Gestational Viral Infections: Role of Host Immune System
Abstract
1. Introduction
2. Methods
3. DNA Viruses and Gestational Infection
3.1. Human Parvoviruses
3.2. Human Hepatitis Viruses
3.3. Human Papillomaviruses
3.4. Human Polyomaviruses
4. Human Herpesviruses
4.1. HSV-1 and HSV-2
4.2. CMV
4.3. HHV-6
4.4. VZV
5. RNA Viruses and Gestational Infection
5.1. Rubella Virus
5.2. Measles Virus
5.3. HIV
6. Emerging Viruses and Pregnancy
6.1. Dengue Virus
6.2. Zika Virus
6.3. West Nile Virus
6.4. SARS-CoV-2
7. Vaccines and Antiviral Therapy in Pregnancy
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mor, G.; Cardenas, I. The immune system in pregnancy: A unique complexity. Am. J. Reprod. Immunol. 2010, 63, 425–433. [Google Scholar] [CrossRef]
- PrabhuDas, M.; Bonney, E.; Caron, K.; Dey, S.; Erlebacher, A.; Fazleabas, A.; Fisher, S.; Golos, T.; Matzuk, M.; McCune, J.M.; et al. Immune mechanisms at the maternal-fetal interface: Perspectives and challenges. Nat. Immunol. 2015, 16, 328–334. [Google Scholar] [CrossRef]
- Ando, T.; Davies, T.F. Self-recognition and the role of fetal microchimerism. Best. Pract. Res. Clin. Endocrinol. Metab. 2004, 18, 197–211. [Google Scholar] [CrossRef]
- Hoo, R.; Nakimuli, A.; Vento-Tormo, R. Innate Immune Mechanisms to Protect Against Infection at the Human Decidual-Placental Interface. Front. Immunol. 2020, 11, 2070. [Google Scholar] [CrossRef]
- Simister, N.E. Placental transport of immunoglobulin G. Vaccine 2003, 21, 3365–3369. [Google Scholar] [CrossRef]
- Polanczyk, M.J.; Carson, B.D.; Subramanian, S.; Afentoulis, M.; Vandenbark, A.A.; Ziegler, S.F.; Offner, H. Cutting edge: Estrogen drives expansion of the CD4+CD25+ regulatory T cell compartment. J. Immunol. 2004, 173, 2227–2230. [Google Scholar] [CrossRef]
- Tai, P.; Wang, J.; Jin, H.; Song, X.; Yan, J.; Kang, Y.; Zhao, L.; An, X.; Du, X.; Chen, X.; et al. Induction of regulatory T cells by physiological level estrogen. J. Cell. Physiol. 2008, 214, 456–464. [Google Scholar] [CrossRef]
- Polanczyk, M.J.; Hopke, C.; Huan, J.; Vandenbark, A.A.; Offner, H. Enhanced FoxP3 expression and Treg cell function in pregnant and estrogen-treated mice. J. Neuroimmunol. 2005, 170, 85–92. [Google Scholar] [CrossRef]
- Areia, A.; Vale-Pereira, S.; Alves, V.; Rodrigues-Santos, P.; Moura, P.; Mota-Pinto, A. Membrane progesterone receptors in human regulatory T cells: A reality in pregnancy. BJOG 2015, 122, 1544–1550. [Google Scholar] [CrossRef]
- Tsuda, S.; Nakashima, A.; Shima, T.; Saito, S. New Paradigm in the Role of Regulatory T Cells During Pregnancy. Front. Immunol. 2019, 10, 573. [Google Scholar] [CrossRef]
- Schumacher, A.; Costa, S.D.; Zenclussen, A.C. Endocrine factors modulating immune responses in pregnancy. Front. Immunol. 2014, 5, 196. [Google Scholar] [CrossRef]
- Steinhoff, M.C.; Omer, S.B.; Roy, E.; Arifeen, S.E.; Raqib, R.; Altaye, M.; Breiman, R.F.; Zaman, K. Influenza immunization in pregnancy--antibody responses in mothers and infants. N. Engl. J. Med. 2010, 362, 1644–1646. [Google Scholar] [CrossRef]
- Watanabe, M.; Iwatani, Y.; Kaneda, T.; Hidaka, Y.; Mitsuda, N.; Morimoto, Y.; Amino, N. Changes in T, B, and NK lymphocyte subsets during and after normal pregnancy. Am. J. Reprod. Immunol. 1997, 37, 368–377. [Google Scholar] [CrossRef]
- Ander, S.E.; Diamond, M.S.; Coyne, C.B. Immune responses at the maternal-fetal interface. Sci. Immunol. 2019, 4, eaat6114. [Google Scholar] [CrossRef]
- Ferreira, L.M.R.; Meissner, T.B.; Tilburgs, T.; Strominger, J.L. HLA-G: At the Interface of Maternal-Fetal Tolerance. Trends Immunol. 2017, 38, 272–286. [Google Scholar] [CrossRef]
- Vento-Tormo, R.; Efremova, M.; Botting, R.A.; Turco, M.Y.; Vento-Tormo, M.; Meyer, K.B.; Park, J.E.; Stephenson, E.; Polanski, K.; Goncalves, A.; et al. Single-cell reconstruction of the early maternal-fetal interface in humans. Nature 2018, 563, 347–353. [Google Scholar] [CrossRef]
- Kraus, T.A.; Engel, S.M.; Sperling, R.S.; Kellerman, L.; Lo, Y.; Wallenstein, S.; Escribese, M.M.; Garrido, J.L.; Singh, T.; Loubeau, M.; et al. Characterizing the pregnancy immune phenotype: Results of the viral immunity and pregnancy (VIP) study. J. Clin. Immunol. 2012, 32, 300–311. [Google Scholar] [CrossRef]
- Luppi, P. How immune mechanisms are affected by pregnancy. Vaccine 2003, 21, 3352–3357. [Google Scholar] [CrossRef]
- Siewiera, J.; El Costa, H.; Tabiasco, J.; Berrebi, A.; Cartron, G.; Le Bouteiller, P.; Jabrane-Ferrat, N. Human cytomegalovirus infection elicits new decidual natural killer cell effector functions. PLoS Pathog. 2013, 9, e1003257. [Google Scholar] [CrossRef]
- Crespo, A.C.; Strominger, J.L.; Tilburgs, T. Expression of KIR2DS1 by decidual natural killer cells increases their ability to control placental HCMV infection. Proc. Natl. Acad. Sci. USA 2016, 113, 15072–15077. [Google Scholar] [CrossRef]
- van der Ploeg, K.; Chang, C.; Ivarsson, M.A.; Moffett, A.; Wills, M.R.; Trowsdale, J. Modulation of Human Leukocyte Antigen-C by Human Cytomegalovirus Stimulates KIR2DS1 Recognition by Natural Killer Cells. Front. Immunol. 2017, 8, 298. [Google Scholar] [CrossRef]
- Moore, A.G.; Brown, D.A.; Fairlie, W.D.; Bauskin, A.R.; Brown, P.K.; Munier, M.L.; Russell, P.K.; Salamonsen, L.A.; Wallace, E.M.; Breit, S.N. The transforming growth factor-ss superfamily cytokine macrophage inhibitory cytokine-1 is present in high concentrations in the serum of pregnant women. J. Clin. Endocrinol. Metab. 2000, 85, 4781–4788. [Google Scholar] [CrossRef]
- Enders, A.C.; King, B.F. The cytology of Hofbauer cells. Anat. Rec. 1970, 167, 231–236. [Google Scholar] [CrossRef]
- Castellucci, M.; Zaccheo, D.; Pescetto, G. A three-dimensional study of the normal human placental villous core. I. The Hofbauer cells. Cell. Tissue Res. 1980, 210, 235–247. [Google Scholar] [CrossRef]
- Wetzka, B.; Clark, D.E.; Charnock-Jones, D.S.; Zahradnik, H.P.; Smith, S.K. Isolation of macrophages (Hofbauer cells) from human term placenta and their prostaglandin E2 and thromboxane production. Hum. Reprod. 1997, 12, 847–852. [Google Scholar] [CrossRef]
- Quicke, K.M.; Bowen, J.R.; Johnson, E.L.; McDonald, C.E.; Ma, H.; O’Neal, J.T.; Rajakumar, A.; Wrammert, J.; Rimawi, B.H.; Pulendran, B.; et al. Zika Virus Infects Human Placental Macrophages. Cell. Host Microbe 2016, 20, 83–90. [Google Scholar] [CrossRef]
- de Noronha, L.; Zanluca, C.; Burger, M.; Suzukawa, A.A.; Azevedo, M.; Rebutini, P.Z.; Novadzki, I.M.; Tanabe, L.S.; Presibella, M.M.; Duarte Dos Santos, C.N. Zika Virus Infection at Different Pregnancy Stages: Anatomopathological Findings, Target Cells and Viral Persistence in Placental Tissues. Front. Microbiol. 2018, 9, 2266. [Google Scholar] [CrossRef]
- Bhatnagar, J.; Rabeneck, D.B.; Martines, R.B.; Reagan-Steiner, S.; Ermias, Y.; Estetter, L.B.; Suzuki, T.; Ritter, J.; Keating, M.K.; Hale, G.; et al. Zika Virus RNA Replication and Persistence in Brain and Placental Tissue. Emerg. Infect. Dis. 2017, 23, 405–414. [Google Scholar] [CrossRef]
- El Costa, H.; Gouilly, J.; Mansuy, J.M.; Chen, Q.; Levy, C.; Cartron, G.; Veas, F.; Al-Daccak, R.; Izopet, J.; Jabrane-Ferrat, N. ZIKA virus reveals broad tissue and cell tropism during the first trimester of pregnancy. Sci. Rep. 2016, 6, 35296. [Google Scholar] [CrossRef]
- Tabata, T.; Petitt, M.; Puerta-Guardo, H.; Michlmayr, D.; Wang, C.; Fang-Hoover, J.; Harris, E.; Pereira, L. Zika Virus Targets Different Primary Human Placental Cells, Suggesting Two Routes for Vertical Transmission. Cell. Host Microbe 2016, 20, 155–166. [Google Scholar] [CrossRef]
- Maidji, E.; Genbacev, O.; Chang, H.T.; Pereira, L. Developmental regulation of human cytomegalovirus receptors in cytotrophoblasts correlates with distinct replication sites in the placenta. J. Virol. 2007, 81, 4701–4712. [Google Scholar] [CrossRef]
- Simister, N.E.; Story, C.M.; Chen, H.L.; Hunt, J.S. An IgG-transporting Fc receptor expressed in the syncytiotrophoblast of human placenta. Eur. J. Immunol. 1996, 26, 1527–1531. [Google Scholar] [CrossRef]
- Rathore, A.P.S.; Saron, W.A.A.; Lim, T.; Jahan, N.; St John, A.L. Maternal immunity and antibodies to dengue virus promote infection and Zika virus-induced microcephaly in fetuses. Sci. Adv. 2019, 5, eaav3208. [Google Scholar] [CrossRef]
- Gupta, S.; Gach, J.S.; Becerra, J.C.; Phan, T.B.; Pudney, J.; Moldoveanu, Z.; Joseph, S.B.; Landucci, G.; Supnet, M.J.; Ping, L.H.; et al. The Neonatal Fc receptor (FcRn) enhances human immunodeficiency virus type 1 (HIV-1) transcytosis across epithelial cells. PLoS Pathog. 2013, 9, e1003776. [Google Scholar] [CrossRef]
- Pereira, L.; Maidji, E.; McDonagh, S.; Genbacev, O.; Fisher, S. Human cytomegalovirus transmission from the uterus to the placenta correlates with the presence of pathogenic bacteria and maternal immunity. J. Virol. 2003, 77, 13301–13314. [Google Scholar] [CrossRef]
- Zaga-Clavellina, V.; Diaz, L.; Olmos-Ortiz, A.; Godinez-Rubi, M.; Rojas-Mayorquin, A.E.; Ortuno-Sahagun, D. Central role of the placenta during viral infection: Immuno-competences and miRNA defensive responses. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 166182. [Google Scholar] [CrossRef]
- Goncalves, L.F.; Chaiworapongsa, T.; Romero, R. Intrauterine infection and prematurity. Ment. Retard. Dev. Disabil. Res. Rev. 2002, 8, 3–13. [Google Scholar] [CrossRef]
- Coyne, C.B. The Tree(s) of Life: The Human Placenta and My Journey to Learn More about It. PLoS Pathog. 2016, 12, e1005515. [Google Scholar] [CrossRef]
- Delorme-Axford, E.; Sadovsky, Y.; Coyne, C.B. The Placenta as a Barrier to Viral Infections. Annu. Rev. Virol. 2014, 1, 133–146. [Google Scholar] [CrossRef]
- Arora, N.; Sadovsky, Y.; Dermody, T.S.; Coyne, C.B. Microbial Vertical Transmission during Human Pregnancy. Cell. Host Microbe 2017, 21, 561–567. [Google Scholar] [CrossRef]
- Kourtis, A.P.; Read, J.S.; Jamieson, D.J. Pregnancy and infection. N. Engl. J. Med. 2014, 370, 2211–2218. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Nathan Mantel, W.H. Statistical Aspects of the Analysis of Data From Retrospective Studies of Disease. JNCI J. Natl. Cancer Inst. 1959, 22, 719–748. [Google Scholar] [CrossRef]
- Adams Waldorf, K.M.; McAdams, R.M. Influence of infection during pregnancy on fetal development. Reproduction 2013, 146, R151–R162. [Google Scholar] [CrossRef]
- Agrawal, V.; Hirsch, E. Intrauterine infection and preterm labor. Semin. Fetal Neonatal Med. 2012, 17, 12–19. [Google Scholar] [CrossRef]
- Fahey, J.O. Clinical management of intra-amniotic infection and chorioamnionitis: A review of the literature. J. Midwifery Womens Health 2008, 53, 227–235. [Google Scholar] [CrossRef]
- Xu, X.; Zhou, Y.; Wei, H. Roles of HLA-G in the Maternal-Fetal Immune Microenvironment. Front. Immunol. 2020, 11, 592010. [Google Scholar] [CrossRef]
- Jasinski-Bergner, S.; Schmiedel, D.; Mandelboim, O.; Seliger, B. Role of HLA-G in Viral Infections. Front. Immunol. 2022, 13, 826074. [Google Scholar] [CrossRef]
- Rai, K.R.; Shrestha, P.; Yang, B.; Chen, Y.; Liu, S.; Maarouf, M.; Chen, J.L. Acute Infection of Viral Pathogens and Their Innate Immune Escape. Front. Microbiol. 2021, 12, 672026. [Google Scholar] [CrossRef]
- Monette, A.; Mouland, A.J. T Lymphocytes as Measurable Targets of Protection and Vaccination Against Viral Disorders. Int. Rev. Cell. Mol. Biol. 2019, 342, 175–263. [Google Scholar] [CrossRef]
- Finlay, B.B.; McFadden, G. Anti-immunology: Evasion of the host immune system by bacterial and viral pathogens. Cell 2006, 124, 767–782. [Google Scholar] [CrossRef] [PubMed]
- Gregori, S.; Amodio, G.; Quattrone, F.; Panina-Bordignon, P. HLA-G Orchestrates the Early Interaction of Human Trophoblasts with the Maternal Niche. Front. Immunol. 2015, 6, 128. [Google Scholar] [CrossRef]
- Rizzo, R.; D’Accolti, M.; Bortolotti, D.; Caccuri, F.; Caruso, A.; Di Luca, D.; Caselli, E. Human Herpesvirus 6A and 6B inhibit in vitro angiogenesis by induction of Human Leukocyte Antigen, G. Sci. Rep. 2018, 8, 17683. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, P.; Naik, S.; Agrawal, S. Role of HLA-G, HLA-E and KIR2DL4 in Pregnancy. Int. J. Hum. Genet. 2017, 7, 219–233. [Google Scholar] [CrossRef]
