Potential Effects of Essential Oil from Plinia cauliflora (Mart.) Kausel on Leishmania: In Vivo, In Vitro, and In Silico Approaches
Abstract
1. Introduction
2. Materials and Methods
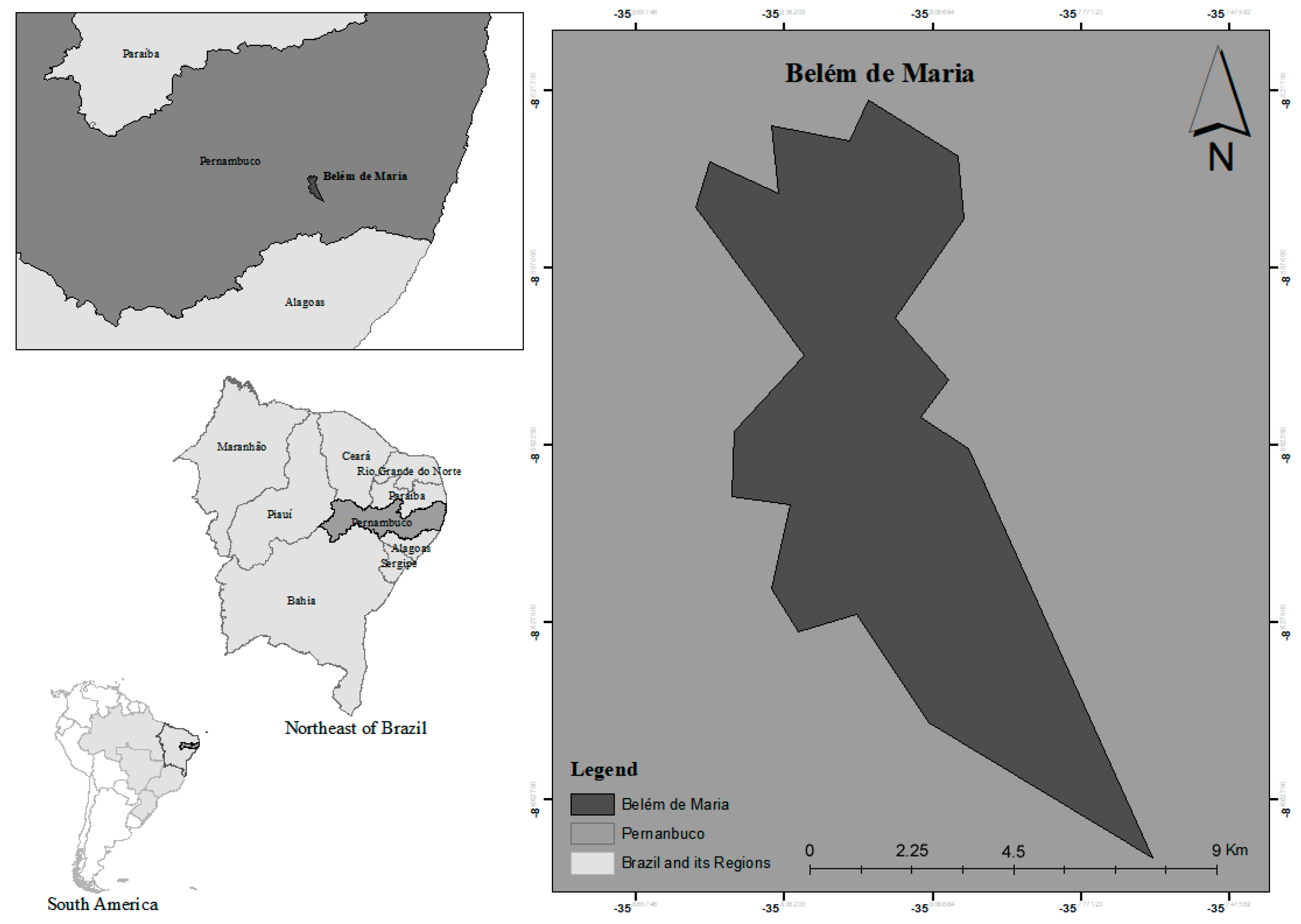
2.1. Plant Material
2.2. Isolation and Chemical Characterization of the Essential Oil from P. cauliflora (PCEO)
2.3. Cytotoxicity in Mammalian Cells
2.4. Leishmanicidal Activity of PCEO on Leishmania amazonensis and Leishmania braziliensis
2.5. Scanning Electron Microscopy
2.6. In Silico ADMET Analysis
2.7. Carrageenan-Induced Paw Edema
2.8. Xylol-Induced Ear Edema
2.9. Carrageenan-Induced Peritonitis
2.10. Statistical Analysis
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Ramos, E.H.; Moraes, M.M.; Nerys, L.L.d.A.; Nascimento, S.C.; Militão, G.C.; de Figueiredo, R.C.; da Câmara, C.A.; Silva, T.G. Chemical composition, leishmanicidal and cytotoxic activities of the essential oils from Mangifera indica L. var. Rosa and Espada. BioMed Res. Int. 2014, 2014, 734946. [Google Scholar] [CrossRef] [PubMed]
- Tedla, D.G.; Bariagabr, F.H.; Abreha, H.H. Incidence and trends of leishmaniasis and its risk factors in Humera, Western Tigray. J. Parasitol. Res. 2018, 2018, 8463097. [Google Scholar]
- Ribeiro, T.G.; Chávez-Fumagalli, M.A.; Valadares, D.G.; Franca, J.R.; Lage, P.S.; Duarte, M.C.; Andrade, P.H.; Martins, V.T.; Costa, L.E.; Arruda, A.L. Antileishmanial activity and cytotoxicity of Brazilian plants. Exp. Parasitol. 2014, 143, 60–68. [Google Scholar] [CrossRef]
- Uliana, S.R.; Trinconi, C.T.; Coelho, A.C. Chemotherapy of leishmaniasis: Present challenges. Parasitology 2018, 145, 464–480. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, S.V.C.B.; Costa, C.H.N. Treatment of cutaneous leishmaniasis with thermotherapy in Brazil: An efficacy and safety study. An. Bras. Dermatol. 2018, 93, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Holanda, V.N.; da Silva, W.V.; do Nascimento, P.H.; Oliveira, R.N.; de Menezes Lima, V.L.; de Figueiredo, R.C.B.Q. Desafios e perspectivas no tratamento da Leishmaniose Tegumentar: Revisão de literatura. Rev. Interfaces Saúde Humanas E Tecnol. 2019, 6, 140–157. [Google Scholar]
- Marques, S.A.; Merlotto, M.R.; Ramos, P.M.; Marques, M.E.A. American tegumentary leishmaniasis: Severe side effects of pentavalent antimonial in a patient with chronic renal failure. An. Bras. Dermatol. 2019, 94, 355–357. [Google Scholar] [CrossRef]
- Taslimi, Y.; Agbajogu, C.; Brynjolfsson, S.F.; Masoudzadeh, N.; Mashayekhi, V.; Gharibzadeh, S.; Östensson, M.; Nakka, S.S.; Mizbani, A.; Rafati, S.; et al. Profiling inflammatory response in lesions of cutaneous leishmaniasis patients using a non-invasive sampling method combined with a high-throughput protein detection assay. Cytokine 2020, 130, 155056. [Google Scholar] [CrossRef]
- Arevalo, I.; Ward, B.; Miller, R.; Meng, T.-C.; Najar, E.; Alvarez, E.; Matlashewski, G.; Alejandro, L.-C. Successful Treatment of Drug-Resistant Cutaneous Leishmaniasis in Humans by Use of Imiquimod, an Immunomodulator. Clin. Infect. Dis. 2001, 33, 1847–1851. [Google Scholar] [CrossRef]
- Petrovska, B.B. Historical review of medicinal plants’ usage. Pharmacogn. Rev. 2012, 6, 1. [Google Scholar] [CrossRef]
- ul-Hassan, S.S.; Jin, H.-z.; Abu-Izneid, T.; Rauf, A.; Ishaq, M.; Suleria, H.A.R. Stress-driven discovery in the natural products: A gateway towards new drugs. Biomed. Pharmacother. 2019, 109, 459–467. [Google Scholar]
- Tietbohl, L.A.; Lima, B.G.; Fernandes, C.P.; Santos, M.G.; Silva, F.E.; Denardin, E.L.; Bachinski, R.; Alves, G.G.; Silva-Filho, M.V.; Rocha, L. Comparative study and anticholinesterasic evaluation of essential oils from leaves, stems and flowers of Myrciaria floribunda (H. West ex Willd.) O. Berg. Lat. Am. J. Pharm. 2012, 31, 637–641. [Google Scholar]
- Weli, A.; Al-Kaabi, A.; Al-Sabahi, J.; Said, S.; Hossain, M.A.; Al-Riyami, S. Chemical composition and biological activities of the essential oils of Psidium guajava leaf. J. King Saud Univ. Sci. 2018, 31, 993–998. [Google Scholar] [CrossRef]
