Antimicrobial Activity of Ligilactobacillus animalis SWLA-1 and Its Cell-Free Supernatant against Multidrug-Resistant Bacteria and Its Potential Use as an Alternative to Antimicrobial Agents
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Bacterial Strains
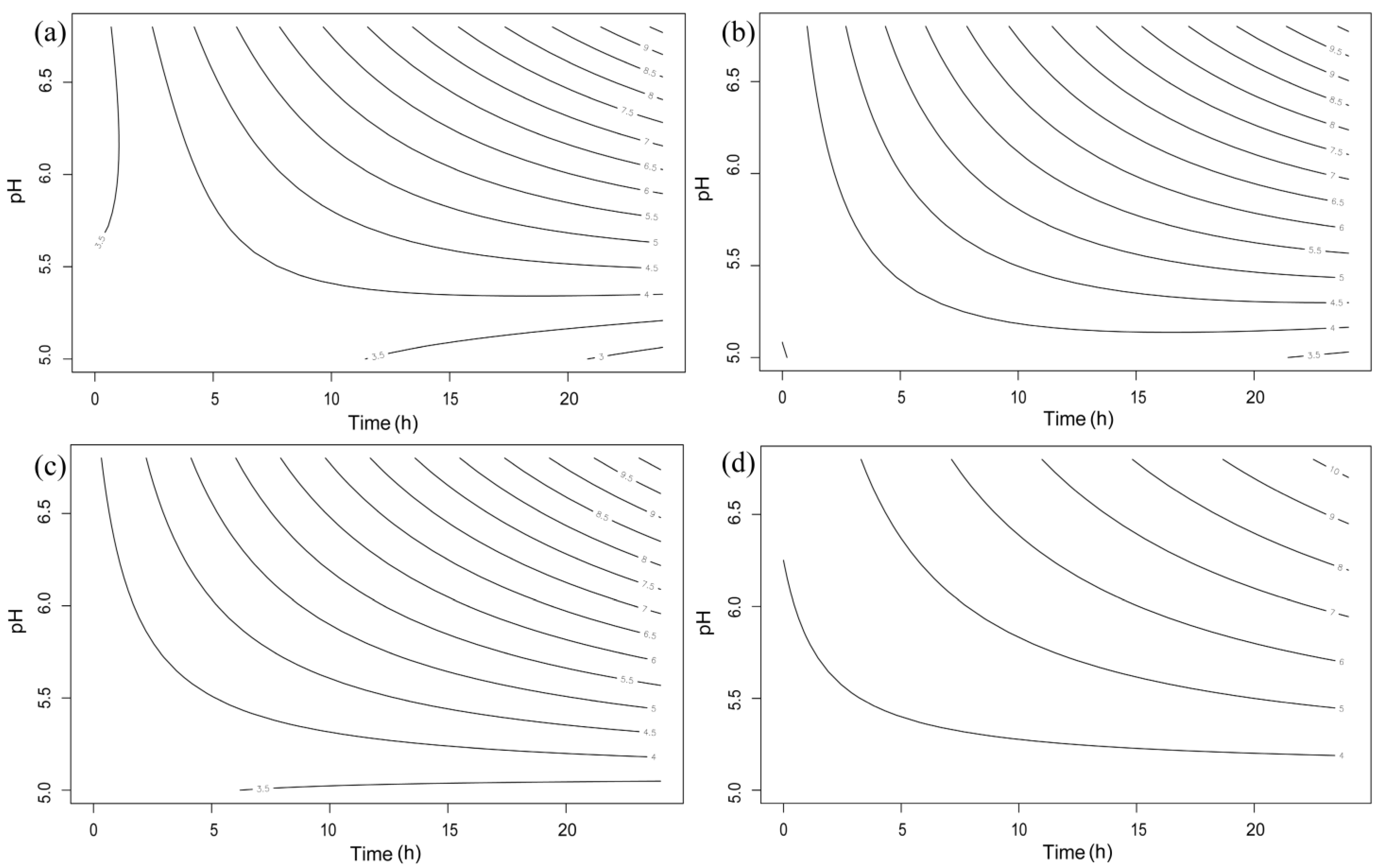
2.2. Effect of pH on Indicator Bacteria
2.3. Comparison of Antimicrobial Activity of L. animalis SWLA-1 with That of Other Lactobacilli
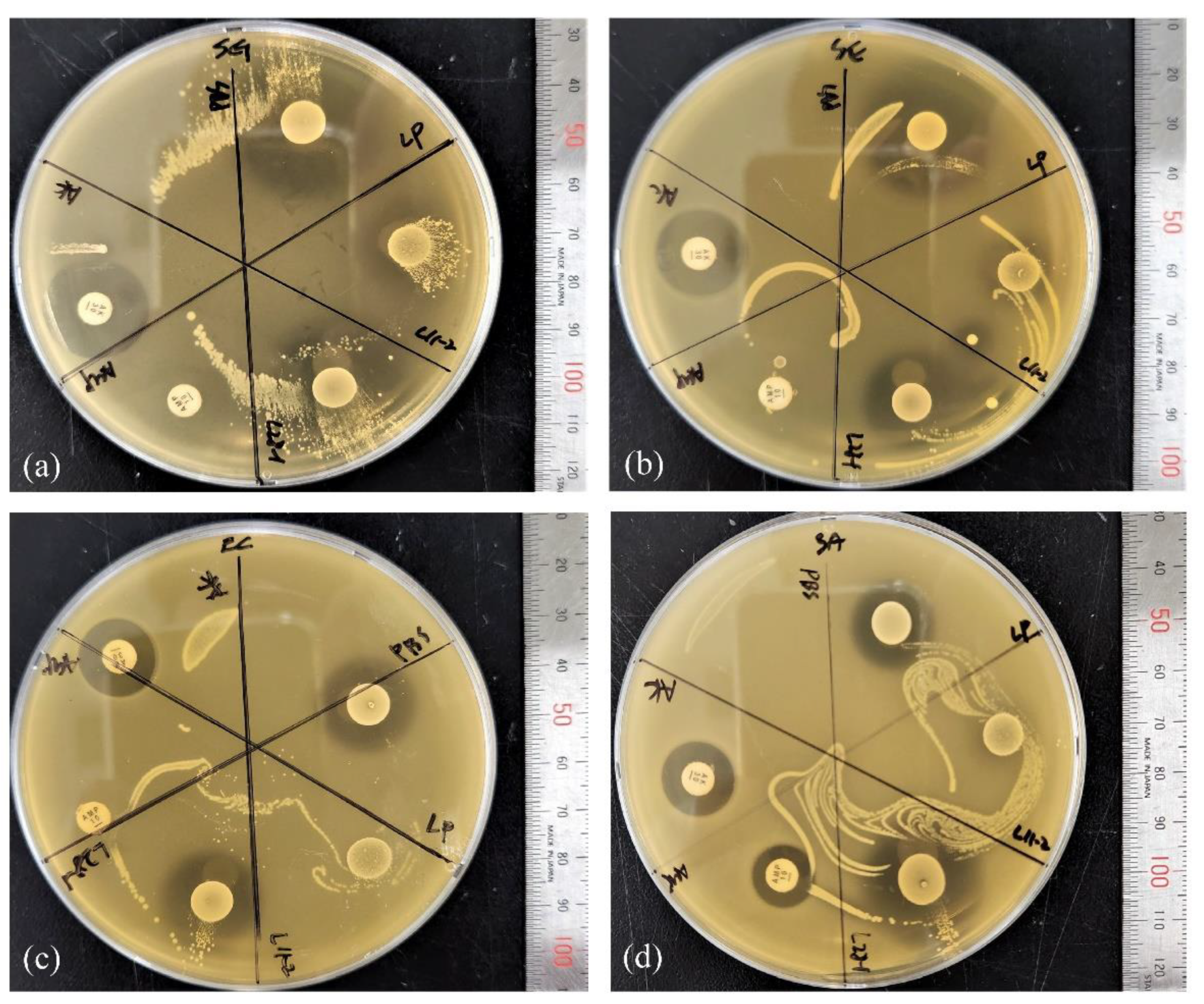
2.3.1. Comparative Agar Spot Assay
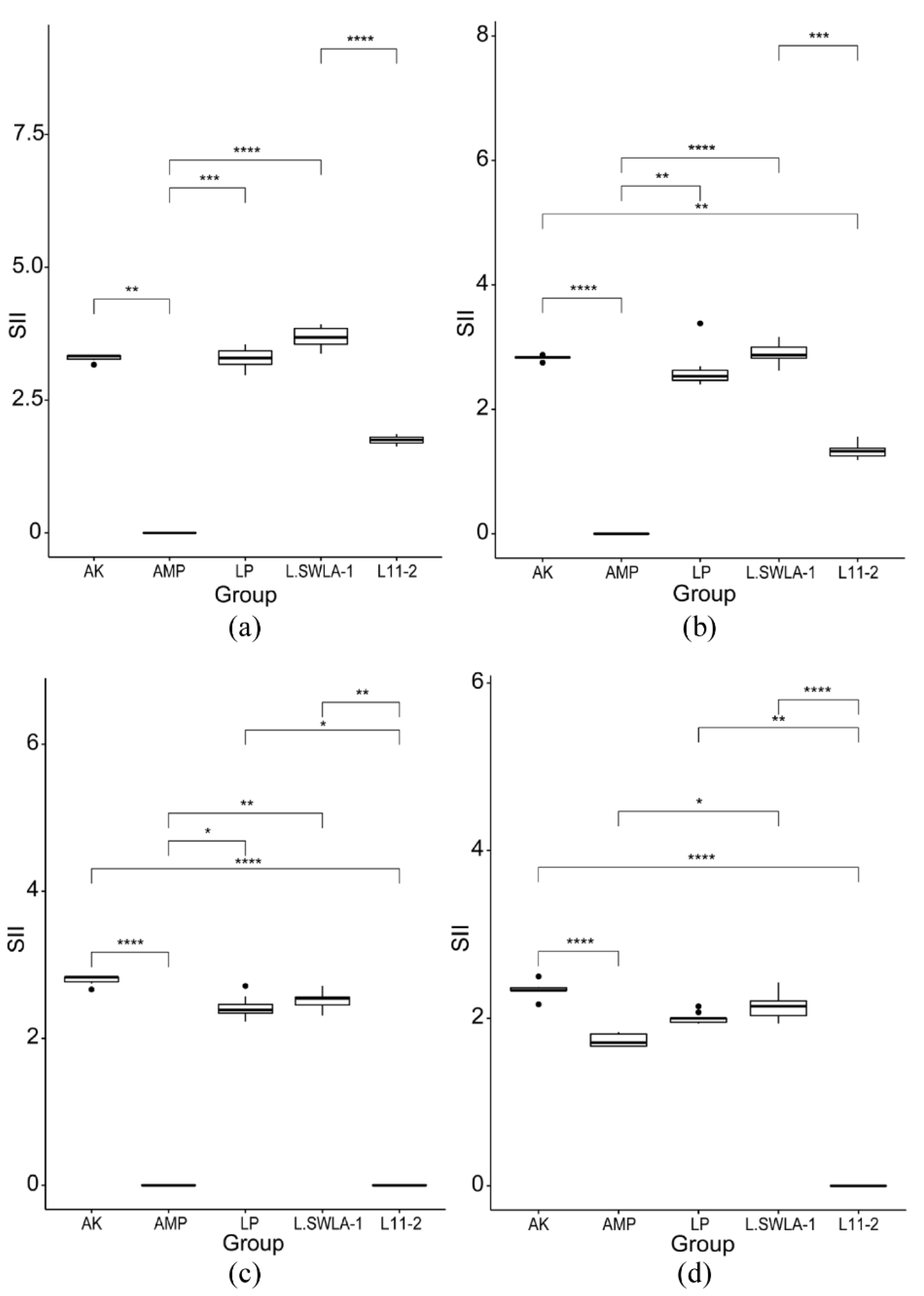
2.3.2. Comparative Coculture Assay
2.4. Antimicrobial Activity of Supernatant Derived from L. animalis SWLA-1
2.4.1. Preparation of Cell-Free Supernatant
2.4.2. Various Treatments and Effects on Antimicrobial Activity of CFS
2.5. Statistical Analysis
3. Results
3.1. Effect of pH on Indicator Bacteria
3.2. Comparative Agar Spot Assay
3.3. Comparative Coculture Assay
3.4. Effects of Various Treatments on CFS Antimicrobial Activity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Narvhus, J.A.; Axelsson, L. lactic Acid Bacteria. In Encyclopedia of Food Sciences and Nutrition; Academic Press: Cambridge, MA, USA, 2003; pp. 3465–3472. [Google Scholar]
- Schumacher, A.E.; Heuser, G.F. Isolation of an Organism Responsible for the Increased Riboflavin Content of the Feces of the Fowl. Poult. Sci. 1941, 20, 272–277. [Google Scholar] [CrossRef]
- Brown, E.W.; Bosworth, A.W. Studies of Infant Feeding Xvi: A Bacteriologic Study of the Feces and the Food of Normal Babies Receiving Breast Milk. Am. J. Dis. Child. 1922, 23, 243–258. [Google Scholar] [CrossRef]
- Patten, D.A.; Laws, A.P. Lactobacillus-produced exopolysaccharides and their potential health benefits: A review. Benef. Microbes 2015, 6, 457–471. [Google Scholar] [CrossRef] [PubMed]
