Novel Virus Air Sampler Based on Electrostatic Precipitation and Air Sampling of SARS-CoV-2
Abstract
:1. Introduction
2. Material and Methods
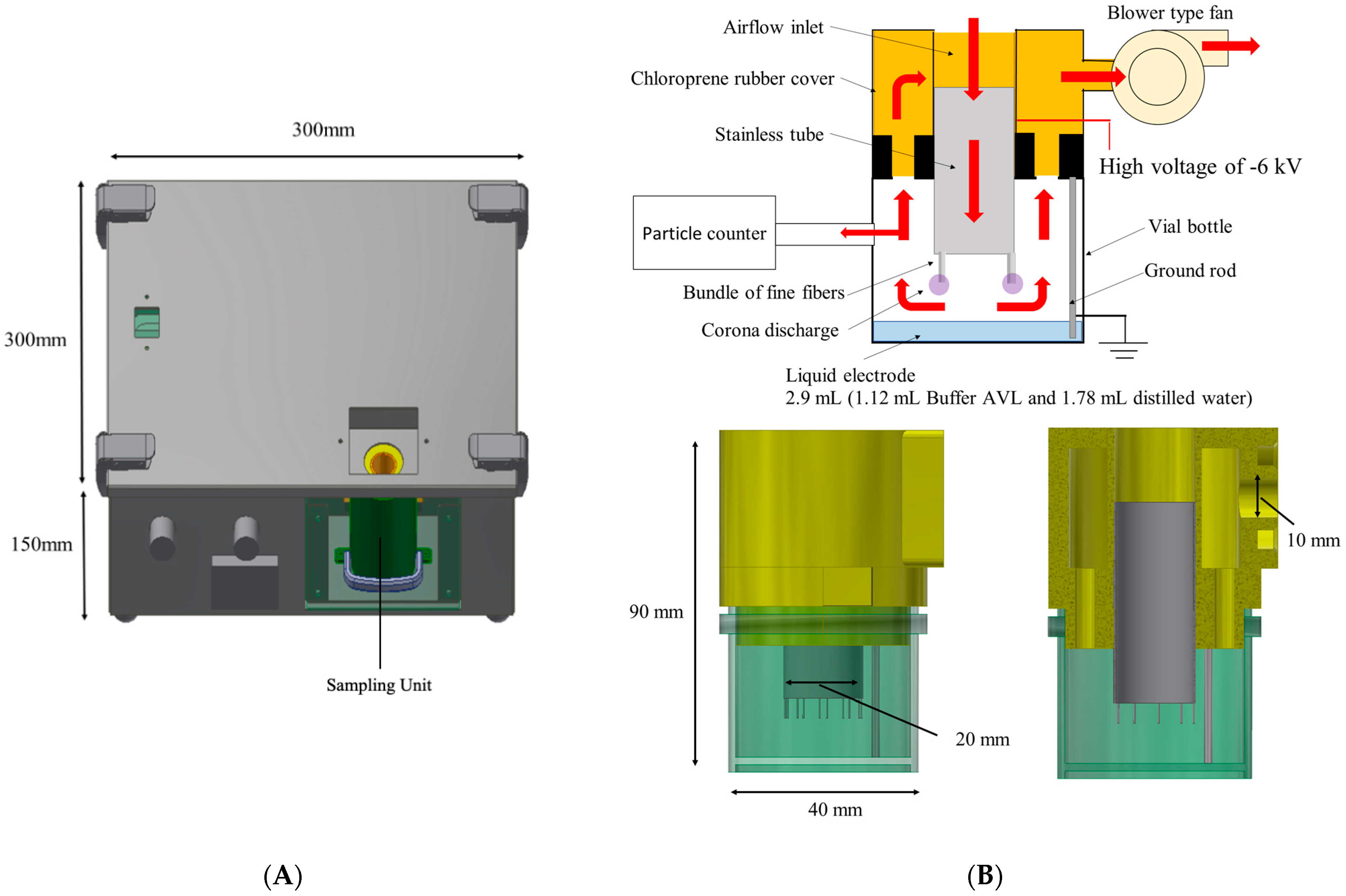
2.1. Structure and Performance of the Developed Air Sampler
2.2. Measurement of the Particle Collection Efficiency of the Developed Air Sampler When Compared with an Impinger and a Filter-Type Air Sampler
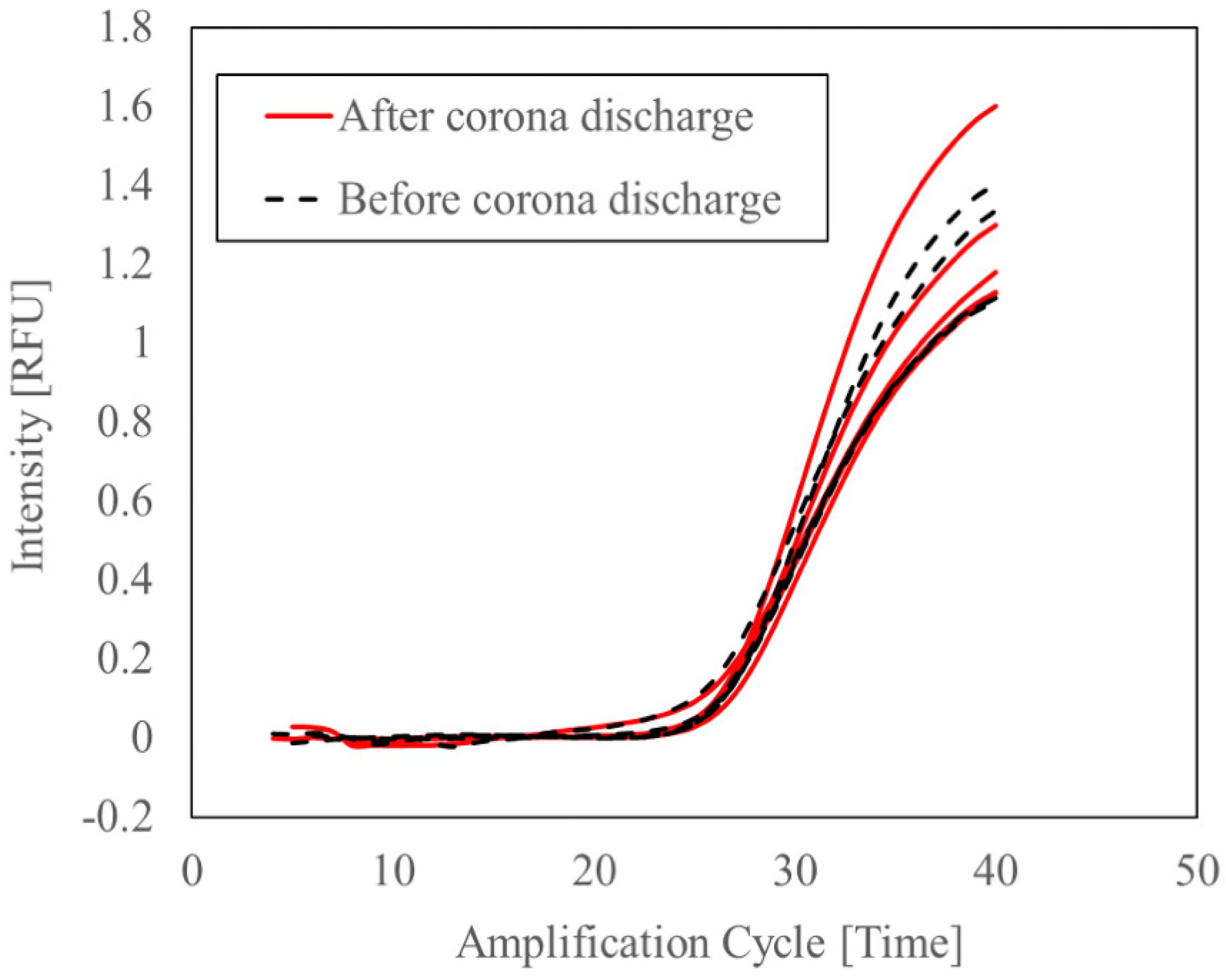
2.3. Evaluation of the Protective Effect of the Viral Lysis Buffer on RNA from Damage Caused by Exposure to Corona Discharge
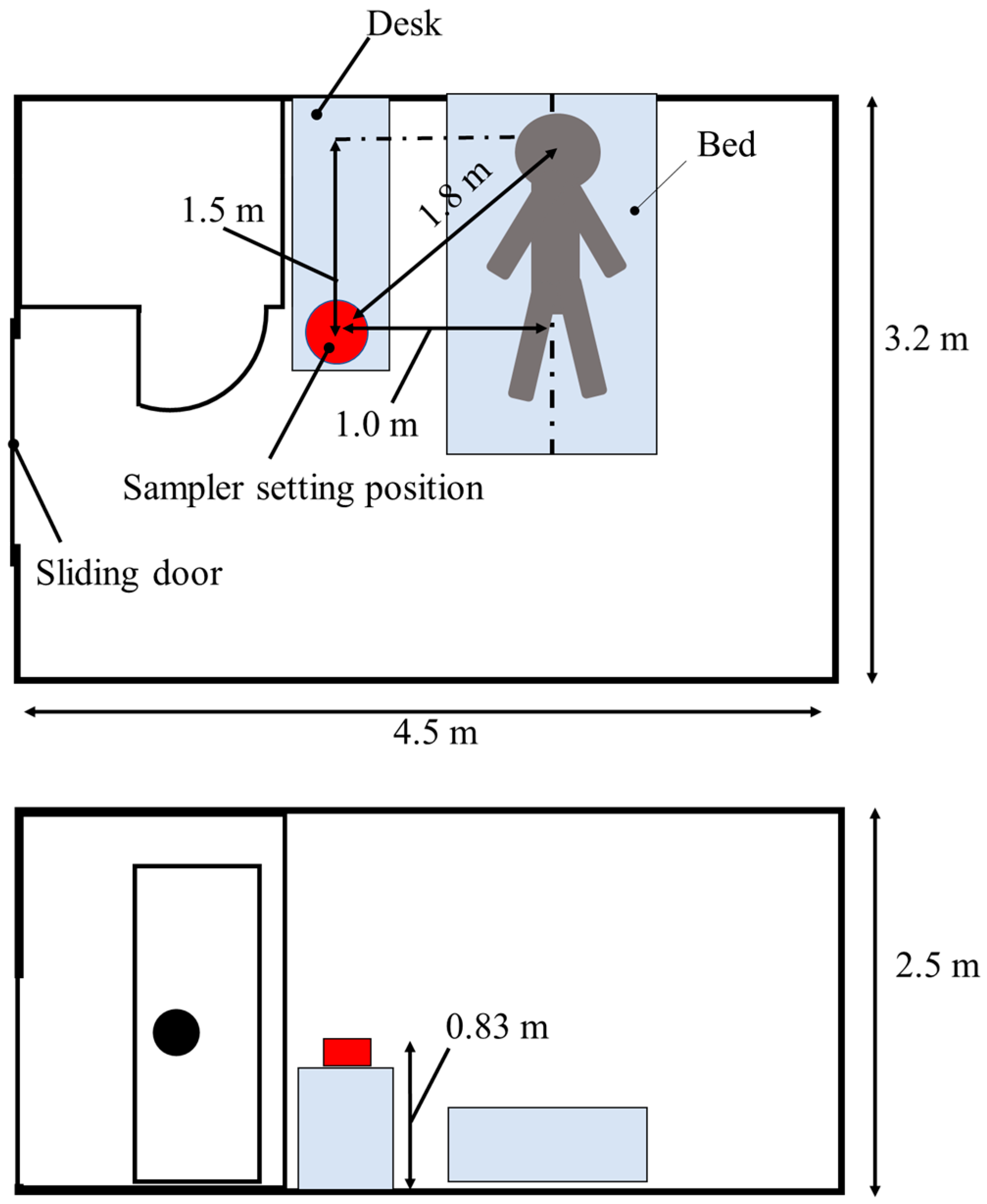
2.4. Measurement of the Concentration of SARS-CoV-2 RNA in the Air of Hospital Rooms Inhabiting COVID-19 Patients and Public Spaces
3. Results
3.1. Particle Collection Efficiency of the Developed Electrostatic Air Sampler Compared with That of an Impinger and a Filter-Type Air Sampler
3.2. Evaluation of the Protective Effect of the Viral Lysis Buffer on RNA from Damage Caused by Exposure to Corona Discharge
3.3. Measurement of the of SARS-CoV-2 RNA Concentration in the Air of Hospital Rooms Inhabiting COVID-19 Patients and Public Spaces
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McVernon, J.; Liberman, J. WHO keeps covid-19 a public health emergency of international concern. BMJ 2023, 380, 504. [Google Scholar] [CrossRef] [PubMed]
