Outbreak of MRSA in a Gynecology/Obstetrics Department during the COVID-19 Pandemic: A Cautionary Tale
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical Setting and Infection Control Measures
2.2. MRSA Culturing and Typing of Screening Samples
2.3. Environmental Sampling and Testing Method
2.4. Whole Genome Sequencing-Based Typing
2.5. Ethics Statement
3. Results
3.1. Outbreak Management
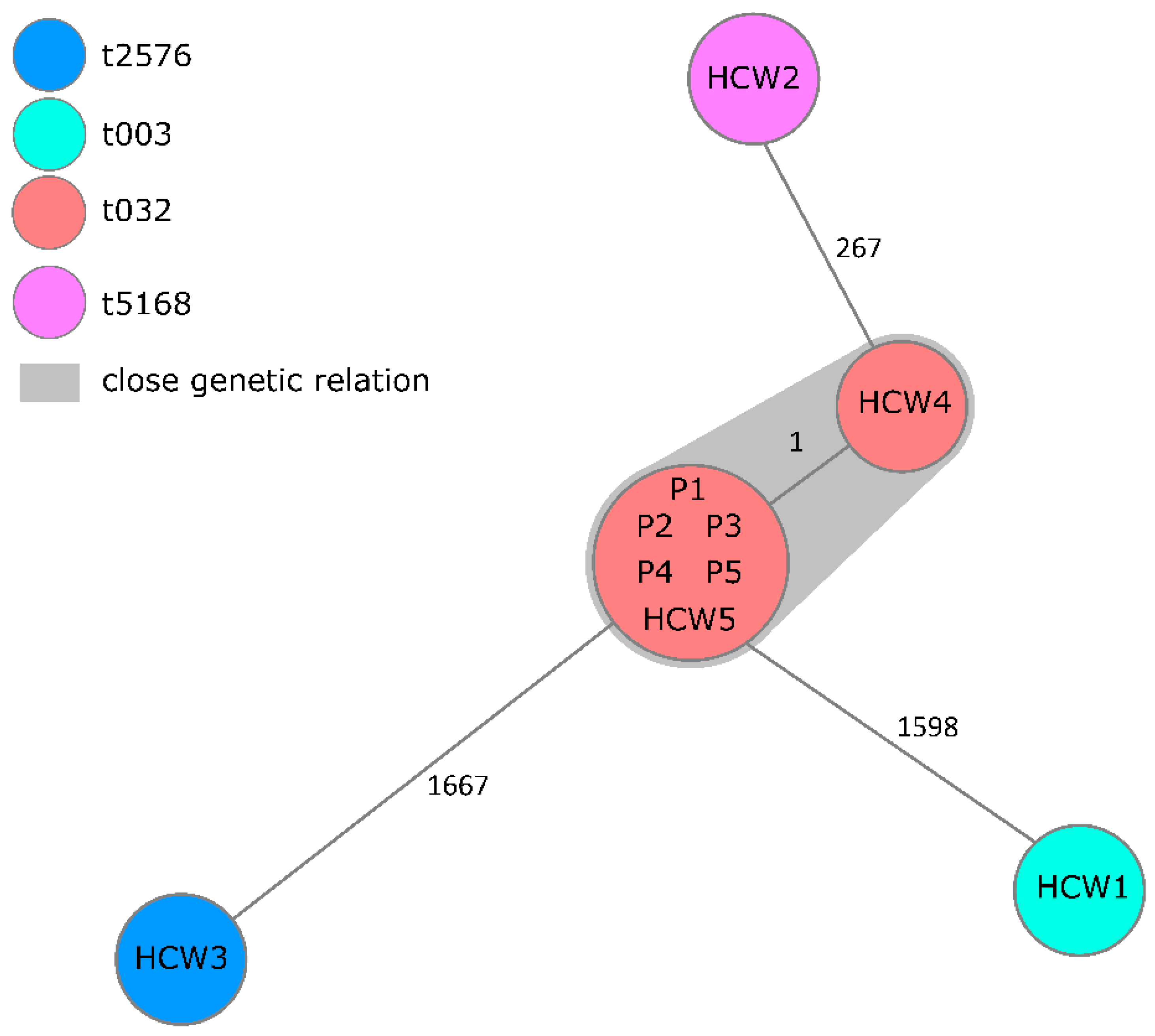
3.2. Whole Genome Sequencing-Based Typing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Acker, K.; Eagen-Torkko, M.; Riley, L.E.; Saiman, L. COVID-19 Infection, Prevention, and Control Considerations in the Obstetric Environment. Clin. Obstet. Gynecol. 2022, 65, 134–147. [Google Scholar] [CrossRef]
- Cole, J.; Barnard, E. The impact of the COVID-19 pandemic on healthcare acquired infections with multidrug resistant organisms. Am. J. Infect. Control 2021, 49, 653–654. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.C.; Chen, S.Y.; Ko, W.C.; Hsueh, P.R. Increased antimicrobial resistance during the COVID-19 pandemic. Int. J. Antimicrob. Agents 2021, 57, 106324. [Google Scholar] [CrossRef] [PubMed]
- Polly, M.; de Almeida, B.L.; Lennon, R.P.; Cortes, M.F.; Costa, S.F.; Guimaraes, T. Impact of the COVID-19 pandemic on the incidence of multidrug-resistant bacterial infections in an acute care hospital in Brazil. Am. J. Infect. Control 2022, 50, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Kampmeier, S.; Tonnies, H.; Correa-Martinez, C.L.; Mellmann, A.; Schwierzeck, V. A nosocomial cluster of vancomycin resistant enterococci among COVID-19 patients in an intensive care unit. Antimicrob. Resist. Infect. Control 2020, 9, 154. [Google Scholar] [CrossRef] [PubMed]
- Porretta, A.D.; Baggiani, A.; Arzilli, G.; Casigliani, V.; Mariotti, T.; Mariottini, F.; Scardina, G.; Sironi, D.; Totaro, M.; Barnini, S.; et al. Increased Risk of Acquisition of New Delhi Metallo-Beta-Lactamase-Producing Carbapenem-Resistant Enterobacterales (NDM-CRE) among a Cohort of COVID-19 Patients in a Teaching Hospital in Tuscany, Italy. Pathogens 2020, 9, 635. [Google Scholar] [CrossRef] [PubMed]
- Gastmeier, P.; Schwab, F.; Behnke, M.; Geffers, C. Decreasing healthcare-associated infections (HAI) is an efficient method to decrease healthcare-associated Methicillin-resistant S. aureus (MRSA) infections Antimicrobial resistance data from the German national nosocomial surveillance system KISS. Antimicrob. Resist. Infect. Control 2012, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, J.S. Methicillin-resistant Staphylococcus aureus in obstetrics. Am. J. Perinatol. 2013, 30, 125–130. [Google Scholar] [CrossRef]