- Souza, L.I.O.; Bezzera-Silva, P.C.; Navarro, D.M.d.A.F.; da Silva, A.G.; dos Santos Correia, M.T.; da Silva, M.V.; de Figueiredo, R.C.B.Q. The chemical composition and trypanocidal activity of volatile oils from Brazilian Caatinga plants. Biomed. Pharmacother. 2017, 96, 1055–1064. [Google Scholar]
- Santos, J.F.S.; Rocha, J.E.; Bezerra, C.F.; do Nascimento Silva, M.K.; de Matos, Y.M.L.S.; de Freitas, T.S.; dos Santos, A.T.L.; da Cruz, R.P.; Machado, A.J.T.; Rodrigues, T.H.S. Chemical composition, antifungal activity and potential anti-virulence evaluation of the Eugenia uniflora essential oil against Candida spp. Food Chem. 2018, 261, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Salem, N.; Kefi, S.; Tabben, O.; Ayed, A.; Jallouli, S.; Feres, N.; Hammami, M.; Khammassi, S.; Hrigua, I.; Nefisi, S. Variation in chemical composition of Eucalyptus globulus essential oil under phenological stages and evidence synergism with antimicrobial standards. Ind. Crops Prod. 2018, 124, 115–125. [Google Scholar]
- Stefanello, M.É.A.; Pascoal, A.C.; Salvador, M.J. Essential oils from neotropical Myrtaceae: Chemical diversity and biological properties. Chem. Biodivers. 2011, 8, 73–94. [Google Scholar] [CrossRef]
- Baseggio, A.M.; Nuñez, C.E.C.; Dragano, N.R.V.; Lamas, C.A.; de Campos Braga, P.A.; Lenquiste, S.A.; Reyes, F.G.R.; Cagnon, V.H.A.; Júnior, M.R.M. Jaboticaba peel extract decrease autophagy in white adipose tissue and prevents metabolic disorders in mice fed with a high-fat diet. PharmaNutrition 2018, 6, 147–156. [Google Scholar] [CrossRef]
- Muylder, G.; Ang, K.K.; Chen, S.; Arkin, M.R.; Engel, J.C.; McKerrow, J.H. A screen against Leishmania intracellular amastigotes: Comparison to a promastigote screen and identification of a host cell-specific hit. PLoS Negl. Trop. Dis. 2011, 5, e1253. [Google Scholar] [CrossRef]
- Assis, P.; Cypriano Dutra, R.; Amarante, C.B.d.; Afonso Miranda Chaves, M.d.G.; Moreira, C.P.d.S.; Brandão, M.A.F.; Raposo, N.R.B. Plinia cauliflora (Mart.) Kausel: Toxicological assays, biological activities, and elemental analysis of organic compounds. Nat. Prod. Res. 2019, 35, 1727–1731. [Google Scholar] [CrossRef]
- Silva, V.P.; Alves, C.C.F.; Miranda, M.L.D.; Bretanha, L.C.; Balleste, M.P.; Micke, G.A.; Silveira, E.V.; Martins, C.H.G.; Ambrosio, M.A.L.V.; de Souza Silva, T. Chemical composition and in vitro leishmanicidal, antibacterial and cytotoxic activities of essential oils of the Myrtaceae family occurring in the Cerrado biome. Ind. Crops Prod. 2018, 123, 638–645. [Google Scholar]
- Gasparotto Junior, A.; de Souza, P.; Lívero, F.A.d.R. Plinia cauliflora (Mart.) Kausel: A comprehensive ethnopharmacological review of a genuinely Brazilian species. J. Ethnopharmacol. 2019, 245, 112169. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, F.; Carvalho, A.F.S.; de Castro Marques, E.; Ribeiro, R.M.; Borges, A.C.R.; da Rocha Borges, M.O. Antidiarrhoeal and antispasmodic activity of leaves of Syzygium cumini L. (Myrtaceae) mediated through calcium channel blockage. Afr. J. Pharm. Pharmacol. 2018, 12, 11–18. [Google Scholar]
- Sá, S.; Chaul, L.T.; Alves, V.F.; Fiuza, T.S.; Tresvenzol, L.M.; Vaz, B.G.; Ferri, P.H.; Borges, L.L.; Paula, J.R. Phytochemistry and antimicrobial activity of Campomanesia adamantium. Rev. Bras. Farmacogn. 2018, 28, 303–311. [Google Scholar] [CrossRef]
- Sarikurkcu, C.; Ozer, M.S.; Calli, N.; Popović-Djordjević, J. Essential oil composition and antioxidant activity of endemic Marrubium parviflorum subsp. oligodon. Ind. Crops Prod. 2018, 119, 209–213. [Google Scholar]
- Paula, P.; de Oliveira Lemos, A.S.; Campos, L.M.; Ferreira, T.G.; de Souza, T.F.; Queiroz, L.S.; Guedes, M.C.M.R.; Martins, M.M.; Goulart Filho, L.R.; Macedo, G.C. Pharmacological investigation of antioxidant and anti-inflammatory activities of leaves and branches extracts from Plinia cauliflora (Jaboticaba). J. Ethnopharmacol. 2021, 280, 114463. [Google Scholar] [CrossRef]
