Proinflammatory Chemokine Levels in Cerebrospinal Fluid of Patients with Neuroinvasive Flavivirus Infections
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Methods
2.2.1. Flavivirus Detection
2.2.2. Chemokine Determination
2.2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
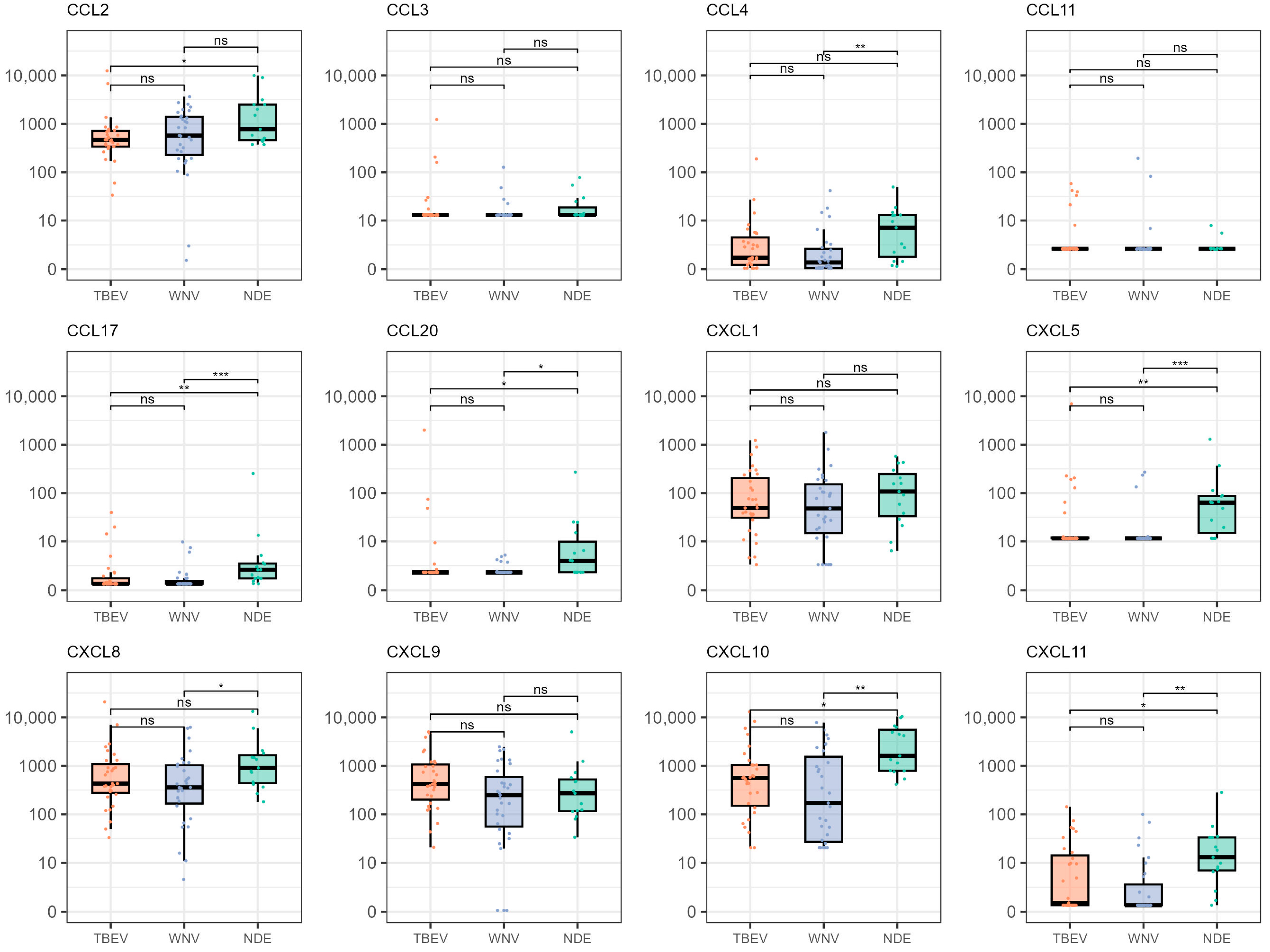
3.2. Chemokine Levels Comparison According to Demographic Characteristics and Clinical Diagnosis
3.3. Correlation Analysis of the Selected Chemokines
3.4. Multivariate Analysis of the Selected Chemokines
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Heuverswyn, J.; Hallmaier-Wacker, L.K.; Beauté, J.; Gomes Dias, J.; Haussig, J.M.; Busch, K.; Kerlik, J.; Markowicz, M.; Mäkelä, H.; Nygren, T.M.; et al. Spatiotemporal spread of tick-borne encephalitis in the EU/EEA, 2012 to 2020. Eurosurveillance 2023, 28, 2200543. [Google Scholar] [CrossRef] [PubMed]
- ECDC. Epidemiological Update: West Nile Virus Transmission Season in Europe. 2018. Available online: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-west-nile-virus-transmission-season-europe-2018 (accessed on 22 February 2024).