- Robert-Koch Institute. Empfehlungen zur Prävention und Kontrolle von Methicillin-resistenten Staphylococcus aureus-Stämmen (MRSA) in medizinischen und pflegerischen Einrichtungen. Bundesgesundheitsbl 2014, 57, 696–732. [Google Scholar]
- Souvorov, A.; Agarwala, R.; Lipman, D.J. SKESA: Strategic k-mer extension for scrupulous assemblies. Genome Biol. 2018, 19, 153. [Google Scholar] [CrossRef]
- Mellmann, A.; Bletz, S.; Boking, T.; Kipp, F.; Becker, K.; Schultes, A.; Prior, K.; Harmsen, D. Real-time genome sequencing of resistant bacteria provides precision infection control in an institutional setting. J. Clin. Microbiol. 2016, 54, 2874–2881. [Google Scholar] [CrossRef] [PubMed]
- Leopold, S.R.; Goering, R.V.; Witten, A.; Harmsen, D.; Mellmann, A. Bacterial Whole-Genome Sequencing Revisited: Portable, Scalable, and Standardized Analysis for Typing and Detection of Virulence and Antibiotic Resistance Genes. J. Clin. Microbiol. 2014, 52, 2365–2370. [Google Scholar] [CrossRef] [PubMed]
- Lacey, S.; Flaxman, D.; Scales, J.; Wilson, A. The usefulness of masks in preventing transient carriage of epidemic methicillin-resistant Staphylococcus aureus by healthcare workers. J. Hosp. Infect. 2001, 48, 308–311. [Google Scholar] [CrossRef] [PubMed]
- Thoma, R.; Seneghini, M.; Seiffert, S.N.; Gysin, D.V.; Scanferla, G.; Haller, S.; Flury, D.; Boggian, K.; Kleger, G.-R.; Filipovic, M.; et al. The challenge of preventing and containing outbreaks of multidrug-resistant organisms and Candida auris during the coronavirus disease 2019 pandemic: Report of a carbapenem-resistant Acinetobacter baumannii outbreak and a systematic review of the literature. Antimicrob. Resist. Infect. Control 2022, 11, 12. [Google Scholar]
- Yap, F.H.; Gomersall, C.D.; Fung, K.S.; Ho, P.L.; Ho, O.M.; Lam, P.K.; Lam, D.T.; Lyon, D.J.; Joynt, G.M. Increase in methicillin-resistant Staphylococcus aureus acquisition rate and change in pathogen pattern associated with an outbreak of severe acute respiratory syndrome. Clin. Infect. Dis. 2004, 39, 511–516. [Google Scholar] [CrossRef]
- Patel, A.; Emerick, M.; Cabunoc, M.K.; Williams, M.H.; Preas, M.A.; Schrank, G.; Rabinowitz, R.; Luethy, P.; Johnson, J.K.; Leekha, S. Rapid Spread and Control of Multidrug-Resistant Gram-Negative Bacteria in COVID-19 Patient Care Units. Emerg. Infect. Dis. 2021, 27, 1234–1237. [Google Scholar] [CrossRef]
- Neely, A.N.; Maley, M.P. Survival of enterococci and staphylococci on hospital fabrics and plastic. J. Clin. Microbiol. 2000, 38, 724–726. [Google Scholar] [CrossRef]