- Crovesy, L.; Ostrowski, M.; Ferreira, D.M.T.P.; Rosado, E.L.; Soares, M. Effect of Lactobacillus on body weight and body fat in overweight subjects: A systematic review of randomized controlled clinical trials. Int. J. Obes. 2017, 41, 1607–1614. [Google Scholar] [CrossRef] [PubMed]
- Dowarah, R.; Verma, A.K.; Agarwal, N. The use of Lactobacillus as an alternative of antibiotic growth promoters in pigs: A review. Anim. Nutr. 2017, 3, 1–6. [Google Scholar] [CrossRef]
- Chassaing, B.; Cascales, E. Antibacterial Weapons: Targeted Destruction in the Microbiota. Trends Microbiol. 2018, 26, 329–338. [Google Scholar] [CrossRef]
- Zhou, Q.; Gu, R.; Li, P.; Lu, Y.; Chen, L.; Gu, Q. Anti-Salmonella mode of action of natural L-phenyl lactic acid purified from Lactobacillus plantarum ZJ316. Appl. Microbiol. Biotechnol. 2020, 104, 5283–5292. [Google Scholar] [CrossRef]
- De Scoville, C.; De Brouwer, C.; Dujardin, M. Nobel chronicle: Fleming and Gratia. Lancet 1999, 354, 258. [Google Scholar] [CrossRef]
- Gross, M. The race against antibiotics resistance. Curr. Biol. 2019, 29, R859–R861. [Google Scholar] [CrossRef]
- Hernández-González, J.; Martínez-Tapia, A.; Lazcano-Hernández, G.; García-Pérez, B.; Castrejón-Jiménez, N. Bacteriocins from lactic acid bacteria. A powerful alternative as antimicrobials, probiotics, and immunomodulators in veterinary medicine. Animals 2021, 11, 979. [Google Scholar] [CrossRef]
- Soltani, S.; Hammami, R.; Cotter, P.D.; Rebuffat, S.; Said, L.B.; Gaudreau, H.; Bédard, F.; Biron, E.; Drider, D.; Fliss, I. Bacteriocins as a new generation of antimicrobials: Toxicity aspects and regulations. FEMS Microbiol. Rev. 2021, 45, fuaa039. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Lee, J.-B.; Park, S.-Y.; Choi, I.-S.; Lee, S.-W. Antimicrobial activity of dominant Ligilactobacillus animalis strains in healthy canine feces and their probiotic potential. FEMS Microbiol. Lett. 2022, 369, fnac115. [Google Scholar] [CrossRef]