- ECDC. Epidemiological Update: West Nile Virus Transmission Season in Europe. 2022. Available online: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-west-nile-virus-transmission-season-europe-2022 (accessed on 22 February 2024).
- Riccardi, N.; Antonello, R.M.; Luzzati, R.; Zajkowska, J.; Di Bella, S.; Giacobbe, D.R. Tick-borne encephalitis in Europe: A brief update on epidemiology, diagnosis, prevention, and treatment. Eur. J. Intern. Med. 2019, 62, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pustijanac, E.; Buršić, M.; Talapko, J.; Škrlec, I.; Meštrović, T.; Lišnjić, D. Tick-Borne Encephalitis Virus: A Comprehensive Review of Transmission, Pathogenesis, Epidemiology, Clinical Manifestations, Diagnosis, and Prevention. Microorganisms 2023, 11, 1634. [Google Scholar] [CrossRef] [PubMed]
- Ruzek, D.; Avšič Županc, T.; Borde, J.; Chrdle, A.; Eyer, L.; Karganova, G.; Kholodilov, I.; Knap, N.; Kozlovskaya, L.; Matveev, A.; et al. Tick-borne encephalitis in Europe and Russia: Review of pathogenesis, clinical features, therapy, and vaccines. Antivir. Res. 2019, 164, 23–51. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.; Ferenczi, E.; Moussa, K.; Eliott, D.; Matiello, M. Clinical Spectrum of West Nile Virus Neuroinvasive Disease. Neurohospitalist 2020, 10, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Santini, M.; Haberle, S.; Židovec-Lepej, S.; Savić, V.; Kusulja, M.; Papić, N.; Višković, K.; Župetić, I.; Savini, G.; Barbić, L.; et al. Severe West Nile Virus Neuroinvasive Disease: Clinical Characteristics, Short- and Long-Term Outcomes. Pathogens 2022, 11, 52. [Google Scholar] [CrossRef] [PubMed]
- Vilibic-Cavlek, T.; Krcmar, S.; Bogdanic, M.; Tomljenovic, M.; Barbic, L.; Roncevic, D.; Sabadi, D.; Vucelja, M.; Santini, M.; Hunjak, B.; et al. An Overview of Tick-Borne Encephalitis Epidemiology in Endemic Regions of Continental Croatia, 2017–2023. Microorganisms 2024, 12, 386. [Google Scholar] [CrossRef] [PubMed]
- Vilibic-Cavlek, T.; Savic, V.; Klobucar, A.; Ferenc, T.; Ilic, M.; Bogdanic, M.; Tabain, I.; Stevanovic, V.; Santini, M.; Curman Posavec, M.; et al. Emerging trends in the West Nile virus epidemiology in Croatia in the ‘One Health’ context, 2011–2020. Trop. Med. Infect. Dis. 2021, 6, 140. [Google Scholar] [CrossRef] [PubMed]
- Barbic, L.; Savic, V.; Bogdanic, M.; Madic, J.; Sabadi, D.; Al-Mufleh, M.; Stevanovic, V.; Hruskar, Z.; Lakoseljac, D.; Roncevic, D.; et al. Re-emergence of neuroinvasive flaviviruses in the 2022 transmission season in Croatia. In Proceedings of the 33rd ECCMID, Copenhagen, Denmark, 15–18 April 2023; p. 2914, Book of Abstracts. [Google Scholar]
- Zidovec-Lepej, S.; Vilibic-Cavlek, T.; Ilic, M.; Gorenec, L.; Grgic, I.; Bogdanic, M.; Radmanic, L.; Ferenc, T.; Sabadi, D.; Savic, V.; et al. Quantification of Antiviral Cytokines in serum, Cerebrospinal Fluid and Urine of Patients with Tick-borne Encephalitis in Croatia. Vaccines 2022, 10, 1825. [Google Scholar] [CrossRef]
- Zidovec-Lepej, S.; Vilibic-Cavlek, T.; Barbic, L.; Ilic, M.; Savic, V.; Tabain, I.; Ferenc, T.; Grgic, I.; Gorenec, L.; Bogdanic, M.; et al. Antiviral cytokine response in neuroinvasive and non-neuroinvasive West Nile virus infection. Viruses 2021, 13, 342. [Google Scholar] [CrossRef]
