Parenteral Vaccination with a Live Brucella melitensis Mutant Protects against Wild-Type B. melitensis 16M Challenge
Abstract
1. Introduction
2. Materials and Methods
2.1. Brucella Strains
2.2. Mice
2.3. Evaluation of znBMZ’s and znBM-mC’s Attenuation in Macrophages
2.4. Assessment of znBM-mC’s Attenuation In Vivo
2.5. Evaluation of znBMZ’s Efficacy following Parenteral Vaccination
2.6. Evaluation of Cellular Immunity and Cytokine Analysis
2.7. Statistical Analysis
3. Results
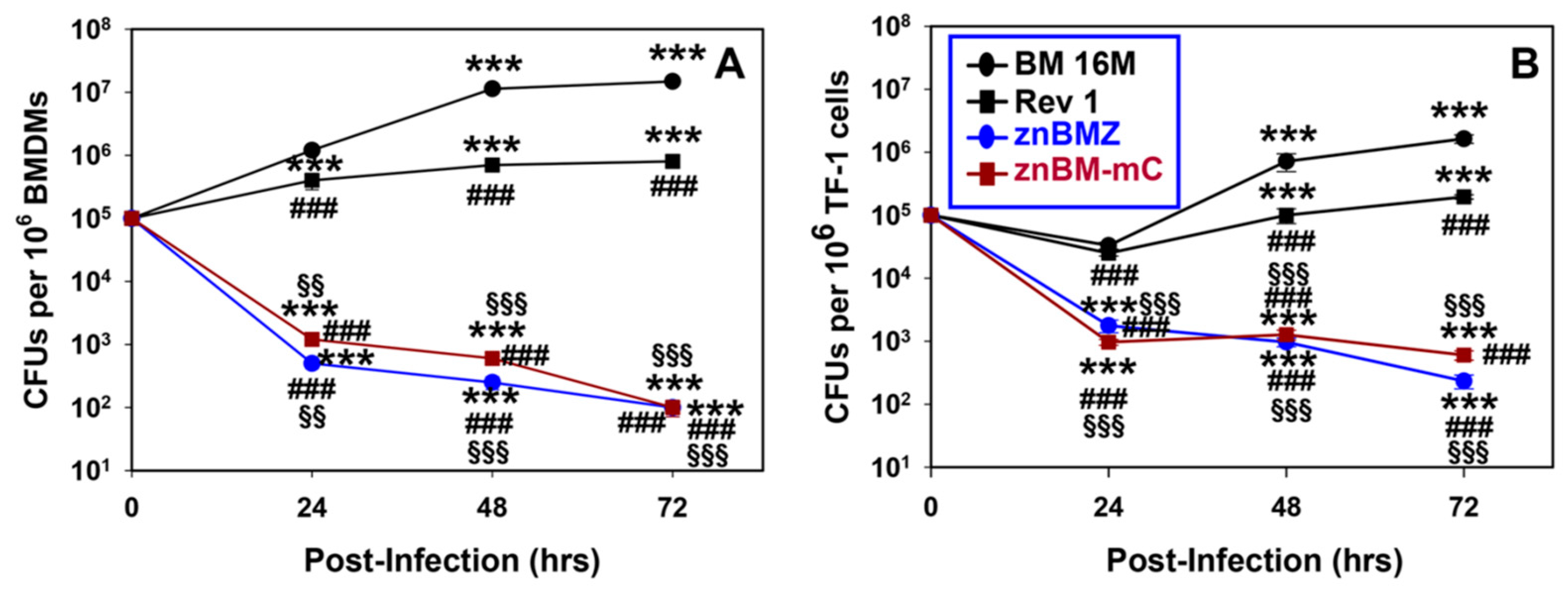
3.1. znBMZ and znBM-mC Are Attenuated in Mouse Macrophages and Human Myeloid Cells
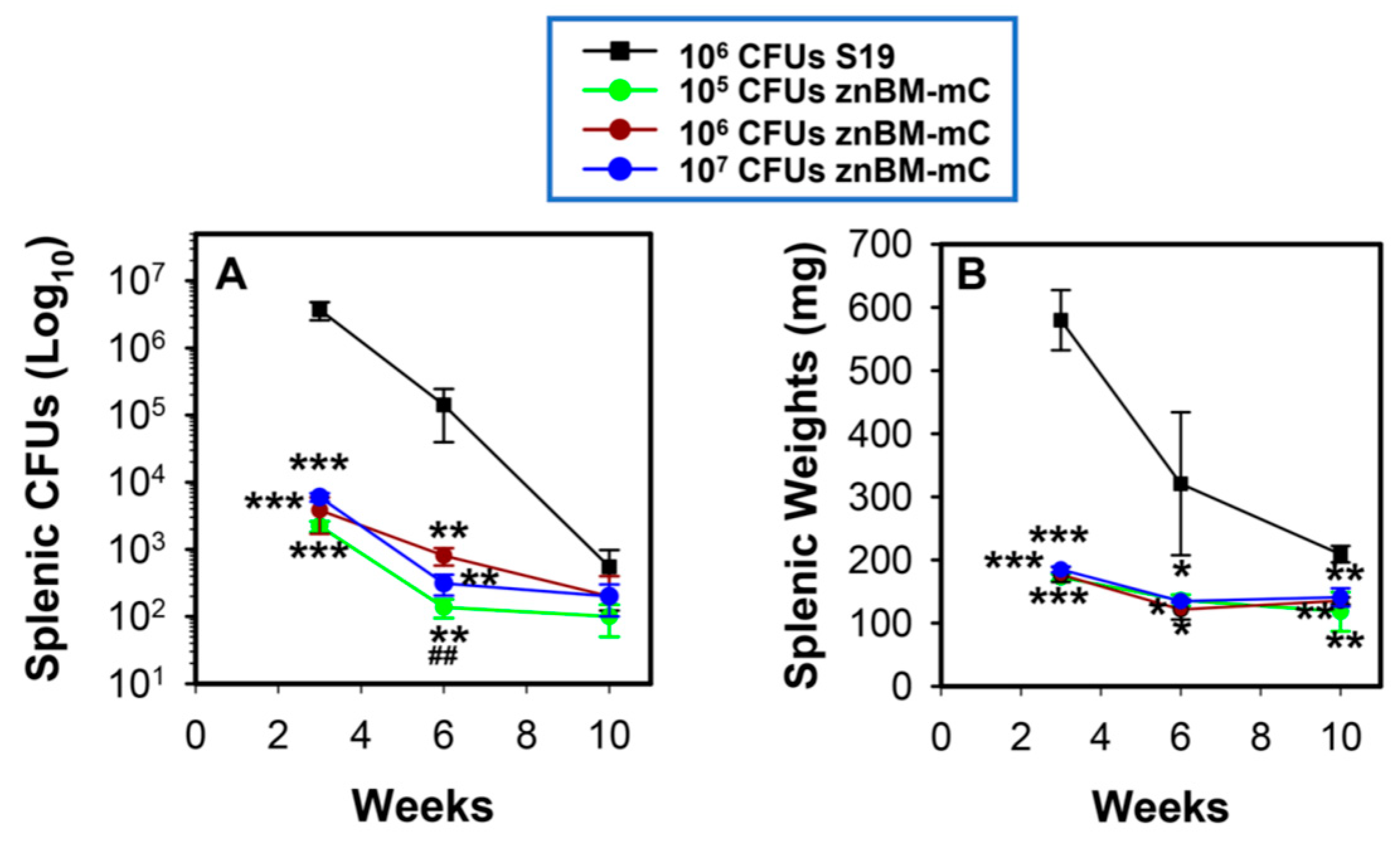
3.2. znBM-mC Is Attenuated In Vivo
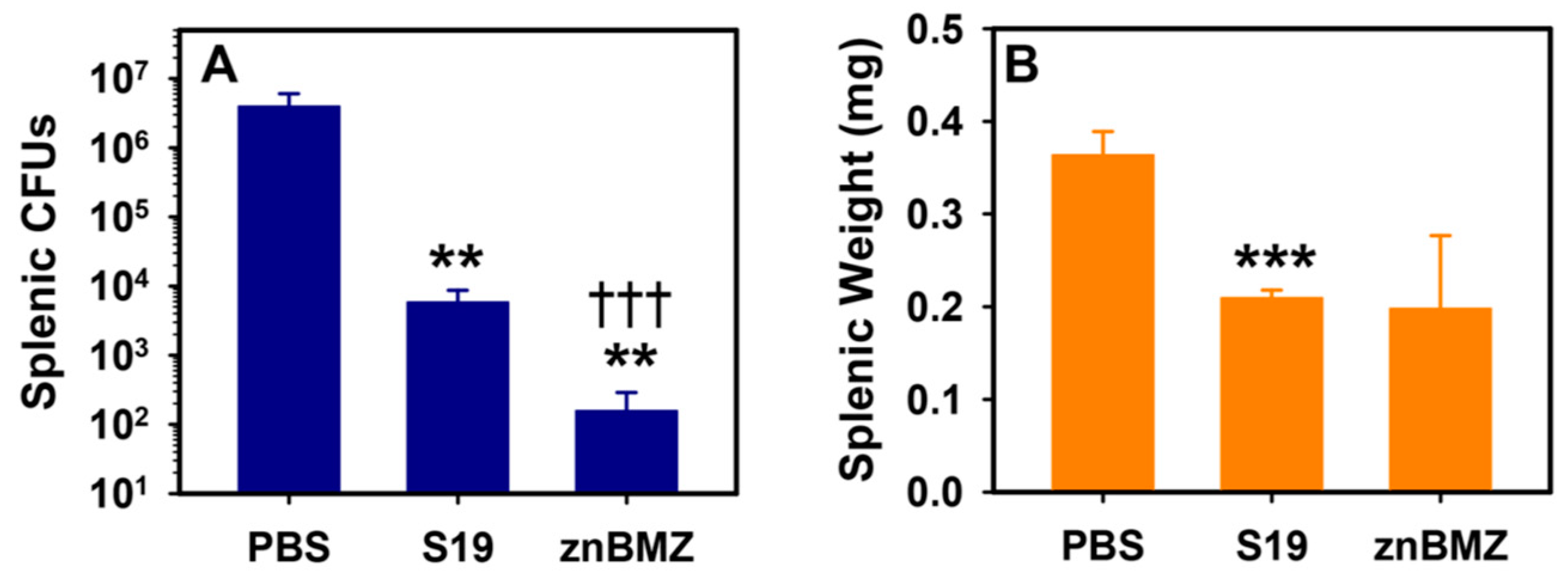
3.3. IP Vaccination of BALB/c Mice with znBMZ Confers Immune Protection
3.4. IP Vaccination with znBMZ Stimulates Induction of CD4+ and CD8+ T Effector Memory Cells (Tems)
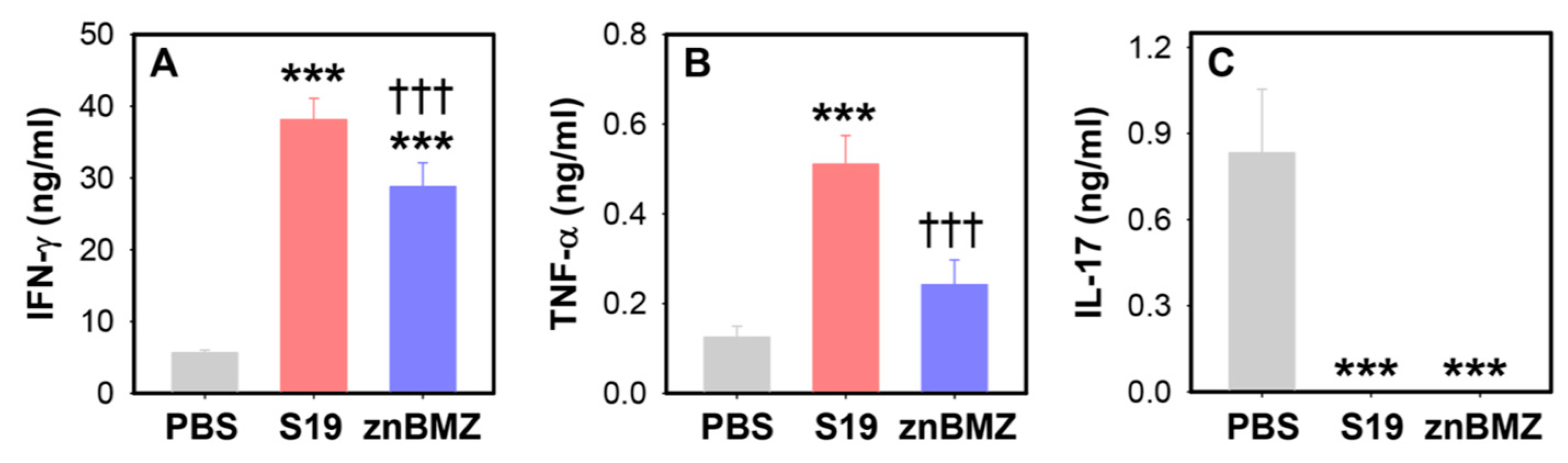
3.5. IP Vaccination with znBMZ Stimulates IFN-γ Production
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Whatmore, A.M.; Foster, J.T. Emerging diversity and ongoing expansion of the genus Brucella. Infect. Genet. Evol. 2021, 92, 104865. [Google Scholar] [CrossRef] [PubMed]
- Roop, R.M., 2nd; Barton, I.S.; Hopersberger, D.; Martin, D.W. Uncovering the Hidden Credentials of Brucella Virulence. Microbiol. Mol. Biol. Rev. 2021, 85, e00021-19. [Google Scholar] [CrossRef] [PubMed]
- Poester, F.P.; Samartino, L.E.; Santos, R.L. Pathogenesis and pathobiology of brucellosis in livestock. Rev. Sci. Tech. 2013, 32, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.C.; Palmer, M.V. Advancement of knowledge of Brucella over the past 50 years. Vet. Pathol. 2014, 51, 1076–1089. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, P.; Ficht, T.A.; Rice-Ficht, A.; Rossetti, C.A.; Adams, L.G. Pathogenesis and Immunobiology of Brucellosis. Am. J. Pathol. 2015, 185, 1505–1517. [Google Scholar] [CrossRef] [PubMed]