- Freitas, T.P.; Taver, I.B.; Spricigo, P.C.; do Amaral, L.B.; Purgatto, E.; Jacomino, A.P. Volatile Compounds and Physicochemical Quality of Four Jabuticabas (Plinia sp.). Molecules 2020, 25, 4543. [Google Scholar]
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectrometry; Allured Publishing Corporation: Carol Stream, IL, USA, 2007; Volume 456. [Google Scholar]
- Medeiros, M.d.G.F.; Da Silva, A.C.; Citó, A.M.d.G.L.; Borges, A.R.; De Lima, S.G.; Lopes, J.A.D.; Figueiredo, R.C.B.Q. In Vitro antileishmanial activity and cytotoxicity of essential oil from Lippia sidoides Cham. Parasitol. Int. 2011, 60, 237–241. [Google Scholar] [CrossRef]
- Aliança, A.S.d.S.; Anjos, K.F.L.d.; De Vasconcelos Reis, T.N.; Higino, T.M.M.; Brelaz-de-Castro, M.C.A.; Bianco, É.M.; De Figueiredo, R.C.B.Q. The In Vitro Biological Activity of the Brazilian Brown Seaweed Dictyota mertensii against Leishmania amazonensis. Molecules 2014, 19, 14052–14065. [Google Scholar]
- Winter, C.A.; Risley, E.A.; Nuss, G.W. Carrageenin-induced edema in hind paw of the rat as an assay for antiinflammatory drugs. Proc. Soc. Exp. Biol. Med. 1962, 111, 544–547. [Google Scholar] [CrossRef]
- Rocha, F.F.; Neves, E.; Costa, E.A.; Matos, L.G.; Müller, A.H.; Guilhon, G.; Cortes, W.S.; Vanderlinde, F.A. Evaluation of antinociceptive and antiinflammatory effects of Croton pullei var. glabrior Lanj.(Euphorbiaceae). Rev. Bras. Farmacogn. 2008, 18, 344–349. [Google Scholar] [CrossRef]
- Souza, G.E.; Ferreira, S. Blockade by antimacrophage serum of the migration of PMN neutrophils into the inflamed peritoneal cavity. Agents Actions 1985, 17, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, J.C.; Sertié, J.A.; Barbosa, M.V.; Patrício, K.C.; Caputo, L.R.; Sarti, S.J.; Ferreira, L.P.; Bastos, J.K. Anti-inflammatory activity of the crude extract from the fruits of Pterodon emarginatus Vog. J. Ethnopharmacol. 1999, 64, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Apel, M.A.; Lima, M.E.; Sobral, M.; Young, M.C.M.; Cordeiro, I.; Schapoval, E.E.; Henriques, A.T.; Moreno, P.R.H. Anti-inflammatory activity of essential oil from leaves of Myrciaria tenella and Calycorectes sellowianus. Pharm. Biol. 2010, 48, 433–438. [Google Scholar] [CrossRef] [PubMed]
- de Moraes, Â.A.; de Jesus Pereira Franco, C.; Ferreira, O.O.; Varela, E.L.; do Nascimento, L.D.; Cascaes, M.M.; da Silva, D.R.; Percário, S.; de Oliveira, M.S.; de Aguiar Andrade, E.H. Myrcia paivae O. Berg (Myrtaceae) Essential oil, first study of the chemical composition and antioxidant potential. Molecules 2022, 27, 5460. [Google Scholar] [CrossRef] [PubMed]
- Saad, N.Y.; Muller, C.D.; Lobstein, A. Major bioactivities and mechanism of action of essential oils and their components. Flavour Fragr. J. 2013, 28, 269–279. [Google Scholar] [CrossRef]
- Fidyt, K.; Fiedorowicz, A.; Strządała, L.; Szumny, A. β-caryophyllene and β-caryophyllene oxide—Natural compounds of anticancer and analgesic properties. Cancer Med. 2016, 5, 3007–3017. [Google Scholar]
- Coté, H.; Boucher, M.-A.; Pichette, A.; Legault, J. Anti-inflammatory, antioxidant, antibiotic, and cytotoxic activities of Tanacetum vulgare L. essential oil and its constituents. Medicines 2017, 4, 34. [Google Scholar] [CrossRef]
- Ishikawa, T.; dos Santos Donatini, R.; Diaz, I.E.C.; Yoshida, M.; Bacchi, E.M.; Kato, E.T.M. Evaluation of gastroprotective activity of Plinia edulis (Vell.) Sobral (Myrtaceae) leaves in rats. J. Ethnopharmacol. 2008, 118, 527–529. [Google Scholar]
- Apel, M.A.; Sobral, M.; Zuanazzi, J.å.; Henriques, A.T. Essential oil composition of four Plinia species (Myrtaceae). Flavour Fragr. J. 2006, 21, 565–567. [Google Scholar] [CrossRef]
- Xu, X.; Tang, Z.; Liang, Y. Comparative analysis of plant essential oils by GC-MS coupled with integrated chemometric resolution methods. Anal. Methods 2010, 2, 359–367. [Google Scholar] [CrossRef]
