Clinical Effects of Streptococcus salivarius K12 in Hospitalized COVID-19 Patients: Results of a Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
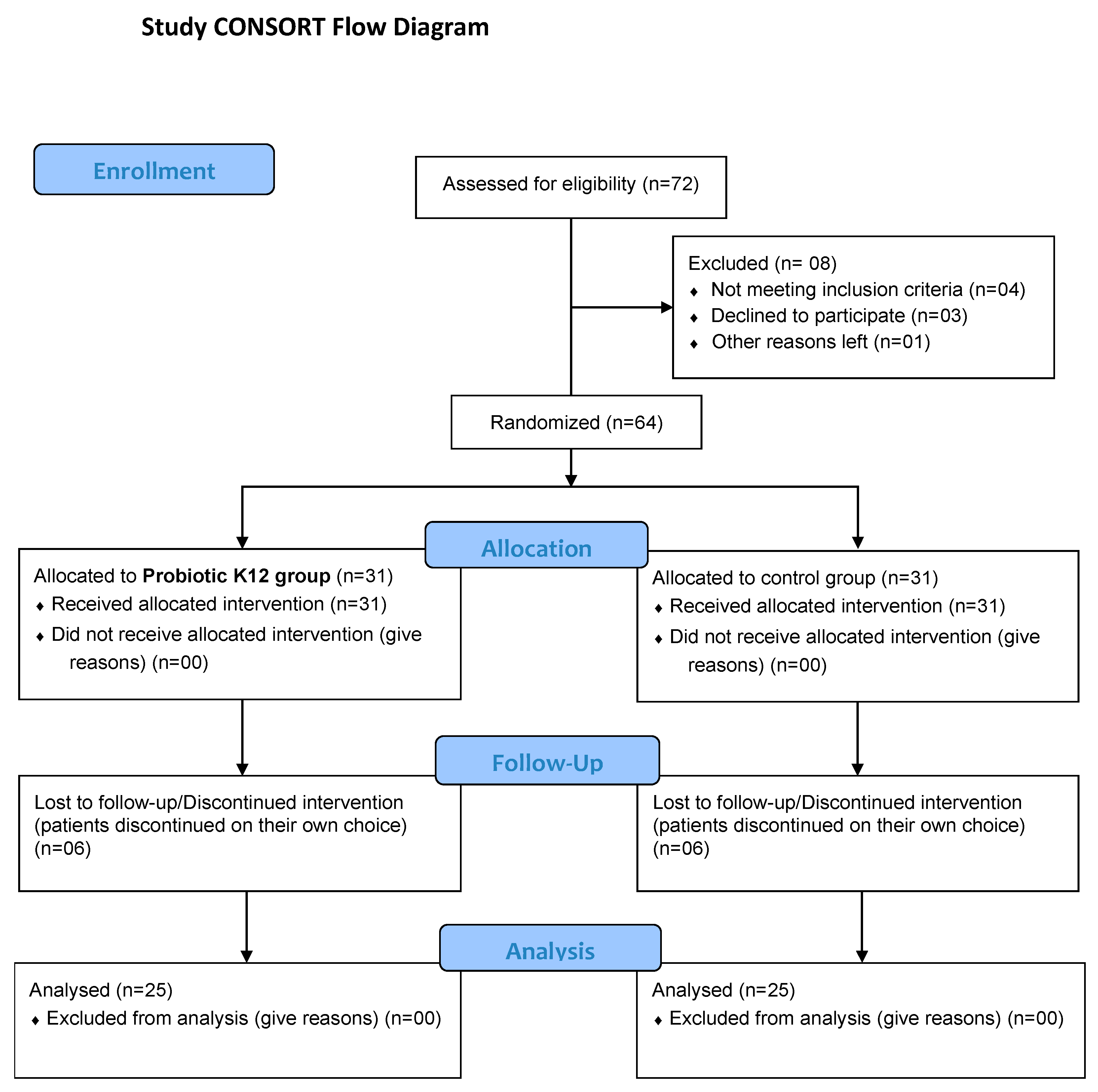
2.1. Study and Criteria
2.2. Treatment Protocol
2.3. Tested Product
2.4. Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, J.; Li, F.; Tian, Z. Role of microbiota on lung homeostasis and diseases. Sci. China Life Sci. 2017, 60, 1407–1415. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Xiao, Y.; Kang, L.; Ma, W.; Shi, L.; Zhang, L.; Zhou, Z.; Yang, J.; Zhong, J.; Yang, D.; et al. Genomic Diversity of Severe Acute Respiratory Syndrome–Coronavirus 2 in Patients With Coronavirus Disease 2019. Clin. Infect. Dis. 2020, 71, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Zemanick, E.T.; Wagner, B.D.; Robertson, C.E.; Ahrens, R.C.; Chmiel, J.F.; Clancy, J.P.; Gibson, R.L.; Harris, W.T.; Kurland, G.; Laguna, T.A.; et al. Airway microbiota across age and disease spectrum in cystic fibrosis. Eur. Respir. J. 2017, 50, 1700832. [Google Scholar] [CrossRef] [PubMed]
- Hilty, M.; Burke, C.; Pedro, H.; Cardenas, P.; Bush, A.; Bossley, C.; Davies, J.; Ervine, A.; Poulter, L.; Pachter, L.; et al. Disordered microbial communities in asthmatic airways. PLoS ONE 2010, 5, e8578. [Google Scholar] [CrossRef]
- Jia, G.; Zhi, A.; Lai, P.F.H.; Wang, G.; Xia, Y.; Xiong, Z.-Q.; Zhang, H.; Che, N.; Ai, L. The oral microbiota—A mechanistic role for systemic diseases. Br. Dent. J. 2018, 224, 447–455. [Google Scholar] [CrossRef]
- Wang, J.; Li, F.; Sun, R.; Gao, X.; Wei, H.; Li, L.-J.; Tian, Z. Bacterial colonization dampens influenza-mediated acute lung injury via induction of M2 alveolar macrophages. Nat. Commun. 2013, 4, 2106. [Google Scholar] [CrossRef]
- Hoogerwerf, J.J.; de Vos, A.F.; Bresser, P.; van der Zee, J.S.; Pater, J.M.; de Boer, A.; Tanck, M.; Lundell, D.L.; Her-Jenh, C.; Draing, C.; et al. Lung Inflammation Induced by Lipoteichoic Acid or Lipopolysaccharide in Humans. Am. J. Respir. Crit. Care Med. 2008, 178, 34–41. [Google Scholar] [CrossRef]
- Akata, K.; van Eeden, S.F. Lung Macrophage Functional Properties in Chronic Obstructive Pulmonary Disease. Int. J. Mol. Sci. 2020, 21, 853. [Google Scholar] [CrossRef]
- Bradley, E.S.; Zeamer, A.L.; Bucci, V.; Cincotta, L.; Salive, M.C.; Dutta, P.; Mutaawe, S.; Anya, O.; Tocci, C.; Moormann, A.; et al. Oropharyngeal Microbiome Profiled at Admission is Predictive of the Need for Respiratory Support Among COVID-19 Patients. Med. Rxiv. 2022, Preprint. [Google Scholar] [CrossRef]
- Khan, A.A.; Khan, Z. COVID-2019-associated overexpressed Prevotella proteins mediated host–pathogen interactions and their role in coronavirus outbreak. Bioinformatics 2020, 36, 4065–4069. [Google Scholar] [CrossRef]