- Byndloss, M.X.; Tsolis, R.M. Brucella spp. virulence factors and immunity. Annu. Rev. Anim. Biosci. 2016, 4, 111–127. [Google Scholar] [CrossRef] [PubMed]
- Pascual, D.W.; Goodwin, Z.I.; Bhagyaraj, E.; Hoffman, C.; Yang, X. Activation of mucosal immunity as a novel therapeutic strategy for combating brucellosis. Front. Microbiol. 2022, 13, 1018165. [Google Scholar] [CrossRef]
- Dean, A.S.; Crump, L.; Greter, H.; Schelling, E.; Zinsstag, J. Global burden of human brucellosis: A systematic review of disease frequency. PLoS Negl. Trop. Dis. 2012, 6, e1865. [Google Scholar] [CrossRef]
- Rubach, M.P.; Halliday, J.E.; Cleaveland, S.; Crump, J.A. Brucellosis in low income and middle income countries. Curr. Opin. Infect. Dis. 2013, 26, 404–412. [Google Scholar] [CrossRef]
- Welburn, S.C.; Beange, I.; Ducrotoy, M.J.; Okello, A.L. The neglected zoonoses the case for integrated control and advocacy. Clin. Microbiol. Infect. 2015, 21, 433–443. [Google Scholar] [CrossRef]
- McDermott, J.; Grace, D.; Zinsstag, J. Economics of brucellosis impact and control in low-income countries. Rev. Sci. Tech. 2013, 32, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Kiiza, D.; Denagamage, T.; Serra, R.; Maunsell, F.; Kiker, G.; Benavides, B.; Hernandez, J.A. A systematic review of economic assessments for brucellosis control interventions in livestock populations. Prev. Vet. Med. 2023, 213, 105878. [Google Scholar] [CrossRef] [PubMed]
- Ariza, J.; Corredoira, J.; Pallares, R.; Viladrich, P.F.; Rufi, G.; Pujol, M.; Gudiol, F. Characteristics of and risk factors for relapse of brucellosis in humans. Clin. Infect. Dis. 1995, 20, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.P.; Mulder, M.; Gilman, R.H.; Smits, H.L. Human brucellosis. Lancet Infect. Dis. 2007, 7, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Mableson, H.E.; Okello, A.; Picozzi, K.; Welburn, S.C. Neglected zoonotic diseases-the long and winding road to advocacy. PLoS Negl. Trop. Dis. 2014, 8, e2800. