for Europe (WHO/EURO). A 30-Fold Rise of Measles Cases in 2023 in the WHO European Region Warrants Urgent Action; WHO EURO: Geneva, Sweden, 2023; Available online: https://www.who.int/europe/news/item/14-12-2023-a-30-fold-rise-of-measles-cases-in-2023-in-the-who-european-region-warrants-urgent-action (accessed on 12 June 2024).
- Perfetto, B.; Paduano, G.; Grimaldi, E.; Sansone, V.; Donnarumma, G.; Di Giuseppe, G. Seroprevalence for Measles, Varicella, Mumps and Rubella in the Trainee Obstetric Population: A Survey in Southern Italy. Vaccines 2024, 12, 335. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Measles on the Rise in the EU/EEA: Considerations for Public Health Response; ECDC: Stockholm, Sweden, 2024; ISBN 978-92-9498-693-1. [Google Scholar] [CrossRef]
- ISS Epicentro Measles. Available online: https://www.epicentro.iss.it/morbillo/aggiornamenti (accessed on 20 April 2024).
- World Health Organization (WHO). Measles and Rubella Laboratory Documents; WHO: Geneva, Sweden, 2018; Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/immunization-analysis-and-insights/surveillance/surveillance-for-vpds/laboratory-networks/measles-and-rubella-laboratory-network/manual-for-the-laboratory-based-surveillance-of-measles-rubella-and-congenital-rubella-syndrome (accessed on 15 July 2018).
- Lo, N.C.; Hotez, P.J. Public health and economic consequences of vaccine hesitancy for measles in the United States. JAMA Pediatr. 2017, 171, 887–892. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Regional Office for Europe (WHO Euro). Eliminating Measles and Rubella—Framework for the Verification Process in the WHO European Region; WHO Euro: Copenhagen, Denmark, 2014; Available online: http://www.euro.who.int/__data/assets/pdf_file/0009/247356/Eliminating-measles-and-rubella-Framework-for-the-verification-process-in-the-WHO-European-Region.pdf (accessed on 12 June 2024).
- ISS Epicentro Measles. Available online: https://www.epicentro.iss.it/morbillo/bollettino/RM_News_2022_66.pdf (accessed on 12 June 2024).
- Limavady, A.; Tu, I.T.; Bedford, H. Guarding the gatekeepers: A comprehensive approach to control nosocomial measles. Infection 2024, 52, 1195–1206. [Google Scholar] [CrossRef]
- Ferrari, C.; Somma, G.; Olesen, O.; Buonomo, E.; Pasanisi Zingarello, M.; Mazza, A.; Rizza, S.; Di Giampaolo, L.; Magrini, A.; Ponzani, F.; et al. Measles vaccine uptake among Italian medical students compared to the pre-COVID-19 era. Hum. Vaccin. Immunother. 2023, 19, 2252681. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Trabucco Aurilio, M.; Iannuzzi, I.; Di Giampaolo, L.; Pietroiusti, A.; Ferrari, C.; Coppeta, L. A cross-sectional serological study for measles among Italian medical students in 2020. Open Public Health J. 2020, 13, 692–695. [Google Scholar] [CrossRef]
- Filia, A.; Bella, A.; Del Manso, M.; Baggieri, M.; Marchi, A.; Bucci, P.; Magurano, F.; Nicoletti, L.; Rota, M.C. Morbillo & Rosolia News, N 58 Gennaio 2020. Available online: https://www.epicentro.iss.it/morbillo/bollettino/RM_News_2019_58.pdf (accessed on 13 June 2024).
- Filia, A.; Bella, A.; Del Manso, M.; Baggieri, M.; Magurano, F.; Rota, M.C. Ongoing outbreak with well over 4000 measles cases in Italy from January to end August 2017—What is making elimination so difficult? Euro Surveill. 2017, 22, 30614. [Google Scholar] [CrossRef] [PubMed]
- Green, M.S.; Schwartz, N.; Peer, V. Gender differences in measles incidence rates in a multi-year, pooled analysis, based on national data from seven high-income countries. BMC Infect. Dis. 2022, 22, 358. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Italian Legislative Decree 73/2017.