- Houchins, J.P.; Lanier, L.L.; Niemi, E.C.; Phillips, J.H.; Ryan, J.C. Natural killer cell cytolytic activity is inhibited by NKG2-A and activated by NKG2-C. J. Immunol. 1997, 158, 3603–3609. [Google Scholar] [CrossRef] [PubMed]
- Apps, R.; Gardner, L.; Hiby, S.E.; Sharkey, A.M.; Moffett, A. Conformation of human leucocyte antigen-C molecules at the surface of human trophoblast cells. Immunology 2008, 124, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, A.M.; Gardner, L.; Hiby, S.; Farrell, L.; Apps, R.; Masters, L.; Goodridge, J.; Lathbury, L.; Stewart, C.A.; Verma, S.; et al. Killer Ig-like receptor expression in uterine NK cells is biased toward recognition of HLA-C and alters with gestational age. J. Immunol. 2008, 181, 39–46. [Google Scholar] [CrossRef]
- Moffett, A.; Loke, C. Immunology of placentation in eutherian mammals. Nat. Rev. Immunol. 2006, 6, 584–594. [Google Scholar] [CrossRef]
- Seliger, B.; Ritz, U.; Ferrone, S. Molecular mechanisms of HLA class I antigen abnormalities following viral infection and transformation. Int. J. Cancer 2006, 118, 129–138. [Google Scholar] [CrossRef]
- Caselli, E.; Campioni, D.; Cavazzini, F.; Gentili, V.; Bortolotti, D.; Cuneo, A.; Di Luca, D.; Rizzo, R. Acute human herpesvirus-6A infection of human mesothelial cells modulates HLA molecules. Arch. Virol. 2015, 160, 2141–2149. [Google Scholar] [CrossRef]
- Davis, Z.B.; Cogswell, A.; Scott, H.; Mertsching, A.; Boucau, J.; Wambua, D.; Le Gall, S.; Planelles, V.; Campbell, K.S.; Barker, E. A Conserved HIV-1-Derived Peptide Presented by HLA-E Renders Infected T-cells Highly Susceptible to Attack by NKG2A/CD94-Bearing Natural Killer Cells. PLoS Pathog. 2016, 12, e1005421. [Google Scholar] [CrossRef] [PubMed]
- Llano, M.; Guma, M.; Ortega, M.; Angulo, A.; Lopez-Botet, M. Differential effects of US2, US6 and US11 human cytomegalovirus proteins on HLA class Ia and HLA-E expression: Impact on target susceptibility to NK cell subsets. Eur. J. Immunol. 2003, 33, 2744–2754. [Google Scholar] [CrossRef]
- Rizzo, R.; Trentini, A.; Bortolotti, D.; Manfrinato, M.C.; Rotola, A.; Castellazzi, M.; Melchiorri, L.; Di Luca, D.; Dallocchio, F.; Fainardi, E.; et al. Matrix metalloproteinase-2 (MMP-2) generates soluble HLA-G1 by cell surface proteolytic shedding. Mol. Cell. Biochem. 2013, 381, 243–255. [Google Scholar] [CrossRef]
- Nattermann, J.; Feldmann, G.; Ahlenstiel, G.; Langhans, B.; Sauerbruch, T.; Spengler, U. Surface expression and cytolytic function of natural killer cell receptors is altered in chronic hepatitis C. Gut 2006, 55, 869–877. [Google Scholar] [CrossRef]
- Goncalves, M.A.; Le Discorde, M.; Simoes, R.T.; Rabreau, M.; Soares, E.G.; Donadi, E.A.; Carosella, E.D. Classical and non-classical HLA molecules and p16(INK4a) expression in precursors lesions and invasive cervical cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 141, 70–74. [Google Scholar] [CrossRef]
- Mogensen, T.H. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin. Microbiol. Rev. 2009, 22, 240–273. [Google Scholar] [CrossRef]
- Chan, Y.K.; Gack, M.U. Viral evasion of intracellular DNA and RNA sensing. Nat. Rev. Microbiol. 2016, 14, 360–373. [Google Scholar] [CrossRef]
- Wies, E.; Wang, M.K.; Maharaj, N.P.; Chen, K.; Zhou, S.; Finberg, R.W.; Gack, M.U. Dephosphorylation of the RNA sensors RIG-I and MDA5 by the phosphatase PP1 is essential for innate immune signaling. Immunity 2013, 38, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, O.; Akira, S. Pattern recognition receptors and inflammation. Cell 2010, 140, 805–820. [Google Scholar] [CrossRef] [PubMed]
- Tamura, K.; Ishikawa, G.; Yoshie, M.; Ohneda, W.; Nakai, A.; Takeshita, T.; Tachikawa, E. Glibenclamide inhibits NLRP3 inflammasome-mediated IL-1beta secretion in human trophoblasts. J. Pharmacol. Sci. 2017, 135, 89–95. [Google Scholar] [CrossRef]
- Kim, Y.M.; Romero, R.; Oh, S.Y.; Kim, C.J.; Kilburn, B.A.; Armant, D.R.; Nien, J.K.; Gomez, R.; Mazor, M.; Saito, S.; et al. Toll-like receptor 4: A potential link between "danger signals," the innate immune system, and preeclampsia? Am. J. Obstet. Gynecol. 2005, 193, 921–927. [Google Scholar] [CrossRef]
- Koga, K.; Cardenas, I.; Aldo, P.; Abrahams, V.M.; Peng, B.; Fill, S.; Romero, R.; Mor, G. Activation of TLR3 in the trophoblast is associated with preterm delivery. Am. J. Reprod. Immunol. 2009, 61, 196–212. [Google Scholar] [CrossRef]
- Romero, R.; Kusanovic, J.P.; Chaiworapongsa, T.; Hassan, S.S. Placental bed disorders in preterm labor, preterm PROM, spontaneous abortion and abruptio placentae. Best Pr. Res. Clin. Obstet. Gynaecol. 2011, 25, 313–327. [Google Scholar] [CrossRef]
- Motomura, K.; Hara, M.; Ito, I.; Morita, H.; Matsumoto, K. Roles of human trophoblasts’ pattern recognition receptors in host defense and pregnancy complications. J. Reprod. Immunol. 2023, 156, 103811. [Google Scholar] [CrossRef] [PubMed]
- Amiot, L.; Vu, N.; Samson, M. Immunomodulatory properties of HLA-G in infectious diseases. J. Immunol. Res. 2014, 2014, 298569. [Google Scholar] [CrossRef] [PubMed]
- Estes, M.K. Fields Virology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; p. 1347. [Google Scholar]
- Ornoy, A.; Ergaz, Z. Parvovirus B19 infection during pregnancy and risks to the fetus. Birth Defects Res. 2017, 109, 311–323. [Google Scholar] [CrossRef]
- de Jong, E.P.; Walther, F.J.; Kroes, A.C.; Oepkes, D. Parvovirus B19 infection in pregnancy: New insights and management. Prenat. Diagn. 2011, 31, 419–425. [Google Scholar] [CrossRef]
- De Jong, E.P.; Lindenburg, I.T.; van Klink, J.M.; Oepkes, D.; van Kamp, I.L.; Walther, F.J.; Lopriore, E. Intrauterine transfusion for parvovirus B19 infection: Long-term neurodevelopmental outcome. Am. J. Obstet. Gynecol. 2012, 206, 204.e1–204.e5. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.G.; Pegado, C.S.; Cubel Rde, C.; Fonseca, M.E.; Sloboda, I.; Nascimento, J.P. Feto-placentary pathology in human parvovirus B19 infection. Rev. Inst. Med. Trop. Sao Paulo 1998, 40, 145–150. [Google Scholar] [CrossRef]
- Jordan, J.A.; Huff, D.; DeLoia, J.A. Placental cellular immune response in women infected with human parvovirus B19 during pregnancy. Clin. Diagn. Lab. Immunol. 2001, 8, 288–292. [Google Scholar] [CrossRef]
- Arechavaleta-Velasco, F.; Gomez, L.; Ma, Y.; Zhao, J.; McGrath, C.M.; Sammel, M.D.; Nelson, D.B.; Parry, S. Adverse reproductive outcomes in urban women with adeno-associated virus-2 infections in early pregnancy. Hum. Reprod. 2008, 23, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Koi, H.; Zhang, J.; Makrigiannakis, A.; Getsios, S.; MacCalman, C.D.; Kopf, G.S.; Strauss, J.F., 3rd; Parry, S. Differential expression of the coxsackievirus and adenovirus receptor regulates adenovirus infection of the placenta. Biol. Reprod. 2001, 64, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Arechavaleta-Velasco, F.; Ma, Y.; Zhang, J.; McGrath, C.M.; Parry, S. Adeno-associated virus-2 (AAV-2) causes trophoblast dysfunction, and placental AAV-2 infection is associated with preeclampsia. Am. J. Pathol. 2006, 168, 1951–1959. [Google Scholar] [CrossRef]
- Arechavaleta-Velasco, F.; Koi, H.; Strauss, J.F., 3rd; Parry, S. Viral infection of the trophoblast: Time to take a serious look at its role in abnormal implantation and placentation? J. Reprod. Immunol. 2002, 55, 113–121. [Google Scholar] [CrossRef]
- Tobiasch, E.; Rabreau, M.; Geletneky, K.; Larue-Charlus, S.; Severin, F.; Becker, N.; Schlehofer, J.R. Detection of adeno-associated virus DNA in human genital tissue and in material from spontaneous abortion. J. Med. Virol. 1994, 44, 215–222. [Google Scholar] [CrossRef]
- Botquin, V.; Cid-Arregui, A.; Schlehofer, J.R. Adeno-associated virus type 2 interferes with early development of mouse embryos. J. Gen. Virol. 1994, 75 Pt 10, 2655–2662. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.W.; Lao, T.T. Hepatitis B—Vertical transmission and the prevention of mother-to-child transmission. Best. Pract. Res. Clin. Obstet. Gynaecol. 2020, 68, 78–88. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, S.; Liu, M.; Wang, Q.; Shen, H.; Zhang, Y. Maternal pre-pregnancy infection with hepatitis B virus and the risk of preterm birth: A population-based cohort study. Lancet Glob. Health 2017, 5, e624–e632. [Google Scholar] [CrossRef]
- Tian, T.; Sun, D.; Wang, P.; Wang, H.; Bai, X.; Yang, X.; Wang, Z.; Dong, M. Roles of Toll-like Receptor 7 and 8 in Prevention of Intrauterine Transmission of Hepatitis B Virus. Cell. Physiol. Biochem. 2015, 37, 445–453. [Google Scholar] [CrossRef]
- Cui, H.; Li, Q.L.; Chen, J.; Na, Q.; Liu, C.X. Hepatitis B virus X protein modifies invasion, proliferation and the inflammatory response in an HTR-8/SVneo cell model. Oncol. Rep. 2015, 34, 2090–2098. [Google Scholar] [CrossRef]
- Giugliano, S.; Petroff, M.G.; Warren, B.D.; Jasti, S.; Linscheid, C.; Ward, A.; Kramer, A.; Dobrinskikh, E.; Sheiko, M.A.; Gale, M., Jr.; et al. Hepatitis C Virus Sensing by Human Trophoblasts Induces Innate Immune Responses and Recruitment of Maternal NK Cells: Potential Implications for Limiting Vertical Transmission. J. Immunol. 2015, 195, 3737–3747. [Google Scholar] [CrossRef] [PubMed]
- Kushner, T.; Terrault, N.A. Hepatitis C in Pregnancy: A Unique Opportunity to Improve the Hepatitis C Cascade of Care. Hepatol. Commun. 2019, 3, 20–28. [Google Scholar] [CrossRef]
- Rusyn, I.; Lemon, S.M. Mechanisms of HCV-induced liver cancer: What did we learn from in vitro and animal studies? Cancer Lett. 2014, 345, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Khakoo, S.I.; Thio, C.L.; Martin, M.P.; Brooks, C.R.; Gao, X.; Astemborski, J.; Cheng, J.; Goedert, J.J.; Vlahov, D.; Hilgartner, M.; et al. HLA and NK cell inhibitory receptor genes in resolving hepatitis C virus infection. Science 2004, 305, 872–874. [Google Scholar] [CrossRef]
- Hurtado, C.W.; Golden-Mason, L.; Brocato, M.; Krull, M.; Narkewicz, M.R.; Rosen, H.R. Innate immune function in placenta and cord blood of hepatitis C--seropositive mother-infant dyads. PLoS ONE 2010, 5, e12232. [Google Scholar] [CrossRef]
- Wu, C.; Wu, X.; Xia, J. Hepatitis E virus infection during pregnancy. Virol. J. 2020, 17, 73. [Google Scholar] [CrossRef] [PubMed]
- Bose, P.D.; Das, B.C.; Kumar, A.; Gondal, R.; Kumar, D.; Kar, P. High viral load and deregulation of the progesterone receptor signaling pathway: Association with hepatitis E-related poor pregnancy outcome. J. Hepatol. 2011, 54, 1107–1113. [Google Scholar] [CrossRef]
- Yang, C.; Hao, X.; Li, Y.; Long, F.; He, Q.; Huang, F.; Yu, W. Successful Establishment of Hepatitis E Virus Infection in Pregnant BALB/c Mice. Viruses 2019, 11, 451. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.C.; Mariz, F.C.; Silva, M.A.; Jesus, A.L. Human papillomavirus vertical transmission: Review of current data. Clin. Infect. Dis. 2013, 56, 1451–1456. [Google Scholar] [CrossRef]
- Racicot, K.; Mor, G. Risks associated with viral infections during pregnancy. J. Clin. Investig. 2017, 127, 1591–1599. [Google Scholar] [CrossRef]
- Gomez, L.M.; Ma, Y.; Ho, C.; McGrath, C.M.; Nelson, D.B.; Parry, S. Placental infection with human papillomavirus is associated with spontaneous preterm delivery. Hum. Reprod. 2008, 23, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Slatter, T.L.; Hung, N.G.; Clow, W.M.; Royds, J.A.; Devenish, C.J.; Hung, N.A. A clinicopathological study of episomal papillomavirus infection of the human placenta and pregnancy complications. Mod. Pathol. 2015, 28, 1369–1382. [Google Scholar] [CrossRef] [PubMed]
- Palefsky, J.M.; Gillison, M.L.; Strickler, H.D. Chapter 16: HPV vaccines in immunocompromised women and men. Vaccine 2006, 24 (Suppl. S3), S3/140-146. [Google Scholar] [CrossRef]