- Alsved, M.; Matamis, A.; Bohlin, R.; Richter, M.; Bengtsson, P.E.; Fraenkel, C.J.; Medstrand, P.; Löndahl, J. Exhaled respiratory particles during singing and talking. Aerosol Sci. Technol. 2020, 54, 1245–1248. [Google Scholar] [CrossRef]
- Cai, J.; Sun, W.; Huang, J.; Gamber, M.; Wu, J.; He, G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1343. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W.; Marr, L.C.; Li, Y.; Dancer, S.J. Covid-19 has redefined airborne transmission. BMJ 2021, 373, 913. [Google Scholar] [CrossRef]
- Dinoi, A.; Feltracco, M.; Chirizzi, D.; Trabucco, S.; Conte, M.; Gregoris, E.; Barbaro, E.; La Bella, G.; Ciccarese, G.; Belosi, F.; et al. A review on measurements of SARS-CoV-2 genetic material in air in outdoor and indoor environments: Implication for airborne transmission. Sci. Total Environ. 2022, 809, 151137. [Google Scholar] [CrossRef]
- Nakanishi, A.; Saiki, A.; Ohta, K.; Tanimura, Y.; Yasuda, H.; Mizuno, A. Evaluation Method on Removability of Airborne Virus—Evaluation Method Using Bacteriophage φX 174-. J. Inst. Electrostat. JPN 2011, 35, 108–113. [Google Scholar]
- Fabian, P.; McDevitt, J.J.; Houseman, E.A.; Milton, D.K. Airborne influenza virus detection with four aerosol samplers using molecular and infectivity assays: Considerations for a new infectious virus aerosol sampler. Indoor Air 2009, 19, 433–441. [Google Scholar] [CrossRef] [Green Version]
