Imaging of Musculoskeletal Soft-Tissue Infections in Clinical Practice: A Comprehensive Updated Review
Abstract
:1. Introduction
2. Imaging of Soft-Tissue infections: General Considerations
2.1. Cellulitis
2.2. Necrotizing and Non-Necrotizing Fascitiis
2.3. Soft-Tissue Foreign Body
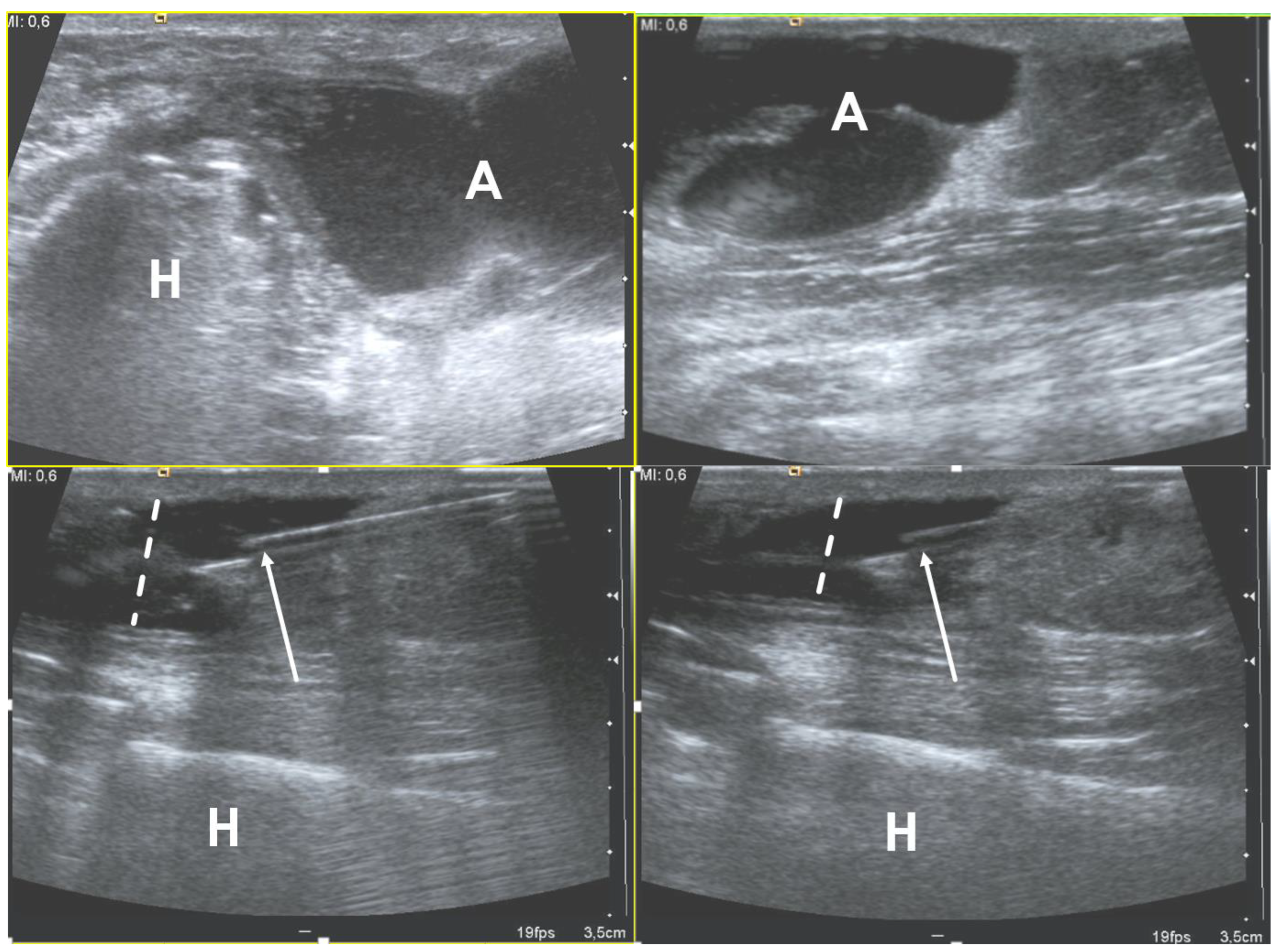
2.4. Abscess
2.5. Infectious Myositis
2.6. Infectious Tenosynovitis and Bursitis
3. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turecki, M.B.; Taljanovic, M.S.; Stubbs, A.Y.; Graham, A.R.; Holden, D.A.; Hunter, T.B.; Rogers, L.F. Imaging of Musculoskeletal Soft Tissue Infections. Skelet. Radiol. 2010, 39, 957–971. [Google Scholar] [CrossRef] [PubMed]
- Altmayer, S.; Verma, N.; Dicks, E.A.; Oliveira, A. Imaging Musculoskeletal Soft Tissue Infections. Semin. Ultrasound. CT MR 2020, 41, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Headley, A.J. Necrotizing soft tissue infections: A primary care review. Am. Fam. Physician 2003, 68, 323–328. [Google Scholar]
- McHenry, C.R.; Piotrowski, J.J.; Petrinic, D.; Malangoni, M.A. Determinants of Mortality for Necrotizing Soft-Tissue Infections. Ann. Surg. 1995, 221, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Bosshardt, T.L.; Henderson, V.J.; Organ, C.H. Necrotizing soft-tissue infections. Arch. Surg. 1996, 131, 846–852. [Google Scholar] [CrossRef]
- Chauhan, S.; Jain, S.; Varma, S.; Chauhan, S.S. Tropical pyomyositis (myositis tropicans): Current perspective. Postgrad. Med. J. 2004, 80, 267–270. [Google Scholar] [CrossRef] [Green Version]
- Elliott, D.; Kufera, J.A.; Myers, R.A. The microbiology of necrotizing soft tissue infections. Am. J. Surg. 2000, 179, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.K.; Sanders, C.V. Skin and soft tissue infections in critical care. Crit. Care Clin. 1998, 14, 251–262. [Google Scholar] [CrossRef]
- Bystritsky, R.J. Cellulitis. Infect. Dis. Clin. N. Am. 2021, 35, 49–60. [Google Scholar] [CrossRef]
- Stevens, D.L.; Bryant, A.E.; Goldstein, E.J. Necrotizing soft tissue infections. Infect. Dis. Clin. N. Am. 2021, 35, 135–155. [Google Scholar] [CrossRef]
- Hayeri, M.R.; Ziai, P.; Shehata, M.L.; Teytelboym, O.M.; Huang, B.K. Soft-tissue infections and their imaging mimics: From cellulitis to necrotizing fasciitis. Radiographics 2016, 36, 1888–1910. [Google Scholar] [CrossRef]
- Simpfendorfer, C.S. Radiologic approach to musculoskeletal infections. Infect. Dis. Clin. N. Am. 2017, 31, 299–324. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-D.; Wu, J.S. Imaging of musculoskeletal soft tissue infection. Semin. Roentgenol. 2017, 52, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.S.; Habib, P. MR imaging of urgent inflammatory and infectious conditions affecting the soft tissues of the musculoskeletal system. Emerg. Radiol. 2009, 16, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Schmid, M.R.; Kossmann, T.; Duewell, S. Differentiation of necrotizing fasciitis and cellulitis using mr imaging. AJR Am. J. Roentgenol. 1998, 170, 615–620. [Google Scholar] [CrossRef]
- Kim, H.S.; Lee, J.; Yi, S.Y.; Jun, H.J.; Choi, Y.-L.; Ahn, G.H.; Seo, S.W.; Lim, D.H.; Ahn, Y.C.; Park, J.O.; et al. Liposarcoma: Exploration of clinical prognostic factors for risk based stratification of therapy. BMC Cancer 2009, 9, 205. [Google Scholar] [CrossRef] [Green Version]