- Moodley, M.; Moodley, J.; Chetty, R.; Herrington, C.S. The role of steroid contraceptive hormones in the pathogenesis of invasive cervical cancer: A review. Int. J. Gynecol. Cancer 2003, 13, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Linthorst, J.; Welkers, M.R.A.; Sistermans, E.A. Clinically relevant DNA viruses in pregnancy. Prenat. Diagn. 2023, 43, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Gibson, P.E.; Booth, J.C.; Clewley, J.P. Genomic typing of BK virus in clinical specimens by direct sequencing of polymerase chain reaction products. J. Med. Virol. 1993, 41, 11–17. [Google Scholar] [CrossRef]
- Markowitz, R.B.; Eaton, B.A.; Kubik, M.F.; Latorra, D.; McGregor, J.A.; Dynan, W.S. BK virus and JC virus shed during pregnancy have predominantly archetypal regulatory regions. J. Virol. 1991, 65, 4515–4519. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; Chakraborty, T. High reactivation of BK virus variants in Asian Indians with renal disorders and during pregnancy. Virus Genes. 2004, 28, 157–168. [Google Scholar] [CrossRef]
- Cheungpasitporn, W.; Thongprayoon, C.; Craici, I.M.; Sharma, K.; Chesdachai, S.; Khoury, N.J.; Ettore, A.S. Reactivation of BK polyomavirus during pregnancy, vertical transmission, and clinical significance: A meta-analysis. J. Clin. Virol. 2018, 102, 56–62. [Google Scholar] [CrossRef]
- Boldorini, R.; Allegrini, S.; Miglio, U.; Paganotti, A.; Cocca, N.; Zaffaroni, M.; Riboni, F.; Monga, G.; Viscidi, R. Serological evidence of vertical transmission of JC and BK polyomaviruses in humans. J. Gen. Virol. 2011, 92, 1044–1050. [Google Scholar] [CrossRef]
- Coleman, D.V.; Gardner, S.D.; Mulholland, C.; Fridiksdottir, V.; Porter, A.A.; Lilford, R.; Valdimarsson, H. Human polyomavirus in pregnancy. A model for the study of defence mechanisms to virus reactivation. Clin. Exp. Immunol. 1983, 53, 289–296. [Google Scholar] [PubMed]
- Cohen, J.I. Herpesvirus latency. J. Clin. Investig. 2020, 130, 3361–3369. [Google Scholar] [CrossRef]
- Enright, A.M.; Prober, C.G. Neonatal herpes infection: Diagnosis, treatment and prevention. Semin. Neonatol. 2002, 7, 283–291. [Google Scholar] [CrossRef]
- Kriebs, J.M. Understanding herpes simplex virus: Transmission, diagnosis, and considerations in pregnancy management. J. Midwifery Womens Health 2008, 53, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Dinc, B.; Bozdayi, G.; Biri, A.; Kalkanci, A.; Dogan, B.; Bozkurt, N.; Rota, S. Molecular detection of cytomegalovirus, herpes simplex virus 2, human papillomavirus 16-18 in Turkish pregnants. Braz. J. Infect. Dis. 2010, 14, 569–574. [Google Scholar] [CrossRef]
- Brown, Z.A.; Wald, A.; Morrow, R.A.; Selke, S.; Zeh, J.; Corey, L. Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant. JAMA 2003, 289, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Brown, Z.A.; Gardella, C.; Wald, A.; Morrow, R.; Corey, L. Genital Herpes Complicating Pregnancy. Obstet. Gynecol. 2006, 107, 426. [Google Scholar] [CrossRef]
- Brown, Z.A.; Benedetti, J.; Selke, S.; Ashley, R.; Watts, D.H.; Corey, L. Asymptomatic maternal shedding of herpes simplex virus at the onset of labor: Relationship to preterm labor. Obstet. Gynecol. 1996, 87, 483–488. [Google Scholar] [CrossRef]
- Schust, D.J.; Hill, A.B.; Ploegh, H.L. Herpes simplex virus blocks intracellular transport of HLA-G in placentally derived human cells. J. Immunol. 1996, 157, 3375–3380. [Google Scholar] [CrossRef]
- Norskov-Lauritsen, N.; Aboagye-Mathisen, G.; Juhl, C.B.; Petersen, P.M.; Zachar, V.; Ebbesen, P. Herpes simplex virus infection of cultured human term trophoblast. J. Med. Virol. 1992, 36, 162–166. [Google Scholar] [CrossRef]
- Robb, J.A.; Benirschke, K.; Barmeyer, R. Intrauterine latent herpes simplex virus infection: I. Spontaneous abortion. Hum. Pathol. 1986, 17, 1196–1209. [Google Scholar] [CrossRef] [PubMed]
- Brown, Z.A.; Vontver, L.A.; Benedetti, J.; Critchlow, C.W.; Sells, C.J.; Berry, S.; Corey, L. Effects on infants of a first episode of genital herpes during pregnancy. N. Engl. J. Med. 1987, 317, 1246–1251. [Google Scholar] [CrossRef]
- Jabłońska, A.; Studzińska, M.; Suski, P.; Kalinka, J.; Paradowska, E. Enhanced expression of IFI16 and RIG-I in human third-trimester placentas following HSV-1 infection. Clin. Exp. Immunol. 2018, 193, 255–263. [Google Scholar] [CrossRef]
- Leruez-Ville, M.; Foulon, I.; Pass, R.; Ville, Y. Cytomegalovirus infection during pregnancy: State of the science. Am. J. Obstet. Gynecol. 2020, 223, 330–349. [Google Scholar] [CrossRef]
- Lycke, E.; Norrby, S.R. HerpesVirus Infections: State of the Art. Scand. J. Infect. Dis. 2015, 23, 1–118. [Google Scholar] [CrossRef]
- Kenneson, A.; Cannon, M.J. Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev. Med. Virol. 2007, 17, 253–276. [Google Scholar] [CrossRef] [PubMed]
- Fowler, K.B.; Stagno, S.; Pass, R.F.; Britt, W.J.; Boll, T.J.; Alford, C.A. The outcome of congenital cytomegalovirus infection in relation to maternal antibody status. N. Engl. J. Med. 1992, 326, 663–667. [Google Scholar] [CrossRef]
- de Vries, J.J.; van Zwet, E.W.; Dekker, F.W.; Kroes, A.C.; Verkerk, P.H.; Vossen, A.C. The apparent paradox of maternal seropositivity as a risk factor for congenital cytomegalovirus infection: A population-based prediction model. Rev. Med. Virol. 2013, 23, 241–249. [Google Scholar] [CrossRef]
- Amsler, L.; Verweij, M.; DeFilippis, V.R. The tiers and dimensions of evasion of the type I interferon response by human cytomegalovirus. J. Mol. Biol. 2013, 425, 4857–4871. [Google Scholar] [CrossRef]
- Botto, S.; Abraham, J.; Mizuno, N.; Pryke, K.; Gall, B.; Landais, I.; Streblow, D.N.; Fruh, K.J.; DeFilippis, V.R. Human Cytomegalovirus Immediate Early 86-kDa Protein Blocks Transcription and Induces Degradation of the Immature Interleukin-1beta Protein during Virion-Mediated Activation of the AIM2 Inflammasome. mBio 2019, 10, e02510-18. [Google Scholar] [CrossRef]
- Zou, H.M.; Huang, Z.F.; Yang, Y.; Luo, W.W.; Wang, S.Y.; Luo, M.H.; Fu, Y.Z.; Wang, Y.Y. Human Cytomegalovirus Protein UL94 Targets MITA to Evade the Antiviral Immune Response. J. Virol. 2020, 94, e00022-20. [Google Scholar] [CrossRef]
- Fu, Y.Z.; Su, S.; Zou, H.M.; Guo, Y.; Wang, S.Y.; Li, S.; Luo, M.H.; Wang, Y.Y. Human Cytomegalovirus DNA Polymerase Subunit UL44 Antagonizes Antiviral Immune Responses by Suppressing IRF3- and NF-kappaB-Mediated Transcription. J. Virol. 2019, 93, e00181-19. [Google Scholar] [CrossRef] [PubMed]
- Chan, G.; Guilbert, L.J. Ultraviolet-inactivated human cytomegalovirus induces placental syncytiotrophoblast apoptosis in a Toll-like receptor-2 and tumour necrosis factor-alpha dependent manner. J. Pathol. 2006, 210, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, S.; Lowen, B.; Chan, G.; Davey, A.; Riddell, M.; Guilbert, L.J. Human cytomegalovirus interacts with toll-like receptor 2 and CD14 on syncytiotrophoblasts to stimulate expression of TNFalpha mRNA and apoptosis. Placenta 2009, 30, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Jablonska, A.; Swierzko, A.S.; Studzinska, M.; Suski, P.; Kalinka, J.; Lesnikowski, Z.J.; Cedzynski, M.; Paradowska, E. Insight into the expression of RIG-I-like receptors in human third trimester placentas following ex vivo cytomegalovirus or vesicular stomatitis virus infection. Mol. Immunol. 2020, 126, 143–152. [Google Scholar] [CrossRef]
- Lin, A.; Xu, H.; Yan, W. Modulation of HLA expression in human cytomegalovirus immune evasion. Cell. Mol. Immunol. 2007, 4, 91–98. [Google Scholar]
- Rizzo, R.; Vercammen, M.; van de Velde, H.; Horn, P.A.; Rebmann, V. The importance of HLA-G expression in embryos, trophoblast cells, and embryonic stem cells. Cell. Mol. Life Sci. 2011, 68, 341–352. [Google Scholar] [CrossRef]
- Rizzo, R.; Andersen, A.S.; Lassen, M.R.; Sorensen, H.C.; Bergholt, T.; Larsen, M.H.; Melchiorri, L.; Stignani, M.; Baricordi, O.R.; Hviid, T.V. Soluble human leukocyte antigen-G isoforms in maternal plasma in early and late pregnancy. Am. J. Reprod. Immunol. 2009, 62, 320–338. [Google Scholar] [CrossRef]
- Jun, Y.; Kim, E.; Jin, M.; Sung, H.C.; Han, H.; Geraghty, D.E.; Ahn, K. Human cytomegalovirus gene products US3 and US6 down-regulate trophoblast class I MHC molecules. J. Immunol. 2000, 164, 805–811. [Google Scholar] [CrossRef]
- Onno, M.; Pangault, C.; Le Friec, G.; Guilloux, V.; Andre, P.; Fauchet, R. Modulation of HLA-G antigens expression by human cytomegalovirus: Specific induction in activated macrophages harboring human cytomegalovirus infection. J. Immunol. 2000, 164, 6426–6434. [Google Scholar] [CrossRef]
- Park, B.; Spooner, E.; Houser, B.L.; Strominger, J.L.; Ploegh, H.L. The HCMV membrane glycoprotein US10 selectively targets HLA-G for degradation. J. Exp. Med. 2010, 207, 2033–2041. [Google Scholar] [CrossRef]
- Barel, M.T.; Ressing, M.; Pizzato, N.; van Leeuwen, D.; Le Bouteiller, P.; Lenfant, F.; Wiertz, E.J. Human cytomegalovirus-encoded US2 differentially affects surface expression of MHC class I locus products and targets membrane-bound, but not soluble HLA-G1 for degradation. J. Immunol. 2003, 171, 6757–6765. [Google Scholar] [CrossRef]
- Schust, D.J.; Tortorella, D.; Seebach, J.; Phan, C.; Ploegh, H.L. Trophoblast class I major histocompatibility complex (MHC) products are resistant to rapid degradation imposed by the human cytomegalovirus (HCMV) gene products US2 and US11. J. Exp. Med. 1998, 188, 497–503. [Google Scholar] [CrossRef]
- Crespo, A.C.; van der Zwan, A.; Ramalho-Santos, J.; Strominger, J.L.; Tilburgs, T. Cytotoxic potential of decidual NK cells and CD8+ T cells awakened by infections. J. Reprod. Immunol. 2017, 119, 85–90. [Google Scholar] [CrossRef]
- Yan, W.H.; Lin, A.; Chen, B.G.; Zhou, M.Y.; Dai, M.Z.; Chen, X.J.; Gan, L.H.; Zhu, M.; Shi, W.W.; Li, B.L. Possible roles of KIR2DL4 expression on uNK cells in human pregnancy. Am. J. Reprod. Immunol. 2007, 57, 233–242. [Google Scholar] [CrossRef]
- Beziat, V.; Hilton, H.G.; Norman, P.J.; Traherne, J.A. Deciphering the killer-cell immunoglobulin-like receptor system at super-resolution for natural killer and T-cell biology. Immunology 2017, 150, 248–264. [Google Scholar] [CrossRef]
- Tanaka, K.; Yamada, H.; Minami, M.; Kataoka, S.; Numazaki, K.; Minakami, H.; Tsutsumi, H. Screening for vaginal shedding of cytomegalovirus in healthy pregnant women using real-time PCR: Correlation of CMV in the vagina and adverse outcome of pregnancy. J. Med. Virol. 2006, 78, 757–759. [Google Scholar] [CrossRef]
- Salvany-Celades, M.; van der Zwan, A.; Benner, M.; Setrajcic-Dragos, V.; Bougleux Gomes, H.A.; Iyer, V.; Norwitz, E.R.; Strominger, J.L.; Tilburgs, T. Three Types of Functional Regulatory T Cells Control T Cell Responses at the Human Maternal-Fetal Interface. Cell. Rep. 2019, 27, 2537–2547 e2535. [Google Scholar] [CrossRef]
- Lissauer, D.; Choudhary, M.; Pachnio, A.; Goodyear, O.; Moss, P.A.; Kilby, M.D. Cytomegalovirus sero positivity dramatically alters the maternal CD8+ T cell repertoire and leads to the accumulation of highly differentiated memory cells during human pregnancy. Hum. Reprod. 2011, 26, 3355–3365. [Google Scholar] [CrossRef]
- Ameres, S.; Mautner, J.; Schlott, F.; Neuenhahn, M.; Busch, D.H.; Plachter, B.; Moosmann, A. Presentation of an immunodominant immediate-early CD8+ T cell epitope resists human cytomegalovirus immunoevasion. PLoS Pathog. 2013, 9, e1003383. [Google Scholar] [CrossRef]
- van Egmond, A.; van der Keur, C.; Swings, G.M.; Scherjon, S.A.; Claas, F.H. The possible role of virus-specific CD8(+) memory T cells in decidual tissue. J. Reprod. Immunol. 2016, 113, 1–8. [Google Scholar] [CrossRef]
- Liu, W.; Niu, Z.; Li, Q.; Pang, R.T.; Chiu, P.C.; Yeung, W.S. MicroRNA and Embryo Implantation. Am. J. Reprod. Immunol. 2016, 75, 263–271. [Google Scholar] [CrossRef]
- Cai, M.; Kolluru, G.K.; Ahmed, A. Small Molecule, Big Prospects: MicroRNA in Pregnancy and Its Complications. J. Pregnancy 2017, 2017, 6972732. [Google Scholar] [CrossRef]
- Bortolotti, D.; Gentili, V.; Santi, E.; Taliento, C.; Vitagliano, A.; Schiuma, G.; Beltrami, S.; Rizzo, S.; Lanza, G.; Rizzo, R.; et al. Late-onset intrauterine growth restriction and HHV-6 infection: A pilot study. J. Med. Virol. 2021, 93, 6317–6322. [Google Scholar] [CrossRef] [PubMed]