- Bachelerie, F.; Ben-Baruch, A.; Burkhardt, A.M.; Combadiere, C.; Farber, J.M.; Graham, G.J.; Horuk, R.; Sparre-Ulrich, A.H.; Locati, M.; Luster, A.D.; et al. International Union of Pharmacology. LXXXIX. Update on the extended family of chemokine receptors and introducing a new nomenclature for atypical chemokine receptors. Pharmacol. Rev. 2014, 66, 1–79. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Wang, T. Recent Advances in Understanding West Nile Virus Host Immunity and Viral Pathogenesis. F1000Research 2018, 7, 338. [Google Scholar] [CrossRef] [PubMed]
- Bai, F.; Thompson, E.A.; Vig, P.J.S.; Leis, A.A. Current Understanding of West Nile Virus Clinical Manifestations, Immune Responses, Neuroinvasion, and Immunotherapeutic Implications. Pathogens 2019, 8, 193. [Google Scholar] [CrossRef] [PubMed]
- Tobler, L.H.; Cameron, M.J.; Lanteri, M.C.; Prince, H.E.; Danesh, A.; Persad, D.; Lanciotti, R.S.; Norris, P.J.; Kelvin, D.J.; Busch, M.P. Interferon and Interferon-Induced Chemokine Expression Is Associated with Control of Acute Viremia in West Nile Virus-Infected Blood Donors. J. Infect. Dis. 2008, 198, 979–983. [Google Scholar] [CrossRef] [PubMed]
- Fares-Gusmao, R.; Rocha, B.C.; Sippert, E.; Lanteri, M.C.; Áñez, G.; Rios, M. Differential Pattern of Soluble Immune Markers in Asymptomatic Dengue, West Nile and Zika Virus Infections. Sci. Rep. 2019, 9, 17172. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, K.W.; Sachs, D.; Bardina, S.V.; Michlmayr, D.; Rodriguez, C.A.; Sum, J.; Foster, G.A.; Krysztof, D.; Stramer, S.L.; Lim, J.K. Differences in Early Cytokine Production Are Associated with Development of a Greater Number of Symptoms Following West Nile Virus Infection. J. Infect. Dis. 2016, 214, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.N.; Hause, A.M.; Walker, C.M.; Orange, J.S.; Hasbun, R.; Murray, K.O. Evaluation of Prolonged Fatigue Post–West Nile Virus Infection and Association of Fatigue with Elevated Antiviral and Proinflammatory Cytokines. Viral Immunol. 2014, 27, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Lepej, S.Z.; Misić-Majerus, L.; Jeren, T.; Rode, O.D.; Remenar, A.; Sporec, V.; Vince, A. Chemokines CXCL10 and CXCL11 in the cerebrospinal fluid of patients with tick-borne encephalitis. Acta Neurol. Scand. 2007, 115, 109–114. [Google Scholar] [CrossRef]
- Toczylowski, K.; Grygorczuk, S.; Osada, J.; Wojtkowska, M.; Bojkiewicz, E.; Wozinska-Klepadlo, M.; Potocka, P.; Sulik, A. Evaluation of cerebrospinal fluid CXCL13 concentrations and lymphocyte subsets in tick-borne encephalitis. Int. J. Infect. Dis. 2020, 93, 40–47. [Google Scholar] [CrossRef]
- Zajkowska, J.; Moniuszko-Malinowska, A.; Pancewicz, S.A.; Muszyńska-Mazur, A.; Kondrusik, M.; Grygorczuk, S.; Swierzbińska-Pijanowska, R.; Dunaj, J.; Czupryna, P. Evaluation of CXCL10, CXCL11, CXCL12 and CXCL13 chemokines in serum and cerebrospinal fluid in patients with tick borne encephalitis (TBE). Adv. Med. Sci. 2011, 56, 311–317. [Google Scholar] [CrossRef]