- Garcia, N.M.; Cai, J. Aggressive soft tissue infections. Surg. Clin. N. Am. 2018, 98, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, J.; Gottlieb, M.; Long, B.; Perkins, J.C. Necrotizing soft tissue infections (NSTI): Pearls and pitfalls for the emergency clinician. J. Emerg. Med. 2022, 62, 480–491. [Google Scholar] [CrossRef] [PubMed]
- Stevens, D.L.; Bryant, A.E. Necrotizing Soft-Tissue Infections. N. Engl. J. Med. 2017, 377, 2253–2265. [Google Scholar] [CrossRef] [PubMed]
- Paz Maya, S.; Dualde Beltrán, D.; Lemercier, P.; Leiva-Salinas, C. Necrotizing fasciitis: An urgent diagnosis. Skelet. Radiol. 2014, 43, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Malghem, J.; Lecouvet, F.E.; Omoumi, P.; Maldague, B.E.; Vande Berg, B.C. Necrotizing fasciitis: Contribution and limitations of diagnostic imaging. Jt. Bone Spine 2013, 80, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.-H.; Khin, L.-W.; Heng, K.-S.; Tan, K.-C.; Low, C.-O. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit. Care Med. 2004, 32, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Fernando, S.M.; Tran, A.; Cheng, W.; Rochwerg, B.; Kyeremanteng, K.; Seely, A.J.E.; Inaba, K.; Perry, J.J. Necrotizing soft tissue infection: Diagnostic accuracy of physical examination, imaging, and lrinec score: A systematic review and meta-analysis. Ann. Surg. 2019, 269, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Tso, D.K.; Singh, A.K. Necrotizing fasciitis of the lower extremity: Imaging pearls and pitfalls. Br. J. Radiol. 2018, 91, 20180093. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, A.A.; Baker, K.S.; Gould, E.S.; Gupta, R. Necrotizing fasciitis and its mimics: What radiologists need to know. AJR Am. J. Roentgenol. 2015, 204, 128–139. [Google Scholar] [CrossRef]
- Lahham, S.; Shniter, I.; Desai, M.; Andary, R.; Saadat, S.; Fox, J.C.; Pierce, S. Point of care ultrasound in the diagnosis of necrotizing fasciitis. Am. J. Emerg. Med. 2022, 51, 397–400. [Google Scholar] [CrossRef]
- Castleberg, E.; Jenson, N.; Dinh, V.A. Diagnosis of necrotizing faciitis with bedside ultrasound: The STAFF exam. West. J. Emerg. Med. 2014, 15, 111–113. [Google Scholar] [CrossRef]
- Shyy, W.; Knight, R.S.; Goldstein, R.; Isaacs, E.D.; Teismann, N.A. Sonographic findings in necrotizing fasciitis: Two ends of the spectrum. J. Ultrasound Med. 2016, 35, 2273–2277. [Google Scholar] [CrossRef]
- Kehrl, T. Point-of-Care ultrasound diagnosis of necrotizing fasciitis missed by computed tomography and magnetic resonance imaging. J. Emerg. Med. 2014, 47, 172–175. [Google Scholar] [CrossRef]
- Lin, C.-N.; Hsiao, C.-T.; Chang, C.-P.; Huang, T.-Y.; Hsiao, K.-Y.; Chen, Y.-C.; Fann, W.-C. The relationship between fluid accumulation in ultrasonography and the diagnosis and prognosis of patients with necrotizing fasciitis. Ultrasound Med. Biol. 2019, 45, 1545–1550. [Google Scholar] [CrossRef]
- Ballard, D.H. Presence of deep fascial fluid in imaging necrotizing fasciitis: Importance of this feature in diagnosing necrotizing fasciitis without imaging manifestations of soft tissue gas. Ultrasound Med. Biol. 2019, 45, 3081. [Google Scholar] [CrossRef] [PubMed]
- Kwee, R.M.; Kwee, T.C. Diagnostic performance of mri and ct in diagnosing necrotizing soft tissue infection: A systematic review. Skelet. Radiol. 2022, 51, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Carbonetti, F.; Cremona, A.; Carusi, V.; Guidi, M.; Iannicelli, E.; Di Girolamo, M.; Sergi, D.; Clarioni, A.; Baio, G.; Antonelli, G.; et al. The role of contrast enhanced computed tomography in the diagnosis of necrotizing fasciitis and comparison with the laboratory risk indicator for necrotizing fasciitis (LRINEC). Radiol. Med. 2016, 121, 106–121. [Google Scholar] [CrossRef] [PubMed]
