The Impact of the COVID-19 Pandemic on Influenza Transmission in Poland
Abstract
:1. Introduction
2. Materials and Methods
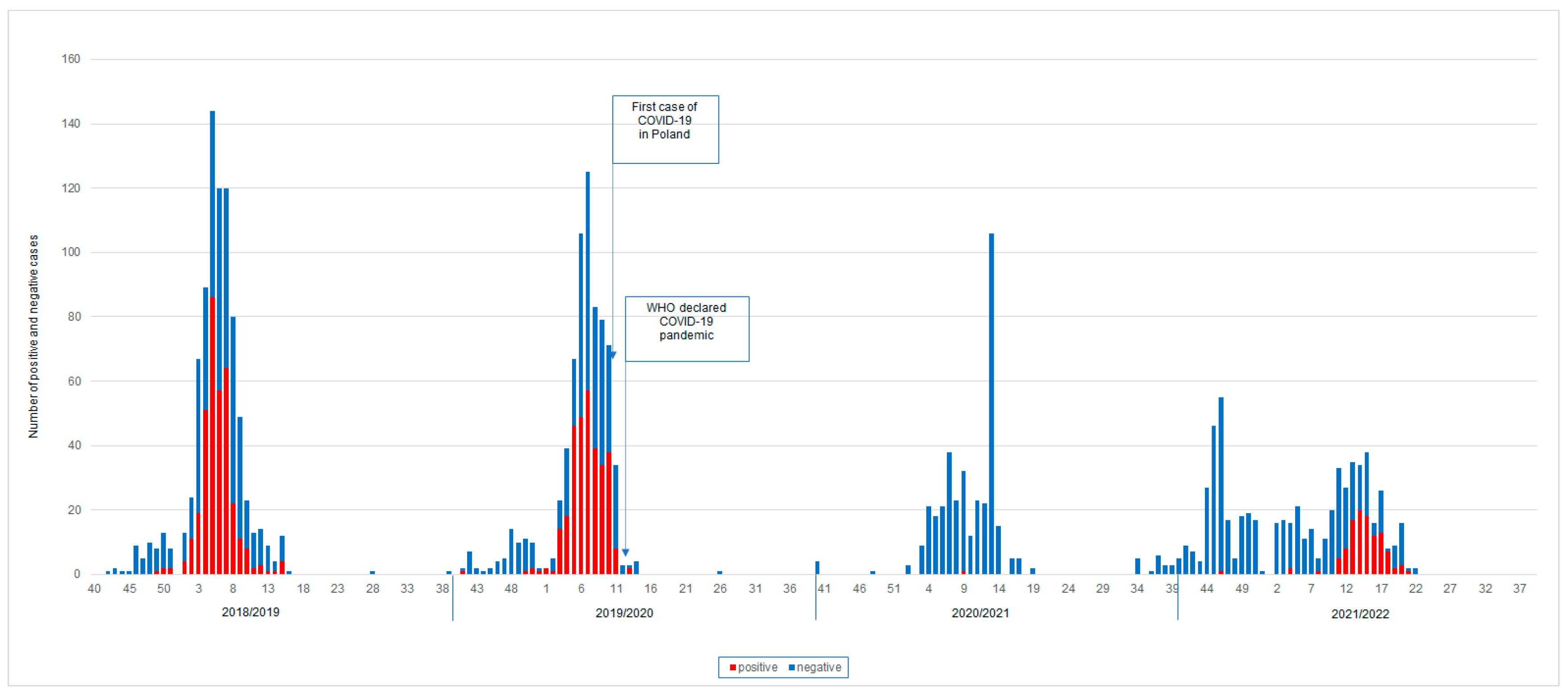
3. Results
3.1. Peak of Incidence
3.2. Percentage of Positive Samples
3.3. Predomination of Influenza Types and Subtypes
3.4. Averaged Data from Epidemic Seasons before and after Pandemics
3.5. Age Groups
3.6. Voivodships
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guo, G.; Ye, L.; Pan, K.; Chen, Y.; Xing, D.; Yan, K.; Chen, Z.; Ding, N.; Li, W.; Huang, H.; et al. New insights of emerging SARS-CoV-2: Epidemiology, etiology, clinical features, clinical treatment, and prevention. Front. Cell Dev. Biol. 2020, 8, 410. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 9 May 2020).