- Grygorczuk, S.; Parczewski, M.; Świerzbińska, R.; Czupryna, P.; Moniuszko, A.; Dunaj, J.; Kondrusik, M.; Pancewicz, S. The increased concentration of macrophage migration inhibitory factor in serum and cerebrospinal fluid of patients with tick-borne encephalitis. J. Neuroinflamm. 2017, 14, 126. [Google Scholar] [CrossRef] [PubMed]
- Grygorczuk, S.; Świerzbińska, R.; Kondrusik, M.; Dunaj, J.; Czupryna, P.; Moniuszko, A.; Siemieniako, A.; Pancewicz, S. The intrathecal expression and pathogenetic role of Th17 cytokines and CXCR2-binding chemokines in tick-borne encephalitis. J. Neuroinflamm. 2018, 15, 115. [Google Scholar] [CrossRef] [PubMed]
- Grygorczuk, S.; Osada, J.; Toczyłowski, K.; Sulik, A.; Czupryna, P.; Moniuszko-Malinowska, A.; Kondrusik, M.; Świerzbińska, R.; Dunaj, J.; Pancewicz, S.; et al. The lymphocyte populations and their migration into the central nervous system in tick-borne encephalitis. Ticks Tick-Borne Dis. 2020, 11, 101467. [Google Scholar] [CrossRef] [PubMed]
- Grygorczuk, S.; Czupryna, P.; Pancewicz, S.; Świerzbińska, R.; Dunaj, J.; Siemieniako, A.; Moniuszko-Malinowska, A. The increased intrathecal expression of the monocyte-attracting chemokines CCL7 and CXCL12 in tick-borne encephalitis. J. Neurovirol. 2021, 27, 452–462. [Google Scholar] [CrossRef] [PubMed]
- Palus, M.; Formanová, P.; Salát, J.; Žampachová, E.; Elsterová, J.; Růžek, D. Analysis of serum levels of cytokines, chemokines, growth factors, and monoamine neurotransmitters in patients with tick-borne encephalitis: Identification of novel inflammatory markers with implications for pathogenesis. J. Med. Virol. 2015, 87, 885–892. [Google Scholar] [CrossRef]
- Bogovič, P.; Kastrin, A.; Lotrič-Furlan, S.; Ogrinc, K.; Avšič Županc, T.; Korva, M.; Knap, N.; Resman Rus, K.; Strle, K.; Strle, F. Comparison of laboratory and immune characteristics of the initial and second phase of tick-borne encephalitis. Emerg. Microbes Infect. 2022, 11, 1647–1656. [Google Scholar] [CrossRef]
- Fowler, Å.; Ygberg, S.; Bogdanovic, G.; Wickström, R. Biomarkers in cerebrospinal fluid of children with tick-borne encephalitis: Association with long-term outcome. Pediatr. Infect. Dis. J. 2016, 35, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Günther, G.; Haglund, M.; Lindquist, L.; Forsgren, M.; Andersson, J.; Andersson, B.; Sköldenberg, B. Tick-borne encephalitis is associated with low levels of interleukin-10 in cerebrospinal fluid. Infect. Ecol. Epidemiol. 2011, 1, 6029. [Google Scholar] [CrossRef]
- Bogovič, P.; Lusa, L.; Korva, M.; Pavletič, M.; Rus, K.R.; Lotrič-Furlan, S.; Avšič-Županc, T.; Strle, K.; Strle, F. Inflammatory Immune Responses in the Pathogenesis of Tick-Borne Encephalitis. J. Clin. Med. 2019, 8, 731. [Google Scholar] [CrossRef] [PubMed]
- Bogovič, P.; Lusa, L.; Korva, M.; Lotrič-Furlan, S.; Resman-Rus, K.; Pavletič, M.; Avšič-Županc, T.; Strle, K.; Strle, F. Inflammatory Immune Responses in Patients with Tick-Borne Encephalitis: Dynamics and Association with the Outcome of the Disease. Microorganisms 2019, 7, 514. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. EU Case Definitions. Available online: https://www.ecdc.europa.eu/en/all-topics/eu-case-definitions (accessed on 10 January 2024).
