Identification of Bacillus anthracis Strains from Animal Cases in Ethiopia and Genetic Characterization by Whole-Genome Sequencing
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Anthrax Outbreak Investigation
2.3. Sample Collection and Transportation
Samples Collected from Suspected Animal Anthrax Outbreaks
2.4. Isolation and Identification of B. anthracis
2.4.1. Identification Using Gram-Staining and Capsule Staining
2.4.2. Culture
2.4.3. Biochemical Test
2.5. Molecular Detection and Characterization
2.5.1. Growth of B. anthracis and DNA Extraction
2.5.2. Diagnostic Real-Time PCR for Detecting Plasmid Markers of B. anthracis
2.5.3. Whole Genome Sequencing
2.5.4. Comparison with Public Database Entries
2.5.5. Phylogenetic Analysis
3. Results
3.1. Findings from Anthrax Outbreak Investigation
3.2. Identification and Characterization of B. anthracis Strains
3.3. Genetic Characteristics of B. anthracis Strains Isolated from Animals
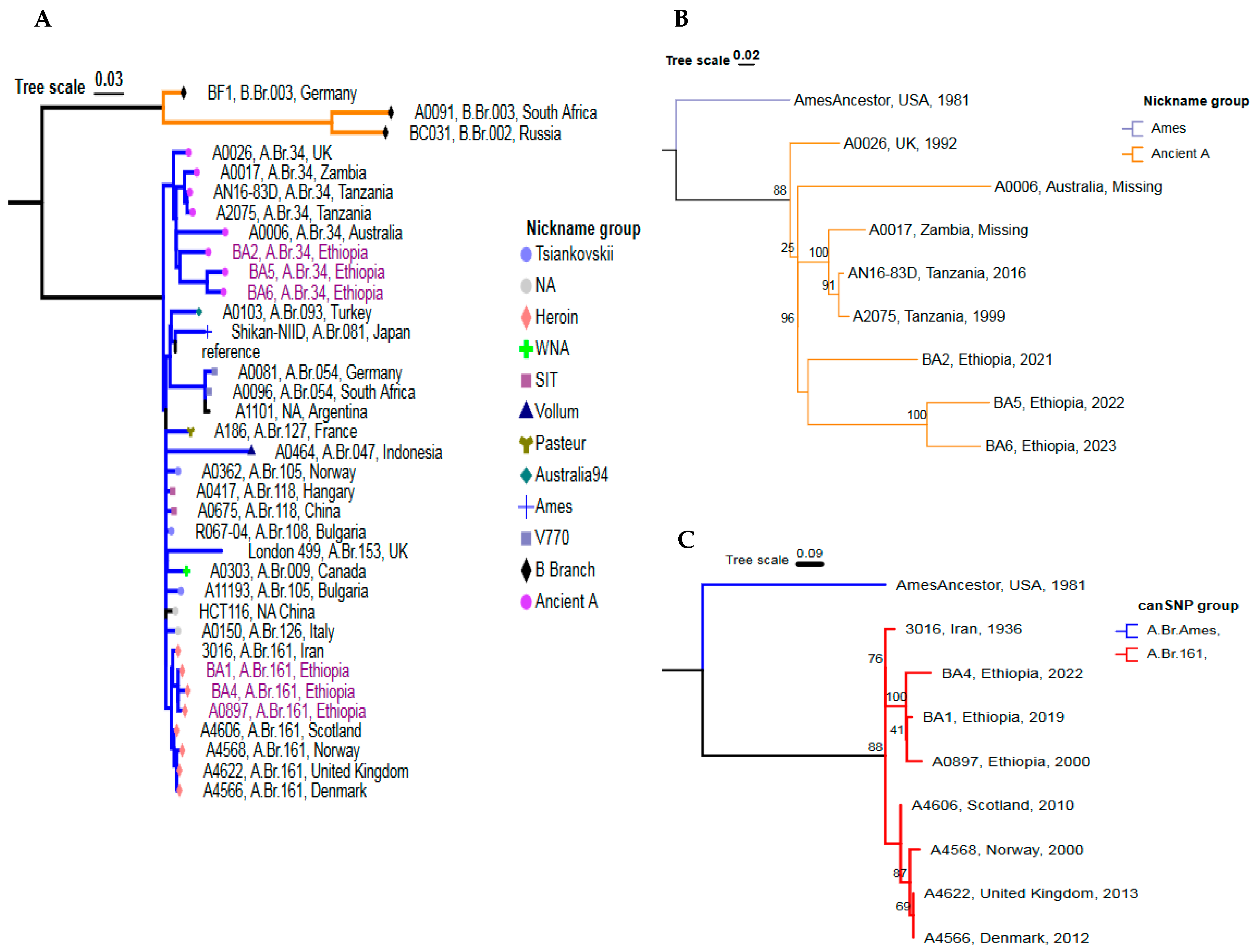
3.4. Global Phylogenetic Placement of the Ethiopian B. anthracis Strains
3.5. Detailed Genetic Positioning of the 5 Outbreak Strains Using cgMLST Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fasanella, A.; Galante, D.; Garofolo, G.; Jones, M.H. Anthrax Undervalued Zoonosis. Vet. Microbiol. 2010, 140, 318–331. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Control of Neglected Zoonotic Diseases: Community Based Interventions for NZDs Prevention and Control: Report of the Third Conference Organized with ICONZ, DFID-RiU, SOS, EU, TDR and FAO with the Participation of ILRI and OIE: 23–24 November 2010, WHO Heaquarters, Geneva, Switzerland; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Swartz, M.N. Recognition and Management of Anthrax—An Update. N. Engl. J. Med. 2001, 345, 1621–1626. [Google Scholar] [CrossRef] [PubMed]
- Carlson, C.J.; Kracalik, I.T.; Ross, N.; Alexander, K.A.; Hugh-Jones, M.E.; Fegan, M.; Elkin, B.T.; Epp, T.; Shury, T.K.; Zhang, W.; et al. The Global Distribution of Bacillus anthracis and Associated Anthrax Risk to Humans, Livestock and Wildlife. Nat. Microbiol. 2019, 4, 1337–1343. [Google Scholar] [CrossRef] [PubMed]
- Bezymennyi, M.; Bagamian, K.H.; Barro, A.; Skrypnyk, A.; Skrypnyk, V.; Blackburn, J.K. Spatio-Temporal Patterns of Livestock Anthrax in Ukraine during the Past Century (1913–2012). Appl. Geogr. 2014, 54, 129–138. [Google Scholar] [CrossRef]
- Pilo, P.; Perreten, V.; Frey, J. Molecular Epidemiology of Bacillus anthracis: Determining the Correct Origin. Appl. Environ. Microbiol. 2008, 74, 2928–2931. [Google Scholar] [CrossRef]
