Mobile Phones: Reservoirs of Resistant Bacteria during the COVID-19 Pandemic in Abu Dhabi, United Arab Emirates
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Study Design
2.3. Inclusion and Exclusion Criteria
2.4. Sample Size and Sample Collection
2.5. Bacterial Culture and Identification
2.6. Antimicrobial Susceptibility Test (AST)
3. Results
3.1. Participants’ Characteristics
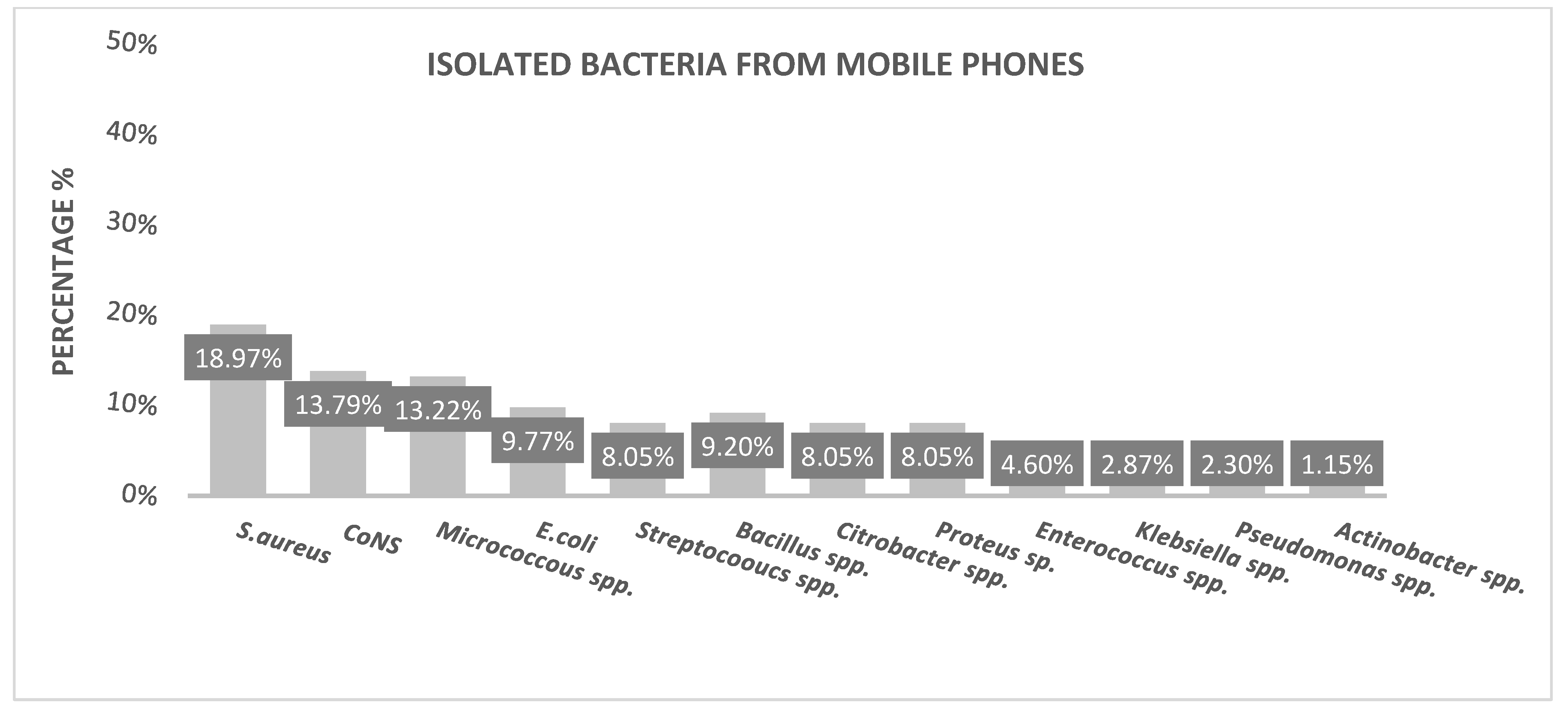
3.2. Mobile Phone Contamination
3.3. Antimicrobial Susceptibility Pattern of Bacterial Isolates
4. Discussion
5. Limitations
- The use of a self-reported questionnaire may create some biases since respondents may offer biased self-estimation.