- Rosas-Salazar, C.; Kimura, K.S.; Shilts, M.H.; Strickland, B.A.; Freeman, M.H.; Wessinger, B.C.; Gupta, V.; Brown, H.M.; Rajagopala, S.V.; Turner, J.H.; et al. SARS-CoV-2 infection and viral load are associated with the upper respiratory tract microbiome. J. Allergy Clin. Immunol. 2021, 147, 1226–1233.e2. [Google Scholar] [CrossRef] [PubMed]
- Haran, J.P.; Bradley, E.; Zeamer, A.L.; Cincotta, L.; Salive, M.-C.; Dutta, P.; Mutaawe, S.; Anya, O.; Meza-Segura, M.; Moormann, A.M.; et al. Inflammation-type dysbiosis of the oral microbiome associates with the duration of COVID-19 symptoms and long COVID. JCI Insight 2021, 6, e152346. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Liu, S.; Zhang, Z.; Lee, X.; Wu, W.; Huang, Z.; Lei, Z.; Xu, W.; Chen, D.; Wu, X.; et al. Association between the nasopharyngeal microbiome and metabolome in patients with COVID-19. Synth. Syst. Biotechnol. 2021, 6, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Ventero, M.P.; Cuadrat, R.R.C.; Vidal, I.; Andrade, B.G.N.; Molina-Pardines, C.; Haro-Moreno, J.M.; Coutinho, F.H.; Merino, E.; Regitano, L.C.A.; Silveira, C.B.; et al. Nasopharyngeal Microbial Communities of Patients Infected With SARS-CoV-2 That Developed COVID-19. Front. Microbiol. 2021, 12, 637430. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.H.; Annavajhala, M.K.; Chong, A.M.; Park, H.; Nobel, Y.R.; Soroush, A.; Blackett, J.W.; Krigel, A.; Phipps, M.M.; Freedberg, D.E.; et al. Oral Microbiome Alterations and SARS-CoV-2 Saliva Viral Load in Patients with COVID-19. Microbiol. Spectr. 2021, 9, e0005521. [Google Scholar] [CrossRef] [PubMed]
- Tamanai-Shacoori, Z.; Le Gall-David, S.; Moussouni, F.; Sweidan, A.; Polard, E.; Bousarghin, L.; Jolivet-Gougeon, A. SARS-CoV-2 and Prevotella spp.: Friend or foe? A systematic literature review. J. Med. Microbiol. 2022, 71, 001520. [Google Scholar] [CrossRef]
- Iebba, V.; Zanotta, N.; Campisciano, G.; Zerbato, V.; Di Bella, S.; Cason, C.; Luzzati, R.; Confalonieri, M.; Palamara, A.T.; Comar, M. Profiling of Oral Microbiota and Cytokines in COVID-19 Patients. Front. Microbiol. 2021, 12, 671813. [Google Scholar] [CrossRef]
- Di Pierro, F. A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SAR S-CoV-2. Minerva Medica 2020, 111, 281–283. [Google Scholar] [CrossRef]
- Cernioglo, K.; Kalanetra, K.M.; Meier, A.; Lewis, Z.T.; Underwood, M.A.; Mills, D.A.; Smilowitz, J.T. Multi-Strain Probiotic Supplementation with a Product Containing Human-Native S. salivarius K12 in Healthy Adults Increases Oral S. salivarius. Nutrients 2021, 13, 4392. [Google Scholar] [CrossRef]
- Li, S.; Yang, S.; Zhou, Y.; Disoma, C.; Dong, Z.; Du, A.; Zhang, Y.; Chen, Y.; Huang, W.; Chen, J.; et al. Microbiome Profiling Using Shotgun Metagenomic Sequencing Identified Unique Microorganisms in COVID-19 Patients With Altered Gut Microbiota. Front. Microbiol. 2021, 12, 712081. [Google Scholar] [CrossRef]