- Timofeev, V.S.; Bakhteeva, I.V.; Dyatlov, I.A. Genotyping of Bacillus anthracis and Closely Related Microorganisms. Russ. J. Genet. 2018, 54, 1–11. [Google Scholar] [CrossRef]
- Turnbull, P.C.B. Anthrax in Humans and Animals, 4th ed.; World Health Organization: Geneva, Switzerland, 2008; ISBN 92-4-154753-7. [Google Scholar]
- Derzelle, S.; Thierry, S. Genetic Diversity of Bacillus anthracis in Europe: Genotyping Methods in Forensic and Epidemiologic Investigations. Biosecurity Bioterrorism Biodefense Strategy Pract. Sci. 2013, 11, S166–S176. [Google Scholar] [CrossRef] [PubMed]
- Mwakapeje, E.R.; Høgset, S.; Fyumagwa, R.; Nonga, H.E.; Mdegela, R.H.; Skjerve, E. Anthrax Outbreaks in the Humans-Livestock and Wildlife Interface Areas of Northern Tanzania: A Retrospective Record Review 2006–2016. BMC Public Health 2018, 18, 106. [Google Scholar] [CrossRef] [PubMed]
- Rondinone, V.; Serrecchia, L.; Parisi, A.; Fasanella, A.; Manzulli, V.; Cipolletta, D.; Galante, D. Genetic Characterization of Bacillus anthracis Strains Circulating in Italy from 1972 to 2018. PLoS ONE 2020, 15, e0227875. [Google Scholar] [CrossRef]
- Chiaverini, A.; Abdel-Glil, M.Y.; Linde, J.; Galante, D.; Rondinone, V.; Fasanella, A.; Cammà, C.; D’Alterio, N.; Garofolo, G.; Tomaso, H. Whole Genome Sequencing for Studying Bacillus anthracis from an Outbreak in the Abruzzo Region of Italy. Microorganisms 2020, 8, 87. [Google Scholar] [CrossRef]
- Abdel-Glil, M.Y.; Chiaverini, A.; Garofolo, G.; Fasanella, A.; Parisi, A.; Harmsen, D.; Jolley, K.A.; Elschner, M.C.; Tomaso, H.; Linde, J.; et al. A Whole-Genome-Based Gene-by-Gene Typing System for Standardized High-Resolution Strain Typing of Bacillus anthracis. J. Clin. Microbiol. 2021, 59, e02889-20. [Google Scholar] [CrossRef] [PubMed]
- Keim, P.; Van Ert, M.N.; Pearson, T.; Vogler, A.J.; Huynh, L.Y.; Wagner, D.M. Anthrax Molecular Epidemiology and Forensics: Using the Appropriate Marker for Different Evolutionary Scales. Infect. Genet. Evol. 2004, 4, 205–213. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.; Gorely, T. Family Correlates of Fruit and Vegetable Consumption in Children and Adolescents: A Systematic Review. Public Health Nutr. 2009, 12, 267–283. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.; Mohammad, I.; Warner, S.; Paskin, R.; Constable, F.; Fegan, M. Genetic Diversity of Australian Bacillus anthracis Isolates Revealed by Multiple-Locus Variable-Number Tandem Repeat Analysis. Microorganisms 2020, 8, 886. [Google Scholar] [CrossRef] [PubMed]
- Van Ert, M.N.; Easterday, W.R.; Huynh, L.Y.; Okinaka, R.T.; Hugh-Jones, M.E.; Ravel, J.; Zanecki, S.R.; Pearson, T.; Simonson, T.S.; U’Ren, J.M.; et al. Global Genetic Population Structure of Bacillus anthracis. PLoS ONE 2007, 2, e461. [Google Scholar] [CrossRef]