- Participants were not asked if they removed their phone covers before cleaning them, nor if they allowed their phones to dry after the cleaning process.
- The study did not address the effect of period variations.
- The percentage of participants over 45 is 21.5% (n = 22). However, the number of participants who were over 65 years old is unknown. Therefore, it is not possible to assess the unintended consequences of this AMR in the elderly population.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Messina, G.; Quercioli, C.; Burgassi, S.; Nistic, F.; Lupoli, A.; Nante, N. How many bacteria live on the keyboard of your computer? Am. J. Infect. Control 2011, 39, 616–618. [Google Scholar] [CrossRef] [PubMed]
- Vinall, G.; Cogan, T.; Jeffery, A.; Tivers, M. Staphylococcal bacterial contamination of portable electronic devices in a large veterinary hospital. J. Small Anim. Pract. 2021, 62, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, R.; Lee, D.; Hayhurst, E. Mobile phones as fomites for potential pathogens in hospitals: Microbiome analysis reveals hidden contaminants. J. Hosp. Infect. 2020, 104, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Huffman, S.; Webb, C.; Spina, S.P. Investigation into the cleaning methods of smartphones and wearables from infectious contamination in a patient care environment (I-SWIPE). Am. J. Infect. Control 2020, 48, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Number Of Smartphone & Mobile Phone Users Worldwide (Billions). Available online: https://www.bankmycell.com/blog/how-many-phones-are-in-the-world (accessed on 30 January 2023).
- Statista Research Department. Statistic_Id617136_Worldwide-Digital-Population-April-2022.Pdf. Available online: https://www.statista.com/statistics/612450/uae-active-mobile-phone-subscriptions/ (accessed on 30 January 2023).
- Shukla, P.; Khalid, B.; Yaqoob, S.; Ahmad, S. Involvement of Mobile phones as a source for Nosocomial infections. Asian J. Med. Sci. 2021, 12, 126–129. Available online: https://www.nepjol.info/index.php/AJMS/article/view/34788 (accessed on 30 January 2023). [CrossRef]
- Alfoteih, Y.; Azizi, S.; Khajehkarimoddini, L.; Jaber, Z.A.S. Shisha—The hazardous 14 pastime: Microbial investigation of shisha apparatus in public cafés in the UAE. Malays. J. Public Health Med. 2018, 18, 101–108. [Google Scholar]
- Bodena, D.; Teklemariam, Z.; Balakrishnan, S.; Tesfa, T. Bacterial contamination of mobile phones of health professionals in Eastern Ethiopia: Antimicrobial susceptibility and associated factors. Trop. Med. Health 2019, 47, 15. [Google Scholar] [CrossRef]
- Al-Zubaidy, K.I. Bacterial Contamination on Mobile Phone Devices of Undergraduate Students in Al-Qurna Education College-Basrah. Kawakib. World J. Pharm. Res. 2019, 8. Available online: https://faculty.uobasrah.edu.iq/uploads/publications/1586702513.pdf (accessed on 30 January 2023).