- Filkins, L.M.; Hampton, T.; Gifford, A.H.; Gross, M.J.; Hogan, D.A.; Sogin, M.L.; Morrison, H.; Paster, B.J.; O’Toole, G.A. Prevalence of Streptococci and Increased Polymicrobial Diversity Associated with Cystic Fibrosis Patient Stability. J. Bacteriol. 2012, 194, 4709–4717. [Google Scholar] [CrossRef]
- Bao, L.; Zhang, C.; Dong, J.; Zhao, L.; Li, Y.; Sun, J. Oral Microbiome and SARS-CoV-2: Beware of Lung Co-infection. Front. Microbiol. 2020, 11, 1840. [Google Scholar] [CrossRef] [PubMed]
- Di Pierro, F.; Colombo, M. The administration of S. salivarius K12 to children may reduce the rate of SARS-CoV-2 infection. Minerva Med. 2021, 112, 514–516. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Lin, X.; Xiang, X.; Liu, W.; Fang, Y.; Chen, H.; Tang, F.; Guo, H.; Chen, D.; Hu, X.; et al. Oropharyngeal Probiotic ENT-K12 Prevents Respiratory Tract Infections among Frontline Medical Staff Fighting Against COVID-19: A Pilot Study. Front. Bioeng. Biotechnol. 2021, 9, 646184. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, C.; Stuart, B.; Leaver, H.; Lown, M.; Willcox, M.; Moore, M.; Little, P. Effectiveness of the probiotic Streptococcus salivarius K12 for the treatment and/or prevention of sore throat: A systematic review. Clin. Microbiol. Infect. 2019, 25, 673–680. [Google Scholar] [CrossRef]
- Burton, J.P.; Chilcott, C.N.; Wescombe, P.A.; Tagg, J.R. Extended Safety Data for the Oral Cavity Probiotic Streptococcus salivarius K12. Probiotics Antimicrob. Proteins 2010, 2, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Burton, J.; Cowley, S.; Simon, R.; McKinney, J.; Wescombe, P.; Tagg, J. Evaluation of safety and human tolerance of the oral probiotic Streptococcus salivarius K12: A randomized, placebo-controlled, double-blind study. Food Chem. Toxicol. 2011, 49, 2356–2364. [Google Scholar] [CrossRef] [PubMed]
- Burton, J.P.; Wescombe, P.A.; Moore, C.J.; Chilcott, C.N.; Tagg, J.R. Safety Assessment of the Oral Cavity Probiotic Streptococcus salivarius K12. Appl. Environ. Microbiol. 2006, 72, 3050–3053. [Google Scholar] [CrossRef]
- Moffatt, M.F.; Cookson, W.O. The lung microbiome in health and disease. Clin. Med. (Lond.) 2017, 17, 525–529. [Google Scholar] [CrossRef]
- Mammen, M.J.; Scannapieco, F.A.; Sethi, S. Oral-lung microbiome interactions in lung diseases. Periodontology 2020, 83, 234–241. [Google Scholar] [CrossRef]
- Huffnagle, G.B.; Dickson, R.P.; Lukacs, N.W. The respiratory tract microbiome and lung inflammation: A two-way street. Mucosal Immunol. 2017, 10, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Yadava, K.; Pattaroni, C.; Sichelstiel, A.K.; Trompette, A.; Gollwitzer, E.S.; Salami, O.; von Garnier, C.; Nicod, L.P.; Marsland, B.J. Microbiota Promotes Chronic Pulmonary Inflammation by Enhancing IL-17A and Autoantibodies. Am. J. Respir. Crit. Care Med. 2016, 193, 975–987. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Gail, M.H.; Consonni, D.; Carugno, M.; Humphrys, M.; Pesatori, A.C.; Caporaso, N.E.; Goedert, J.J.; Ravel, J.; Landi, M.T. Characterizing human lung tissue microbiota and its relationship to epidemiological and clinical features. Genome Biol. 2016, 17, 163. [Google Scholar] [CrossRef] [PubMed]