- Sahl, J.W.; Pearson, T.; Okinaka, R.; Schupp, J.M.; Gillece, J.D.; Heaton, H.; Birdsell, D.; Hepp, C.; Fofanov, V.; Noseda, R.; et al. A Bacillus anthracis Genome Sequence from the Sverdlovsk 1979 Autopsy Specimens. MBio 2016, 7, e01501-16. [Google Scholar] [CrossRef]
- Pieracci, E.G.; Hall, A.J.; Gharpure, R.; Haile, A.; Walelign, E.; Deressa, A.; Bahiru, G.; Kibebe, M.; Walke, H.; Belay, E. Prioritizing Zoonotic Diseases in Ethiopia Using a One Health Approach. One Health 2016, 2, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Romha, G.; Girmay, W. Knowledge, Attitude and Practice towards Anthrax in Northern Ethiopia: A Mixed Approach Study. BMC Infect. Dis. 2020, 20, 814. [Google Scholar] [CrossRef] [PubMed]
- Bahiru, G.; Bekele, A.; Seraw, B.; Boulanger, L.; Ali, A. Human and Animal Anthrax in Ethiopia: A Retrospective Record Review 2009–2013. Ethiop. Vet. J. 2016, 20, 76–85. [Google Scholar] [CrossRef]
- Abayneh, T.; Getachew, B.; Gelaye, E.; Traxler, R.; Vieira, A.R. Viability Evaluation of Freeze Dried and Suspension Anthrax Spore Vaccine Formulations Stored at Different Temperatures. Vaccine 2021, 39, 6245–6249. [Google Scholar] [CrossRef] [PubMed]
- Shiferaw, G. Anthrax in Wabessa Village in the Dessie Zuria District of Ethiopia. Rev. Sci. Tech. -Off. Int. Epizoot. 2004, 23, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Wassi, B.; Fantaw, S.; Mekonene, Y.; Teshale, A.M.; Yitagesu, Y.; Tsige, E.; Getahun, D.; Tasew, G.; Abichu, G.; Moges, B.; et al. First PCR Confirmed Anthrax Outbreaks in Ethiopia—Amhara Region, 2018–2019. PLoS Negl. Trop. Dis. 2022, 16, e0010181. [Google Scholar]
- Eremenko, E.; Pechkovskii, G.; Pisarenko, S.; Ryazanova, A.; Kovalev, D.; Semenova, O.G.; Aksenova, L.; Timchenko, L.; Golovinskaya, T.; Bobrisheva, O.G.; et al. Phylogenetics of Bacillus anthracis Isolates from Russia and Bordering Countries. Infect. Genet. Evol. 2021, 92, 104890. [Google Scholar] [CrossRef] [PubMed]
- Price, E.P.; Seymour, M.L.; Sarovich, D.S.; Latham, J.; Wolken, S.R.; Mason, J.; Vincent, G.; Drees, K.P.; Beckstrom-Sternberg, S.M.; Phillippy, A.M.; et al. Molecular Epidemiologic Investigation of an Anthrax Outbreak among Heroin Users, Europe. Emerg. Infect. Dis. 2012, 18, 1307. [Google Scholar] [CrossRef] [PubMed]
- Multisectoral Zoonotic Diseases Outbreak Investigation Guideline. Available online: http://onehealthethiopia.org/index.php/resources/strategies-and-guidelines/download/3-strategies-and-guidelines/20-multisectoral-zoonotic-diseases-outbreak-investigation-guideline (accessed on 10 February 2024).