- Hernández, D.; Cardell, E.; Zárate, V. Antimicrobial activity of lactic acid bacteria isolated from Tenerife cheese: Initial characterization of plantaricin TF711, a bacteriocin-like substance produced by Lactobacillus plantarum TF711. J. Appl. Microbiol. 2005, 99, 77–84. [Google Scholar] [CrossRef]
- Turner, M.; Waldherr, F.; Loessner, M.; Giffard, P. Antimicrobial activity of lysostaphin and a Listeria monocytogenes bacteriophage endolysin produced and secreted by lactic acid bacteria. Syst. Appl. Microbiol. 2007, 30, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Scillato, M.; Spitale, A.; Mongelli, G.; Privitera, G.F.; Mangano, K.; Cianci, A.; Stefani, S.; Santagati, M. Antimicrobial properties of Lactobacillus cell-free supernatants against multidrug-resistant urogenital pathogens. Microbiologyopen 2021, 10, e1173. [Google Scholar] [CrossRef]
- Spus, M.; Liu, H.; Wels, M.; Abee, T.; Smid, E.J. Isolation and characterization of Lactobacillus helveticus DSM 20075 variants with improved autolytic capacity. Int. J. Food Microbiol. 2017, 241, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Bearson, S.; Bearson, B.; Foster, J.W. Acid stress responses in enterobacteria. FEMS Microbiol. Lett. 1997, 147, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Rode, T.M.; Møretrø, T.; Langsrud, S.; Langsrud, Ø.; Vogt, G.; Holck, A. Responses of Staphylococcus aureus exposed to HCl and organic acid stress. Can. J. Microbiol. 2010, 56, 777–792. [Google Scholar] [CrossRef] [PubMed]
- Adetoye, A.; Pinloche, E.; Adeniyi, B.A.; Ayeni, F.A. Characterization and anti-salmonella activities of lactic acid bacteria isolated from cattle faeces. BMC Microbiol. 2018, 18, 96. [Google Scholar] [CrossRef] [PubMed]