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Cheers, C. Endogenous interleukin-12 is involved in resistance to Brucella abortus infection. Infect. Immun. 1995, 63, 1387–1390. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Cheers, C. Control of IL-12 and IFN-γ production in response to live or dead bacteria by TNF and other factors. J. Immunol. 1998, 161, 1447–1453. [Google Scholar] [CrossRef]
- Murphy, E.A.; Sathiyaseelan, J.; Parent, M.A.; Zou, B.; Baldwin, C.L. Interferon-γ is crucial for surviving a Brucella abortus infection in both resistant C57BL/6 and susceptible BALB/c mice. Immunology 2001, 103, 511–518. [Google Scholar] [CrossRef]
- Vitry, M.A.; De Trez, C.; Goriely, S.; Dumoutier, L.; Akira, S.; Ryffel, B.; Carlier, Y.; Letesson, J.J.; Muraille, E. Crucial role of gamma interferon-producing CD4+ Th1 cells but dispensable function of CD8+ T cell, B cell, Th2, and Th17 responses in the control of Brucella melitensis infection in mice. Infect. Immun. 2012, 80, 4271–4280. [Google Scholar] [CrossRef]
- Hanot Mambres, D.; Machelart, A.; Potemberg, G.; De Trez, C.; Ryffel, B.; Letesson, J.J.; Muraille, E. Identification of immune effectors essential to the control of primary and secondary intranasal infection with Brucella melitensis in mice. J. Immunol. 2016, 196, 3780–3793. [Google Scholar] [CrossRef]
- Demars, A.; Lison, A.; Machelart, A.; Van Vyve, M.; Potemberg, G.; Vanderwinden, J.M.; De Bolle, X.; Letesson, J.J.; Muraille, E. Route of Infection Strongly Impacts the Host-Pathogen Relationship. Front. Immunol. 2019, 10, 1589. [Google Scholar] [CrossRef] [PubMed]