- Mushabati, N.A.; Samutela, M.T.; Yamba, K.; Ngulube, J.; Nakazwe, R.; Nkhoma, P.; Kalonda, A. Bacterial contamination of mobile phones of healthcare workers at the University Teaching Hospital, Lusaka, Zambia. Infect. Prev. Pract. 2021, 3, 100126. [Google Scholar] [CrossRef]
- Gastmeier, P.; Brunkhorst, F.; Schrappe, M.; Kern, W.; Geffers, C. Wie viele nosokomiale Infektionen sind vermeidbar? How many nosocomial infections are avoidable? DMW—Dtsch. Med. Wochenschrift. 2010, 135, 91–93. Available online: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0029-1244823 (accessed on 30 January 2023). [CrossRef]
- Tannhäuser, R.; Nickel, O.; Lindner, M.; Bethge, A.; Wolf, J.; Borte, S.; Lübbert, C. Bacterial contamination of the smartphones of healthcare workers in a German tertiary-care hospital before and during the COVID-19 pandemic. Am. J. Infect. Control 2022, 50, 414–419. [Google Scholar] [CrossRef]
- Hu, Y.; Xu, L.; Wang, X.; Qin, X.; Wan, S.; Luo, Q.; Ding, Y.; Xiao, X.; Xiong, F. Changes before and after COVID-19 pandemic on the personal hygiene behaviors and incidence of peritonitis in peritoneal-dialysis patients: A multi-center retrospective study. Int. Urol. Nephrol. 2022, 54, 411–419. Available online: https://link.springer.com/10.1007/s11255-021-02924-5 (accessed on 30 January 2023). [CrossRef]
- The United Arab Emirates Government Portal the Official Guide to Living. 2020. Available online: https://u.ae/en#/ (accessed on 30 January 2023).
- World Health Organization Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 30 January 2023).
- Forbes, B.A.; Sahm, D.F.; Weissfeld, A.S. Bailey and Scott’s Diagnostic Microbiology, 12th ed.; Mosby: London, UK, 2007; 1024p. [Google Scholar]
- CLSI (Clinical and Laboratory Standards Institute). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. CLSI Document M100-S25. Vol. 32; CLSI: Wayne, PA, USA, 2015; pp. 1–184. [Google Scholar]
- Khadka, S.; Bosco Nshimiyimana, J.; Thapa, A.; Akayezu, V.; Mwizerwa, E.M.; Woldetsadik, A.G. Bacterial profile of mobile phones used by college students in Kigali, Rwanda. Int. J. Appl. Microbiol. Biotechnol. Res. 2018, 6, 87–94. Available online: http://www.bluepenjournals.org/ijambr/abstract/2018/August/Khadka_et_al.php (accessed on 30 January 2023).
- Rozario, S.R.; Rahman, H.; Fakhruddin, A.N.M.; Rabbani, K.A. Prevalence of multidrug-Resistant bacteria on mobile phone surface. J. Microsc. Ultrastruct. 2020, 8, 14. [Google Scholar] [PubMed]
- Olsen, M.; Lohning, A.; Campos, M.; Jones, P.; McKirdy, S.; Alghafri, R. Mobile phones of paediatric hospital staff are never cleaned and commonly used in toilets with implications for healthcare nosocomial diseases. Sci. Rep. 2021, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Dhama, K.; Patel, S.K.; Kumar, R.; Masand, R.; Rana, J.; Yatoo, M.I.; Tiwari, R.; Sharun, K.; Mohapatra, R.K.; Natesan, S.; et al. The role of disinfectants and sanitizers during COVID-19 pandemic: Advantages and deleterious effects on humans and the environment. Environ. Sci. Pollut. Res. 2021, 28, 34211–34228. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Liao, M.; He, B.; Liu, J.; Hu, X.; Yan, D.; Wang, J. Impact of the COVID-19 pandemic on household disinfectant consumption behaviors and related environmental concerns: A questionnaire-based survey in China. J. Environ. Chem. Eng. 2021, 9, 106168. [Google Scholar] [CrossRef] [PubMed]