- Delahooke, D.M.; Barclay, G.R.; Poxton, I.R. A re-appraisal of the biological activity of bacteroides LPS. J. Med. Microbiol. 1995, 42, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Di Pierro, F.; Risso, P.; Poggi, E.; Timitilli, A.; Bolloli, S.; Bruno, M.; Caneva, E.; Riccardo, C.; Giannattasio, A. Use of Streptococcus salivarius K12 to reduce the incidence of pharyngo-tonsillitis and acute otitis media in children: A retrospective analysis in not-recurrent pediatric subjects. Minerva Pediatr. 2018, 70, 240–245. [Google Scholar] [CrossRef]
- Di Pierro, F.; Colombo, M.; Giuliani, M.G.; Danza, M.L.; Basile, I.; Bollani, T.; Conti, A.M.; Zanvit, A.; Rottoli, A.S. Effect of administration of Streptococcus salivarius K12 on the occurrence of streptococcal pharyngo-tonsillitis, scarlet fever and acute otitis media in 3 years old children. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4601–4606. [Google Scholar]
- Di Pierro, F.; Colombo, M.; Zanvit, A.; Rottoli, A.S. Positive clinical outcomes derived from using Streptococcus salivarius K12 to prevent streptococcal pharyngotonsillitis in children: A pilot investigation. Drug Health Patient Saf. 2016, 8, 77–81. [Google Scholar] [CrossRef]
- Di Pierro, F.; Colombo, M.; Zanvit, A.; Risso, P.; Rottoli, A. Use of Streptococcus salivarius K12 in the prevention of streptococcal and viral pharyngotonsillitis in children. Drug Health Patient Saf. 2014, 6, 15–20. [Google Scholar] [CrossRef]
- Di Pierro, F.; Di Pasquale, D.; Di Cicco, M. Oral use of Streptococcus salivarius K12 in children with secretory otitis media: Preliminary results of a pilot, uncontrolled study. Int. J. Gen. Med. 2015, 8, 303–308. [Google Scholar] [CrossRef]
- Di Pierro, F.; Adami, T.; Rapacioli, G.; Giardini, N.; Streitberger, C. Clinical evaluation of the oral probiotic Streptococcus salivarius K12 in the prevention of recurrent pharyngitis and/or tonsillitis caused by Streptococcus pyogenes in adults. Expert Opin. Biol. Ther. 2012, 13, 339–343. [Google Scholar] [CrossRef]
- Marini, G.; Sitzia, E.; Panatta, M.L.; De Vincentiis, G.C. Pilot study to explore the prophylactic efficacy of oral probiotic Streptococcus salivarius K12 in preventing recurrent pharyngo-tonsillar episodes in pediatric patients. Int. J. Gen. Med. 2019, 12, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Hyink, O.; Wescombe, P.A.; Upton, M.; Ragland, N.; Burton, J.P.; Tagg, J.R. Salivaricin A2 and the Novel Lantibiotic Salivaricin B Are Encoded at Adjacent Loci on a 190-Kilobase Transmissible Megaplasmid in the Oral Probiotic Strain Streptococcus salivarius K12. Appl. Environ. Microbiol. 2007, 73, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Mokhtar, M.; Rismayuddin, N.A.R.; Yassim, A.S.M.; Ahmad, H.; Wahab, R.A.; Dashper, S.; Arzmi, M.H. Streptococcus salivarius K12 inhibits Candida albicans aggregation, biofilm formation and dimorphism. Biofouling 2021, 37, 767–776. [Google Scholar] [CrossRef]