- Ablashi, D.; Agut, H.; Alvarez-Lafuente, R.; Clark, D.A.; Dewhurst, S.; DiLuca, D.; Flamand, L.; Frenkel, N.; Gallo, R.; Gompels, U.A.; et al. Classification of HHV-6A and HHV-6B as distinct viruses. Arch. Virol. 2014, 159, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Eliassen, E.; Marci, R.; Di Luca, D.; Rizzo, R. The use of heparin in infertility and recurrent pregnancy loss: Are its antiviral properties at play? Med. Hypotheses 2017, 102, 41–47. [Google Scholar] [CrossRef]
- De Bolle, L.; Naesens, L.; De Clercq, E. Update on human herpesvirus 6 biology, clinical features, and therapy. Clin. Microbiol. Rev. 2005, 18, 217–245. [Google Scholar] [CrossRef] [PubMed]
- Di Luca, D.; Dolcetti, R.; Mirandola, P.; De Re, V.; Secchiero, P.; Carbone, A.; Boiocchi, M.; Cassai, E. Human herpesvirus 6: A survey of presence and variant distribution in normal peripheral lymphocytes and lymphoproliferative disorders. J. Infect. Dis. 1994, 170, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Kondo, K.; Kondo, T.; Okuno, T.; Takahashi, M.; Yamanishi, K. Latent human herpesvirus 6 infection of human monocytes/macrophages. J. Gen. Virol. 1991, 72 Pt 6, 1401–1408. [Google Scholar] [CrossRef]
- Marci, R.; Gentili, V.; Bortolotti, D.; Lo Monte, G.; Caselli, E.; Bolzani, S.; Rotola, A.; Di Luca, D.; Rizzo, R. Presence of HHV-6A in Endometrial Epithelial Cells from Women with Primary Unexplained Infertility. PLoS ONE 2016, 11, e0158304. [Google Scholar] [CrossRef]
- Caselli, E.; Bortolotti, D.; Marci, R.; Rotola, A.; Gentili, V.; Soffritti, I.; D’Accolti, M.; Lo Monte, G.; Sicolo, M.; Barao, I.; et al. HHV-6A Infection of Endometrial Epithelial Cells Induces Increased Endometrial NK Cell-Mediated Cytotoxicity. Front. Microbiol. 2017, 8, 2525. [Google Scholar] [CrossRef]
- Rizzo, R.; Soffritti, I.; D’Accolti, M.; Bortolotti, D.; Di Luca, D.; Caselli, E. HHV-6A/6B Infection of NK Cells Modulates the Expression of miRNAs and Transcription Factors Potentially Associated to Impaired NK Activity. Front. Microbiol. 2017, 8, 2143. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.L.; Gong, F.; Tang, Y.; Li, X.; Li, X.; Yang, X.; Lu, G. Inhibition of Endometrial Tiam1/Rac1 Signals Induced by miR-22 Up-Regulation Leads to the Failure of Embryo Implantation During the Implantation Window in Pregnant Mice. Biol. Reprod. 2015, 92, 152. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, D.; Soffritti, I.; D’Accolti, M.; Gentili, V.; Di Luca, D.; Rizzo, R.; Caselli, E. HHV-6A Infection of Endometrial Epithelial Cells Affects miRNA Expression and Trophoblast Cell Attachment. Reprod. Sci. 2020, 27, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, R.; Lo Monte, G.; Bortolotti, D.; Graziano, A.; Gentili, V.; Di Luca, D.; Marci, R. Impact of soluble HLA-G levels and endometrial NK cells in uterine flushing samples from primary and secondary unexplained infertile women. Int. J. Mol. Sci. 2015, 16, 5510–5516. [Google Scholar] [CrossRef]
- Sen, N.; Mukherjee, G.; Sen, A.; Bendall, S.C.; Sung, P.; Nolan, G.P.; Arvin, A.M. Single-cell mass cytometry analysis of human tonsil T cell remodeling by varicella zoster virus. Cell. Rep. 2014, 8, 633–645. [Google Scholar] [CrossRef]
- Kawana, K.; Yoshikawa, H.; Sata, T. Post-partum detection of varicella-zoster virus DNA in the placenta. Int. J. Gynaecol. Obstet. 1996, 55, 165–166. [Google Scholar] [CrossRef]
- Sauerbrei, A.; Wutzler, P. Herpes simplex and varicella-zoster virus infections during pregnancy: Current concepts of prevention, diagnosis and therapy. Part 2: Varicella-zoster virus infections. Med. Microbiol. Immunol. 2007, 196, 95–102. [Google Scholar] [CrossRef]
- McGregor, J.A.; Mark, S.; Crawford, G.P.; Levin, M.J. Varicella zoster antibody testing in the care of pregnant women exposed to varicella. Am. J. Obstet. Gynecol. 1987, 157, 281–284. [Google Scholar] [CrossRef]
- Kangro, H.O.; Manzoor, S.; Harper, D.R. Antibody avidity following varicella-zoster virus infections. J. Med. Virol. 1991, 33, 100–105. [Google Scholar] [CrossRef]
- Asano, Y.; Hiroishi, Y.; Itakura, N.; Hirose, S.; Kajita, Y.; Nagai, T.; Yazaki, T.; Takahashi, M. Immunoglobulin Subclass Antibodies to Varicefla-Zoster Virus. Pediatrics 1987, 80, 933–936. [Google Scholar] [CrossRef]
- Junker, A.K.; Tilley, P. Varicella-zoster virus antibody avidity and IgG-subclass patterns in children with recurrent chickenpox. J. Med. Virol. 1994, 43, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Itakura, N.; Kajita, Y.; Suga, S.; Yoshikawa, T.; Yazaki, T.; Ozaki, T.; Yamanishi, K.; Takahashi, M. Severity of viremia and clinical findings in children with varicella. J. Infect. Dis. 1990, 161, 1095–1098. [Google Scholar] [CrossRef]
- Gerlini, G.; Mariotti, G.; Bianchi, B.; Pimpinelli, N. Massive recruitment of type I interferon producing plasmacytoid dendritic cells in varicella skin lesions. J. Investig. Dermatol. 2006, 126, 507–509. [Google Scholar] [CrossRef]
- Arvin, A.M.; Koropchak, C.M.; Williams, B.R.; Grumet, F.C.; Foung, S.K. Early immune response in healthy and immunocompromised subjects with primary varicella-zoster virus infection. J. Infect. Dis. 1986, 154, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Banovic, T.; Yanilla, M.; Simmons, R.; Robertson, I.; Schroder, W.A.; Raffelt, N.C.; Wilson, Y.A.; Hill, G.R.; Hogan, P.; Nourse, C.B. Disseminated varicella infection caused by varicella vaccine strain in a child with low invariant natural killer T cells and diminished CD1d expression. J. Infect. Dis. 2011, 204, 1893–1901. [Google Scholar] [CrossRef]
- Duncan, C.J.; Hambleton, S. Varicella zoster virus immunity: A primer. J. Infect. 2015, 71 (Suppl. S1), S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Dhanya, C.R.; Shailaja, A.; Mary, A.S.; Kandiyil, S.P.; Savithri, A.; Lathakumari, V.S.; Veettil, J.T.; Vandanamthadathil, J.J.; Madhavan, M. RNA Viruses, Pregnancy and Vaccination: Emerging Lessons from COVID-19 and Ebola Virus Disease. Pathogens 2022, 11, 800. [Google Scholar] [CrossRef] [PubMed]
- Bebell, L.M.; Oduyebo, T.; Riley, L.E. Ebola virus disease and pregnancy: A review of the current knowledge of Ebola virus pathogenesis, maternal, and neonatal outcomes. Birth Defects Res. 2017, 109, 353–362. [Google Scholar] [CrossRef]
- Aghaeepour, N.; Ganio, E.A.; McIlwain, D.; Tsai, A.S.; Tingle, M.; Van Gassen, S.; Gaudilliere, D.K.; Baca, Q.; McNeil, L.; Okada, R.; et al. An immune clock of human pregnancy. Sci. Immunol. 2017, 2, eaan2946. [Google Scholar] [CrossRef]
- Kay, A.W.; Fukuyama, J.; Aziz, N.; Dekker, C.L.; Mackey, S.; Swan, G.E.; Davis, M.M.; Holmes, S.; Blish, C.A. Enhanced natural killer-cell and T-cell responses to influenza A virus during pregnancy. Proc. Natl. Acad. Sci. USA 2014, 111, 14506–14511. [Google Scholar] [CrossRef] [PubMed]
- Lurie, S.; Rahamim, E.; Piper, I.; Golan, A.; Sadan, O. Total and differential leukocyte counts percentiles in normal pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 136, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Liu, J.; Liu, S.; Xia, M.; Zhang, X.; Han, D.; Jiang, Y.; Wang, C.; Cao, X. Methyltransferase SETD2-Mediated Methylation of STAT1 Is Critical for Interferon Antiviral Activity. Cell 2017, 170, 492–506 e414. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Bowden, D.S. Rubella virus replication and links to teratogenicity. Clin. Microbiol. Rev. 2000, 13, 571–587. [Google Scholar] [CrossRef] [PubMed]
- Gregg, N.M. Congenital Cataract Following German Measles in the Mother. In Problems of Birth Defects; Springer: Berlin/Heidelberg, Germany, 1941; pp. 170–180. [Google Scholar]
- Best, J.M.; Enders, G. Chapter 3 Laboratory Diagnosis of Rubella and Congenital Rubella. Perspect. Med. Virol. 2006, 15, 39–77. [Google Scholar]
- Breeze, A.C. Infectious diseases of the fetus and newborn infant, 6th edn. Arch. Dis. Child.-Fetal Neonatal Ed. 2007, 92, F156. [Google Scholar] [CrossRef]
- Ramondetti, F.; Sacco, S.; Comelli, M.; Bruno, G.; Falorni, A.; Iannilli, A.; d’Annunzio, G.; Iafusco, D.; Songini, M.; Toni, S.; et al. Type 1 diabetes and measles, mumps and rubella childhood infections within the Italian Insulin-dependent Diabetes Registry. Diabet. Med. 2012, 29, 761–766. [Google Scholar] [CrossRef]
- Thong, Y.H.; Steele, R.W.; Vincent, M.M.; Hensen, S.A.; Bellanti, J.A. Impaired in vitro cell-mediated immunity to rubella virus during pregnancy. N. Engl. J. Med. 1973, 289, 604–606. [Google Scholar] [CrossRef]
- O’Shea, S.; Corbett, K.M.; Barrow, S.M.; Banatvala, J.E.; Best, J.M. Rubella reinfection; role of neutralising antibodies and cell-mediated immunity. Clin. Diagn. Virol. 1994, 2, 349–358. [Google Scholar] [CrossRef]
- South, M.A.; Montgomery, J.R.; Rawls, W.E. Immune deficiency in congenital rubella and other viral infections. Birth Defects Orig. Artic. Ser. 1975, 11, 234–238. [Google Scholar]
- Mace, M.; Cointe, D.; Six, C.; Levy-Bruhl, D.; Parent du Chatelet, I.; Ingrand, D.; Grangeot-Keros, L. Diagnostic value of reverse transcription-PCR of amniotic fluid for prenatal diagnosis of congenital rubella infection in pregnant women with confirmed primary rubella infection. J. Clin. Microbiol. 2004, 42, 4818–4820. [Google Scholar] [CrossRef] [PubMed]
- McLean, H.Q.; Fiebelkorn, A.P.; Temte, J.L.; Wallace, G.S.; Centers for Disease, C. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: Summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2013, 62, 1–34. [Google Scholar] [PubMed]
- Ragusa, R.; Platania, A.; Cuccia, M.; Zappala, G.; Giorgianni, G.; D’Agati, P.; Bellia, M.A.; Marranzano, M. Measles and Pregnancy: Immunity and Immunization-What Can Be Learned from Observing Complications during an Epidemic Year. J. Pregnancy 2020, 2020, 6532868. [Google Scholar] [CrossRef]
- Strebel, P.M.; Orenstein, W.A. Measles. N. Engl. J. Med. 2019, 381, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Raghupathy, R. Th1-type immunity is incompatible with successful pregnancy. Immunol. Today 1997, 18, 478–482. [Google Scholar] [CrossRef]
- Eke, A.C.; Lockman, S.; Mofenson, L.M. Antiretroviral Treatment of HIV/AIDS During Pregnancy. JAMA 2023, 329, 1308–1309. [Google Scholar] [CrossRef]
- Pfeifer, C.; Bunders, M.J. Maternal HIV infection alters the immune balance in the mother and fetus; implications for pregnancy outcome and infant health. Curr. Opin. HIV AIDS 2016, 11, 138–145. [Google Scholar] [CrossRef]
- Mellor, A.L.; Munn, D.H. Immunology at the maternal-fetal interface: Lessons for T cell tolerance and suppression. Annu. Rev. Immunol. 2000, 18, 367–391. [Google Scholar] [CrossRef] [PubMed]
- Uchide, N.; Ohyama, K.; Bessho, T.; Takeichi, M.; Toyoda, H. Possible roles of proinflammatory and chemoattractive cytokines produced by human fetal membrane cells in the pathology of adverse pregnancy outcomes associated with influenza virus infection. Mediators Inflamm. 2012, 2012, 270670. [Google Scholar] [CrossRef]
- Mwanyumba, F.; Gaillard, P.; Inion, I.; Verhofstede, C.; Claeys, P.; Chohan, V.; Vansteelandt, S.; Mandaliya, K.; Praet, M.; Temmerman, M. Placental inflammation and perinatal transmission of HIV-1. J. Acquir. Immune Defic. Syndr. 2002, 29, 262–269. [Google Scholar] [CrossRef]
- Shive, C.L.; Clagett, B.; McCausland, M.R.; Mudd, J.C.; Funderburg, N.T.; Freeman, M.L.; Younes, S.A.; Ferrari, B.M.; Rodriguez, B.; McComsey, G.A.; et al. Inflammation Perturbs the IL-7 Axis, Promoting Senescence and Exhaustion that Broadly Characterize Immune Failure in Treated HIV Infection. J. Acquir. Immune Defic. Syndr. 2016, 71, 483–492. [Google Scholar] [CrossRef]
- Moffett, A.; Hiby, S.E.; Sharkey, A.M. The role of the maternal immune system in the regulation of human birthweight. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2015, 370, 20140071. [Google Scholar] [CrossRef] [PubMed]
- Hiby, S.E.; Apps, R.; Sharkey, A.M.; Farrell, L.E.; Gardner, L.; Mulder, A.; Claas, F.H.; Walker, J.J.; Redman, C.W.; Morgan, L.; et al. Maternal activating KIRs protect against human reproductive failure mediated by fetal HLA-C2. J. Clin. Investig. 2010, 120, 4102–4110. [Google Scholar] [CrossRef]