- Aminu, O.R.; Lembo, T.; Zadoks, R.N.; Biek, R.; Lewis, S.; Kiwelu, I.; Mmbaga, B.T.; Mshanga, D.; Shirima, G.; Denwood, M.; et al. Practical and Effective Diagnosis of Animal Anthrax in Endemic Low-Resource Settings. PLoS Negl. Trop. Dis. 2020, 14, e0008655. [Google Scholar] [CrossRef] [PubMed]
- Carter, G.R. Bacillus. In Diagnostic Procedure in Veterinary Bacteriology and Mycology; Elsevier: Amsterdam, The Netherlands, 1990; pp. 221–228. [Google Scholar]
- Braun, P.; Beyer, W.; Hanczaruk, M.; Riehm, J.M.; Antwerpen, M.; Otterbein, C.; Oesterheld, J.; Grass, G. Reoccurring Bovine Anthrax in Germany on the Same Pasture after 12 Years. J. Clin. Microbiol. 2022, 60, e02291-21. [Google Scholar] [CrossRef] [PubMed]
- Fasanella, A.; Garofolo, G.; Hossain, M.J.; Shamsuddin, M.; Blackburn, J.K.; Hugh-Jones, M. Bangladesh Anthrax Outbreaks Are Probably Caused by Contaminated Livestock Feed. Epidemiol. Infect. 2013, 141, 1021–1028. [Google Scholar] [CrossRef]
- Dauphin, L.A.; Bowen, M.D. A Simple Method for the Rapid Removal of Bacillus anthracis Spores from DNA Preparations. J. Microbiol. Methods 2009, 76, 212–214. [Google Scholar] [CrossRef] [PubMed]
- Pisarenko, S.V.; Eremenko, E.I.; Kovalev, D.A.; Ryazanova, A.G.; Evchenko, A.Y.; Aksenova, L.Y.; Dugarzhapova, Z.F.; Kravets, E.V.; Semenova, O.V.; Bobrysheva, O.V.; et al. Molecular Genotyping of 15 B. Anthracis Strains Isolated in Eastern Siberia and Far East. Mol. Phylogenet. Evol. 2021, 159, 107116. [Google Scholar] [CrossRef]
- Ellerbrok, H.; Nattermann, H.; Özel, M.; Beutin, L.; Appel, B.; Pauli, G. Rapid and Sensitive Identification of Pathogenic and Apathogenic Bacillus anthracis by Real-Time PCR. FEMS Microbiol. Lett. 2002, 214, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Farina, D.; Bianco, A.; Manzulli, V.; Castellana, S.; Parisi, A.; Caruso, M.; Fraccalvieri, R.; Serrecchia, L.; Rondinone, V.; Pace, L.; et al. Antimicrobial and Phylogenomic Characterization of Bacillus cereus Group Strains Isolated from Different Food Sources in Italy. Antibiotics 2024, 13, 898. [Google Scholar] [CrossRef] [PubMed]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A New Genome Assembly Algorithm and Its Applications to Single-Cell Sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef]
- Mikheenko, A.; Prjibelski, A.; Saveliev, V.; Antipov, D.; Gurevich, A. Versatile Genome Assembly Evaluation with QUAST-LG. Bioinformatics 2018, 34, I142–I150. [Google Scholar] [CrossRef]