- ISS Epicentro. Le Vaccinazioni in Italia. Available online: https://www.epicentro.iss.it/vaccini/dati_Ita#measles (accessed on 13 June 2024).
- Bolotin, S.; Osman, S.; Hughes, S.L.; Ariyarajah, A.; Tricco, A.C.; Khan, S.; Li, L.; Johnson, C.; Friedman, L.; Gul, N.; et al. In Elimination Settings, Measles Antibodies Wane after Vaccination but not after Infection: A Systematic Review and Meta-Analysis. J. Infect. Dis. 2022, 226, 1127–1139. [Google Scholar] [CrossRef]
- Wang, Q.; Wang, W.; Winter, A.K.; Zhan, Z.; Ajelli, M.; Trentini, F.; Wang, L.; Li, F.; Yang, J.; Xiang, X.; et al. Long-term measles antibody profiles following different vaccine schedules in China, a longitudinal study. Nat. Commun. 2023, 14, 1746. [Google Scholar] [CrossRef]
- Friedrich, M. Measles Cases Rise Around the Globe. JAMA 2019, 321, 238. [Google Scholar] [CrossRef] [PubMed]
- Taheri Soodejani, M.; Basti, M.; Tabatabaei, S.M.; Rajabkhah, K. Measles, mumps, and rubella (MMR) vaccine and COVID-19: A systematic review. Int. J. Mol. Epidemiol. Genet. 2021, 12, 35–39. [Google Scholar] [PubMed] [PubMed Central]
- Fidel, P.L., Jr.; Noverr, M.C. Could an unrelated live attenuated vaccine serve as a preventive measure to dampen septic inflammation associated with COVID-19 infection? mBio 2020, 11, e00907-20. [Google Scholar] [CrossRef]
- Saad, M.E.; Elsalamony, R.A. Measles vaccines may provide partial protection against COVID-19. Int. J. Cancer Biomed. Res. 2020, 5, 14–19. [Google Scholar] [CrossRef]
- Salman, S.; Salem, M.L. Routine childhood immunization may protect against COVID-19. Med. Hypotheses 2020, 140, 109689. [Google Scholar] [CrossRef] [PubMed]
- Coppeta, L.; Pietroiusti, A.; Morucci, L.; Neri, A.; Ferraro, M.; Magrini, A. Workplace vaccination against measles in a teaching hospital of Rome. J. Hosp. Infect. 2019, 101, 364–365. [Google Scholar] [CrossRef]
- Freund, R.; Krivine, A.; Prévost, A.; Magrini, A. Measles immunity and measles vaccine acceptance among health-care workers in Paris, France. J. Hosp. Infect. 2013, 84, 38–43. [Google Scholar] [CrossRef]
- Coppeta, L.; Ferrari, C.; Somma, G.; Giovinazzo, V.; Buonomo, E.; Trabucco Aurilio, M.; Treglia, M.; Magrini, A. Serological Evaluation for Measles among Italian and Foreign Medical Students in a University Hospital in Rome. Vaccines 2023, 11, 1256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- WHO Coronavirus Disease (COVID-19): Herd Immunity, Lockdowns and COVID-19. Available online: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19#:~:text=The%20percentage%20of%20people%20who,among%20those%20who%20are%20vaccinated (accessed on 14 June 2024).
- Kaur, M.; Coppeta, L.; Olesen, O.F. Vaccine Hesitancy among Healthcare Workers in Europe: A Systematic Review. Vaccines 2023, 11, 1657. [Google Scholar] [CrossRef]
- Fehér, Á.; Fekete, M.; Varga, J.T.; Horváth, I. Az orvostanhallgatók vakcinológiai tájékozottsága [Medical students’ knowledge on vaccinology]. Orv. Hetil. 2019, 160, 1193–1199. [Google Scholar] [CrossRef] [PubMed]
- Riva, M.A.; Paladino, M.E.; Paleari, A.; Belingheri, M. Workplace COVID-19 vaccination, challenges and opportunities. Occup. Med. 2022, 72, 235–237. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Hooste, W.L.C. Influenza vaccination at the workplace. Vaccine 2022, 40, 2367–2368. [Google Scholar] [CrossRef] [PubMed]
- CDC Measles Prevention: Recommendations of the Immunization Practices Advisory Committee (ACIP). Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00041753.htm (accessed on 28 April 2024).