- Haig, C.W.; Mackay, W.G.; Walker, J.T.; Williams, C. Bioaerosol sampling: Sampling mechanisms, bioefficiency and field studies. J. Hosp. Infect. 2016, 93, 242–255. [Google Scholar] [CrossRef]
- Mizuno, A.; Yasuda, H. Damages of Biological Components in Bacteria and Bacteriophages Exposed to Atmospheric Non-thermal Plasma. In Plasma for Bio-Decontamination, Medicine and Food Security (NATO Science for Peace and Security Series A: Chemistry and Biology); 2012th ed.; Machala, Z., Hensel, K., Akishev, Y., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 79–92. [Google Scholar]
- Kisanuki, Y.; Fukuda, K.; Makishima, Y.; Kitabayashi, K.; Katsushima, S.; Debacher, N.; Takashima, K.; Mizuno, A. Corona Discharge with Bundle of Fine Conductive Fibers for Electrostatic Precipitation of Fine Smoke Particles. Int. J. Plasma Environ. Sci. Technol. 2019, 13, 21–25. [Google Scholar]
- Kim, H.R.; An, S.; Hwang, J. High air flow-rate electrostatic sampler for the rapid monitoring of airborne coronavirus and influenza viruses. J. Hazard. Mater. 2021, 412, 125219. [Google Scholar] [CrossRef]
- Roux, J.M.; Kaspari, O.; Heinrich, R.; Hanschmann, N.; Grunow, R. Investigation of a New Electrostatic Sampler for Concentrating Biological and Non-Biological Aerosol Particles. Aerosol Sci. Technol. 2013, 47, 463–471. [Google Scholar] [CrossRef] [Green Version]