- Bruls, R.J.M.; Kwee, R.M. CT in necrotizing soft tissue infection: Diagnostic criteria and comparison with LRINEC score. Eur. Radiol. 2021, 31, 8536–8541. [Google Scholar] [CrossRef]
- McGillicuddy, E.A.; Lischuk, A.W.; Schuster, K.M.; Kaplan, L.J.; Maung, A.; Lui, F.Y.; Bokhari, S.A.J.; Davis, K.A. Development of a computed tomography-based scoring system for necrotizing soft-tissue infections. J. Trauma. 2011, 70, 894–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.-T.; Kim, Y.J.; Won Lee, J.; Kim, Y.J.; Park, S.-W.; Lim, M.K.; Suh, C.H. Can necrotizing infectious fasciitis be differentiated from nonnecrotizing infectious fasciitis with mr imaging? Radiology 2011, 259, 816–824. [Google Scholar] [CrossRef]
- Yoon, M.A.; Chung, H.W.; Yeo, Y.; Yoo, H.J.; Kang, Y.; Chee, C.G.; Lee, M.H.; Lee, S.H.; Shin, M.J. Distinguishing necrotizing from non-necrotizing fasciitis: A new predictive scoring integrating MRI in the LRINEC score. Eur. Radiol. 2019, 29, 3414–3423. [Google Scholar] [CrossRef]
- Kim, M.-C.; Kim, S.; Cho, E.B.; Lee, G.Y.; Choi, S.-H.; Kim, S.O.; Chung, J.-W. Utility of magnetic resonance imaging for differentiating necrotizing fasciitis from severe cellulitis: A magnetic resonance indicator for necrotizing fasciitis (MRINEC) algorithm. J. Clin. Med. 2020, 9, E3040. [Google Scholar] [CrossRef]
- Ali, S.Z.; Srinivasan, S.; Peh, W.C.G. MRI in necrotizing fasciitis of the extremities. Br. J. Radiol. 2014, 87, 20130560. [Google Scholar] [CrossRef] [Green Version]
- Weaver, J.S.; Omar, I.M.; Mar, W.A.; Klauser, A.S.; Winegar, B.A.; Mlady, G.W.; McCurdy, W.E.; Taljanovic, M.S. Magnetic resonance imaging of musculoskeletal infections. Pol. J. Radiol. 2022, 87, e141–e162. [Google Scholar] [CrossRef]
- Seok, J.H.; Jee, W.-H.; Chun, K.-A.; Kim, J.-Y.; Jung, C.-K.; Kim, Y.R.; Eo, W.-K.; Kim, Y.-S.; Chung, Y.G. Necrotizing fasciitis versus pyomyositis: Discrimination with using mr imaging. Korean J. Radiol. 2009, 10, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Potini, V.C.; Francisco, R.; Shamian, B.; Tan, V. Sequelae of foreign bodies in the wrist and hand. Hand 2013, 8, 77–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carneiro, B.C.; Cruz, I.A.N.; Chemin, R.N.; Rizzetto, T.A.; Guimarães, J.B.; Silva, F.D.; Junior, C.Y.; Pastore, D.; Ormond Filho, A.G.; Nico, M.A.C. Multimodality imaging of foreign bodies: New insights into old challenges. Radiographics 2020, 40, 1965–1986. [Google Scholar] [CrossRef] [PubMed]
- Jarraya, M.; Hayashi, D.; de Villiers, R.V.; Roemer, F.W.; Murakami, A.M.; Cossi, A.; Guermazi, A. Multimodality imaging of foreign bodies of the musculoskeletal system. AJR Am. J. Roentgenol. 2014, 203, W92–W102. [Google Scholar] [CrossRef] [PubMed]
- Brunner, J.; Russel, M.; Herr, K.; Benjamin, E.; Myers, L.; Boyko, O.; Jaffray, P.; Reddy, S. Nonsuicidal self-injury-related foreign bodies in the emergency department. Semin. Ultrasound CT MR 2015, 36, 80–87. [Google Scholar] [CrossRef]
- Del Cura, J.L.; Aza, I.; Zabala, R.M.; Sarabia, M.; Korta, I. US-guided localization and removal of soft-tissue foreign bodies. Radiographics 2020, 40, 1188–1195. [Google Scholar] [CrossRef]