- Alter, G.; Malenfant, J.M.; Delabre, R.M.; Burgett, N.C.; Yu, X.G.; Lichterfeld, M.; Zaunders, J.; Altfeld, M. Increased natural killer cell activity in viremic HIV-1 infection. J. Immunol. 2004, 173, 5305–5311. [Google Scholar] [CrossRef] [PubMed]
- Alter, G.; Teigen, N.; Davis, B.T.; Addo, M.M.; Suscovich, T.J.; Waring, M.T.; Streeck, H.; Johnston, M.N.; Staller, K.D.; Zaman, M.T.; et al. Sequential deregulation of NK cell subset distribution and function starting in acute HIV-1 infection. Blood 2005, 106, 3366–3369. [Google Scholar] [CrossRef] [PubMed]
- Behbahani, H.; Popek, E.; Garcia, P.; Andersson, J.; Spetz, A.L.; Landay, A.; Flener, Z.; Patterson, B.K. Up-regulation of CCR5 expression in the placenta is associated with human immunodeficiency virus-1 vertical transmission. Am. J. Pathol. 2000, 157, 1811–1818. [Google Scholar] [CrossRef]
- Blois, S.M.; Ilarregui, J.M.; Tometten, M.; Garcia, M.; Orsal, A.S.; Cordo-Russo, R.; Toscano, M.A.; Bianco, G.A.; Kobelt, P.; Handjiski, B.; et al. A pivotal role for galectin-1 in fetomaternal tolerance. Nat. Med. 2007, 13, 1450–1457. [Google Scholar] [CrossRef]
- Kammerer, U.; Eggert, A.O.; Kapp, M.; McLellan, A.D.; Geijtenbeek, T.B.; Dietl, J.; van Kooyk, Y.; Kampgen, E. Unique appearance of proliferating antigen-presenting cells expressing DC-SIGN (CD209) in the decidua of early human pregnancy. Am. J. Pathol. 2003, 162, 887–896. [Google Scholar] [CrossRef]
- Carles, G. What are the true consequences of dengue during pregnancy? Lancet Infect. Dis. 2016, 16, 765–766. [Google Scholar] [CrossRef]
- Machado, C.R.; Machado, E.S.; Rohloff, R.D.; Azevedo, M.; Campos, D.P.; de Oliveira, R.B.; Brasil, P. Is pregnancy associated with severe dengue? A review of data from the Rio de Janeiro surveillance information system. PLoS Negl. Trop. Dis. 2013, 7, e2217. [Google Scholar] [CrossRef]
- Basurko, C.; Everhard, S.; Matheus, S.; Restrepo, M.; Hilderal, H.; Lambert, V.; Boukhari, R.; Duvernois, J.P.; Favre, A.; Valmy, L.; et al. A prospective matched study on symptomatic dengue in pregnancy. PLoS ONE 2018, 13, e0202005. [Google Scholar] [CrossRef]
- Charlier, C.; Beaudoin, M.C.; Couderc, T.; Lortholary, O.; Lecuit, M. Arboviruses and pregnancy: Maternal, fetal, and neonatal effects. Lancet Child. Adolesc. Health 2017, 1, 134–146. [Google Scholar] [CrossRef] [PubMed]
- Vogt, M.B.; Lahon, A.; Arya, R.P.; Spencer Clinton, J.L.; Rico-Hesse, R. Dengue viruses infect human megakaryocytes, with probable clinical consequences. PLoS Negl. Trop. Dis. 2019, 13, e0007837. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.A.; Schwertz, H.; Hottz, E.D.; Rowley, J.W.; Manne, B.K.; Washington, A.V.; Hunter-Mellado, R.; Tolley, N.D.; Christensen, M.; Eustes, A.S.; et al. Human megakaryocytes possess intrinsic antiviral immunity through regulated induction of IFITM3. Blood 2019, 133, 2013–2026. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Moreno, J.; Hernandez, J.C.; Urcuqui-Inchima, S. Effect of high doses of vitamin D supplementation on dengue virus replication, Toll-like receptor expression, and cytokine profiles on dendritic cells. Mol. Cell. Biochem. 2020, 464, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Uno, N.; Ross, T.M. Dengue virus and the host innate immune response. Emerg. Microbes Infect. 2018, 7, 167. [Google Scholar] [CrossRef]
- Brasil, P.; Pereira, J.P., Jr.; Moreira, M.E.; Ribeiro Nogueira, R.M.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.A.; Salles, T.S.; et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N. Engl. J. Med. 2016, 375, 2321–2334. [Google Scholar] [CrossRef]
- Coyne, C.B.; Lazear, H.M. Zika virus—reigniting the TORCH. Nat. Rev. Microbiol. 2016, 14, 707–715. [Google Scholar] [CrossRef]
- Honein, M.A.; Dawson, A.L.; Petersen, E.E.; Jones, A.M.; Lee, E.H.; Yazdy, M.M.; Ahmad, N.; Macdonald, J.; Evert, N.; Bingham, A.; et al. Birth Defects Among Fetuses and Infants of US Women With Evidence of Possible Zika Virus Infection During Pregnancy. JAMA 2017, 317, 59–68. [Google Scholar] [CrossRef]
- Reynolds, M.R.; Jones, A.M.; Petersen, E.E.; Lee, E.H.; Rice, M.E.; Bingham, A.; Ellington, S.R.; Evert, N.; Reagan-Steiner, S.; Oduyebo, T.; et al. Vital Signs: Update on Zika Virus-Associated Birth Defects and Evaluation of All U.S. Infants with Congenital Zika Virus Exposure—U.S. Zika Pregnancy Registry, 2016. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 366–373. [Google Scholar] [CrossRef]
- Cumming, H.E.; Bourke, N.M. Type I IFNs in the female reproductive tract: The first line of defense in an ever-changing battleground. J. Leukoc. Biol. 2019, 105, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Racicot, K.; Kwon, J.Y.; Aldo, P.; Silasi, M.; Mor, G. Understanding the complexity of the immune system during pregnancy. Am. J. Reprod. Immunol. 2014, 72, 107–116. [Google Scholar] [CrossRef]
- Ruiz, R.J.; Fullerton, J.; Dudley, D.J. The interrelationship of maternal stress, endocrine factors and inflammation on gestational length. Obstet. Gynecol. Surv. 2003, 58, 415–428. [Google Scholar] [CrossRef] [PubMed]
- Bardina, S.V.; Bunduc, P.; Tripathi, S.; Duehr, J.; Frere, J.J.; Brown, J.A.; Nachbagauer, R.; Foster, G.A.; Krysztof, D.; Tortorella, D.; et al. Enhancement of Zika virus pathogenesis by preexisting antiflavivirus immunity. Science 2017, 356, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.A.; Singh, G.; Acklin, J.A.; Lee, S.; Duehr, J.E.; Chokola, A.N.; Frere, J.J.; Hoffman, K.W.; Foster, G.A.; Krysztof, D.; et al. Dengue Virus Immunity Increases Zika Virus-Induced Damage during Pregnancy. Immunity 2019, 50, 751–762 e755. [Google Scholar] [CrossRef] [PubMed]
- Shim, B.S.; Kwon, Y.C.; Ricciardi, M.J.; Stone, M.; Otsuka, Y.; Berri, F.; Kwal, J.M.; Magnani, D.M.; Jackson, C.B.; Richard, A.S.; et al. Zika Virus-Immune Plasmas from Symptomatic and Asymptomatic Individuals Enhance Zika Pathogenesis in Adult and Pregnant Mice. mBio 2019, 10, e00758-19. [Google Scholar] [CrossRef]
- Simoni, M.K.; Jurado, K.A.; Abrahams, V.M.; Fikrig, E.; Guller, S. Zika virus infection of Hofbauer cells. Am. J. Reprod. Immunol. 2017, 77, e12613. [Google Scholar] [CrossRef]
- Bayer, A.; Lennemann, N.J.; Ouyang, Y.; Bramley, J.C.; Morosky, S.; Marques, E.T., Jr.; Cherry, S.; Sadovsky, Y.; Coyne, C.B. Type III Interferons Produced by Human Placental Trophoblasts Confer Protection against Zika Virus Infection. Cell. Host Microbe 2016, 19, 705–712. [Google Scholar] [CrossRef]
- Noronha, L.; Zanluca, C.; Azevedo, M.L.; Luz, K.G.; Santos, C.N. Zika virus damages the human placental barrier and presents marked fetal neurotropism. Mem. Inst. Oswaldo Cruz 2016, 111, 287–293. [Google Scholar] [CrossRef]
- Jurado, K.A.; Simoni, M.K.; Tang, Z.; Uraki, R.; Hwang, J.; Householder, S.; Wu, M.; Lindenbach, B.D.; Abrahams, V.M.; Guller, S.; et al. Zika virus productively infects primary human placenta-specific macrophages. JCI Insight 2016, 1. [Google Scholar] [CrossRef]
- Adibi, J.J.; Zhao, Y.; Cartus, A.R.; Gupta, P.; Davidson, L.A. Placental Mechanics in the Zika-Microcephaly Relationship. Cell. Host Microbe 2016, 20, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Winkler, C.W.; Myers, L.M.; Woods, T.A.; Messer, R.J.; Carmody, A.B.; McNally, K.L.; Scott, D.P.; Hasenkrug, K.J.; Best, S.M.; Peterson, K.E. Adaptive Immune Responses to Zika Virus Are Important for Controlling Virus Infection and Preventing Infection in Brain and Testes. J. Immunol. 2017, 198, 3526–3535. [Google Scholar] [CrossRef] [PubMed]
- Regla-Nava, J.A.; Elong Ngono, A.; Viramontes, K.M.; Huynh, A.T.; Wang, Y.T.; Nguyen, A.T.; Salgado, R.; Mamidi, A.; Kim, K.; Diamond, M.S.; et al. Cross-reactive Dengue virus-specific CD8(+) T cells protect against Zika virus during pregnancy. Nat. Commun. 2018, 9, 3042. [Google Scholar] [CrossRef] [PubMed]
- Elong Ngono, A.; Vizcarra, E.A.; Tang, W.W.; Sheets, N.; Joo, Y.; Kim, K.; Gorman, M.J.; Diamond, M.S.; Shresta, S. Mapping and Role of the CD8(+) T Cell Response During Primary Zika Virus Infection in Mice. Cell. Host Microbe 2017, 21, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Tang, W.W.; Sheets, N.; Ellison, J.; Sette, A.; Kim, K.; Shresta, S. Identification of Zika virus epitopes reveals immunodominant and protective roles for dengue virus cross-reactive CD8(+) T cells. Nat. Microbiol. 2017, 2, 17036. [Google Scholar] [CrossRef]
- Wen, J.; Shresta, S. T Cell Immunity to Zika and Dengue Viral Infections. J. Interferon Cytokine Res. 2017, 37, 475–479. [Google Scholar] [CrossRef]
- Ngono, A.E.; Shresta, S. Immune Response to Dengue and Zika. Annu. Rev. Immunol. 2018, 36, 279–308. [Google Scholar] [CrossRef]
- Seong, R.K.; Lee, J.K.; Shin, O.S. Zika Virus-Induction of the Suppressor of Cytokine Signaling 1/3 Contributes to the Modulation of Viral Replication. Pathogens 2020, 9, 163. [Google Scholar] [CrossRef]
- Kumar, A.; Devi, S.G.; Kar, P.; Agarwal, S.; Husain, S.A.; Gupta, R.K.; Sharma, S. Association of cytokines in hepatitis E with pregnancy outcome. Cytokine 2014, 65, 95–104. [Google Scholar] [CrossRef]
- Foo, S.S.; Chen, W.; Chan, Y.; Lee, W.S.; Lee, S.A.; Cheng, G.; Nielsen-Saines, K.; Brasil, P.; Jung, J.U. Biomarkers and immunoprofiles associated with fetal abnormalities of ZIKV-positive pregnancies. JCI Insight 2018, 3, e124152. [Google Scholar] [CrossRef]
- Camacho-Zavala, E.; Santacruz-Tinoco, C.; Munoz, E.; Chacon-Salinas, R.; Salazar-Sanchez, M.I.; Grajales, C.; Gonzalez-Ibarra, J.; Borja-Aburto, V.H.; Jaenisch, T.; Gonzalez-Bonilla, C.R. Pregnant Women Infected with Zika Virus Show Higher Viral Load and Immunoregulatory Cytokines Profile with CXCL10 Increase. Viruses 2021, 13, 80. [Google Scholar] [CrossRef] [PubMed]
- Barros, J.B.S.; da Silva, P.A.N.; Koga, R.C.R.; Gonzalez-Dias, P.; Carmo Filho, J.R.; Nagib, P.R.A.; Coelho, V.; Nakaya, H.I.; Fonseca, S.G.; Pfrimer, I.A.H. Acute Zika Virus Infection in an Endemic Area Shows Modest Proinflammatory Systemic Immunoactivation and Cytokine-Symptom Associations. Front. Immunol. 2018, 9, 821. [Google Scholar] [CrossRef] [PubMed]
- Yockey, L.J.; Iwasaki, A. Interferons and Proinflammatory Cytokines in Pregnancy and Fetal Development. Immunity 2018, 49, 397–412. [Google Scholar] [CrossRef] [PubMed]
- Naveca, F.G.; Pontes, G.S.; Chang, A.Y.; Silva, G.; Nascimento, V.A.D.; Monteiro, D.; Silva, M.S.D.; Abdalla, L.F.; Santos, J.H.A.; Almeida, T.A.P.; et al. Analysis of the immunological biomarker profile during acute Zika virus infection reveals the overexpression of CXCL10, a chemokine linked to neuronal damage. Mem. Inst. Oswaldo Cruz 2018, 113, e170542. [Google Scholar] [CrossRef] [PubMed]
- Lum, F.M.; Lye, D.C.B.; Tan, J.J.L.; Lee, B.; Chia, P.Y.; Chua, T.K.; Amrun, S.N.; Kam, Y.W.; Yee, W.X.; Ling, W.P.; et al. Longitudinal Study of Cellular and Systemic Cytokine Signatures to Define the Dynamics of a Balanced Immune Environment During Disease Manifestation in Zika Virus-Infected Patients. J. Infect. Dis. 2018, 218, 814–824. [Google Scholar] [CrossRef] [PubMed]
- O’Garra, A.; Vieira, P.L.; Vieira, P.; Goldfeld, A.E. IL-10-producing and naturally occurring CD4+ Tregs: Limiting collateral damage. J. Clin. Invest. 2004, 114, 1372–1378. [Google Scholar] [CrossRef]
- Pealer, L.N.; Marfin, A.A.; Petersen, L.R.; Lanciotti, R.S.; Page, P.L.; Stramer, S.L.; Stobierski, M.G.; Signs, K.; Newman, B.; Kapoor, H.; et al. Transmission of West Nile virus through blood transfusion in the United States in 2002. N. Engl. J. Med. 2003, 349, 1236–1245. [Google Scholar] [CrossRef]
- Iwamoto, M.; Jernigan, D.B.; Guasch, A.; Trepka, M.J.; Blackmore, C.G.; Hellinger, W.C.; Pham, S.M.; Zaki, S.; Lanciotti, R.S.; Lance-Parker, S.E.; et al. Transmission of West Nile virus from an organ donor to four transplant recipients. N. Engl. J. Med. 2003, 348, 2196–2203. [Google Scholar] [CrossRef]
- From the Centers for Disease Control and Prevention. Possible West Nile virus transmission to an infant through breast-feeding—Michigan, 2002. JAMA 2002, 288, 1976–1977.