- Stashenko, E.E.; Jaramillo, B.E.; Martínez, J.R. Comparación de la composición química y de la actividad antioxidante in vitro de los metabolitos secundarios volátiles de plantas de la familia Verbenaceae. Rev. Acad. Colomb. Cienc. 2003, 27, 579–597. [Google Scholar] [CrossRef]
- Pinheiro, P.F.; Queiroz, V.T.D.; Rondelli, V.M.; Costa, A.V.; Marcelino, T.D.P.; Pratissoli, D. Insecticidal activity of citronella grass essential oil on Frankliniella schultzei and Myzus persicae. Ciênc. E Agrotecnol. 2013, 37, 138–144. [Google Scholar]
- Tchoumbougnang, F.; Zollo, P.A.; Boyom, F.F.; Nyegue, M.A.; Bessière, J.M.; Menut, C. Aromatic plants of tropical Central Africa. XLVIII. Comparative study of the essential oils of four Hyptis species from Cameroon: H. lanceolata Poit., H. pectinata (L.) Poit., H. spicigera Lam. and H. suaveolens Poit. Flavour Fragr. J. 2005, 20, 340–343. [Google Scholar] [CrossRef]
- Nagappan, T.; Ramasamy, P.; Vairappan, C.S. Chemotaxonomical markers in essential oil of Murraya koenigii. Nat. Prod. Commun. 2012, 7, 1934578X1200701034. [Google Scholar] [CrossRef]
- Zachariah, T.J.; Leela, N.K.; Maya, K.M.; Rema, J.; Mathew, P.A.; Vipin, T.M.; Krishnamoorthy, B. Chemical composition of leaf oils of Myristica beddomeii (King), Myristica fragrans (Houtt.) and Myristica malabarica (Lamk.). J. Spices Aromat. Crops 2008, 17, 10–15. [Google Scholar]
- Dugo, P.; Mondello, L.; Zappia, G.; Bonaccorsi, I.; Cotroneo, A.; Russo, M.T. The Composition of the Volatile Fraction and the Enantiomeric Distribution of Five Volatile Components of Faustrime Oil (Monocitrus australatica x Fortunella sp. × Citrus urantifolia). J. Essent. Oil Res. 2004, 16, 328–333. [Google Scholar] [CrossRef]
- Shellie, R.; Marriott, P.; Zappia, G.; Mondello, L.; Dugo, G. Interactive use of linear retention indices on polar and apolar columns with an MS-library for reliable characterization of Australian tea tree and other Melaleuca sp. oils. J. Essent. Oil Res. 2003, 15, 305–312. [Google Scholar]
- Babushok, V.I.; Linstrom, P.J.; Zenkevich, I.G. Retention indices for frequently reported compounds of plant essential oils. J. Phys. Chem. Ref. Data 2011, 40, 4. [Google Scholar] [CrossRef]
- Mondello, L.; Zappia, G.; Cotroneo, A.; Bonaccorsi, I.; Chowdhury, J.U.; Yusuf, M.; Dugo, G. Studies on the essential oil-bearing plants of Bangladesh. Part VIII. Composition of some Ocimum oils O. basilicum L. var. purpurascens; O. sanctum L. green; O. sanctum L. purple; O. americanum L., citral type; O. americanum L., camphor type. Flavour Fragr. J. 2002, 17, 335–340. [Google Scholar]
- Sharifiar, F.; Yassa, N.; Mozaffarian, V. Bioactivity of major components from the seeds of Bunium persicum (Boiss.) Fedtch. Pak. J. Pharm. Sci. 2010, 23, 300–304. [Google Scholar]
- Angioni, A.; Barra, A.; Coroneo, V.; Dessi, S.; Cabras, P. Chemical composition, seasonal variability, and antifungal activity of Lavandula stoechas L. ssp. stoechas essential oils from stem/leaves and flowers. J. Agric. Food Chem. 2006, 54, 4364–4370. [Google Scholar] [CrossRef] [PubMed]
- Hudaib, M.; Aburjai, T. Volatile components of Thymus vulgaris L. from wild-growing and cultivated plants in Jordan. Flavour Fragr. J. 2007, 22, 322–327. [Google Scholar] [CrossRef]
- Asuming, W.A.; Beauchamp, P.S.; Descalzo, J.T.; Dev, B.C.; Dev, V.; Frost, S.; Ma, C.W. Essential oil composition of four Lomatium Raf. species and their chemotaxonomy. Biochem. Syst. Ecol. 2005, 33, 17–26. [Google Scholar] [CrossRef]
- Zhao, C.; Zeng, Y.; Wan, M.; Li, R.; Liang, Y.; Li, C.; Zeng, Z.; Chau, F.-T. Comparative analysis of essential oils from eight herbal medicines with pungent flavor and cool nature by GC-MS and chemometric resolution methods. J. Sep. Sci. 2009, 32, 660–670. [Google Scholar] [CrossRef] [PubMed]
- Miri, A.; Monsef-Esfahani, H.R.; Amini, M.; Amanzadeh, Y.; Hadjiakhoondi, A.; Hajiaghaee, R.; Ebrahimi, A. Comparative chemical composition and antioxidant properties of the essential oils and aromatic water from Teucrium persicum Boiss. Iran. J. Pharm. Res. IJPR 2012, 11, 573. [Google Scholar] [PubMed]