- Anderson, M.A.; Newmeyer, W.L.; Kilgore, E.S. Diagnosis and treatment of retained foreign bodies in the hand. Am. J. Surg. 1982, 144, 63–67. [Google Scholar] [CrossRef]
- Sheikh, Z.; Brooks, P.J.; Barzilay, O.; Fine, N.; Glogauer, M. Macrophages, foreign body giant cells and their response to implantable biomaterials. Materials 2015, 8, 5671–5701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luttikhuizen, D.T.; Harmsen, M.C.; Van Luyn, M.J.A. Cellular and molecular dynamics in the foreign body reaction. Tissue Eng. 2006, 12, 1955–1970. [Google Scholar] [CrossRef]
- Pagán, A.J.; Ramakrishnan, L. The formation and function of granulomas. Annu. Rev. Immunol. 2018, 36, 639–665. [Google Scholar] [CrossRef]
- Ipaktchi, K.; Demars, A.; Park, J.; Ciarallo, C.; Livermore, M.; Banegas, R. Retained palmar foreign body presenting as a late hand infection: Proposed diagnostic algorithm to detect radiolucent objects. Patient Saf. Surg. 2013, 7, 25. [Google Scholar] [CrossRef]
- Manthey, D.E.; Storrow, A.B.; Milbourn, J.M.; Wagner, B.J. Ultrasound versus radiography in the detection of soft-tissue foreign bodies. Ann. Emerg. Med. 1996, 28, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Boyse, T.D.; Fessell, D.P.; Jacobson, J.A.; Lin, J.; van Holsbeeck, M.T.; Hayes, C.W. US of soft-tissue foreign bodies and associated complications with surgical correlation. Radiographics 2001, 21, 1251–1256. [Google Scholar] [CrossRef]
- Bray, P.W.; Mahoney, J.L.; Campbell, J.P. Sensitivity and specificity of ultrasound in the diagnosis of foreign bodies in the hand. J. Hand Surg. Am. 1995, 20, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Rubin, J.M.; Adler, R.S.; Bude, R.O.; Fowlkes, J.B.; Carson, P.L. Clean and Dirty Shadowing at US: A Reappraisal. Radiology 1991, 181, 231–236. [Google Scholar] [CrossRef]
- Davae, K.C.; Sofka, C.M.; DiCarlo, E.; Adler, R.S. Value of power doppler imaging and the hypoechoic halo in the sonographic detection of foreign bodies: Correlation with histopathologic findings. J. Ultrasound Med. 2003, 22, 1309–1313; quiz 1314–1316. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, J.A.; Powell, A.; Craig, J.G.; Bouffard, J.A.; van Holsbeeck, M.T. Wooden foreign bodies in soft tissue: Detection at US. Radiology 1998, 206, 45–48. [Google Scholar] [CrossRef]
- Tahmasebi, M.; Zareizadeh, H.; Motamedfar, A. Accuracy of ultrasonography in detecting radiolucent soft-tissue foreign bodies. Indian J. Radiol. Imaging 2014, 24, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Aras, M.H.; Miloglu, O.; Barutcugil, C.; Kantarci, M.; Ozcan, E.; Harorli, A. Comparison of the sensitivity for detecting foreign bodies among conventional plain radiography, computed tomography and ultrasonography. Dentomaxillofac. Radiol. 2010, 39, 72–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, J.J.; Bancroft, L.W.; Kransdorf, M.J. Wooden foreign bodies: Imaging appearance. AJR Am. J. Roentgenol. 2002, 178, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Ruder, T.D.; Thali, Y.; Bolliger, S.A.; Somaini-Mathier, S.; Thali, M.J.; Hatch, G.M.; Schindera, S.T. Material differentiation in forensic radiology with single-source dual-energy computed tomography. Forensic Sci. Med. Pathol. 2013, 9, 163–169. [Google Scholar] [CrossRef]
- Ingraham, C.R.; Mannelli, L.; Robinson, J.D.; Linnau, K.F. Radiology of foreign bodies: How do we image them? Emerg. Radiol. 2015, 22, 425–430. [Google Scholar] [CrossRef]