- Dorneles, E.M.; Lima, G.K.; Teixeira-Carvalho, A.; Araújo, M.S.; Martins-Filho, O.A.; Sriranganathan, N.; Al Qublan, H.; Heinemann, M.B.; Lage, A.P. Immune Response of Calves Vaccinated with Brucella abortus S19 or RB51 and Revaccinated with RB51. PLoS ONE 2015, 10, e0136696. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.L.; Bowen, R.A.; Gonzalez-Juarrero, M. Cell mediated immune response in goats after experimental challenge with the virulent Brucella melitensis strain 16M and the reduced virulence strain Rev. 1. Vet. Immunol. Immunopathol. 2018, 202, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Boggiatto, P.M.; Schaut, R.G.; Olsen, S.C. Enhancing the detection of Brucella-specific CD4+ T cell responses in cattle via in vitro antigenic expansion and restimulation. Front. Immunol. 2020, 11, 1944. [Google Scholar] [CrossRef]
- Rodriguez-Zapata, M.; Salmeron, I.; Manzano, L.; Salmeron, O.J.; Prieto, A.; Alvarez-Mon, M. Defective interferon-gamma production by T-lymphocytes from patients with acute brucellosis. Eur. J. Clin. Investig. 1996, 26, 136–140. [Google Scholar] [CrossRef]
- Rafiei, A.; Ardestani, S.K.; Kariminia, A.; Keyhani, A.; Mohraz, M.; Amirkhani, A. Dominant Th1 cytokine production in early onset of human brucellosis followed by switching towards Th2 along prolongation of disease. J. Infect. 2006, 53, 315–324. [Google Scholar] [CrossRef]
- Hedayatizadeh-Omran, A.; Rafiei, A.; Hajilooi, M.; Haghshenas, M. Interferon-γ low producer genotype +5644 over presented in patients with focal brucellosis. Pak. J. Biol. Sci. 2010, 13, 1036–1041. [Google Scholar] [CrossRef][Green Version]
- Atluri, V.L.; Xavier, M.N.; de Jong, M.F.; den Hartigh, A.B.; Tsolis, R.M. Interactions of the human pathogenic Brucella species with their hosts. Annu. Rev. Microbiol. 2011, 65, 523–541. [Google Scholar] [CrossRef]
- Zinsstag, J.; Schelling, E.; Roth, F.; Bonfoh, B.; de Savigny, D.; Tanner, M. Human benefits of animal interventions for zoonosis control. Emerg. Infect. Dis. 2007, 13, 527–531. [Google Scholar] [CrossRef]