- Moon, S.-Y.; Cliff, M.A.; Li-Chan, E.C.Y. Odour-active components of simulated beef flavour analysed by solid phase microextraction and gas chromatography-mass spectrometry and -olfactometry. Food Res. Int. 2006, 39, 294–308. [Google Scholar]
- Ádámová, M.; Oriňák, A.; Halás, L. Retention indices as identification tool in pyrolysis-capillary gas chromatography. J. Chromatogr. A 2005, 1087, 131–141. [Google Scholar] [CrossRef]
- Zouari, N.; Ayadi, I.; Fakhfakh, N.; Rebai, A.; Zouari, S. Variation of chemical composition of essential oils in wild populations of Thymus algeriensis Boiss. et Reut., a North African endemic Species. Lipids Health Dis. 2012, 11, 28. [Google Scholar] [CrossRef]
- Leela, N.K.; Vipin, T.M.; Shafeekh, K.M.; Priyanka, V.; Rema, J. Chemical composition of essential oils from aerial parts of Cinnamomum malabatrum (Burman f.) Bercht & Presl. Flavour Fragr. J. 2009, 24, 13–16. [Google Scholar]
- Ning, H.; Zheng, F.; Sun, B.; Xie, J.; Liu, Y. Solvent-free microwave extraction of essential oil from Zanthoxylum bungeanum Maxim. Food Environ. Ind. 2008, 34, 179–184. [Google Scholar]
- Hudaib, M.; Speroni, E.; Di Pietra, A.M.; Cavrini, V. GC/MS evaluation of thyme (Thymus vulgaris L.) oil composition and variations during the vegetative cycle. J. Pharm. Biomed. Anal. 2002, 29, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Taveira, F.; De Lima, W.; Andrade, E.; Maia, J. Seasonal essential oil variation of Aniba canelilla. Biochem. Syst. Ecol. 2003, 31, 69–75. [Google Scholar] [CrossRef]
- Ríos, Y.K.; Otero, A.C.; Muñoz, D.L.; Echeverry, M.; Robledo, S.M.; Yepes, M.A. Actividad citotóxica y leishmanicida in vitro del aceite esencial de manzanilla (Matricaria chamomilla). Rev. Colomb. Cienc. Químico-Farm. 2008, 37, 200–211. [Google Scholar]
- Chang, H.-J.; Kim, J.-M.; Lee, J.-C.; Kim, W.-K.; Chun, H.S. Protective effect of β-caryophyllene, a natural bicyclic sesquiterpene, against cerebral ischemic injury. J. Med. Food 2013, 16, 471–480. [Google Scholar] [CrossRef]
- Souza, M.; Siani, A.C.; Ramos, M.; Menezes-de-Lima, O., Jr.; Henriques, M. Evaluation of anti-inflammatory activity of essential oils from two Asteraceae species. Die Pharm. Int. J. Pharm. Sci. 2003, 58, 582–586. [Google Scholar]
- Silva Mazutti, S.; Rezende, C.C.; Martins, G.G.; Silva, E.G.; Gomes, S.; Pic-Taylor, A.; Fonseca-Bazzo, Y.; Silveira, D.; Magalhães, P. Wound Healing Effect of Essential Oil Extracted from Eugenia dysenterica DC (Myrtaceae) Leaves. Molecules 2018, 24, 2. [Google Scholar] [CrossRef]
- Kima, P.E. The amastigote forms of Leishmania are experts at exploiting host cell processes to establish infection and persist. Int. J. Parasitol. 2007, 37, 1087–1096. [Google Scholar] [CrossRef]
- Boyom, F.F.; Ngouana, V.; Zollo, P.H.A.; Menut, C.; Bessiere, J.M.; Gut, J.; Rosenthal, P.J. Composition and anti-plasmodial activities of essential oils from some Cameroonian medicinal plants. Phytochemistry 2003, 64, 1269–1275. [Google Scholar] [CrossRef]
- Al-Salem, W.S.; Solórzano, C.; Weedall, G.D.; Dyer, N.A.; Kelly-Hope, L.; Casas-Sánchez, A.; Alraey, Y.; Alyamani, E.J.; Halliday, A.; Balghonaim, S.M. Old World cutaneous leishmaniasis treatment response varies depending on parasite species, geographical location and development of secondary infection. Parasites Vectors 2019, 12, 195. [Google Scholar]
- Delgado-Altamirano, R.; López-Palma, R.I.; Monzote, L.; Delgado-Domínguez, J.; Becker, I.; Rivero-Cruz, J.F.; Esturau-Escofet, N.; Vázquez-Landaverde, P.A.; Rojas-Molina, A. Chemical constituents with leishmanicidal activity from a pink-yellow cultivar of Lantana camara var. aculeata (L.) collected in Central Mexico. Int. J. Mol. Sci. 2019, 20, 872. [Google Scholar] [PubMed]