- Vally, Z. Public perceptions, anxiety and the perceived efficacy of health-protective behaviours to mitigate the spread of the SARS-CoV-2/COVID-19 pandemic. Public Health 2020, 187, 67–73. [Google Scholar] [CrossRef]
- Olsen, M.; Campos, M.; Lohning, A.; Jones, P.; Legget, J.; Bannach-Brown, A.; McKirdy, S.; Alghafri, R.; Tajouri, L. Mobile phones represent a pathway for microbial transmission: A scoping review. Travel Med. Infect. Dis. 2020, 35, 101704. [Google Scholar] [CrossRef]
- Chaka, T.E. Bacterial Isolates from Cell Phones and Hands of Health Care Workers: A Cross Sectional Study in Pediatric Wards at Black Lion Hospital, Addis Ababa, Ethiopia. J. Bacteriol. Parasitol. 2016, 7, 2–7. [Google Scholar] [CrossRef]
- Ulger, F.; Esen, S.; Dilek, A.; Yanik, K.; Gunaydin, M.; Leblebicioglu, H. Are we aware how contaminated our mobile phones with nosocomial pathogens? Ann. Clin. Microbiol. Antimicrob. 2009, 8, 4–7. [Google Scholar]
- Zakai, S.; Mashat, A.; Abumohssin, A.; Samarkandi, A.; Almaghrabi, B.; Barradah, H.; Jiman-Fatani, A. Bacterial contamination of cell phones of medical students at King Abdulaziz University, Jeddah, Saudi Arabia. J. Microsc. Ultrastruct. 2016, 4, 143. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Abdelwahab, G.E.; Zackaria, H.; Ishag, A.; Mohamed, Z.; Hammadi, A.; Mohamed, S.; Al neyadi, S.S.A.; Al Mansoori, A.M.A.; Al Hamadi, F.H.A.; Al Hamadi, I.A.S.; et al. Antibiotics Resistance in Escherichia coli Isolated from Livestock in the Emirate of Abu Dhabi, UAE, 2014–2019. Int. J. Microbiol. 2022, 2022, 3411560. [Google Scholar] [CrossRef] [PubMed]
- Karlowsky, J.A.; Bouchillon, S.K.; El, R.; Kotb, M.; Mohamed, N.; Stone, G.G.; Sahm, D.F. In vitro activity of ceftazidime/avibactam against clinical isolates of Enterobacterales and Pseudomonas aeruginosa from Middle Eastern and African countries: ATLAS global surveillance programme 2015–18. JAC Antimicrob. Resist. 2021, 3, 4–9. [Google Scholar] [CrossRef]
- Al-ajmi, D.; Rahman, S.; Banu, S. Occurrence, virulence genes, and antimicrobial profiles of Escherichia coli O157 isolated from ruminants slaughtered in Al Ain, United Arab Emirates. BMC Microbiol. 2020, 20, 210. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, A.R.; Safaee, M.M.; Wuest, W.M.; Furst, A.L. The silent pandemic: Emergent antibiotic resistances following the global response to SARS-CoV-2. iScience 2021, 24, 102304. [Google Scholar] [CrossRef]
| Overall (n = 102) | ||
|---|---|---|
| n | % | |
| Age | ||
| 22–34 | 48 | 47.1 |
| 35–44 | 32 | 31.4 |
| ≥45 | 22 | 21.5 |
| Gender | ||
| Male | 53 | 52 |
| Female | 49 | 48 |
| Marital status | ||
| Single | 34 | 33.3 |
| Married | 68 | 66.7 |
| Education level | ||
| Bachelor | 51 | 50 |
| Master | 18 | 17.6 |
| Doctorate | 33 | 32.4 |