- Eidelman, M.; Bialik, V.; Miller, Y.; Kassis, I. Plantar puncture wounds in children: Analysis of 80 hospitalized patients and late sequelae. Isr. Med. Assoc. J. 2003, 5, 268–271. [Google Scholar] [PubMed]
- Johnson, P.W.; Collins, M.S.; Wenger, D.E. Diagnostic utility of t1-weighted mri characteristics in evaluation of osteomyelitis of the foot. AJR Am. J. Roentgenol. 2009, 192, 96–100. [Google Scholar] [CrossRef]
- Alaia, E.F.; Chhabra, A.; Simpfendorfer, C.S.; Cohen, M.; Mintz, D.N.; Vossen, J.A.; Zoga, A.C.; Fritz, J.; Spritzer, C.E.; Armstrong, D.G.; et al. MRI nomenclature for musculoskeletal infection. Skelet. Radiol. 2021, 50, 2319–2347. [Google Scholar] [CrossRef]
- Paydar, K.Z.; Hansen, S.L.; Charlebois, E.D.; Harris, H.W.; Young, D.M. Inappropriate antibiotic use in soft tissue infections. Arch. Surg. 2006, 141, 850–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frazee, B.W.; Lynn, J.; Charlebois, E.D.; Lambert, L.; Lowery, D.; Perdreau-Remington, F. High prevalence of methicillin-resistant staphylococcus aureus in emergency department skin and soft tissue infections. Ann. Emerg. Med. 2005, 45, 311–320. [Google Scholar] [CrossRef]
- Struk, D.W.; Munk, P.L.; Lee, M.J.; Ho, S.G.; Worsley, D.F. Imaging of soft tissue infections. Radiol. Clin. N. Am. 2001, 39, 277–303. [Google Scholar] [CrossRef] [PubMed]
- Bureau, N.J.; Chhem, R.K.; Cardinal, E. Musculoskeletal infections: US manifestations. Radiographics 1999, 19, 1585–1592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craig, J.G. Infection: Ultrasound-guided procedures. Radiol. Clin. N. Am. 1999, 37, 669–678. [Google Scholar] [CrossRef]
- Loyer, E.M.; Kaur, H.; David, C.L.; DuBrow, R.; Eftekhari, F.M. Importance of dynamic assessment of the soft tissues in the sonographic diagnosis of echogenic superficial abscesses. J. Ultrasound Med. 1995, 14, 669–671. [Google Scholar] [CrossRef] [PubMed]
- Fayad, L.M.; Carrino, J.A.; Fishman, E.K. Musculoskeletal infection: Role Of CT In the emergency department. Radiographics 2007, 27, 1723–1736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, L.D.; Frassica, F.J.; Bluemke, D.A.; Fishman, E.K. CT and MRI evaluation of musculoskeletal infection. Crit. Rev. Diagn. Imaging 1997, 38, 535–568. [Google Scholar]
- Chandnani, V.P.; Beltran, J.; Morris, C.S.; Khalil, S.N.; Mueller, C.F.; Burk, J.M.; Bennett, W.F.; Shaffer, P.B.; Vasila, M.S.; Reese, J. Acute experimental osteomyelitis and abscesses: Detection with MR IMAGING versus CT. Radiology 1990, 174, 233–236. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, B.; Wilson, N.; Doyle, A.J. The “penumbra sign” on t1-weighted MRI for differentiating musculoskeletal infection from tumour. Skelet. Radiol. 2007, 36, 417–421. [Google Scholar] [CrossRef]
- Chun, C.W.; Jung, J.-Y.; Baik, J.S.; Jee, W.-H.; Kim, S.K.; Shin, S.H. Detection of soft-tissue abscess: Comparison of diffusion-weighted imaging to contrast-enhanced MRI. J. Magn. Reason. Imaging 2018, 47, 60–68. [Google Scholar] [CrossRef]
- Kumar, Y.; Wadhwa, V.; Phillips, L.; Pezeshk, P.; Chhabra, A. MR imaging of skeletal muscle signal alterations: Systematic approach to evaluation. Eur. J. Radiol. 2016, 85, 922–935. [Google Scholar] [CrossRef]
- Harish, S.; Chiavaras, M.M.; Kotnis, N.; Rebello, R. MR imaging of skeletal soft tissue infection: Utility of diffusion-weighted imaging in detecting abscess formation. Skelet. Radiol. 2011, 40, 285–294. [Google Scholar] [CrossRef]