- da Franca Rodrigues, K.A.; Amorim, L.V.; Dias, C.N.; Moraes, D.F.C.; Carneiro, S.M.P.; de Amorim Carvalho, F.A. Syzygium cumini (L.) Skeels essential oil and its major constituent α-pinene exhibit anti-Leishmania activity through immunomodulation in vitro. J. Ethnopharmacol. 2015, 160, 32–40. [Google Scholar]
- Moreira, R.R.D.; Santos, A.G.d.; Carvalho, F.A.; Perego, C.H.; Crevelin, E.J.; Crotti, A.E.M.; Cogo, J.; Cardoso, M.L.C.; Nakamura, C.V. Antileishmanial activity of Melampodium divaricatum and Casearia sylvestris essential oils on Leishmania amazonensis. Rev. Inst. Med. Trop. São Paulo 2019, 61, e33. [Google Scholar] [CrossRef] [PubMed]
- Ioset, J.-R.; Brun, R.; Wenzler, T.; Kaiser, M.; Yardley, V. Drug Screening for Kinetoplastids Diseases. In A Training Manual for Screening in Neglected Diseases; DNDi and Pan-Asian Screening Network: Geneva, Switzerland, 2009. [Google Scholar]
- Demarchi, I.G.; Thomazella, M.V.; de Souza Terron, M.; Lopes, L.; Gazim, Z.C.; Cortez, D.A.G.; Donatti, L.; Aristides, S.M.A.; Silveira, T.G.V.; Lonardoni, M.V.C. Antileishmanial activity of essential oil and 6, 7-dehydroroyleanone isolated from Tetradenia riparia. Exp. Parasitol. 2015, 157, 128–137. [Google Scholar] [PubMed]
- Almeida-Souza, F.; Taniwaki, N.N.; Amaral, A.C.F.; Souza, C.d.S.F.d.; Calabrese, K.d.S.; Abreu-Silva, A.L. Ultrastructural changes and death of Leishmania infantum promastigotes induced by Morinda citrifolia Linn. fruit (Noni) juice treatment. Evid. Based Complement. Altern. Med. 2016, 2016, 5063540. [Google Scholar] [CrossRef] [PubMed]
- Neves, L.O.; Talhari, A.C.; Gadelha, E.P.N.; da Silva Júnior, R.M.; Guerra, J.A.d.O.; Ferreira, L.C.d.L.; Talhari, S. Estudo clínico randomizado comparando antimoniato de meglumina, pentamidina e anfotericina B para o tratamento da leishmaniose cutânea ocasionada por Leishmania guyanensis. An. Bras. Dermatol 2011, 86, 1092–1101. [Google Scholar] [CrossRef]
- Gama Bitencourt, J.J.; Pazin, W.M.; Ito, A.S.; Barioni, M.B.; de Paula Pinto, C.; dos Santos, M.A.; Guimarães, T.H.S.; dos Santos, M.R.M.; Valduga, C.J. Miltefosine-loaded lipid nanoparticles: Improving miltefosine stability and reducing its hemolytic potential toward erythtocytes and its cytotoxic effect on macrophages. Biophys. Chem. 2016, 217, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Myatt, G.J.; Ahlberg, E.; Akahori, Y.; Allen, D.; Amberg, A.; Anger, L.T.; Aptula, A.; Auerbach, S.; Beilke, L.; Bellion, P. In silico toxicology protocols. Regul. Toxicol. Pharmacol. 2018, 96, 1–17. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef]
- Costa, W.K.; de Oliveira, J.R.S.; de Oliveira, A.M.; da Silva Santos, I.B.; da Cunha, R.X.; de Freitas, A.F.S.; da Silva, J.W.L.M.; Silva, V.B.G.; de Oliveira Farias, J.C.R.; da Silva, A.G. Essential oil from Eugenia stipitata McVaugh leaves has antinociceptive, anti-inflammatory and antipyretic activities without showing toxicity in mice. Ind. Crops Prod. 2020, 144, 112059. [Google Scholar]
- Goodwin, R.; Bunch, J.; McGinnity, D. Mass spectrometry imaging in oncology drug discovery. In Advances in Cancer Research; Elsevier: Amsterdam, The Netherlands, 2017; Volume 134, pp. 133–171. [Google Scholar]
- Li, D.; Chen, L.; Li, Y.; Tian, S.; Sun, H.; Hou, T. ADMET evaluation in drug discovery. 13. Development of in silico prediction models for P-glycoprotein substrates. Mol. Pharm. 2014, 11, 716–726. [Google Scholar] [CrossRef] [PubMed]
- Montanari, F.; Ecker, G.F. Prediction of drug–ABC-transporter interaction—Recent advances and future challenges. Adv. Drug Deliv. Rev. 2015, 86, 17–26. [Google Scholar] [PubMed]
- Srivalli, K.M.R.; Lakshmi, P. Overview of P-glycoprotein inhibitors: A rational outlook. Braz. J. Pharm. Sci. 2012, 48, 353–367. [Google Scholar] [CrossRef]
- Trinconi, C.T.; Reimao, J.Q.; Bonano, V.I.; Espada, C.R.; Miguel, D.C.; Yokoyama-Yasunaka, J.K.; Uliana, S.R. Topical tamoxifen in the therapy of cutaneous leishmaniasis. Parasitology 2018, 145, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Wienkers, L.C.; Heath, T.G. Predicting in vivo drug interactions from in vitro drug discovery data. Nat. Rev. Drug Discov. 2005, 4, 825. [Google Scholar] [CrossRef]