- Kim, S.; Watanabe, K.; Shirahata, T.; Watarai, M. Zinc uptake system (znuA locus) of Brucella abortus is essential for intracellular survival and virulence in mice. J. Vet. Med. Sci. 2004, 66, 1059–1063. [Google Scholar] [CrossRef]
- Yang, X.; Becker, T.; Jun, S.M.; Walters, N.; Pascual, D.W. Deletion of znuA virulence factor attenuates Brucella abortus and confers protection against wild-type challenge. Infect. Immun. 2006, 74, 3874–3879. [Google Scholar] [CrossRef][Green Version]
- Roop, R.M. Metal acquisition and virulence in Brucella. Anim. Health Res. Rev. 2012, 13, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Loisel-Meyer, S.; Jiménez de Bagüés, M.P.; Bassères, E.; Dornand, J.; Köhler, S.; Liautard, J.P.; Jubier-Maurin, V. Requirement of norD for Brucella suis virulence in a murine model of in vitro and in vivo infection. Infect. Immun. 2006, 74, 1973–1976. [Google Scholar] [CrossRef]
- Yang, X.; Clapp, B.; Thornburg, T.; Hoffman, C.; Pascual, D.W. Vaccination with a ΔnorD ΔznuA Brucella abortus mutant confers potent protection against virulent challenge. Vaccine 2016, 34, 5290–5297. [Google Scholar] [CrossRef]
- Wang, H.; Hoffman, C.; Yang, X.; Clapp, B.; Pascual, D.W. Targeting resident memory T cell immunity culminates in pulmonary and systemic protection against Brucella infection. PLoS Pathog. 2020, 16, e1008176. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, Z.I.; Yang, X.; Hoffman, C.; Pascual, D.W. Live mucosal vaccination stimulates potent protection via varied CD4+ and CD8+ T cell subsets against wild-type Brucella melitensis 16M challenge. Front. Immunol. 2022, 13, 995327. [Google Scholar] [CrossRef] [PubMed]
- Clapp, B.; Yang, X.; Thornburg, T.; Walters, N.; Pascual, D.W. Nasal vaccination stimulates CD8+ T cells for potent protection against mucosal Brucella melitensis challenge. Immunol. Cell Biol. 2016, 94, 496–508. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Clapp, B.; Hoffman, C.; Yang, X.; Pascual, D.W. A single nasal dose vaccination with a Brucella abortus mutant potently protects against pulmonary infection. J. Immunol. 2023, 210, 1576–1588. [Google Scholar] [CrossRef]