- Ladhani, L.; Pardon, G.; Moons, P.; Goossens, H.; van der Wijngaart, W. Electrostatic Sampling of Patient Breath for Pathogen Detection: A Pilot Study. Front. Mech. Eng. 2020, 6, 40. [Google Scholar] [CrossRef]
- Abdel-Salam, M.; Nakano, M.; Tanino, M.; Mizuno, A. Culturing of cells as influenced by exposure to AC and DC fields. J. Phys. Conf. Ser. 2008, 142, 012051. [Google Scholar] [CrossRef]
- Tanaka, Y.; Yasuda, H.; Kurita, H.; Takashima, K.; Mizuno, A. Analysis of the Inactivation Mechanism of Bacteriophage φX174 by Atmospheric Pressure Discharge Plasma. IEEE Trans. Ind. Appl. 2014, 50, 1397–1401. [Google Scholar] [CrossRef]
- Yasuda, H.; Hashimoto, M.; Rahman, M.; Takashima, K.; Mizuno, A. States of Biological Components in Bacteria and Bacteriophages during Inactivation by Atmospheric Dielectric Barrier Discharges. Plasma Process. Polym. 2008, 5, 615–621. [Google Scholar] [CrossRef]
- Yasuda, H.; Miura, T.; Kurita, H.; Takashima, K.; Mizuno, A. Biological Evaluation of DNA Damage in Bacteriophages Inactivated by Atmospheric Pressure Cold Plasma. Plasma Process. Polym. 2010, 7, 301–308. [Google Scholar] [CrossRef]
- Santarpia, J.L.; Herrera, V.L.; Rivera, D.N.; Ratnesar-Shumate, S.; Reid, S.P.; Denton, P.W.; Martens, J.W.S.; Fang, Y.; Conoan, N.; Callahan, M.V.; et al. The size and culturability of patient-generated SARS-CoV-2 aerosol. J. Expo. Sci. Environ. Epidemiol. 2022, 32, 706–711. [Google Scholar] [CrossRef]