- Hayes, E.B.; O’Leary, D.R. West Nile virus infection: A pediatric perspective. Pediatrics 2004, 113, 1375–1381. [Google Scholar] [CrossRef]
- O’Leary, D.R.; Kuhn, S.; Kniss, K.L.; Hinckley, A.F.; Rasmussen, S.A.; Pape, W.J.; Kightlinger, L.K.; Beecham, B.D.; Miller, T.K.; Neitzel, D.F.; et al. Birth outcomes following West Nile Virus infection of pregnant women in the United States: 2003-2004. Pediatrics 2006, 117, e537–e545. [Google Scholar] [CrossRef] [PubMed]
- Cordoba, L.; Escribano-Romero, E.; Garmendia, A.; Saiz, J.C. Pregnancy increases the risk of mortality in West Nile virus-infected mice. J. Gen. Virol. 2007, 88, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Armah, H.B.; Wang, G.; Omalu, B.I.; Tesh, R.B.; Gyure, K.A.; Chute, D.J.; Smith, R.D.; Dulai, P.; Vinters, H.V.; Kleinschmidt-DeMasters, B.K.; et al. Systemic distribution of West Nile virus infection: Postmortem immunohistochemical study of six cases. Brain Pathol. 2007, 17, 354–362. [Google Scholar] [CrossRef]
- Garcia, M.N.; Hasbun, R.; Murray, K.O. Persistence of West Nile virus. Microbes Infect. 2015, 17, 163–168. [Google Scholar] [CrossRef]
- Gack, M.U.; Diamond, M.S. Innate immune escape by Dengue and West Nile viruses. Curr. Opin. Virol. 2016, 20, 119–128. [Google Scholar] [CrossRef] [PubMed]
- King, N.J.; Kesson, A.M. Interferon-independent increases in class I major histocompatibility complex antigen expression follow flavivirus infection. J. Gen. Virol. 1988, 69 Pt 10, 2535–2543. [Google Scholar] [CrossRef]
- Liu, Y.; King, N.; Kesson, A.; Blanden, R.V.; Mullbacher, A. Flavivirus infection up-regulates the expression of class I and class II major histocompatibility antigens on and enhances T cell recognition of astrocytes in vitro. J. Neuroimmunol. 1989, 21, 157–168. [Google Scholar] [CrossRef]
- Bao, S.; King, N.J.; Dos Remedios, C.G. Flavivirus induces MHC antigen on human myoblasts: A model of autoimmune myositis? Muscle Nerve 1992, 15, 1271–1277. [Google Scholar] [CrossRef]
- King, N.J.; Maxwell, L.E.; Kesson, A.M. Induction of class I major histocompatibility complex antigen expression by West Nile virus on gamma interferon-refractory early murine trophoblast cells. Proc. Natl. Acad. Sci. USA 1989, 86, 911–915. [Google Scholar] [CrossRef]
- Monath, T. Pathobiology of the Flaviviruses. In The Togaviridae and Flaviviridae Edited by: Schlesinger SSMJ; Springer: Berlin/Heidelberg, Germany, 1986. [Google Scholar]
- Sugamata, M.; Miura, T. Japanese encephalitis virus infection in fetal mice at different stages of pregnancy I. Stillbirth. Acta virologica 1982, 26, 279–282. [Google Scholar]
- Senapati, S.; Banerjee, P.; Bhagavatula, S.; Kushwaha, P.P.; Kumar, S. Contributions of human ACE2 and TMPRSS2 in determining host-pathogen interaction of COVID-19. J. Genet. 2021, 100, 1–16. [Google Scholar] [CrossRef]
- Pique-Regi, R.; Romero, R.; Tarca, A.L.; Sendler, E.D.; Xu, Y.; Garcia-Flores, V.; Leng, Y.; Luca, F.; Hassan, S.S.; Gomez-Lopez, N. Single cell transcriptional signatures of the human placenta in term and preterm parturition. Elife 2019, 8, e52004. [Google Scholar] [CrossRef] [PubMed]
- Pique-Regi, R.; Romero, R.; Tarca, A.L.; Luca, F.; Xu, Y.; Alazizi, A.; Leng, Y.; Hsu, C.D.; Gomez-Lopez, N. Does the human placenta express the canonical cell entry mediators for SARS-CoV-2? Elife 2020, 9, e58716. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, Z.; Yang, L.; Lian, X.; Xie, Y.; Li, S.; Xin, S.; Cao, P.; Lu, J. The MERS-CoV Receptor DPP4 as a Candidate Binding Target of the SARS-CoV-2 Spike. iScience 2020, 23, 101160. [Google Scholar] [CrossRef]
- Dong, L.; Pei, S.; Ren, Q.; Fu, S.; Yu, L.; Chen, H.; Chen, X.; Yin, M. Evaluation of vertical transmission of SARS-CoV-2 in utero: Nine pregnant women and their newborns. Placenta 2021, 111, 91–96. [Google Scholar] [CrossRef]
- Schiuma, G.; Beltrami, S.; Santi, E.; Scutiero, G.; Sanz, J.M.; Semprini, C.M.; Rizzo, S.; Fernandez, M.; Zidi, I.; Gafa, R.; et al. Effect of SARS-CoV-2 infection in pregnancy on CD147, ACE2 and HLA-G expression. Placenta 2023, 132, 38–43. [Google Scholar] [CrossRef]
- Hosier, H.; Farhadian, S.F.; Morotti, R.A.; Deshmukh, U.; Lu-Culligan, A.; Campbell, K.H.; Yasumoto, Y.; Vogels, C.B.; Casanovas-Massana, A.; Vijayakumar, P.; et al. SARS-CoV-2 infection of the placenta. J. Clin. Investig. 2020, 130, 4947–4953. [Google Scholar] [CrossRef] [PubMed]
- Vivanti, A.J.; Vauloup-Fellous, C.; Prevot, S.; Zupan, V.; Suffee, C.; Do Cao, J.; Benachi, A.; De Luca, D. Transplacental transmission of SARS-CoV-2 infection. Nat. Commun. 2020, 11, 3572. [Google Scholar] [CrossRef]
- Facchetti, F.; Bugatti, M.; Drera, E.; Tripodo, C.; Sartori, E.; Cancila, V.; Papaccio, M.; Castellani, R.; Casola, S.; Boniotti, M.B.; et al. SARS-CoV2 vertical transmission with adverse effects on the newborn revealed through integrated immunohistochemical, electron microscopy and molecular analyses of Placenta. EBioMedicine 2020, 59, 102951. [Google Scholar] [CrossRef]
- Schoenmakers, S.; Snijder, P.; Verdijk, R.M.; Kuiken, T.; Kamphuis, S.S.M.; Koopman, L.P.; Krasemann, T.B.; Rousian, M.; Broekhuizen, M.; Steegers, E.A.P.; et al. SARS-CoV-2 placental infection and inflammation leading to fetal distress and neonatal multi-organ failure in an asymptomatic woman. MedRxiv 2020. [Google Scholar] [CrossRef]
- Greco, S.; Sanz, J.M.; Bortolotti, D.; Semprini, C.M.; Gafà, R.; Santi, E.; Maestri, I.; Rizzo, R.; Greco, P.; Passaro, A.J.F.i.M. Case report: Tissue positivity for SARS-CoV-2 in a preterm born infant death of thrombosis. A possible intrauterine transmission. Front. Med. 2023, 10, 1127529. [Google Scholar] [CrossRef]
- Rizzo, R.; Neri, L.M.; Simioni, C.; Bortolotti, D.; Occhionorelli, S.; Zauli, G.; Secchiero, P.; Semprini, C.M.; Laface, I.; Sanz, J.M.; et al. SARS-CoV-2 nucleocapsid protein and ultrastructural modifications in small bowel of a 4-week-negative COVID-19 patient. Clin. Microbiol. Infect. 2021, 27, 936–937. [Google Scholar] [CrossRef]
- Bortolotti, D.; Simioni, C.; Neri, L.M.; Rizzo, R.; Semprini, C.M.; Occhionorelli, S.; Laface, I.; Sanz, J.M.; Schiuma, G.; Rizzo, S.; et al. Relevance of VEGF and CD147 in different SARS-CoV-2 positive digestive tracts characterized by thrombotic damage. FASEB J. 2021, 35, e21969. [Google Scholar] [CrossRef] [PubMed]
- Traina, L.; Mucignat, M.; Rizzo, R.; Gafa, R.; Bortolotti, D.; Passaro, A.; Zamboni, P. COVID-19 induced aorto duodenal fistula following evar in the so called "negative" patient. Vascular 2023, 31, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, D.; Gentili, V.; Rizzo, S.; Schiuma, G.; Beltrami, S.; Spadaro, S.; Strazzabosco, G.; Campo, G.; Carosella, E.D.; Papi, A.; et al. Increased sHLA-G Is Associated with Improved COVID-19 Outcome and Reduced Neutrophil Adhesion. Viruses 2021, 13, 1855. [Google Scholar] [CrossRef] [PubMed]
- de Mendonca Vieira, R.; Meagher, A.; Crespo, A.C.; Kshirsagar, S.K.; Iyer, V.; Norwitz, E.R.; Strominger, J.L.; Tilburgs, T. Human Term Pregnancy Decidual NK Cells Generate Distinct Cytotoxic Responses. J. Immunol. 2020, 204, 3149–3159. [Google Scholar] [CrossRef]