- Wagenvoort, J.H.T.; De Brauwer, E.I.G.B.; Penders, R.J.R.; van der Linden, C.J.; Willems, R.J.; Top, J.; Bonten, M.J. Environmental survival of vancomycin-sensitive ampicillin-resistant Enterococcus faecium (AREfm). Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 1901–1903. [Google Scholar] [CrossRef][Green Version]
- Wee, L.E.I.; Conceicao, E.P.; Tan, J.Y.; Magesparan, K.D.; Amin, I.B.M.; Ismail, B.B.S.; Toh, H.X.; Jin, P.; Zhang, J.; Wee, E.G.L.; et al. Unintended consequences of infection prevention and control measures during COVID-19 pandemic. Am. J. Infect. Control 2021, 49, 469–477. [Google Scholar] [CrossRef]
- Bentivegna, E.; Luciani, M.; Arcari, L.; Santino, I.; Simmaco, M.; Martelletti, P. Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 1003. [Google Scholar] [CrossRef]
- Hirabayashi, A.; Kajihara, T.; Yahara, K.; Shibayama, K.; Sugai, M. Impact of the COVID-19 pandemic on the surveillance of antimicrobial resistance. J. Hosp. Infect. 2021, 117, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, A.; Schranz, M.; Rexroth, U.; Hamouda, O.; Schaade, L.; Diercke, M.; Boender, T.S.; Robert Koch’s Infectious Disease Surveillance, G. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: An analysis of national surveillance data during 1–2016–week 32–2020. Lancet Reg. Health Eur. 2021, 6, 100103. [Google Scholar] [CrossRef] [PubMed]
| Patient No. | Surgical Intervention | MRSA Screening Date and Result | Clinical MRSA Sample | Sampling Date | Hospital- Acquired |
|---|---|---|---|---|---|
| P1 | Curettage | 12 June 2020 negative | Vaginal swab sampling | 27 June 2020 | Yes |
| P2 | Hysterectomy | 26 May 2020 Negative | Drain fluid | 29June 2020 | Yes |
| P3 | Plastic surgery of the breast | 6 July 2020 Negative | Pus from breast tissue | 13 July 2020 | Yes |
| P4 | Cesarean section | 8 June 2020 negative | Surgical wound swab | 6 August 2020 | Yes |
| P5 | Laparotomy | 16 May 2020 negative | Swab sampling of the port puncture site | 21 September 2020 | Yes |
| No. | P | OX | AMX/CA | CEZ | LEV | CLI | VAN | TEI | TMP/SMX | RIF | FOS | LIN | DAP | MUP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | R | R | R | R | R | R | S | S | S | R | R | S | R | I |
| P2 | R | R | R | R | R | R | S | S | S | S | S | S | S | S |
| P3 | R | R | R | R | R | R | S | S | S | S | S | S | S | S |
| P4 | R | R | R | R | R | R | S | S | S | S | S | S | S | S |
| P5 | R | R | R | R | R | R | S | S | S | S | S | S | S | I |
| Sampling Site | Detected Microorganisms |
|---|---|
| Preparation room, work space | Bacillus spp., CNS |