- Merkle, E.M.; Kramme, E.; Vogel, J.; Krämer, S.; Schulte, M.; Usadel, S.; Kern, P.; Brambs, H.J. Bone and soft tissue manifestations of alveolar echinococcosis. Skelet. Radiol. 1997, 26, 289–292. [Google Scholar] [CrossRef]
- Heo, S.H.; Shin, S.S.; Kim, J.W.; Lim, H.S.; Seon, H.J.; Jung, S.-I.; Jeong, Y.Y.; Kang, H.K. Imaging of actinomycosis in various organs: A comprehensive review. Radiographics 2014, 34, 19–33. [Google Scholar] [CrossRef]
- Nash, S.; Rubenstein, J.; Chaiton, A.; Morava-Protzner, I. Adenocarcinoma of the lung metastatic to the psoas muscle. Skelet. Radiol. 1996, 25, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Dion, E.; Forest, M.; Brasseur, J.L.; Amoura, Z.; Grenier, P. Epithelioid sarcoma mimicking abscess: Review of the MRI appearances. Skelet. Radiol. 2001, 30, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-H.; Chen, C.K.-H.; Yeh, L.-R.; Pan, H.-B.; Yang, C.-F. Intra-abdominal gout mimicking pelvic abscess. Skelet. Radiol. 2005, 34, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Bickels, J.; Ben-Sira, L.; Kessler, A.; Wientroub, S. Primary pyomyositis. J. Bone Joint. Surg. Am. 2002, 84, 2277–2286. [Google Scholar] [CrossRef]
- Gubbay, A.J.; Isaacs, D. Pyomyositis in children. Pediatr. Infect. Dis. J. 2000, 19, 1009–1012; quiz 1013. [Google Scholar] [CrossRef] [Green Version]
- Thammaroj, P.; Panitchote, A.; Muktabhant, C.; Chowchuen, P. Discrimination between tuberculous and bacterial pyomyositis in magnetic resonance features. Eur. J. Radiol. Open 2020, 7, 100214. [Google Scholar] [CrossRef]
- Dhanoa, A.; Singh, V.A.; Mansor, A.; Yusof, M.Y.; Lim, K.-T.; Thong, K.-L. Acute haematogenous community-acquired methicillin-resistant staphylococcus aureus osteomyelitis in an adult: Case report and review of literature. BMC Infect. Dis. 2012, 12, 270. [Google Scholar] [CrossRef] [Green Version]
- DeLeo, F.R.; Otto, M.; Kreiswirth, B.N.; Chambers, H.F. Community-associated meticillin-resistant staphylococcus aureus. Lancet 2010, 375, 1557–1568. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, R.J.; Strouse, P.J.; Craig, C.L.; Farley, F.A. Focal pyomyositis of the perisciatic muscles in children. AJR Am. J. Roentgenol. 2002, 179, 1267–1271. [Google Scholar] [CrossRef]
- Gonzalez Moran, G.; Garcia Duran, C.; Albiñana, J. Imaging on pelvic pyomyositis in children related to pathogenesis. J. Child. Orthop. 2009, 3, 479–484. [Google Scholar] [CrossRef] [Green Version]
- Bartoloni, A.; Aparisi Gómez, M.P.; Cirillo, M.; Allen, G.; Battista, G.; Guglielmi, G.; Tomà, P.; Bazzocchi, A. Imaging of the limping child. Eur. J. Radiol. 2018, 109, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.; Kötter, I.; Ernemann, U.; Fenchel, M.; Tzaribatchev, N.; Claussen, C.D.; Horger, M. MRI findings in inflammatory muscle diseases and their noninflammatory mimics. AJR Am. J. Roentgenol. 2009, 192, 1708–1716. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Khaleel, M.; Boothe, E.; Awdeh, H.; Wadhwa, V.; Chhabra, A. Role of diffusion weighted imaging in musculoskeletal infections: Current perspectives. Eur. Radiol. 2017, 27, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, P.L.; Way, A.; Baig, S.; Gopireddy, D.R. MRI of myositis and other urgent muscle-related disorders. Emerg. Radiol. 2021, 28, 409–421. [Google Scholar] [CrossRef] [PubMed]