- The Japan Electrical Manufacturers’ Association. Airborne Viruses Removal Performance of Air Purifiers. Available online: https://www.jema-net.or.jp/Japanese/ha/kuusei/hyoukashiken/hyouka1.pdf (accessed on 23 March 2023).
- Mostafa, H.H.; Carroll, K.C.; Hicken, R.; Berry, G.J.; Manji, R.; Smith, E.; Rakeman, J.L.; Fowler, R.C.; Leelawong, M.; Butler-Wu, S.M.; et al. Multicenter Evaluation of the Cepheid Xpert Xpress SARS-CoV-2/Flu/RSV Test. J. Clin. Microbiol. 2021, 59, e02955-20. [Google Scholar] [CrossRef]
- Shirato, K.; Nao, N.; Katano, H.; Takayama, I.; Saito, S.; Kato, F.; Katoh, H.; Sakata, M.; Nakatsu, Y.; Mori, Y.; et al. Development of Genetic Diagnostic Methods for Novel Coronavirus 2019 (nCoV-2019) in Japan. Jpn. J. Infect. Dis. 2020, 73, 304–307. [Google Scholar] [CrossRef] [Green Version]
- Hadfield, J.; Megill, C.; Bell, S.M.; Huddleston, J.; Potter, B.; Callender, C.; Sagulenko, P.; Bedford, T.; Neher, R.A. Nextstrain: Real-time tracking of pathogen evolution. Bioinformatics 2018, 34, 4121–4123. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labour and Welfare. Visualizing the Data: Information on COVID-19 Infections. Available online: https://covid19.mhlw.go.jp/en/ (accessed on 19 February 2023).