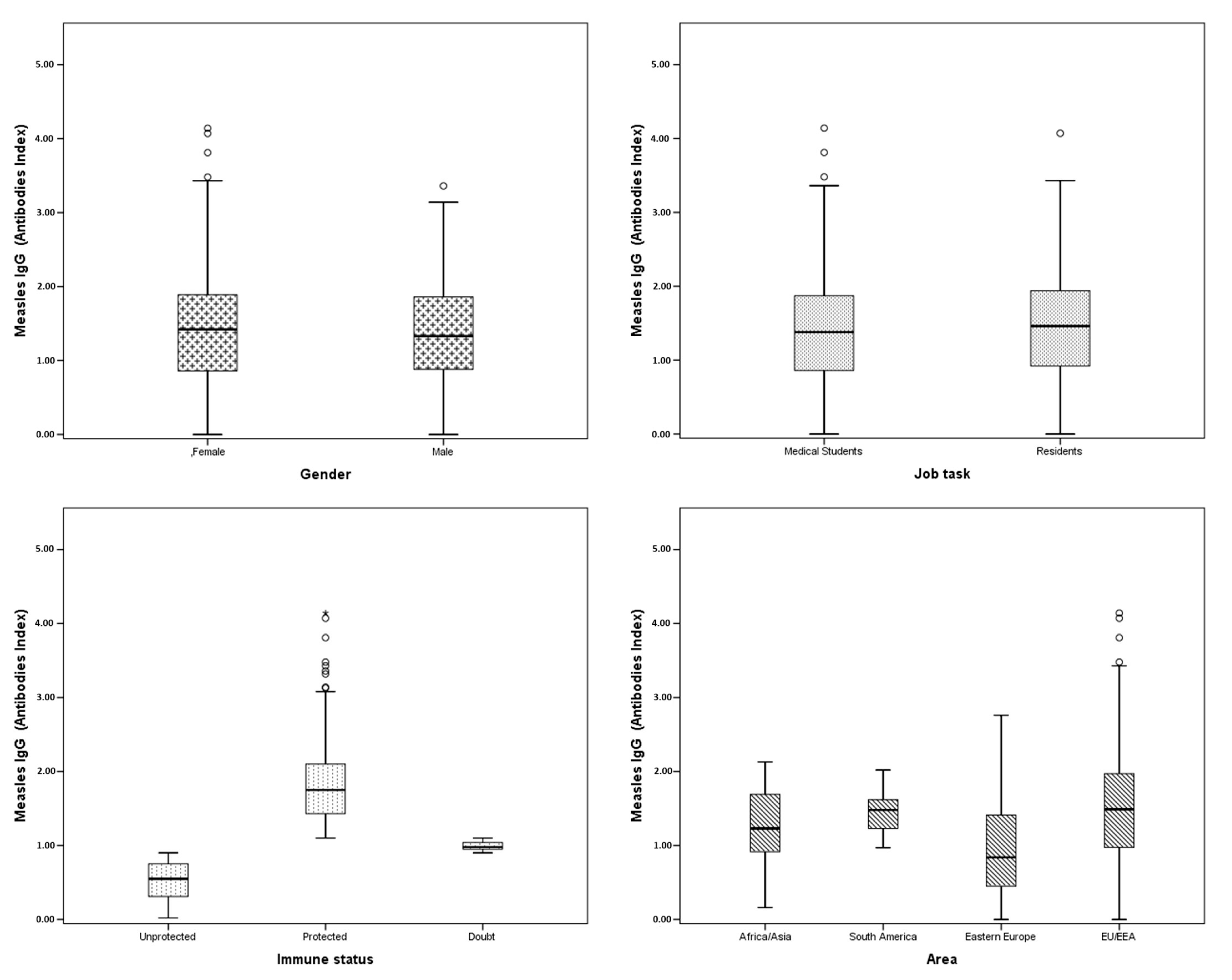
| Characteristics | N (%) | Mean Age ± SD | Mean IgG Level ± SD |
|---|---|---|---|
| Gender | |||
| Male | 267 (31.4%) | 24.9 ± 3.07 | 1.36 ± 0.68 |
| Female | 583 (68.6%) | 24.6 ± 2.89 | 1.41 ± 0.72 |
| Tasks | |||
| Medical students | 669 (78.7%) | 23.6 ± 2.17 | 1.38 ± 0.70 |
| Residents | 181 (21.3%) | 28.9 ± 0.85 | 1.44 ± 0.74 |
| Measles-specific IgG level | |||
| >1.1 AI | 546 (64.2%) | 24.8 ± 3.06 | 1.81 ± 0.49 |
| 0.9–1.1 AI | 82 (9.7%) | 24.7 ± 2.75 | 1.00 ± 0.06 |
| <0.9 AI | 222 (26.1%) | 24.6 ± 2.75 | 0.51 ± 0.26 |
| Area | |||
| EU/EEA | 687 (81.4%) | 24.9 ± 3.10 | 1.48 ± 0.71 |
| Eastern Europe | 133 (15.8%) | 24.1 ± 1.78 | 0.94 ± 0.64 |
| Asia/Africa | 19 (2.2%) | 22.1 ± 2.30 | 1.24 ± 0.54 |
| South America | 5 (0.6%) | 23.4 ± 2.07 | 1.49 ± 0.52 |
| Characteristics | N Protected (%) | Mean Age ± SD | Mean IgG Level |
|---|---|---|---|
| Gender | |||
| Male | 163 (61.0%) | 24.7 ± 3.20 | 1.80 ± 0.45 |
| Female | 383 (65.7%) | 24.8 ± 3.00 | 1.82 ± 0.50 |
| Tasks | |||
| Medical students | 422 (63.1%) | 23.5 ± 2.29 | 1.81 ± 0.48 |
| Residents | 124 (68.5%) | 28.9 ± 0.85 | 1.82 ± 0.52 |
| Area | |||
| EU/EEA | 484 (70.5%) | 24.8 ± 3.12 | 1.83 ± 0.50 |
| Eastern Europe | 46 (34.6%) | 25.0 ± 2.25 | 1.69 ± 0.41 |
| Asia/Africa | 12 (63.2%) | 22.0 ± 2.41 | 1.53 ± 0.31 |