- MacDonald, K.W.; Chanyi, R.M.; Macklaim, J.M.; Cadieux, P.A.; Reid, G.; Burton, J.P. Streptococcus salivarius inhibits immune activation by periodontal disease pathogens. BMC Oral Health 2021, 21, 245. [Google Scholar] [CrossRef] [PubMed]
- Adam, E. Streptococcus salivarius K12 and M18 Probiotics Reduce Periodontal Pathogen-Induced Inflammation. Meeting. 2011; IADR/AADR/CADR General Session (San Diego, California). Poster Session: Systemic Antibiotics, Antimicrobials, and Immune Modulators. Available online: https://www.researchgate.net/publication/266764016_Streptococcus_salivarius_K12_and_M18_Probiotics_Reduce_Periodontal_Pathogen-induced_Inflammation (accessed on 11 September 2022).
- Channappanavar, R.; Perlman, S. Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology. Semin. Immunopathol. 2017, 39, 529–539. [Google Scholar] [CrossRef]
- Bouwer, A.L.; Saunderson, S.C.; Dunn, A.C.; Lester, K.L.; Crowley, L.R.; Jack, R.W.; McLellan, A.D. Rapid Interferon-Gamma Release from Natural Killer Cells Induced by a Streptococcal Commensal. J. Interf. Cytokine Res. 2013, 33, 459–466. [Google Scholar] [CrossRef]
- Wescombe, P.A.; Hale, J.D.; Heng, N.C.; Tagg, J.R. Developing oral probiotics from Streptococcus salivarius. Future Microbiol. 2012, 7, 1355–1371. [Google Scholar] [CrossRef]
- Laws, G.L.; Hale, J.D.F.; Kemp, R.A. Human Systemic Immune Response to Ingestion of the Oral Probiotic Streptococcus salivarius BLIS K12. Probiotics Antimicrob. Proteins 2021, 13, 1521–1529. [Google Scholar] [CrossRef]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef]


| Group SOC | Group K12 | p = 0.2121 | |
|---|---|---|---|
| N | 25 | 25 | |
| Sex: male/female | 16/9 | 13/12 | |
| Age (both sex) | 51.3 ± 16.0 | 45.8 ± 14.6 | |
| Male age | 51.2 ± 15.4 | 50.2 ± 13.0 | |
| Female age | 51.4 ± 18.1 | 41.1 ± 15.3 |
| Pathologies | Number of Patients | ||
|---|---|---|---|
| Group SOC | Group K12 | p = 0.5436 | |
| Allergic asthma | 1 | 0 | |
| Autoimmune disorder (AD) | 1 | 1 | |
| Non-Hodgkin’s lymphoma | 0 | 1 | |
| Chronic kidney disease (CKD) | 0 | 1 | |
| Diabetes mellitus (DM) | 1 | 1 | |
| CKD + DM | 1 | 1 | |
| Chronic liver disease | 2 | 0 | |
| Coronary artery disease (CAD) | 2 | 0 | |
| Dengue fever | 0 | 1 | |
| DM + AD | 0 | 1 | |
| DM + breast cancer | 1 | 0 | |
| DM + hypercholesterolemia | 0 | 2 | |
| Hypertension (Ht) | 2 | 7 | |
| DM + CAD + Ht | 2 | 1 | |
| DM + obesity | 0 | 2 | |
| DM + psoriasis | 0 | 1 | |
| DM + Ht | 2 | 0 | |
| DM + Ht + others | 0 | 1 | |