- Olsen, S.C.; Stoffregen, W.S. Essential role of vaccines in brucellosis control and eradication programs for livestock. Expert Rev. Vaccines 2005, 4, 915–928. [Google Scholar] [CrossRef]
- Rossetti, C.A.; Arenas-Gamboa, A.M.; Maurizio, E. Caprine brucellosis: A historically neglected disease with significant impact on public health. PLoS Negl. Trop. Dis. 2017, 11, e0005692. [Google Scholar] [CrossRef]
- Darbandi, A.; Alamdary, S.Z.; Koupaei, M.; Ghanavati, R.; Heidary, M.; Talebi, M. Evaluation of immune responses to Brucella vaccines in mouse models: A systematic review. Front. Vet. Sci. 2022, 9, 903890. [Google Scholar] [CrossRef] [PubMed]
- Lubroth, J.; Rweyemamu, M.M.; Viljoen, G.; Diallo, A.; Dungu, B.; Amanfu, W. Veterinary vaccines and their use in developing countries. Rev. Sci. Tech. 2007, 26, 179–201. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.R.; Cotrim de Almeida, J.V.F.; Cardoso de Oliveira, I.R.; Faria de Oliveira, L.; Pereira, L.J.; Zangerônimo, M.G.; Lage, A.P.; Dorneles, E.M.S. Occupational exposure to Brucella spp.: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2020, 14, e0008164. [Google Scholar] [CrossRef] [PubMed]
- Buswell, M.L.; Hourigan, M.; Nault, A.J.; Bender, J.B. Needlestick injuries in agriculture workers and prevention programs. J. Agromedicine 2016, 21, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.C.; Bricker, B.; Palmer, M.V.; Jensen, A.E.; Cheville, N.F. Responses of cattle to two dosages of Brucella abortus strain RB51: Serology, clearance and efficacy. Res. Vet. Sci. 1999, 66, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Dadar, M.; Shahali, Y.; Whatmore, A.M. Human brucellosis caused by raw dairy products: A review on the occurrence, major risk factors and prevention. Int. J. Food Microbiol. 2019, 292, 39–47. [Google Scholar] [CrossRef]