- Walker, B.J.; Abeel, T.; Shea, T.; Priest, M.; Abouelliel, A.; Sakthikumar, S.; Cuomo, C.A.; Zeng, Q.; Wortman, J.; Young, S.K.; et al. Pilon: An Integrated Tool for Comprehensive Microbial Variant Detection and Genome Assembly Improvement. PLoS ONE 2014, 9, e112963. [Google Scholar] [CrossRef]
- Angiuoli, S.V.; Gussman, A.; Klimke, W.; Cochrane, G.; Field, D.; Garrity, G.M.; Kodira, C.D.; Kyrpides, N.; Madupu, R.; Markowitz, V.; et al. Toward an Online Repository of Standard Operating Procedures (SOPs) for (Meta) Genomic Annotation. OMICS J. Integr. Biol. 2008, 12, 137–141. [Google Scholar] [CrossRef]
- Sloggett, C.; Goonasekera, N.; Afgan, E. BioBlend: Automating Pipeline Analyses within Galaxy and CloudMan. Bioinformatics 2013, 29, 1685–1686. [Google Scholar] [CrossRef] [PubMed]
- Köster, J.; Rahmann, S. Snakemake—A Scalable Bioinformatics Workflow Engine. Bioinformatics 2012, 28, 2520–2522. [Google Scholar] [CrossRef]
- Andrews, S. FastQC: A Quality Control Tool for High Throughput Sequence Data; Babraham Bioinformatics: Cambridge, UK, 2010. [Google Scholar]
- Wood, D.E.; Salzberg, S.L. Kraken: Ultrafast Metagenomic Sequence Classification Using Exact Alignments. Genome Biol. 2014, 15, R46. [Google Scholar] [CrossRef]
- Carroll, L.M.; Marston, C.K.; Kolton, C.B.; Gulvik, C.A.; Gee, J.E.; Weiner, Z.P.; Kovac, J. Strains Associated with Two 2020 Welder Anthrax Cases in the United States Belong to Separate Lineages within Bacillus cereus Sensu Lato. Pathogens 2022, 11, 856. [Google Scholar] [CrossRef]
- Liu, B.; Zheng, D.; Jin, Q.; Chen, L.; Yang, J. VFDB 2019: A Comparative Pathogenomic Platform with an Interactive Web Interface. Nucleic Acids Res. 2019, 47, D687–D692. [Google Scholar] [CrossRef] [PubMed]
- Seemann, T. ABRicate: Mass Screening of Contigs for Antimicrobial and Virulence Genes; Department of Microbiology and Immunology, The University of Melbourne: Melbourne, Australia, 2018. [Google Scholar]
- Feldgarden, M.; Brover, V.; Haft, D.H.; Prasad, A.B.; Slotta, D.J.; Tolstoy, I.; Tyson, G.H.; Zhao, S.; Hsu, C.-H.; McDermott, P.F.; et al. Validating the AMRFinder Tool and Resistance Gene Database by Using Antimicrobial Resistance Genotype-Phenotype Correlations in a Collection of Isolates. Antimicrob. Agents Chemother. 2019, 63, e00483-19. [Google Scholar] [CrossRef] [PubMed]