| DM + others | 0 | 1 | |
| Others | 10 | 3 | |
| Mean | 1.72 | 1.68 | |
| Parameters (M ± SD) | Group SOC | Group K12 | p * |
|---|---|---|---|
| CRP | 100.28 ± 56.71 | 75.60 ± 41.95 | 0.0872 |
| D-dimer | 1.99 ± 1.16 | 2.33 ± 1.76 | 0.4146 |
| LDH | 460.24 ± 186.61 | 400.68 ± 175.97 | 0.2514 |
| Ferritin | 910.44 ± 528.57 | 793.58 ± 467.46 | 0.4161 |
| O2 saturation (%) | 93.72 ± 1.40 | 92.58 ± 2–95 | 0.0963 |
| Volume O2 (L/min) | SOC (%) | K12 (%) | p = 0.0416 |
|---|---|---|---|
| 0 | 2 (8) | 5 (23.81) | |
| 1 | 0 (0) | 1 (4.76) | |
| 2 | 0 (0) | 4 (19.05) | |
| 3 | 2 (8) | 0 (0) | |
| 4 | 1 (4) | 0 (0) | |
| 5 | 2 (8) | 5 (23.81) | |
| 8 | 4 (16) | 2 (9.52) | |
| 10 | 4 (16) | 0 (0) | |
| 12 | 4 (16) | 2 (9.52) | |
| 15 | 3 (12) | 2 (9.52) | |
| 20 | 3 (12) | 0 (0) | |
| Total patients | 25 (100) | 21 (80.95) |
| Parameter | SOC | K12 | p * | ||
|---|---|---|---|---|---|
| ≤Day 1 | >Day 1 | ≤Day 1 | >Day 1 | ||
| CRP | 14 | 11 | 16 | 9 | 0.5637 |
| D-dimer | 12 | 13 | 14 | 11 | 0.5713 |
| LDH | 9 | 16 | 15 | 10 | 0.1573 |
| Ferritin | 6 | 19 | 13 | 11 | 0.0303 |
| Oxygen saturation | 7 | 18 | 6 | 18 | 0.8121 |
| Fever | 23 | 2 | 25 | 0 | 0.1489 |
| Supplementary oxygen | 8 | 17 | 14 | 8 | 0.0301 |
| SOC (%) | K12 (%) | |
|---|---|---|
| Died before being transferred to ICU | 2 | 0 |
| Transferred to ICU | 8 | 8 |
| Died in ICU | 6 | 3 |
| Recovery from ICU | 2 | 5 |
| Total deaths | 8 | 3 |
| Parameter | SOC | K12 | * p = 0.0022 | ||
|---|---|---|---|---|---|
| Lower | Higher | Lower | Higher | ||
| Dead | 0 | 8 | 0 | 2 | |
| Alive | 8 | 9 | 15 | 5 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Pierro, F.; Iqtadar, S.; Mumtaz, S.U.; Bertuccioli, A.; Recchia, M.; Zerbinati, N.; Khan, A. Clinical Effects of Streptococcus salivarius K12 in Hospitalized COVID-19 Patients: Results of a Preliminary Study. Microorganisms 2022, 10, 1926. https://doi.org/10.3390/microorganisms10101926
Di Pierro F, Iqtadar S, Mumtaz SU, Bertuccioli A, Recchia M, Zerbinati N, Khan A. Clinical Effects of Streptococcus salivarius K12 in Hospitalized COVID-19 Patients: Results of a Preliminary Study. Microorganisms. 2022; 10(10):1926. https://doi.org/10.3390/microorganisms10101926
Chicago/Turabian StyleDi Pierro, Francesco, Somia Iqtadar, Sami Ullah Mumtaz, Alexander Bertuccioli, Martino Recchia, Nicola Zerbinati, and Amjad Khan. 2022. "Clinical Effects of Streptococcus salivarius K12 in Hospitalized COVID-19 Patients: Results of a Preliminary Study" Microorganisms 10, no. 10: 1926. https://doi.org/10.3390/microorganisms10101926
APA StyleDi Pierro, F., Iqtadar, S., Mumtaz, S. U., Bertuccioli, A., Recchia, M., Zerbinati, N., & Khan, A. (2022). Clinical Effects of Streptococcus salivarius K12 in Hospitalized COVID-19 Patients: Results of a Preliminary Study. Microorganisms, 10(10), 1926. https://doi.org/10.3390/microorganisms10101926