- Bortolotti, D.; Gentili, V.; Rizzo, S.; Rotola, A.; Rizzo, R. SARS-CoV-2 Spike 1 Protein Controls Natural Killer Cell Activation via the HLA-E/NKG2A Pathway. Cells 2020, 9, 1975. [Google Scholar] [CrossRef]
- Braud, V.; Jones, E.Y.; McMichael, A. The human major histocompatibility complex class Ib molecule HLA-E binds signal sequence-derived peptides with primary anchor residues at positions 2 and 9. Eur. J. Immunol. 1997, 27, 1164–1169. [Google Scholar] [CrossRef]
- Anfossi, N.; Andre, P.; Guia, S.; Falk, C.S.; Roetynck, S.; Stewart, C.A.; Breso, V.; Frassati, C.; Reviron, D.; Middleton, D.; et al. Human NK cell education by inhibitory receptors for MHC class I. Immunity 2006, 25, 331–342. [Google Scholar] [CrossRef]
- Lesseur, C.; Jessel, R.H.; Ohrn, S.; Ma, Y.; Li, Q.; Dekio, F.; Brody, R.I.; Wetmur, J.G.; Gigase, F.A.J.; Lieber, M.; et al. Gestational SARS-CoV-2 infection is associated with placental expression of immune and trophoblast genes. Placenta 2022, 126, 125–132. [Google Scholar] [CrossRef]
- Chauhan, G.; Madou, M.J.; Kalra, S.; Chopra, V.; Ghosh, D.; Martinez-Chapa, S.O. Nanotechnology for COVID-19: Therapeutics and Vaccine Research. ACS Nano 2020, 14, 7760–7782. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekar, V.; Singh, A.V.; Maharjan, R.S.; Dakua, S.P.; Balakrishnan, S.; Dash, S.; Laux, P.; Luch, A.; Singh, S.; Pradhan, M. Perspectives on the Technological Aspects and Biomedical Applications of Virus-Like Particles/Nanoparticles in Reproductive Biology: Insights on the Medicinal and Toxicological Outlook. Adv. NanoBiomed Res. 2022, 2, 2200010. [Google Scholar] [CrossRef]
- Boix-Besora, A.; Lorenzo, E.; Lavado-Garcia, J.; Godia, F.; Cervera, L. Optimization, Production, Purification and Characterization of HIV-1 GAG-Based Virus-like Particles Functionalized with SARS-CoV-2. Vaccines 2022, 10, 250. [Google Scholar] [CrossRef]
- Garg, H.; Mehmetoglu-Gurbuz, T.; Ruddy, G.M.; Joshi, A. Capsid containing virus like particle vaccine against Zika virus made from a stable cell line. Vaccine 2019, 37, 7123–7131. [Google Scholar] [CrossRef] [PubMed]
- Shojaei, S.; Ali, M.S.; Suresh, M.; Upreti, T.; Mogourian, V.; Helewa, M.; Labouta, H.I. Dynamic placenta-on-a-chip model for fetal risk assessment of nanoparticles intended to treat pregnancy-associated diseases. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 166131. [Google Scholar] [CrossRef] [PubMed]
- Villar, L.; Dayan, G.H.; Arredondo-Garcia, J.L.; Rivera, D.M.; Cunha, R.; Deseda, C.; Reynales, H.; Costa, M.S.; Morales-Ramirez, J.O.; Carrasquilla, G.; et al. Efficacy of a tetravalent dengue vaccine in children in Latin America. N. Engl. J. Med. 2015, 372, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Ravel, G.; Rogue, A.; Spézia, F.; Mantel, N.; Gould, S.; Forster, R. Transfer of tetravalent dengue vaccine during gestation and lactation in mice. Toxicology Letters 2015, 238. [Google Scholar] [CrossRef]
- Riley, L.E.; Jamieson, D.J. Inclusion of Pregnant and Lactating Persons in COVID-19 Vaccination Efforts. Ann. Intern. Med. 2021, 174, 701–702. [Google Scholar] [CrossRef]
- Januszek, S.M.; Faryniak-Zuzak, A.; Barnas, E.; Lozinski, T.; Gora, T.; Siwiec, N.; Szczerba, P.; Januszek, R.; Kluz, T. The Approach of Pregnant Women to Vaccination Based on a COVID-19 Systematic Review. Medicina (Kaunas) 2021, 57. [Google Scholar] [CrossRef]
- Poland, G.A.; Jacobson, R.M.; Koutsky, L.A.; Tamms, G.M.; Railkar, R.; Smith, J.F.; Bryan, J.T.; Cavanaugh, P.F., Jr.; Jansen, K.U.; Barr, E. Immunogenicity and reactogenicity of a novel vaccine for human papillomavirus 16: A 2-year randomized controlled clinical trial. Mayo. Clin. Proc. 2005, 80, 601–610. [Google Scholar] [CrossRef]
- Bonde, U.; Joergensen, J.S.; Lamont, R.F.; Mogensen, O. Is HPV vaccination in pregnancy safe? Hum. Vaccin Immunother 2016, 12, 1960–1964. [Google Scholar] [CrossRef] [PubMed]
- Scheller, N.M.; Pasternak, B.; Molgaard-Nielsen, D.; Svanstrom, H.; Hviid, A. Quadrivalent HPV Vaccination and the Risk of Adverse Pregnancy Outcomes. N. Engl. J. Med. 2017, 376, 1223–1233. [Google Scholar] [CrossRef] [PubMed]
- Celikel, A.; Ustunsoz, A.; Guvenc, G. Determination of vaccination status of pregnant women during pregnancy and the affecting factors. J. Clin. Nurs. 2014, 23, 2142–2150. [Google Scholar] [CrossRef] [PubMed]
- Swamy, G.K.; Garcia-Putnam, R. Vaccine-preventable diseases in pregnancy. Am. J. Perinatol. 2013, 30, 89–97. [Google Scholar] [CrossRef]
- Makris, M.C.; Polyzos, K.A.; Mavros, M.N.; Athanasiou, S.; Rafailidis, P.I.; Falagas, M.E. Safety of hepatitis B, pneumococcal polysaccharide and meningococcal polysaccharide vaccines in pregnancy: A systematic review. Drug. Saf. 2012, 35, 1–14. [Google Scholar] [CrossRef]
- Hieu, N.T.; Kim, K.H.; Janowicz, Z.; Timmermans, I. Comparative efficacy, safety and immunogenicity of Hepavax-Gene and Engerix-B, recombinant hepatitis B vaccines, in infants born to HBsAg and HBeAg positive mothers in Vietnam: An assessment at 2 years. Vaccine 2002, 20, 1803–1808. [Google Scholar] [CrossRef]
- Shivananda; Somani, V.; Srikanth, B.S.; Mohan, M.; Kulkarni, P.S. Comparison of two hepatitis B vaccines (GeneVac-B and Engerix-B) in healthy infants in India. Clin. Vaccin. Immunol. 2006, 13, 661–664. [Google Scholar] [CrossRef]
- Hernandez-Bernal, F.; Aguilar-Betancourt, A.; Aljovin, V.; Arias, G.; Valenzuela, C.; de Alejo, K.P.; Hernandez, K.; Oquendo, O.; Figueredo, N.; Figueroa, N.; et al. Comparison of four recombinant hepatitis B vaccines applied on an accelerated schedule in healthy adults. Hum. Vaccin. 2011, 7, 1026–1036. [Google Scholar] [CrossRef]
- Van Damme, P.; Minervini, G.; Liss, C.L.; McCarson, B.; Vesikari, T.; Boslego, J.W.; Bhuyan, P.K. Safety, tolerability and immunogenicity of a recombinant hepatitis B vaccine manufactured by a modified process in healthy young adults. Hum. Vaccin. 2009, 5, 92–97. [Google Scholar] [CrossRef]
- Ayoola, E.A.; Johnson, A.O. Hepatitis B vaccine in pregnancy: Immunogenicity, safety and transfer of antibodies to infants. Int. J. Gynaecol. Obstet. 1987, 25, 297–301. [Google Scholar] [CrossRef]
- Ingardia, C.J.; Kelley, L.; Steinfeld, J.D.; Wax, J.R. Hepatitis B vaccination in pregnancy: Factors influencing efficacy. Obstet. Gynecol. 1999, 93, 983–986. [Google Scholar] [CrossRef]
- Ingardia, C.J.; Kelley, L.; Lerer, T.; Wax, J.R.; Steinfeld, J.D. Correlation of maternal and fetal hepatitis B antibody titers following maternal vaccination in pregnancy. Am. J. Perinatol. 1999, 16, 129–132. [Google Scholar] [CrossRef]
- Sheffield, J.S.; Hickman, A.; Tang, J.; Moss, K.; Kourosh, A.; Crawford, N.M.; Wendel, G.D., Jr. Efficacy of an accelerated hepatitis B vaccination program during pregnancy. Obstet. Gynecol. 2011, 117, 1130–1135. [Google Scholar] [CrossRef] [PubMed]