- Dhama, K.; Patel, S.K.; Kumar, R.; Masand, R.; Rana, J.; Yatoo, M.I.; Tiwari, R.; Sharun, K.; Mohapatra, R.K.; Natesan, S.; et al. The role of disinfectants and sanitizers during COVID-19 pandemic: Advantages and deleterious effects on humans and the environment. Environ. Sci. Pollut. Res. Int. 2021, 28, 34211–34228. [Google Scholar] [CrossRef] [PubMed]
- WHO. Influenza (Seasonal). 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 15 January 2023).
- Uyeki, T.M.; Hui, D.S.; Zambon, M.; Wentworth, D.E.; Monto, A.S. Influenza. Lancet 2022, 400, 693–706. [Google Scholar] [CrossRef] [PubMed]
- Brydak, L.B. Influenza, Pandemic Flu, Myth or Real Threat? Rhythm: Warsaw, Poland, 2008. (In Polish) [Google Scholar]
- Miyah, Y.; Benjelloun, M.; Lairini, S.; Lahrichi, A. COVID-19 impact on public health, environment, human psychology, global socioeconomy, and education. Sci. World J. 2022, 2022, 5578284. [Google Scholar] [CrossRef] [PubMed]
- Adlhoch, C.; Mook, P.; Lamb, F.; Ferland, L.; Melidou, A.; Amato-Gauci, A.J.; Pebody, R. European Influenza Surveillance Network. Very little influenza in the WHO European Region during the 2020/21 season, weeks 40 2020 to 8 2021. Euro Surveill. 2021, 26, 2100221. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Santisteve, P.; Ciancio, B.C.; Nicoll, A.; Lopalco, P.L. The importance of influenza prevention for public health. Hum. Vaccin. Immunother. 2012, 8, 89–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, M.L.; Dobkin, C.; Gorry, D. The Effect of Influenza Vaccination for the Elderly on Hospitalization and Mortality: An Observational Study with a Regression Discontinuity Design. Ann. Intern. Med. 2020, 172, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Brydak, L.B. Health and economic effects of influenza infections in terms of public health in Poland. In Pharmacoeconomics in the Management of Health Care Resources; Nowakowska, E., Ed.; Wolters Kluwer: Warsaw, Poland, 2018; pp. 274–283. (In Polish) [Google Scholar]
- Szczepienia.info. Available online: https://szczepienia.pzh.gov.pl/ (accessed on 10 November 2022).
- Bednarska, K.; Hallmann-Szelińska, E.; Kondratiuk, K.; Brydak, L.B. Influenza surveillance. Postepy Hig. Med. Dosw. 2016, 70, 313–318. [Google Scholar] [CrossRef] [PubMed]
- NIPH NIH–NRI. Case Definitions for Epidemiological Surveillance. 2022. Available online: http://wwwold.pzh.gov.pl/oldpage/epimeld/inne/Def_PL2_6b.pdf (accessed on 20 November 2022).