| Phone type | ||
| Screen Touch | 100 | 98 |
| Keypad | 2 | 2 |
| Phone cover | ||
| Yes | 77 | 75.5 |
| No | 25 | 24.5 |
| Mobile usage frequency at work | ||
| 1–5 times per day | 34 | 33.3 |
| 6–9 times per day | 21 | 20.6 |
| ≥10 times per day | 47 | 46.1 |
| Phone usage in bathrooms | ||
| Yes | 43 | 42.2 |
| No | 59 | 57.8 |
| Frequency of hands washing | ||
| 1–10 per day | 61 | 59.8 |
| 11–20 per day | 41 | 40.2 |
| Mobile phone storage at work | ||
| Desk | 75 | 73.5 |
| Drawer | 4 | 3.9 |
| 18 | 17.6 | |
| Bag | 5 | 4.9 |
| Mobile phone usage by kids, husband or wife | ||
| Yes | 38 | 37.3 |
| No | 64 | 62.7 |
| Phone cleaning | ||
| Wipes | 54 | 52.9 |
| Alcohol | 35 | 34.3 |
| Not applicable | 9 | 8.8 |
| Water | 4 | 3.9 |
| Organism | Antimicrobial Susceptibility (%) | |||||
|---|---|---|---|---|---|---|
| S/R | Ciprofloxacin | CTX | AM | GN | CAZ | |
| S. aureus (n = 33) | S | 100 | 81.8 | 39.3 | 96.9 | 51.5 |
| R | 0 | 18.1 | 60.6 | 3.03 | 48.4 | |
| CoNS (n = 24) | S | 100 | 83.3 | 50 | 100 | 75 |
| R | 0 | 16.6 | 50 | 0 | 25 | |
| E. coli (n = 17) | S | 100 | 82.3 | 52.9 | 100 | 64.7 |
| R | 0 | 17.6 | 47.05 | 0 | 35.3 | |
| Streptococcus spp. (n = 14) | S | 100 | 85.7 | 28.5 | 100 | 35.7 |
| R | 0 | 14.2 | 71.4 | 0 | 64.3 | |
| Bacillus spp. (n = 16) | S | 100 | 75 | 31.25 | 100 | 37.5 |
| R | 0 | 25 | 68.75 | 0 | 62.5 | |
| Citrobacter spp. (n = 14) | S | 100 | 71.4 | 21.4 | 100 | 57.1 |
| R | 0 | 28.5 | 78.5 | 0 | 42.8 | |
| Proteus spp. (n = 14) | S | 100 | 71.4 | 21.4 | 100 | 57.1 |
| R | 0 | 28.5 | 78.5 | 0 | 42.9 | |
| Enterococcus spp. (n = 8) | S | 100 | 100 | 50 | 100 | 62.5 |
| R | 0 | 0 | 50 | 0 | 37.5 | |
| Klebsiella spp. (n = 5) | S | 100 | 60 | 40 | 100 | 40 |
| R | 0 | 40 | 60 | 0 | 60 | |
| Pseudomonas spp. (n = 4) | S | 100 | 50 | 25 | 100 | 25 |
| R | 0 | 50 | 75 | 0 | 75 | |
| Micrococcus (n = 23) | S | 100 | 86.9 | 43.47 | 100 | 65.2 |
| R | 0 | 13.04 | 56.5 | 0 | 34.8 | |
| Actinobacteria (n = 2) | S | 100 | 100 | 50 | 100 | 100 |
| R | 0 | 0 | 50 | 0 | 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kayed, K.; Khoder, G.; Farhat, J.; Ghemrawi, R. Mobile Phones: Reservoirs of Resistant Bacteria during the COVID-19 Pandemic in Abu Dhabi, United Arab Emirates. Microorganisms 2023, 11, 523. https://doi.org/10.3390/microorganisms11020523
Kayed K, Khoder G, Farhat J, Ghemrawi R. Mobile Phones: Reservoirs of Resistant Bacteria during the COVID-19 Pandemic in Abu Dhabi, United Arab Emirates. Microorganisms. 2023; 11(2):523. https://doi.org/10.3390/microorganisms11020523
Chicago/Turabian StyleKayed, Kawthar, Ghalia Khoder, Joviana Farhat, and Rose Ghemrawi. 2023. "Mobile Phones: Reservoirs of Resistant Bacteria during the COVID-19 Pandemic in Abu Dhabi, United Arab Emirates" Microorganisms 11, no. 2: 523. https://doi.org/10.3390/microorganisms11020523
APA StyleKayed, K., Khoder, G., Farhat, J., & Ghemrawi, R. (2023). Mobile Phones: Reservoirs of Resistant Bacteria during the COVID-19 Pandemic in Abu Dhabi, United Arab Emirates. Microorganisms, 11(2), 523. https://doi.org/10.3390/microorganisms11020523