- Wang, Y.X.; Su, W.C.; Wang, Q.; Lin, Y.F.; Zhou, Y.; Lin, L.F.; Ren, S.; Li, Y.T.; Chen, Q.X.; Shi, Y. Antityrosinase and antioxidant activities of guanidine compounds and effect of guanylthiourea on melanogenesis. Process. Biochem. 2019, 85, 84–96. [Google Scholar] [CrossRef]
- Blow, J.A.; Mores, C.N.; Dyer, J.; Dohm, D.J. Viral nucleic acid stabilization by RNA extraction reagent. J. Virol. Methods 2008, 150, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Ladhani, L.; Pardon, G.; Meeuws, H.; van Wesenbeeck, L.; Schmidt, K.; van der Stuyver, L.; Wijngaart, W. Sampling and detection of airborne influenza virus towards point-of-care applications. PLoS ONE 2017, 12, e0174314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berglund, B.; Lindvall, T.; Schwela, D.H.; World Health Organization; Occupational and Environmental Health Team. Guidelines for Community Noise. Available online: https://apps.who.int/iris/handle/10665/66217 (accessed on 19 February 2023).
- BioSampler® Bioaerosol Collection Device. Cat. No. 225 Series. Available online: https://www.skcinc.com/media/documents/KnowledgeCenter/Technical%20Information/Product%20Publications/Operating%20Instructions/BioSampler%20Bioaerosol%20Collection%20Device%20225%20Series%20OI.pdf (accessed on 21 February 2023).
- BioLite+ Air Sampling Pump. Operating Instructions. Available online: https://www.skcinc.com/media/documents/KnowledgeCenter/Technical%20Information/Product%20Publications/Operating%20Instructions/BioLite%20Sample%20Pump%20228-9615%20OI.pdf (accessed on 21 February 2023).
- AirPort MD8. The New Portable Air Sampler. Available online: https://assets.fishersci.com/TFS-Assets/CCG/EU/Sartorius-Stedim-Biotech/brochures/SAR058_EN%20Broch_MD8_Airport.pdf (accessed on 21 February 2023).
- Santarpia, J.L.; Rivera, D.N.; Herrera, V.L.; Morwitzer, M.J.; Creager, H.M.; Santarpia, G.W.; Crown, K.K.; Brett-Major, D.M.; Schnaubelt, E.R.; Broadhurst, M.J.; et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020, 10, 13892. [Google Scholar] [CrossRef] [PubMed]
- Stern, R.A.; Al-Hemoud, A.; Alahmad, B.; Koutrakis, P. Levels and particle size distribution of airborne SARS-CoV-2 at a healthcare facility in Kuwait. Sci. Total Environ. 2021, 782, 146799. [Google Scholar] [CrossRef]
- Guo, Z.D.; Wang, Z.Y.; Zhang, S.F.; Li, X.; Li, L.; Li, C.; Cui, Y.; Fu, R.B.; Dong, Y.Z.; Chi, X.Y.; et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020, 26, 1583–1591. [Google Scholar] [CrossRef]
- Kim, K.S.; Ejima, K.; Iwanami, S.; Fujita, Y.; Ohashi, H.; Koizumi, Y.; Asai, Y.; Nakaoka, S.; Watashi, K.; Aihara, K.; et al. A quantitative model used to compare within-host SARS-CoV-2, MERS-CoV, and SARS-CoV dynamics provides insights into the pathogenesis and treatment of SARS-CoV-2. PLoS Biol. 2021, 19, e3001128. [Google Scholar] [CrossRef]