- Spinnato, P.; Chiesa, A.M.; Ledoux, P.; Kind, M.; Bianchi, G.; Tuzzato, G.; Righi, A.; Crombé, A. Primary soft-tissue lymphomas: Mri features help discriminate from other soft-tissue tumors. Acad. Radiol. 2022; in press. [Google Scholar] [CrossRef]
- Pollen, A.G. Acute infection of the tendon sheaths. Hand. 1974, 6, 21–25. [Google Scholar] [CrossRef]
- Spann, M.; Talmor, M.; Nolan, W.B. Hand infections: Basic principles and management. Surg. Infect. 2004, 5, 210–220. [Google Scholar] [CrossRef]
- Krieger, L.E.; Schnall, S.B.; Holtom, P.D.; Costigan, W. Acute gonococcal flexor tenosynovitis. Orthopedics 1997, 20, 649–650. [Google Scholar] [CrossRef]
- Jeffrey, R.B., Jr.; Laing, F.C.; Schechter, W.P.; Markison, R.E.; Barton, R.M. Acute suppurative tenosynovitis of the hand: Diagnosis with US. Radiol 1987, 162, 741–742. [Google Scholar] [CrossRef]
- Gómez-Rodríguez, N.; Méndez-García, M.J.; Ferreiro-Seoane, J.L.; Ibáñez-Ruán, J.; Penelas-Cortés Bellas, Y. Infectious bursitis: Study of 40 cases in the pre-patellar and olecranon regions. Enferm. Infecc. Microbiol. Clin. 1997, 15, 237–242. [Google Scholar]
- Sambri, A.; Spinnato, P.; Tedeschi, S.; Zamparini, E.; Fiore, M.; Zucchini, R.; Giannini, C.; Caldari, E.; Crombé, A.; Viale, P.; et al. Bone and joint infections: The role of imaging in tailoring diagnosis to improve patients’ care. J. Pers. Med. 2021, 11, 1317. [Google Scholar] [CrossRef]
- Naselli, N.; Facchini, G.; Lima, G.M.; Evangelisti, G.; Ponti, F.; Miceli, M.; Spinnato, P. MRI in differential diagnosis between tuberculous and pyogenic spondylodiscitis. Eur. Spine J. 2022, 31, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Li, H.; Jin, C.; Niu, G.; Guo, B.; Chen, Y.; Yang, J. Differentiation between brucellar and tuberculous spondylodiscitis in the acute and subacute stages by MRI: A retrospective observational study. Acad Radiol. 2018, 25, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Muraoka, H.; Ito, K.; Hirahara, N.; Ichiki, S.; Kondo, T.; Kaneda, T. Magnetic resonance imaging texture analysis in the quantitative evaluation of acute osteomyelitis of the mandibular bone. Dentomaxillofac Radiol. 2022, 51, 20210321. [Google Scholar] [CrossRef] [PubMed]
- Boesen, M.; Kubassova, O.; Sudoł-Szopińska, I.; Maas, M.; Hansen, P.; Nybing, J.D.; Oei, E.H.; Hemke, R.; Guermazi, A. MR imaging of joint infection and inflammation with emphasis on dynamic contrast-enhanced mr imaging. PET Clin. 2018, 13, 523–550. [Google Scholar] [CrossRef] [PubMed]







| Modality | Key Findings |
|---|---|
| Plain radiographs | • Soft tissue edema • Gas tracking along fascial planes |
| US | • Increased echogenicity and thickening of subcutaneous soft tissue • Fluid tracking along the fascia • Gas seen as echogenic foci with dirty posterior acoustic shadowing |
| CT | • Increased signal and stranding of fat (similar to cellulitis) • Deep fascial thickening and fluid along deep and intermuscular fascia • Fluid extending along intermuscular fascial planes • Lack of enhancement of fascia after intravenous contrast • Gas in soft tissue along fascial planes |
| MRI | • Thickening of deep fascia ≥ 3 mm • Fluid extending deep along intermuscular fascial planes • Involvement of more than 3 compartments • Variable enhancement with areas of fascial enhancement (inflammation) and lack thereof (necrosis) • Gas seen as foci of signal void on all sequences • May be band like edema/enhancement in periphery of muscles |
| 1 | Localize foreign body with high frequency linear-array transducer. |