| Preparation room, storage | Bacillus spp., CNS |
| Preparation room, storage | Bacillus spp. |
| Preparation room, storage | Bacillus spp. |
| Preparation room, storage | Bacillus spp., CNS |
| Operation room, PC keyboard | Bacillus spp., S. aureus |
| Operation room, PC keyboard | Bacillus spp., CNS |
| Operation room, perfusor | Bacillus spp., S. aureus |
| Operation room, PC monitor | Bacillus spp., CNS |
| Operation room, supply trolley | Bacillus spp. |
| Operation room, infusion stand | Bacillus spp., CNS |
| Operation room, instruments table | Bacillus spp., CNS |
| Operation room, suture storage | S. aureus, viridans streptococci |
| Operation room, leg support | Bacillus spp., CNS |
| Operation room, remote control | Bacillus spp., S. aureus |
| Operation room, disinfection bottle | Bacillus spp., CNS |
| Operation room, disposable gloves | Bacillus spp. |
| Operation room, disinfection bottle | Bacillus spp., CNS |
| Sterile goods storage, shelves | Bacillus spp., CNS |
| Sterile goods storage, shelves | Bacillus spp., CNS |
| Sterile goods storage, shelves | Bacillus spp., CNS |
| Sterile goods storage, operation set | Bacillus spp., CNS |
| Sterile goods storage, operation set | Bacillus spp., CNS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Möllers, M.; von Wahlde, M.-K.; Schuler, F.; Mellmann, A.; Böing, C.; Schwierzeck, V.; Schneider, J.S.; Kampmeier, S. Outbreak of MRSA in a Gynecology/Obstetrics Department during the COVID-19 Pandemic: A Cautionary Tale. Microorganisms 2022, 10, 689. https://doi.org/10.3390/microorganisms10040689
Möllers M, von Wahlde M-K, Schuler F, Mellmann A, Böing C, Schwierzeck V, Schneider JS, Kampmeier S. Outbreak of MRSA in a Gynecology/Obstetrics Department during the COVID-19 Pandemic: A Cautionary Tale. Microorganisms. 2022; 10(4):689. https://doi.org/10.3390/microorganisms10040689
Chicago/Turabian StyleMöllers, Mareike, Marie-Kristin von Wahlde, Franziska Schuler, Alexander Mellmann, Christian Böing, Vera Schwierzeck, Julia Sophie Schneider, and Stefanie Kampmeier. 2022. "Outbreak of MRSA in a Gynecology/Obstetrics Department during the COVID-19 Pandemic: A Cautionary Tale" Microorganisms 10, no. 4: 689. https://doi.org/10.3390/microorganisms10040689
APA StyleMöllers, M., von Wahlde, M.-K., Schuler, F., Mellmann, A., Böing, C., Schwierzeck, V., Schneider, J. S., & Kampmeier, S. (2022). Outbreak of MRSA in a Gynecology/Obstetrics Department during the COVID-19 Pandemic: A Cautionary Tale. Microorganisms, 10(4), 689. https://doi.org/10.3390/microorganisms10040689