- Dent, V.E.; Williams, R.A.D. Lactobacillus animalis sp. nov., a new species of lactobacillus from the alimentary canal of animals. Zent. Bakteriol. Mikrobiol. Hyg. I. Abt. Orig. C Allg. Angew. Okol. Mikrobiol. 1982, 3, 377–386. [Google Scholar] [CrossRef]
- Beck, C.N.; McDaniel, C.D.; Wamsley, K.G.S.; Kiess, A.S. The potential for inoculating Lactobacillus animalis and Enterococcus faecium alone or in combination using commercial in ovo technology without negatively impacting hatch and post-hatch performance. Poult. Sci. 2019, 98, 7050–7062. [Google Scholar] [CrossRef] [PubMed]
- Karunasena, E.; Kurkure, P.C.; Lackey, R.D.; McMahon, K.W.; Kiernan, E.P.; Graham, S.; Alabady, M.S.; Campos, D.L.; Tatum, O.L.; Brashears, M.M. Effects of the probiotic Lactobacillus animalis in murine Mycobacterium avium subspecies paratuberculosis infection. BMC Microbiol. 2013, 13, 8. [Google Scholar] [CrossRef] [PubMed]
- Tirloni, E.; Cattaneo, P.; Ripamonti, B.; Agazzi, A.; Bersani, C.; Stella, S. In vitro evaluation of Lactobacillus animalis SB310, Lactobacillus paracasei subsp. paracasei SB137 and their mixtures as potential bioprotective agents for raw meat. Food Control 2014, 41, 63–68. [Google Scholar] [CrossRef]
- Sahoo, T.K.; Jena, P.K.; Patel, A.K.; Seshadri, S. Purification and Molecular Characterization of the Novel Highly Potent Bacteriocin TSU4 Produced by Lactobacillus animalis TSU4. Appl. Biochem. Biotechnol. 2015, 177, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Casey, P.; Casey, G.; Gardiner, G.; Tangney, M.; Stanton, C.; Ross, R.; Hill, C.; Fitzgerald, G. Isolation and characterization of anti-Salmonella lactic acid bacteria from the porcine gastrointestinal tract. Lett. Appl. Microbiol. 2004, 39, 431–438. [Google Scholar] [CrossRef]
- Gaudana, S.B.; Dhanani, A.S.; Bagchi, T. Probiotic attributes of Lactobacillus strains isolated from food and of human origin. Br. J. Nutr. 2010, 103, 1620–1628. [Google Scholar] [CrossRef]