- Utkarsh, D.; Loretz, C.; Li, A.P. In Vitro evaluation of hepatotoxic drugs in human hepatocytes from multiple donors: Identification of P450 activity as a potential risk factor for drug-induced liver injuries. Chem. Biol. Interact. 2016, 255, 12–22. [Google Scholar]
- Nembri, S.; Grisoni, F.; Consonni, V.; Todeschini, R. In silico prediction of cytochrome P450-drug interaction: QSARs for CYP3A4 and CYP2C9. Int. J. Mol. Sci. 2016, 17, 914. [Google Scholar]
- Dutra, R.C.; Tavares, C.Z.; Ferraz, S.O.; Sousa, O.V.; Pimenta, D.S. Investigation of analgesic and anti-inflammatory activities of Echinodorus grandiflorus rhizomes methanol extract. Rev. Bras. Farmacogn. 2006, 16, 469–474. [Google Scholar] [CrossRef]
- Veras, B.O.; de Oliveira, M.B.M.; da Silva Oliveira, F.G.; Dos Santos, Y.Q.; de Oliveira, J.R.S.; de Menezes Lima, V.L.; da Silva Almeida, J.R.G.; Navarro, D.M.d.A.F.; de Oliveira Farias, J.C.R.; dos Santos Aguiar, J. Chemical composition and evaluation of the antinociceptive, antioxidant and antimicrobial effects of essential oil from Hymenaea cangaceira (Pinto, Mansano & Azevedo) native to Brazil: A natural medicine. J. Ethnopharmacol. 2020, 247, 112265. [Google Scholar]
- Veras, B.O.; de Oliveira, J.R.S.; de Menezes Lima, V.L.; Navarro, D.M.d.A.F.; de Oliveira Farias, J.C.R.; de Medeiros Moura, G.M.; da Silva, J.W.; de Assis, C.R.D.; Gorlach-Lira, K.; de Assis, P.A.C. The essential oil of the leaves of Verbesina macrophylla (Cass.) SF Blake has antimicrobial, anti-inflammatory and antipyretic activities and is toxicologically safe. J. Ethnopharmacol. 2021, 265, 113248. [Google Scholar]
- Machado, R.R.; Jardim, D.F.; Souza, A.R.; Scio, E.; Fabri, R.L.; Carpanez, A.G.; Grazul, R.M.; de Mendonça, J.P.R.; Lesche, B.; Aarestrup, F.M. The effect of essential oil of Syzygium cumini on the development of granulomatous infl ammation in mice. Rev. Bras. Farmacogn. 2013, 23, 488–496. [Google Scholar]
- Lorençoni, M.F.; Figueira, M.M.; e Silva, M.V.T.; Schmitt, E.F.P.; Endringer, D.C.; Scherer, R.; Barth, T.; Bertolucci, S.K.V.; Fronza, M. Chemical composition and anti-inflammatory activity of essential oil and ethanolic extract of Campomanesia phaea (O. Berg.) Landrum leaves. J. Ethnopharmacol. 2020, 252, 112562. [Google Scholar] [PubMed]
- Li, Y.; Cao, X.; Sun, J.; Zhang, W.; Zhang, J.; Ding, Y.; Liu, Y. Characterization of chemical compositions by a GC-MS/MS approach and evaluation of antioxidant activities of essential oils from Cinnamomum reticulatum Hay, Leptospermum petersonii Bailey, and Juniperus formosana Hayata. Arab. J. Chem. 2021, 15, 103609. [Google Scholar]
- Silva, L.; Nunes-Pinheiro, D.; Morais, S.; Lopes Neto, B.; Santos, G.; Campello, C. Toxicological evaluation and effect of ethyl acetate extract of the fiber of Cocos nucifera L. (Palmae) on inflammatory response in vivo. Rev. Bras. Plantas Med. 2009, 11, 429–434. [Google Scholar] [CrossRef][Green Version]






| Compounds | IR 1 | (%) | Reference |
|---|---|---|---|
| beta-cis-Caryophyllene | 1494 | 24.04 | [42] |
| epi-gamma-Eudesmol | 1624 | 8.00 | [43] |
| 2-Naphthalenemethanol, decahydro-α,α,4a-trimethyl-8-methylene-, [2R-(2α,4aα,8aβ)]- | 1593 | 8.00 | [44] |
| trans-Calamenene | 1527 | 6.69 | [45] |
| 2-Naphthalenemethanol | 1598 | 5.84 | [46] |
| Bicyclogermacrene | 1497 | 5.46 | [47] |
| Germacrene D | 1480 | 4.07 | [48] |
| Alfa-Copaene | 1375 | 3.33 | [49] |
| Cyclohexanemethanol | 1522 | 2.60 | [50] |
| Caryophyllene oxide | 1507 | 2.52 | [51] |
| β-Pinene | 943 | 2.44 | [52] |
| α-Caryophyllene | 1579 | 1.92 | [53] |
| Aromadendrene | 1386 | 1.86 | [54] |
| 1,3,6-Octatriene | 976 | 1.84 | [55] |
| (-)-Spathulenol | 1536 | 1.64 | [56] |
| Cadinadiene | 1452 | 1.63 | [57] |
| Naphthalene [1,2,3,4,4a,7-hexahydro] | 1536 | 1.47 | [58] |