- Young, B.E.; Ong, S.W.X.; Kalimuddin, S.; Low, J.G.; Tan, S.Y.; Loh, J.; Ng, O.T.; Marimuthu, K.; Ang, L.W.; Mak, T.M.; et al. Epidemiologic Features and Clinical Course of Patients Infected with SARS-CoV-2 in Singapore. JAMA 2020, 323, 1488–1494. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Yan, L.M.; Wan, L.; Xiang, T.X.; Le, A.; Liu, J.M.; Peiris, M.; Poon, L.L.M.; Zhang, W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020, 20, 656–657. [Google Scholar] [CrossRef] [Green Version]
- Puhach, O.; Meyer, B.; Eckerle, I. SARS-CoV-2 viral load and shedding kinetics. Nat. Rev. Microbiol. 2023, 21, 147–161. [Google Scholar] [CrossRef]
- Ueki, H.; Furusawa, Y.; Iwatsuki-Horimoto, K.; Imai, M.; Kabata, H.; Nishimura, H.; Kawaoka, Y. Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. mSphere 2020, 5, e00637-20. [Google Scholar] [CrossRef] [PubMed]
- Coleman, K.K.; Wen Tay, D.J.; Tan, K.S.; Xiang Ong, S.W.; Son, T.T.; Koh, M.H.; Chin, Y.Q.; Nasir, H.; Mak, T.M.; Chu, J.J.H.; et al. Viral Load of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Respiratory Aerosols Emitted by Patients with Coronavirus Disease 2019 (COVID-19) While Breathing, Talking, and Singing. Clin. Infect. Dis. 2022, 74, 1722–1728. [Google Scholar] [CrossRef] [PubMed]
- Conte, M.; Feltracco, M.; Chirizzi, D.; Trabucco, S.; Dinoi, A.; Gregoris, E.; Barbaro, E.; La Bella, G.; Ciccarese, G.; Belosi, F.; et al. Airborne concentrations of SARS-CoV-2 in indoor community environments in Italy. Environ. Sci. Pollut. Res. Int. 2022, 29, 13905–13916. [Google Scholar] [CrossRef] [PubMed]
- Schijven, J.; Vermeulen, L.C.; Swart, A.; Meijer, A.; Duizer, E.; de Roda Husman, A.M. Quantitative Microbial Risk Assessment for Airborne Transmission of SARS-CoV-2 via Breathing, Speaking, Singing, Coughing, and Sneezing. Environ. Health Perspect. 2021, 129, 47002. [Google Scholar] [CrossRef] [PubMed]
- Strong, J.E.; Feldmann, H. The Crux of Ebola Diagnostics. J. Infect. Dis. 2017, 216, 1340–1342. [Google Scholar] [CrossRef]
- Xu, Y.; Cheng, M.; Chen, X.; Zhu, J. Current approaches in laboratory testing for SARS-CoV-2. Int. J. Infect. Dis. 2020, 100, 7–9. [Google Scholar] [CrossRef]
- Funk, D.J.; Bullard, J.; Lother, S.; Grande, G.V.; Garnett, L.; Doan, K.; Dust, K.; Kumar, A.; Poliquin, G.; Strong, J. Persistence of live virus in critically ill patients infected with SARS-COV-2: A prospective observational study. Crit. Care 2022, 26, 10. [Google Scholar] [CrossRef]
- Shinoda, H.; Taguchi, Y.; Nakagawa, R.; Makino, A.; Okazaki, S.; Nakano, M.; Muramoto, Y.; Takahashi, C.; Takahashi, I.; Ando, J.; et al. Amplification-free RNA detection with CRISPR–Cas13. Commun. Biol. 2021, 4, 476. [Google Scholar] [CrossRef]