| 2 | Perform color/power Doppler evaluation to visualize adjacent vessels and identify other critical structures at risk for injury (e.g., nerves). |
| 3 | Identify the ideal path to the foreign body and mark the skin surface accordingly. |
| 4 | Sterilely prep and drape the skin surface and place sterile cover on ultrasound probe. |
| 5 | Under ultrasound-guidance, administer 1% lidocaine to skin surface with a 25G needle along the path to the foreign body (using a 22G spinal needle if necessary). |
| 6 | Make a dermatotomy with an 11-blade scalpel. |
| 7 | Insert sterile forceps and use ultrasound to guide to the foreign body. |
| 8 | Grasp the foreign body with the forceps under ultrasound guidance. |
| 9 | Remove the foreign body through the dermatotomy site. |
| 10 | Use ultrasound to evaluate the soft tissues for additional foreign bodies or debris. |
| 11 | Clean the skin surface; a small dermatotomy may be allowed to heal by secondary intention; larger incisions can be closed with topical adhesives or adhesive strips. |
| Foreign Body | Notes | CR | CT | US | MRI |
|---|---|---|---|---|---|
| Glass | 9–24% of FBs 15% of glass injuries have retained FB | Radiopaque Nearly 100% detectable when >2 mm in size | 500–1900 HU | Hyperechoic with posterior reverberation | Low T1 and T2; polygonal with angled margins |
| Metal | Common with gun-related injuries | Radiopaque | >3000 HU | Hyperechoic with posterior reverberation | Magnetic susceptibility artifact |
| Wood | 36% of FBs in hand injuries Only 25% of patients note penetrating injury | Radiolucent | 50–80 HU | Hyperechoic with posterior acoustic shadow; possible reverberation related to gas content | Low T1 and T2; surrounding inflammatory change and enhancement |
| Plastic | Uncommon as plastic rarely shatters | Radiolucent | 10–20 HU | Hyperechoic with posterior reverberation | Low T1 and T2; only detects 50%; no FB reaction |
| Stones | e.g., asphalt or gravel after fall | Radiopaque | >1500 HU | Hyperechoic with posterior acoustic shadow | Low T1 and T2 |
| Calcified Biologics | e.g., sea urchin spine, bones, and teeth | Radiopaque | 300–1900 but decreases as resorbs over time | Thin, linear, and hyperechoic | Low T1 and T2 |
| Non-calcified biologics | e.g., larvae; up to 9% of dermatosis in tropics | Radiolucent | Wide (lung) windows to ID respiratory tract | Echogenic; may have movement in case of larvae | Soft-tissue inflammatory mass |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spinnato, P.; Patel, D.B.; Di Carlo, M.; Bartoloni, A.; Cevolani, L.; Matcuk, G.R.; Crombé, A. Imaging of Musculoskeletal Soft-Tissue Infections in Clinical Practice: A Comprehensive Updated Review. Microorganisms 2022, 10, 2329. https://doi.org/10.3390/microorganisms10122329
Spinnato P, Patel DB, Di Carlo M, Bartoloni A, Cevolani L, Matcuk GR, Crombé A. Imaging of Musculoskeletal Soft-Tissue Infections in Clinical Practice: A Comprehensive Updated Review. Microorganisms. 2022; 10(12):2329. https://doi.org/10.3390/microorganisms10122329
Chicago/Turabian StyleSpinnato, Paolo, Dakshesh B. Patel, Maddalena Di Carlo, Alessandra Bartoloni, Luca Cevolani, George R. Matcuk, and Amandine Crombé. 2022. "Imaging of Musculoskeletal Soft-Tissue Infections in Clinical Practice: A Comprehensive Updated Review" Microorganisms 10, no. 12: 2329. https://doi.org/10.3390/microorganisms10122329