- Cotter, P.D.; Ross, R.P.; Hill, C. Bacteriocins-A viable alternative to antibiotics? Nat. Rev. Microbiol. 2013, 11, 95–105. [Google Scholar] [CrossRef]
- Arena, M.P.; Silvain, A.; Normanno, G.; Grieco, F.; Drider, D.; Spano, G.; Fiocco, D. Use of Lactobacillus plantarum strains as a bio-control strategy against food-borne pathogenic microorganisms. Front. Microbiol. 2016, 7, 464. [Google Scholar] [CrossRef]
- Fuochi, V.; Coniglio, M.A.; Laghi, L.; Rescifina, A.; Caruso, M.; Stivala, A.; Furneri, P.M. Metabolic characterization of supernatants produced by Lactobacillus spp. with in vitro anti-Legionella activity. Front. Microbiol. 2019, 10, 1403. [Google Scholar] [CrossRef]
- Saadatzadeh, A.; Fazeli, M.R.; Jamalifar, H.; Dinarvand, R. Probiotic Properties of Lyophilized Cell Free Extract of Lactobacillus casei. Jundishapur J. Nat. Pharm. Prod. 2013, 8, 131. [Google Scholar] [CrossRef]
- Xiang, Y.-Z.; Zhang, Y.-M.; Liu, Y.-Y.; Zhang, M.; Lin, L.-B.; Zhang, Q.-L. Purification, characterization, and antibacterial and antibiofilm activity of a novel bacteriocin against Salmonella Enteritidis. Food Control 2021, 127, 108110. [Google Scholar] [CrossRef]


| Cocultured Bacteria | Time | pH Value and CFU of Lactobacilli Strains | |||||
|---|---|---|---|---|---|---|---|
| L. plantarum ATCC 14917 | L. animalis SWLA-1 | L. animalis 11-2 | |||||
| pH | log10 CFU/mL | pH | log10 CFU/mL | pH | log10 CFU/mL | ||
| Salmonella gallinarum CNHJ001 | 0 h | 6.80 ± 0.00 | 3.21 ± 0.04 | 6.80 ± 0.00 | 3.18 ± 0.06 | 6.80 ± 0.00 | 3.21 ± 0.04 |
| 4 h | 6.64 ± 0.01 | 4.39 ± 0.02 | 6.63 ± 0.05 | 4.10 ± 0.07 | 6.65 ± 0.02 | 4.25 ± 0.17 | |
| 8 h | 6.55 ± 0.04 | 6.64 ± 0.05 | 6.58 ± 0.02 | 6.26 ± 0.15 | 6.60 ± 0.03 | 5.50 ± 0.22 | |
| 24 h | 4.71 ± 0.04 | 9.21 ± 0.04 | 4.67 ± 0.01 | 9.16 ± 0.07 | 4.70 ± 0.03 | 9.09 ± 0.06 | |