- Bednarska, K.; Hallmann-Szelińska, E.; Kondratiuk, K.; Rabczenko, D.; Brydak, L.B. Novelties in influenza surveillance in Poland. Probl. Hig. Epidemiol. 2016, 97, 101–105. [Google Scholar]
- Adlhoch, C.; Sneiderman, M.; Martinuka, O.; Melidou, A.; Bundle, N.; Fielding, J.; Olsen, S.J.; Penttinen, P.; Pastore, L.; Pebody, R. Spotlight influenza: The 2019/20 influenza season and the impact of COVID-19 on influenza surveillance in the WHO European Region. Eurosurveillance 2021, 26, 2100077. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.J.; Winn, A.K.; Budd, A.P.; Prill, M.M.; Steel, J.; Midgley, C.M.; Kniss, K.; Burns, E.; Rowe, T.; Foust, A.; et al. Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic—United States, 2020–2021. MMWR Morb. Mortal Wkly. Rep. 2021, 70, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Jones, N. How coronavirus lockdowns stopped flu in its tracks. Nature 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.E.; Park, S.W.; Yang, W.; Vecchi, G.A.; Metcalf, C.J.E.; Grenfell, B.T. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc. Natl. Acad. Sci. USA 2020, 117, 30547–30553. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-J.; Chen, T.-C.; Kuo, S.-H.; Hsieh, M.-H.; Chen, Y.-H. Severe complicated influenza declined during the prevention of COVID-19 in Taiwan. Infect. Control. Hosp. Epidemiol. 2021, 42, 499–501. [Google Scholar] [CrossRef] [PubMed]
- Lui, K.L.; Daher, N.; López, D.; Kim, V.; Tan, L.; Cohen, P.M.; Alismail, A. Surgical mask wearing behaviour in COVID-19 pandemic and influenza seasons: A cross-sectional study on healthcare professional students and staff’s perspective in Southern California. BMJ Open 2022, 12, e064677. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus: Information and Recommendations. Webside of the Republic of Poland. 2022. Available online: https://www.gov.pl/web/koronawirus/dystans-spoleczny-i-maseczki (accessed on 20 September 2022). (In Polish)
- Chow, E.J.; Uyeki, T.M.; Chu, H.Y. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat. Rev. Genet. 2022, 17, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Nott, R.; Fuller, T.L.; Brasil, P.; Nielsen-Saines, K. Out-of-Season Influenza during a COVID-19 Void in the State of Rio de Janeiro, Brazil: Temperature Matters. Vaccines 2022, 10, 821. [Google Scholar] [CrossRef] [PubMed]
- Dhanasekaran, V.; Sullivan, S.; Edwards, K.M.; Xie, R.; Khvorov, A.; Valkenburg, S.A.; Cowling, B.J.; Barr, I.G. Human seasonal influenza under COVID-19 and the potential consequences of influenza lineage elimination. Nat. Commun. 2022, 13, 1721. [Google Scholar] [CrossRef] [PubMed]
- Paget, J.; Caini, S.; Del Riccio, M.; van Waarden, W.; Meijer, A. Has influenza B/Yamagata become extinct and what implications might this have for quadrivalent influenza vaccines? Euro Surveill. 2022, 27, 2200753. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Seasonal Influenza 2018–2019; ECDC Annual Epidemiological Report for 2018; ECDC: Stockholm, Sweden, 2019. [Google Scholar]
- European Centre for Disease Prevention and Control. Seasonal Influenza 2019–2020; ECDC Annual Epidemiological Report for 2019; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- European Centre for Disease Prevention and Control. Seasonal Influenza; ECDC Annual Epidemiological Report 2020; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- European Centre for Disease Prevention and Control. Seasonal Influenza 2021–2022; ECDC Annual Epidemiological Report for 2021; ECDC: Stockholm, Sweden, 2022. [Google Scholar]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Łuniewska, K.; Szymański, K.; Kondratiuk, K.; Hallmann, E.; Brydak, L.B. The Impact of the COVID-19 Pandemic on Influenza Transmission in Poland. Microorganisms 2023, 11, 970. https://doi.org/10.3390/microorganisms11040970
Łuniewska K, Szymański K, Kondratiuk K, Hallmann E, Brydak LB. The Impact of the COVID-19 Pandemic on Influenza Transmission in Poland. Microorganisms. 2023; 11(4):970. https://doi.org/10.3390/microorganisms11040970
Chicago/Turabian StyleŁuniewska, Katarzyna, Karol Szymański, Katarzyna Kondratiuk, Ewelina Hallmann, and Lidia Bernadeta Brydak. 2023. "The Impact of the COVID-19 Pandemic on Influenza Transmission in Poland" Microorganisms 11, no. 4: 970. https://doi.org/10.3390/microorganisms11040970
APA StyleŁuniewska, K., Szymański, K., Kondratiuk, K., Hallmann, E., & Brydak, L. B. (2023). The Impact of the COVID-19 Pandemic on Influenza Transmission in Poland. Microorganisms, 11(4), 970. https://doi.org/10.3390/microorganisms11040970