- Jain, C.; Rodriguez-R, L.M.; Phillippy, A.M.; Konstantinidis, K.T.; Aluru, S. High Throughput ANI Analysis of 90K Prokaryotic Genomes Reveals Clear Species Boundaries. Nat. Commun. 2018, 9, 5114. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Chen, Y.; Cai, G.; Cai, R.; Hu, Z.; Wang, H. Tree Visualization by One Table (tvBOT): A Web Application for Visualizing, Modifying and Annotating Phylogenetic Trees. Nucleic Acids Res. 2023, 51, W587–W592. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Alikhan, N.-F.; Sergeant, M.J.; Luhmann, N.; Vaz, C.; Francisco, A.P.; Carriço, J.A.; Achtman, M. GrapeTree: Visualization of Core Genomic Relationships among 100,000 Bacterial Pathogens. Genome Res. 2018, 28, 1395–1404. [Google Scholar] [CrossRef]
- Avberšek, J.; Mićunović, J.; Cociancich, V.; Paller, T.; Kušar, D.; Zajc, U.; Ocepek, M.; Špičić, S.; Duvnjak, S.; Pate, M. A Suggested Diagnostic Approach for Sporadic Anthrax in Cattle to Protect Public Health. Microorganisms 2021, 9, 1567. [Google Scholar] [CrossRef] [PubMed]
- Okinaka, R.T.; Cloud, K.; Hampton, O.; Hoffmaster, A.R.; Hill, K.K.; Keim, P.; Koehler, T.M.; Lamke, G.; Kumano, S.; Mahillon, J.; et al. Sequence and Organization of pXO1, the Large Bacillus anthracis Plasmid Harboring the Anthrax Toxin Genes. J. Bacteriol. 1999, 181, 6509–6515. [Google Scholar] [CrossRef] [PubMed]
- Antwerpen, M.; Beyer, W.; Bassy, O.; Ortega-García, M.V.; Cabria-Ramos, J.C.; Grass, G.; Wölfel, R. Phylogenetic Placement of Isolates within the Trans-Eurasian Clade A. Br. 008/009 of Bacillus anthracis. Microorganisms 2019, 7, 689. [Google Scholar] [CrossRef] [PubMed]
- Grunow, R.; Klee, S.R.; Beyer, W.; George, M.; Grunow, D.; Barduhn, A.; Klar, S.; Jacob, D.; Elschner, M.; Sandven, P.; et al. Anthrax among Heroin Users in Europe Possibly Caused by Same Bacillus anthracis Strain since 2000. Eurosurveillance 2013, 18, 20437. [Google Scholar] [CrossRef] [PubMed]
- Ringertz, S.H.; Høiby, E.A.; Jensenius, M.; Mæhlen, J.; Caugant, D.A.; Myklebust, A.; Fossum, K. Injectional Anthrax in a Heroin Skin-Popper. Lancet 2000, 356, 1574–1575. [Google Scholar] [CrossRef]
- Ramsay, C.N.; Stirling, A.; Smith, J.; Hawkins, G.; Brooks, T.; Hood, J.; Penrice, G.; Browning, L.M.; Ahmed, S. An Outbreak of Infection with Bacillus anthracis in Injecting Drug Users in Scotland. Eurosurveillance 2010, 15, 19465. [Google Scholar] [CrossRef] [PubMed]
- Beyer, W.; Bellan, S.; Eberle, G.; Ganz, H.H.; Getz, W.M.; Haumacher, R.; Hilss, K.A.; Kilian, W.; Lazak, J.; Turner, W.C.; et al. Distribution and Molecular Evolution of Bacillus anthracis Genotypes in Namibia. PLoS Negl. Trop. Dis. 2012, 6, e1534. [Google Scholar] [CrossRef] [PubMed]