- Clapp, B.; Skyberg, J.A.; Yang, X.; Thornburg, T.; Walters, N.; Pascual, D.W. Protective live oral brucellosis vaccines stimulate Th1 and Th17 cell responses. Infect. Immun. 2011, 79, 4165–4174. [Google Scholar] [CrossRef]
- Sakai, S.; Kauffman, K.D.; Schenkel, J.M.; McBerry, C.C.; Mayer-Barber, K.D.; Masopust, D.; Barber, D.L. Cutting edge: Control of Mycobacterium tuberculosis infection by a subset of lung parenchyma-homing CD4 T cells. J. Immunol. 2014, 192, 2965–2969. [Google Scholar] [CrossRef]
- Sallin, M.A.; Sakai, S.; Kauffman, K.D.; Young, H.A.; Zhu, J.; Barber, D.L. Th1 Differentiation Drives the Accumulation of Intravascular, Non-protective CD4 T Cells during Tuberculosis. Cell Rep. 2017, 18, 3091–3104. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, X.; Goodwin, Z.I.; Bhagyaraj, E.; Hoffman, C.; Pascual, D.W. Parenteral Vaccination with a Live Brucella melitensis Mutant Protects against Wild-Type B. melitensis 16M Challenge. Microorganisms 2024, 12, 169. https://doi.org/10.3390/microorganisms12010169
Yang X, Goodwin ZI, Bhagyaraj E, Hoffman C, Pascual DW. Parenteral Vaccination with a Live Brucella melitensis Mutant Protects against Wild-Type B. melitensis 16M Challenge. Microorganisms. 2024; 12(1):169. https://doi.org/10.3390/microorganisms12010169
Chicago/Turabian StyleYang, Xinghong, Zakia I. Goodwin, Ella Bhagyaraj, Carol Hoffman, and David W. Pascual. 2024. "Parenteral Vaccination with a Live Brucella melitensis Mutant Protects against Wild-Type B. melitensis 16M Challenge" Microorganisms 12, no. 1: 169. https://doi.org/10.3390/microorganisms12010169
APA StyleYang, X., Goodwin, Z. I., Bhagyaraj, E., Hoffman, C., & Pascual, D. W. (2024). Parenteral Vaccination with a Live Brucella melitensis Mutant Protects against Wild-Type B. melitensis 16M Challenge. Microorganisms, 12(1), 169. https://doi.org/10.3390/microorganisms12010169