| Cyclohexene | 377 | 1.29 | [59] |
| tau-Muurolol | 1580 | 1.06 | [60] |
| Ledol | 1530 | 1.05 | [61] |
| α-Cubebene | 1344 | 0.97 | [62] |
| Eucalyptol | 1032 | 0.88 | [63] |
| Promastigotes | Amastigotes | |||||||
|---|---|---|---|---|---|---|---|---|
| Cell | CC50 1 (μg/mL) | Leishmania Species | IC50 4 (μg/mL) | ISMØ 5 | ISVC 6 | IC50 (μg/mL) | ISMØ | ISVC |
| mPEC | 137.48 ± 4.6 | La 2 | 5.77 ± 0.9 | 23.81 | 24.78 | 7.31 ± 0.5 | 18.80 | 19.66 |
| Vero | 143.73 ± 3.4 | Lb 3 | 5.60 ± 1.7 | 24.53 | 25.53 | 7.26 ± 0.1 | 18.93 | 19.79 |
| Parameter | CAR 2 | EUD 3 | 2-NAPH 4 | CAL 5 |
|---|---|---|---|---|
| Lipinski Rules Violation | Yes | No | No | Yes |
| Physicochemical properties | ||||
| HBA 6 (≤10) | 0 | 1 | 1 | 0 |
| HBD 7 (≤5) | 0 | 1 | 1 | 0 |
| ClogP 8 (≤5) | 3.29 | 3.19 | 3.11 | 3.19 |
| MW 9 (≤500) g/mol | 204.35 | 222.37 | 222.37 | 202.34 |
| n-ROTB 10 (≤10) | 0 | 1 | 1 | 1 |
| Absorption | ||||
| BBB 11 | No | Yes | Yes | No |
| HIA 12 | Low | High | High | Low |
| P-GP 13 substrate | No | No | No | No |
| Skin permeability (cm/s) | −4.44 | −5.25 | −4.77 | −3.90 |
| Metabolism | ||||
| CYP450 2C9 inhibitor | Yes | No | Yes | No |
| CYP450 2D6 inhibitor | No | No | No | Yes |
| CYP450 2C19 inhibitor | Yes | No | No | No |
| CYP450 3A4 inhibitor | No | No | No | No |
| CYP450 1A2 inhibitor | No | No | No | No |
| Toxicity | ||||
| Mutagenic | No | No | No | No |
| Tumorigenic | No | No | No | No |
| Irritant | No | No | No | No |
| DL50 (mg/kg) 14 | 5000 | 5000 | 2000 | 1710 |
| Tests | Control | Indomethacin 50 mg/kg | PCEO 1 | ||
|---|---|---|---|---|---|
| 50 mg/kg | 100 mg/kg | 200 mg/kg | |||
| Paw edema | |||||
| 0 h | 0.13 ± 0.08 | 0.16 ± 0.08 | 0.08 ± 0.03 | 0.08 ± 0.05 | 0.10 ± 0.01 |
| 1 h | 0.95 ± 0.19 | 0.05 ± 0.01 * | 0.34 ± 0.04 *! | 0.33 ± 0.07 *! | 0.08 ± 0.06 * |
| 2 h | 1.05 ± 0.28 | 0.03 ± 0.02 * | 0.34 ± 0.04 *! | 0.25 ± 0.08 *! | 0.05 ± 0.04 * |
| 3 h | 1.21 ± 0.26 | 0.03 ± 0.02 * | 0.23 ± 0.08 *! | 0.20 ± 0.07 *! | 0.04 ± 0.01 * |
| 4 h | 1.01 ± 0.11 | 0.0 ± 0.01 * | 0.25 ± 0.08 *! | 0.15 ± 0.05 *! | 0.05 ± 0.03 * |
| Ear edema | |||||
| 0 h | 0.04 ± 0.02 | 0.03 ± 0.01 | 0.04 ± 0.04 | 0.05 ± 0.04 | 0.03 ± 0.02 |
| 2 h | 0.13 ± 0.01 | 0.52 ± 0.01 * | 0.04 ± 0.01 *! | 0.01 ± 0.01 *! | 0.01 ± 0.01 *! |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holanda, V.N.; Brito, T.G.S.; Oliveira, J.R.S.d.; Cunha, R.X.d.; Silva, A.P.S.d.; Silva, W.V.d.; Araújo, T.F.S.; Tavares, J.F.; Santos, S.G.d.; Figueiredo, R.C.B.Q.; et al. Potential Effects of Essential Oil from Plinia cauliflora (Mart.) Kausel on Leishmania: In Vivo, In Vitro, and In Silico Approaches. Microorganisms 2024, 12, 207. https://doi.org/10.3390/microorganisms12010207
Holanda VN, Brito TGS, Oliveira JRSd, Cunha RXd, Silva APSd, Silva WVd, Araújo TFS, Tavares JF, Santos SGd, Figueiredo RCBQ, et al. Potential Effects of Essential Oil from Plinia cauliflora (Mart.) Kausel on Leishmania: In Vivo, In Vitro, and In Silico Approaches. Microorganisms. 2024; 12(1):207. https://doi.org/10.3390/microorganisms12010207
Chicago/Turabian StyleHolanda, Vanderlan N., Thaíse G. S. Brito, João R. S. de Oliveira, Rebeca X. da Cunha, Ana P. S. da Silva, Welson V. da Silva, Tiago F. S. Araújo, Josean F. Tavares, Sócrates G. dos Santos, Regina C. B. Q. Figueiredo, and et al. 2024. "Potential Effects of Essential Oil from Plinia cauliflora (Mart.) Kausel on Leishmania: In Vivo, In Vitro, and In Silico Approaches" Microorganisms 12, no. 1: 207. https://doi.org/10.3390/microorganisms12010207
APA StyleHolanda, V. N., Brito, T. G. S., Oliveira, J. R. S. d., Cunha, R. X. d., Silva, A. P. S. d., Silva, W. V. d., Araújo, T. F. S., Tavares, J. F., Santos, S. G. d., Figueiredo, R. C. B. Q., & Lima, V. L. M. (2024). Potential Effects of Essential Oil from Plinia cauliflora (Mart.) Kausel on Leishmania: In Vivo, In Vitro, and In Silico Approaches. Microorganisms, 12(1), 207. https://doi.org/10.3390/microorganisms12010207