- Lekota, K.E.; Hassim, A.; Madoroba, E.; Hefer, C.A.; Van Heerden, H. Phylogenomic Structure of Bacillus anthracis Isolates in the Northern Cape Province, South Africa Revealed Novel Single Nucleotide Polymorphisms. Infect. Genet. Evol. 2020, 80, 104146. [Google Scholar] [CrossRef] [PubMed]
- Pilo, P.; Frey, J. Pathogenicity, Population Genetics and Dissemination of Bacillus anthracis. Infect. Genet. Evol. 2018, 64, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; DeVos, V.; Bryden, H.; Price, L.B.; Hugh-Jones, M.E.; Keim, P. Bacillus anthracis Diversity in Kruger National Park. J. Clin. Microbiol. 2000, 38, 3780–3784. [Google Scholar] [CrossRef] [PubMed]
- Forde, T.L.; Dennis, T.P.; Aminu, O.R.; Harvey, W.T.; Hassim, A.; Kiwelu, I.; Medvecky, M.; Mshanga, D.; Van Heerden, H.; Vogel, A.; et al. Population Genomics of Bacillus anthracis from an Anthrax Hyperendemic Area Reveals Transmission Processes across Spatial Scales and Unexpected Within-Host Diversity. Microb. Genom. 2022, 8, 000759. [Google Scholar] [CrossRef]
- Kuroda, M.; Serizawa, M.; Okutani, A.; Sekizuka, T.; Banno, S.; Inoue, S. Genome-Wide Single Nucleotide Polymorphism Typing Method for Identification of Bacillus anthracis Species and Strains among B. Cereus Group Species. J. Clin. Microbiol. 2010, 48, 2821–2829. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Derzelle, S.; Aguilar-Bultet, L.; Frey, J. Comparative Genomics of Bacillus anthracis from the Wool Industry Highlights Polymorphisms of Lineage A. Br. Vollum. Infect. Genet. Evol. 2016, 46, 50–58. [Google Scholar] [CrossRef]
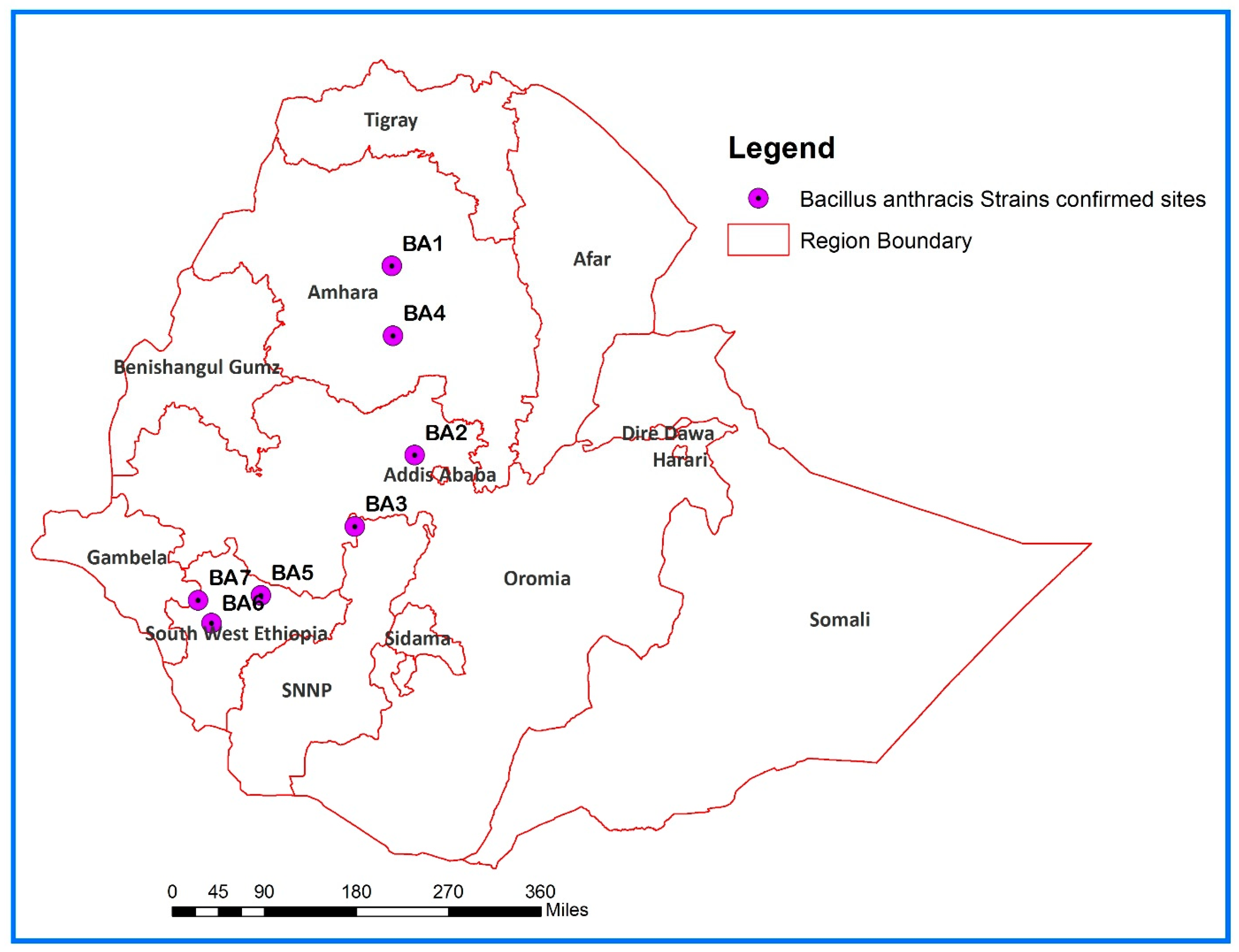


| ID Strain | Source | Year | Region | Zone | District | Kebele | Sample |
|---|---|---|---|---|---|---|---|
| BA1 | Goat | April 2019 | Amhara | South Gondar | Farta | Wowa | Dried meat |
| BA2 | Cow | June 2021 | Oromia | West-Shoa | Ada Berga | Bisha Dima | Bone swab |
| BA3 | Goat | December 2021 | SNNPR | Gurage | Abeshege | Layegnawgerabana Tachegnawtete | Ear tissue |
| BA4 | Goat | April 2022 | Amhara | East Gojjam | Goncha Siso Enese | Angot 028 | Skin contaminated with blood |
| BA5 | Cow | November 2022 | South West Ethiopia | Kefa | Bonga | 02 | Ear tissue, swab of oozing blood |
| BA6 | Cow | March 2023 | South West Ethiopia | Bench Sheko | South-Bench | Debrwork town | Ear tissue, swab of oozing blood |
| BA7 | Cow | 2024 | South West Ethiopia | Sheka | Yeki | Yeki | Ear tissue, swab of oozing blood |
| Target and Primers and Probes | Oligonucleotide Sequence (5′–3′) |
|---|---|
| PA-Forward: | CGG ATC AAG TAT ATG GGA ATA TAG CAA |
| PA-Reverse: | CCG GTT TAG TCG TTT CTA ATG GAT |