| Patient ID | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Age | 80s | 80s | 30s | 50s | 70s | 60s | 80s | 30s | 30s | 30s |
| Gender | Male | Female | Female | Male | Female | Male | Male | Female | Male | Female |
| Severity | Severe | Severe | Moderate | Moderate | Moderate | Moderate | Moderate | Mild | Mild | Mild |
| Variant | Omicron 21K/BA1.1 | Delta 21A | Omicron 21K/BA1.1 | Omicron 21K/BA1.1 | Omicron 21K/BA1.1 | Omicron 21K/Ba2 | Omicron BA.5 | Omicron 21K/BA1.1 | Omicron 21K/BA1.1 | ND ** |
| Vaccination | Unknown | None | None | 2 times | 3 times | 3 times | Unknown | Unknown | None | None |
| Ct value * | 31.5 | 27 | 29.9 | 21.3 | 26.3 | 14.4 | 17.9 | 17.6 | 17.1 | ND ** |
| Days after symptom onset | Viral concentration (copies/m3) | |||||||||
| 0 | ||||||||||
| 1 | ||||||||||
| 2 | 1.1 × 103 | 3.0 × 102 | 3.1 × 102 | |||||||
| 3 | 1.0 × 103 | 2.4 × 104 | ||||||||
| 4 | (dead) | 9.3 × 102 | 1.0 × 103 | 0 | 1.7 × 103 | |||||
| 5 | 4.7 × 103 | 1.0 × 103 | 9.2 × 102 | 1.8 × 102 | 0 | 1.0 × 102 | ||||
| 6 | 6.0 × 102 | 0 | 1.2 × 103 | 1.2 × 102 | ||||||
| 7 | 1.3 × 103 | |||||||||
| 8 | 0 | 0 | ||||||||
| 9 | 0 | |||||||||
| 10 | 2.5 × 102 | 0 | 3.9 × 102 | |||||||
| 11 | 0 | (discharge) | (discharge) | |||||||
| 12 | (discharge) | (discharge) | ||||||||
| 13 | 2.2 × 102 | (discharge) | ||||||||
| 14 | ||||||||||
| 15 | ||||||||||
| 16 | (discharge) | |||||||||
| 17 | 1.4 × 102 | |||||||||
| 18 | 1.3 × 103 | (discharge) | ||||||||
| 19 | (dead) | |||||||||
| 20 | ||||||||||
| Office | Food Court | Station Corridor | |
| Space volume (m3) | 340 | 2000 | 1500 |
| Number of people | 30 | 300 | 100 |
| m3/people | 11 | 6.7 | 15 |
| Ct value | 33.7 | 36.3 | ND ** |
| Virus RNA concentration (copy/m3) | 7.8 × 102 | 1.9 × 102 | ND ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukuda, K.; Baba, H.; Yoshida, M.; Kitabayashi, K.; Katsushima, S.; Sonehara, H.; Mizuno, K.; Kanamori, H.; Tokuda, K.; Nakagawa, A.; et al. Novel Virus Air Sampler Based on Electrostatic Precipitation and Air Sampling of SARS-CoV-2. Microorganisms 2023, 11, 944. https://doi.org/10.3390/microorganisms11040944
Fukuda K, Baba H, Yoshida M, Kitabayashi K, Katsushima S, Sonehara H, Mizuno K, Kanamori H, Tokuda K, Nakagawa A, et al. Novel Virus Air Sampler Based on Electrostatic Precipitation and Air Sampling of SARS-CoV-2. Microorganisms. 2023; 11(4):944. https://doi.org/10.3390/microorganisms11040944
Chicago/Turabian StyleFukuda, Kyohei, Hiroaki Baba, Mie Yoshida, Kouichi Kitabayashi, Shinjirou Katsushima, Hiroki Sonehara, Kazue Mizuno, Hajime Kanamori, Koichi Tokuda, Atsuhiro Nakagawa, and et al. 2023. "Novel Virus Air Sampler Based on Electrostatic Precipitation and Air Sampling of SARS-CoV-2" Microorganisms 11, no. 4: 944. https://doi.org/10.3390/microorganisms11040944