- Grosheide, P.M.; Schalm, S.W.; van Os, H.C.; Fetter, W.P.; Heijtink, R.A. Immune response to hepatitis B vaccine in pregnant women receiving post-exposure prophylaxis. Eur. J. Obstet. Gynecol. Reprod. Biol. 1993, 50, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Charlton, R.A.; Cunnington, M.C.; de Vries, C.S.; Weil, J.G. Data resources for investigating drug exposure during pregnancy and associated outcomes: The General Practice Research Database (GPRD) as an alternative to pregnancy registries. Drug. Saf. 2008, 31, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Hoar, R.M. Developmental Toxicity: Extrapolation Across Species. J. Am. Coll. Toxicol. 2016, 14, 11–20. [Google Scholar] [CrossRef]
- Koren, G.; Pastuszak, A.; Ito, S. Drugs in pregnancy. N. Engl. J. Med. 1998, 338, 1128–1137. [Google Scholar] [CrossRef]
- Lok, A.S.; McMahon, B.J. Chronic hepatitis B: Update 2009. Hepatology 2009, 50, 661–662. [Google Scholar] [CrossRef]
- Brown, Z.A.; Watts, D.H. Antiviral therapy in pregnancy. Clin. Obstet. Gynecol. 1990, 33, 276–289. [Google Scholar] [CrossRef]
- Kang, S.H.; Chua-Gocheco, A.; Bozzo, P.; Einarson, A. Safety of antiviral medication for the treatment of herpes during pregnancy. Can. Fam. Physician. 2011, 57, 427–428. [Google Scholar]
- Pan, C.Q.; Duan, Z.P.; Bhamidimarri, K.R.; Zou, H.B.; Liang, X.F.; Li, J.; Tong, M.J. An algorithm for risk assessment and intervention of mother to child transmission of hepatitis B virus. Clin. Gastroenterol. Hepatol. 2012, 10, 452–459. [Google Scholar] [CrossRef]
- European Association For The Study Of The, L. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J. Hepatol. 2012, 57, 167–185. [Google Scholar] [CrossRef] [PubMed]
- Keeffe, E.B.; Dieterich, D.T.; Han, S.H.; Jacobson, I.M.; Martin, P.; Schiff, E.R.; Tobias, H. A treatment algorithm for the management of chronic hepatitis B virus infection in the United States: 2008 update. Clin. Gastroenterol. Hepatol. 2008, 6, 1315–1341, quiz 1286. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Q.; Lee, H.M. Antiviral therapy for chronic hepatitis B in pregnancy. Semin. Liver. Dis. 2013, 33, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Simsek Yavuz, S.; Unal, S. Antiviral treatment of COVID-19. Turk. J. Med. Sci. 2020, 50, 611–619. [Google Scholar] [CrossRef]
- Grein, J.; Ohmagari, N.; Shin, D.; Diaz, G.; Asperges, E.; Castagna, A.; Feldt, T.; Green, G.; Green, M.L.; Lescure, F.X.; et al. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N. Engl. J. Med. 2020, 382, 2327–2336. [Google Scholar] [CrossRef]
- Amirian, E.S.; Levy, J.K. Current knowledge about the antivirals remdesivir (GS-5734) and GS-441524 as therapeutic options for coronaviruses. One Health 2020, 9, 100128. [Google Scholar] [CrossRef]
- Nasrallah, S.; Nguyen, A.Q.; Hitchings, L.; Wang, J.Q.; Hamade, S.; Maxwell, G.L.; Khoury, A.; Gomez, L.M. Pharmacological treatment in pregnant women with moderate symptoms of coronavirus disease 2019 (COVID-19) pneumonia. J. Matern. Fetal. Neonatal. Med. 2022, 35, 5970–5977. [Google Scholar] [CrossRef]
- Maldarelli, G.A.; Savage, M.; Mazur, S.; Oxford-Horrey, C.; Salvatore, M.; Marks, K.M. Remdesivir Treatment for Severe COVID-19 in Third-Trimester Pregnancy: Case Report and Management Discussion. Open. Forum. Infect. Dis. 2020, 7, ofaa345. [Google Scholar] [CrossRef]
- Anderson, J.; Schauer, J.; Bryant, S.; Graves, C.R. The use of convalescent plasma therapy and remdesivir in the successful management of a critically ill obstetric patient with novel coronavirus 2019 infection: A case report. Case Rep. Womens Health 2020, 27, e00221. [Google Scholar] [CrossRef]
- McCoy, J.A.; Short, W.R.; Srinivas, S.K.; Levine, L.D.; Hirshberg, A. Compassionate use of remdesivir for treatment of severe coronavirus disease 2019 in pregnant women at a United States academic center. Am. J. Obstet. Gynecol. MFM 2020, 2, 100164. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Choudhary, A. Treatment With Remdesivir in Two Pregnant Patients With COVID-19 Pneumonia. Cureus 2021, 13, e14986. [Google Scholar] [CrossRef] [PubMed]
- Schuler-Faccini, L.; Sanseverino, M.; Vianna, F.; da Silva, A.A.; Larrandaburu, M.; Marcolongo-Pereira, C.; Abeche, A.M. Zika virus: A new human teratogen? Implications for women of reproductive age. Clin. Pharmacol. Ther. 2016, 100, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Simmons, C.P.; McPherson, K.; Van Vinh Chau, N.; Hoai Tam, D.T.; Young, P.; Mackenzie, J.; Wills, B. Recent advances in dengue pathogenesis and clinical management. Vaccine 2015, 33, 7061–7068. [Google Scholar] [CrossRef] [PubMed]
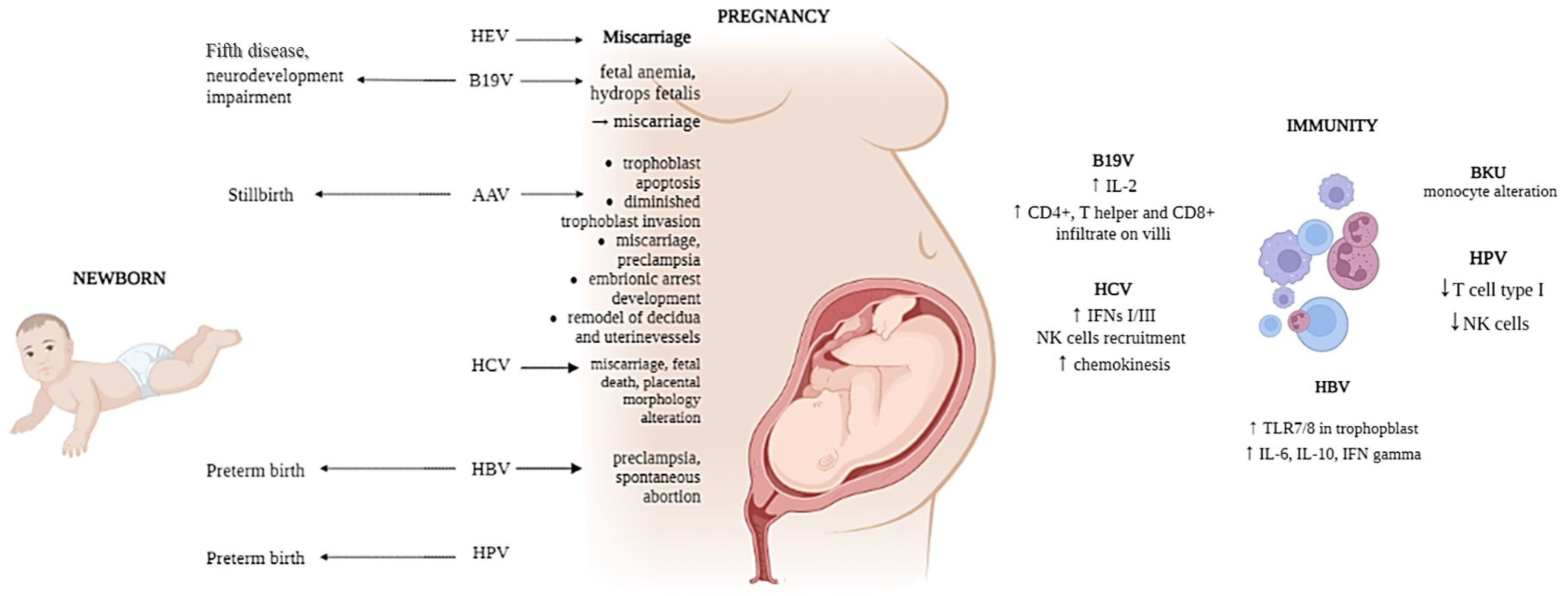
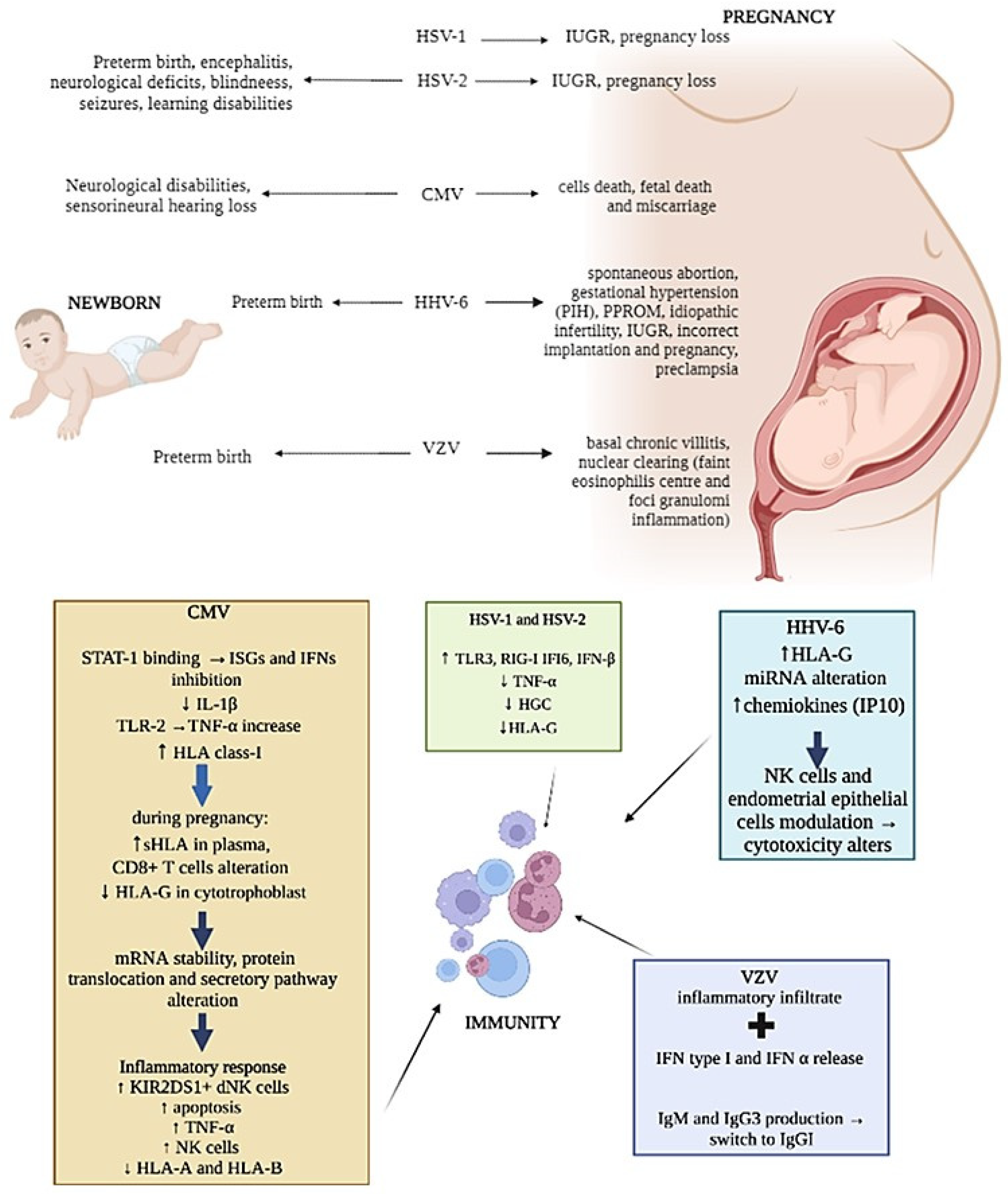
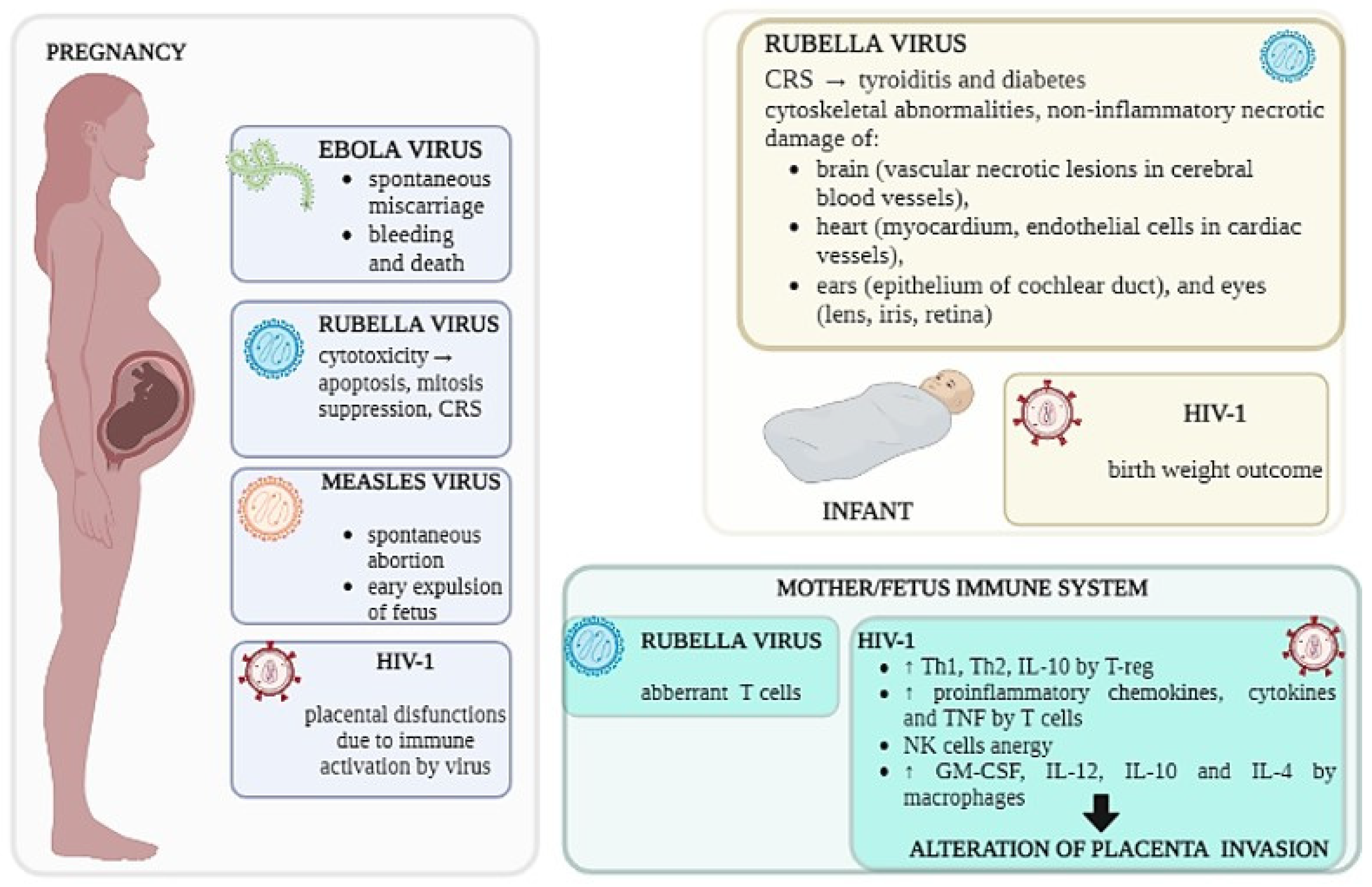
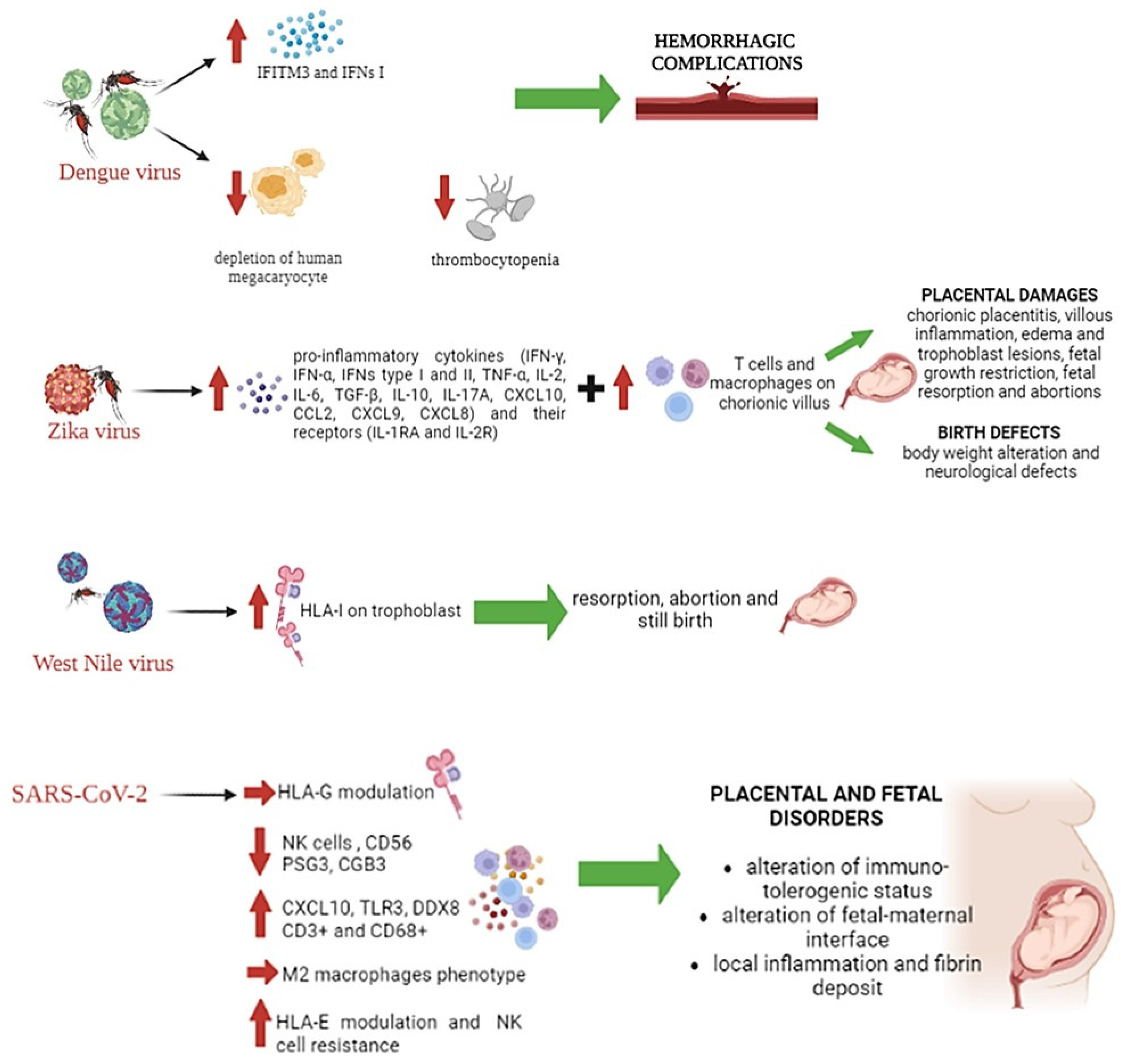
| Infection of Placenta without Infection of the Fetus | Fetal Infection without Placental Infection | Absence of Fetal and Placental Infection | Infection of Placenta and Fetus | |
|---|---|---|---|---|
| Microorganism interaction | Microorganisms reach the intervillous space of the maternal side on placenta. They do not spread to the fetus. | Microorganisms can cross directly through the chorionic villi, using pinocytosis or diaphysis mechanisms. | Interaction of microorganisms that might reach the fetus with placenta. | Microorganisms pass from the infected placenta to the fetal compartment through the chorionic villi, directly infecting fetal membranes and amniotic fluid. |
| Effects | The infection does not involve the fetus thanks to fetal defense mechanisms by placental macrophages and the local production of antibodies and cytokines. | Infection of maternal leukocytes and erythrocytes. | The fetus is protected from the attack of microbial agents by the maternal endothelial reticular system and circulating leukocytes. | Transplacental transmission of infection can lead to death, with a subsequent resorption of the embryo, intrauterine fetal death or premature term birth of infected infant. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beltrami, S.; Rizzo, S.; Schiuma, G.; Speltri, G.; Di Luca, D.; Rizzo, R.; Bortolotti, D. Gestational Viral Infections: Role of Host Immune System. Microorganisms 2023, 11, 1637. https://doi.org/10.3390/microorganisms11071637
Beltrami S, Rizzo S, Schiuma G, Speltri G, Di Luca D, Rizzo R, Bortolotti D. Gestational Viral Infections: Role of Host Immune System. Microorganisms. 2023; 11(7):1637. https://doi.org/10.3390/microorganisms11071637
Chicago/Turabian StyleBeltrami, Silvia, Sabrina Rizzo, Giovanna Schiuma, Giorgia Speltri, Dario Di Luca, Roberta Rizzo, and Daria Bortolotti. 2023. "Gestational Viral Infections: Role of Host Immune System" Microorganisms 11, no. 7: 1637. https://doi.org/10.3390/microorganisms11071637
APA StyleBeltrami, S., Rizzo, S., Schiuma, G., Speltri, G., Di Luca, D., Rizzo, R., & Bortolotti, D. (2023). Gestational Viral Infections: Role of Host Immune System. Microorganisms, 11(7), 1637. https://doi.org/10.3390/microorganisms11071637