| South America | 4 (80.0%) | 23.5 ± 2.38 | 1.58 ± 0.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrari, C.; Somma, G.; Caputi, V.; Treglia, M.; Pallocci, M.; Cenko, F.; Buonomo, E.; Carestia, M.; Di Giampaolo, L.; Olesen, O.F.; et al. Low Rates of Immunity among Medical Students and Residents in the Era of the Resurgence of Measles. Pathogens 2024, 13, 784. https://doi.org/10.3390/pathogens13090784
Ferrari C, Somma G, Caputi V, Treglia M, Pallocci M, Cenko F, Buonomo E, Carestia M, Di Giampaolo L, Olesen OF, et al. Low Rates of Immunity among Medical Students and Residents in the Era of the Resurgence of Measles. Pathogens. 2024; 13(9):784. https://doi.org/10.3390/pathogens13090784
Chicago/Turabian StyleFerrari, Cristiana, Giuseppina Somma, Vittorio Caputi, Michele Treglia, Margherita Pallocci, Fabian Cenko, Ersilia Buonomo, Mariachiara Carestia, Luca Di Giampaolo, Ole F. Olesen, and et al. 2024. "Low Rates of Immunity among Medical Students and Residents in the Era of the Resurgence of Measles" Pathogens 13, no. 9: 784. https://doi.org/10.3390/pathogens13090784
APA StyleFerrari, C., Somma, G., Caputi, V., Treglia, M., Pallocci, M., Cenko, F., Buonomo, E., Carestia, M., Di Giampaolo, L., Olesen, O. F., & Coppeta, L. (2024). Low Rates of Immunity among Medical Students and Residents in the Era of the Resurgence of Measles. Pathogens, 13(9), 784. https://doi.org/10.3390/pathogens13090784