| PA-Probe: | FAM-CTC GAA CTG GAG TGA AGT GTT ACC GCA AAT-BHQ1 |
| Cap-Forward: | ACG TAT GGT GTT TCA AGA TTC ATG |
| Cap-Reverse: | ATT TTC GTC TCA TTC TAC CTC ACC |
| Cap-Probe: | FAM-CCA CGG AAT TCA AAA ATC TCA AAT GGC AT-BHQ1 |
| Strain | Total Number of Reads | GC % | No of Contigs | Total Length, bp | Average Contig Size | N50, bp | Average Coverage Depth | CDs | tRNA | RGF% * |
|---|---|---|---|---|---|---|---|---|---|---|
| BA1 | 1,654,914 | 35.09 | 30 | 5,449,014 | 1,597,919 | 601,456 | 37 | 5714 | 77 | 99.813 |
| BA2 | 1,593,126 | 35.09 | 30 | 5,449,551 | 1,769,796 | 1,162,562 | 39 | 5723 | 77 | 99.818 |
| BA4 | 1,995,290 | 35.10 | 36 | 5,448,948 | 919,145 | 540,904 | 48 | 5716 | 81 | 99.784 |
| BA5 | 2,057,654 | 36.09 | 33 | 5,447,787 | 1,162,720 | 918,280 | 49 | 5722 | 81 | 99.796 |
| BA6 | 1,644,654 | 35.09 | 30 | 5,449,018 | 1,768,025 | 1,198,320 | 41 | 5727 | 78 | 99.797 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olani, A.; Galante, D.; Lakew, M.; Wakjira, B.S.; Mekonnen, G.A.; Rufael, T.; Teklemariam, T.; Kumilachew, W.; Dejene, S.; Woldemeskel, A.; et al. Identification of Bacillus anthracis Strains from Animal Cases in Ethiopia and Genetic Characterization by Whole-Genome Sequencing. Pathogens 2025, 14, 39. https://doi.org/10.3390/pathogens14010039
Olani A, Galante D, Lakew M, Wakjira BS, Mekonnen GA, Rufael T, Teklemariam T, Kumilachew W, Dejene S, Woldemeskel A, et al. Identification of Bacillus anthracis Strains from Animal Cases in Ethiopia and Genetic Characterization by Whole-Genome Sequencing. Pathogens. 2025; 14(1):39. https://doi.org/10.3390/pathogens14010039
Chicago/Turabian StyleOlani, Abebe, Domenico Galante, Matios Lakew, Bayeta Senbeta Wakjira, Getnet Abie Mekonnen, Tesfaye Rufael, Tsegaye Teklemariam, Wondwosen Kumilachew, Shimalis Dejene, Ayele Woldemeskel, and et al. 2025. "Identification of Bacillus anthracis Strains from Animal Cases in Ethiopia and Genetic Characterization by Whole-Genome Sequencing" Pathogens 14, no. 1: 39. https://doi.org/10.3390/pathogens14010039
APA StyleOlani, A., Galante, D., Lakew, M., Wakjira, B. S., Mekonnen, G. A., Rufael, T., Teklemariam, T., Kumilachew, W., Dejene, S., Woldemeskel, A., Wakjira, A., Abichu, G., Ashenafi, B., Kebede, N., Feleke Haile, A., Bari, F. D., Del Sambro, L., & Eguale, T. (2025). Identification of Bacillus anthracis Strains from Animal Cases in Ethiopia and Genetic Characterization by Whole-Genome Sequencing. Pathogens, 14(1), 39. https://doi.org/10.3390/pathogens14010039