| Salmonella enteritidis 190610_1 | 0 h | 6.80 ± 0.00 | 3.22 ± 0.05 | 6.80 ± 0.00 | 3.22 ± 0.04 | 6.80 ± 0.00 | 3.11 ± 0.05 |
| 4 h | 6.61 ± 0.03 | 4.45 ± 0.05 | 6.65 ± 0.02 | 4.33 ± 0.03 | 6.64 ± 0.03 | 4.00 ± 0.08 | |
| 8 h | 6.58 ± 0.04 | 6.96 ± 0.04 | 6.59 ± 0.01 | 6.59 ± 0.09 | 6.60 ± 0.02 | 5.08 ± 0.13 | |
| 24 h | 4.55 ± 0.04 | 9.12 ± 0.04 | 4.53 ± 0.03 | 9.09 ± 0.04 | 4.52 ± 0.02 | 9.01 ± 0.50 | |
| Escherichia coli ROH_0034 | 0 h | 6.80 ± 0.00 | 3.21 ± 0.07 | 6.80 ± 0.00 | 3.24 ± 0.06 | 6.80 ± 0.00 | 3.05 ± 0.03 |
| 4 h | 6.57 ± 0.01 | 4.40 ± 0.08 | 6.60 ± 0.02 | 4.44 ± 0.03 | 6.62 ± 0.04 | 3.41 ± 0.09 | |
| 8 h | 6.53 ± 0.02 | 7.04 ± 0.04 | 6.55 ± 0.03 | 6.60 ± 0.09 | 6.60 ± 0.06 | 5.35 ± 0.13 | |
| 24 h | 4.69 ± 0.03 | 9.09 ± 0.06 | 4.66 ± 0.01 | 8.96 ± 0.04 | 4.68 ± 0.02 | 9.09 ± 0.07 | |
| Staphylococcus aureus ROH_0029 | 0 h | 6.80 ± 0.00 | 3.25 ± 0.03 | 6.80 ± 0.00 | 3.22 ± 0.06 | 6.80 ± 0.00 | 3.12 ± 0.05 |
| 4 h | 6.54 ± 0.02 | 4.32 ± 0.04 | 6.53 ± 0.03 | 4.46 ± 0.05 | 6.58 ± 0.02 | 4.00 ± 0.17 | |
| 8 h | 6.33 ± 0.02 | 7.01 ± 0.06 | 6.31 ± 0.01 | 7.01 ± 0.06 | 6.28 ± 0.03 | 5.38 ± 0.13 | |
| 24 h | 4.55 ± 0.01 | 9.15 ± 0.08 | 4.52 ± 0.02 | 9.11 ± 0.09 | 4.48 ± 0.01 | 9.01 ± 0.49 | |
| Treatment | Condition | Final pH | Residual Antimicrobial Activity (%) | ||||
|---|---|---|---|---|---|---|---|
| Concentration | S. gallinarum | S. enteritidis | E. coli | S. aureus | |||
| CFS (1×) | None | 5.1 | 100 | 100 | 100 | 100 | |
| Concentrated (10×) | Lyophilized, 24 h | 5.1 | 400 | 400 | 400 | 400 | |
| Temperature | |||||||
| 40 °C | Heated, 2 h | 5.1 | 100 | 100 | 100 | 100 | |
| 60 °C | Heated, 2 h | 5.1 | 100 | 100 | 100 | 100 | |
| 80 °C | Heated, 2 h | 5.1 | 100 | 100 16.7 | 100 | 100 | |
| 100 °C | Heated, 30 min | 5.1 | 83.3 16.7 | 83.3 16.7 | 100 | 100 | |
| pH | |||||||
| 2.0 | Exposure to pH 2 at 37 °C, 2 h | 6.8 | 50 | 50 | 50 | 50 | |
| 4.0 | Exposure to pH 4 at 37 °C, 2 h | 6.8 | 50 | 50 | 50 | 50 | |
| 6.0 | Exposure to pH 6 at 37 °C, 2 h | 6.8 | 50 | 25 | 50 | 50 | |
| 8.0 | Exposure to pH 8 at 37 °C, 2 h | 6.8 | 50 | 25 | 50 | 50 | |
| Enzyme | |||||||
| Proteinase K | 2 mg/mL at 37 °C, 2 h | 5.1 | 100 | 66.7 16.7 | 100 | 100 | |
| Trypsin | 1 mg/mL at 37 °C, 2 h | 5.1 | 83.3 16.7 | 66.7 16.7 | 83.3 16.7 | 83.3 16.7 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-J.; Lee, J.-B.; Park, S.-Y.; Choi, I.-S.; Lee, S.-W. Antimicrobial Activity of Ligilactobacillus animalis SWLA-1 and Its Cell-Free Supernatant against Multidrug-Resistant Bacteria and Its Potential Use as an Alternative to Antimicrobial Agents. Microorganisms 2023, 11, 182. https://doi.org/10.3390/microorganisms11010182
Lee H-J, Lee J-B, Park S-Y, Choi I-S, Lee S-W. Antimicrobial Activity of Ligilactobacillus animalis SWLA-1 and Its Cell-Free Supernatant against Multidrug-Resistant Bacteria and Its Potential Use as an Alternative to Antimicrobial Agents. Microorganisms. 2023; 11(1):182. https://doi.org/10.3390/microorganisms11010182
Chicago/Turabian StyleLee, Hong-Jae, Joong-Bok Lee, Seung-Yong Park, In-Soo Choi, and Sang-Won Lee. 2023. "Antimicrobial Activity of Ligilactobacillus animalis SWLA-1 and Its Cell-Free Supernatant against Multidrug-Resistant Bacteria and Its Potential Use as an Alternative to Antimicrobial Agents" Microorganisms 11, no. 1: 182. https://doi.org/10.3390/microorganisms11010182
APA StyleLee, H.-J., Lee, J.-B., Park, S.-Y., Choi, I.-S., & Lee, S.-W. (2023). Antimicrobial Activity of Ligilactobacillus animalis SWLA-1 and Its Cell-Free Supernatant against Multidrug-Resistant Bacteria and Its Potential Use as an Alternative to Antimicrobial Agents. Microorganisms, 11(1), 182. https://doi.org/10.3390/microorganisms11010182