- Schwaiger, M.; Cassinotti, P. Development of a quantitative real-time RT-PCR assay with internal control for the laboratory detection of tick-borne encephalitis virus (TBEV) RNA. J. Clin. Virol. 2003, 27, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Anne Hapip, C.; Liu, B.; Fang, C.T. Highly sensitive TaqMan RT-PCR assay for detection and quantification of both lineages of West Nile virus RNA. J. Clin. Virol. 2006, 36, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Vilibic-Cavlek, T.; Barbic, L.; Stevanovic, V.; Petrovic, G.; Mlinaric-Galinovic, G. IgG Avidity: An Important Serologic Marker for the Diagnosis of Tick-Borne Encephalitis Virus Infection. Pol. J. Microbiol. 2016, 65, 119–121. [Google Scholar] [CrossRef] [PubMed]
- Vilibic-Cavlek, T.; Kristofic, B.; Savic, V.; Kolaric, B.; Barbic, L.; Tabain, I.; Peric, L.; Sabadi, D.; Miklausic, B.; Potocnik-Hunjadi, T.; et al. Diagnostic significance of IgG avidity in symptomatic and asymptomatic West Nile virus infection. Rev. Soc. Bras. Med. Trop. 2018, 51, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Vilibic-Cavlek, T.; Ferenc, T.; Vujica Ferenc, M.; Bogdanic, M.; Potocnik-Hunjadi, T.; Sabadi, D.; Savic, V.; Barbic, L.; Stevanovic, V.; Monaco, F.; et al. Cross-Reactive Antibodies in Tick-Borne Encephalitis: Case Report and Literature Review. Antibodies 2022, 11, 72. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.R-project.org/ (accessed on 4 January 2024).
- Müller, M.; Carter, S.; Hofer, M.J.; Campbell, I.L. Review: The chemokine receptor CXCR3 and its ligands CXCL9, CXCL10 and CXCL11 in neuroimmunity—A tale of conflict and conundrum. Neuropathol. Appl. Neurobiol. 2010, 36, 368–387. [Google Scholar] [CrossRef] [PubMed]
- Bogovič, P.; Lotrič-Furlan, S.; Avšič-Županc, T.; Korva, M.; Kastrin, A.; Lusa, L.; Strle, K.; Strle, F. Comparison of Clinical, Laboratory and Immune Characteristics of the Monophasic and Biphasic Course of Tick-Borne Encephalitis. Microorganisms 2021, 9, 796. [Google Scholar] [CrossRef] [PubMed]
- Bogovič, P.; Strle, F. Tick-borne encephalitis: A review of epidemiology, clinical characteristics, and management. World J. Clin. Cases 2015, 3, 430–441. [Google Scholar] [CrossRef] [PubMed]
- Urošević, A.; Dulović, O.; Milošević, B.; Maksić, N.; Popović, N.; Milošević, I.; Delić, D.; Jevtović, D.; Poluga, J.; Jordović, J.; et al. The Importance of Haematological and Biochemical Findings in Patients with West Nile Virus Neuroinvasive Disease. J. Med. Biochem. 2016, 35, 451–457. [Google Scholar] [CrossRef]
- Guo, L.; Li, N.; Yang, Z.; Li, H.; Zheng, H.; Yang, J.; Chen, Y.; Zhao, X.; Mei, J.; Shi, H.; et al. Role of CXCL5 in Regulating Chemotaxis of Innate and Adaptive Leukocytes in Infected Lungs Upon Pulmonary Influenza Infection. Front. Immunol. 2021, 12, 785457. [Google Scholar] [CrossRef]
- Karpus, W.J.; Kennedy, K.J. MIP-1alpha and MCP-1 differentially regulate acute and relapsing autoimmune encephalomyelitis as well as Th1/Th2 lymphocyte differentiation. J. Leukoc. Biol. 1997, 62, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Grygorczuk, S.; Zajkowska, J.; Swierzbińska, R.; Pancewicz, S.; Kondrusik, M.; Hermanowska-Szpakowicz, T. Elevated concentration of the chemokine CCL3 (MIP-1alpha) in cerebrospinal fluid and serum of patients with tick borne encephalitis. Adv. Med. Sci. 2006, 51, 340–344. [Google Scholar] [PubMed]
- Lupancu, T.J.; Eivazitork, M.; Hamilton, J.A.; Achuthan, A.A.; Lee, K.M. CCL17/TARC in autoimmunity and inflammation-not just a T-cell chemokine. Immunol. Cell Biol. 2023, 101, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Sachi, N.; Kamiyama, N.; Saechue, B.; Ozaka, S.; Dewayani, A.; Ariki, S.; Chalalai, T.; Soga, Y.; Fukuda, C.; Kagoshima, Y.; et al. CCL20/CCR6 chemokine signaling is not essential for pathogenesis in an experimental autoimmune encephalomyelitis mouse model of multiple sclerosis. Biochem. Biophys. Res. Commun. 2023, 641, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Dey, R.; Bishayi, B. Microglial Inflammatory Responses to SARS-CoV-2 Infection: A Comprehensive Review. Cell. Mol. Neurobiol. 2023, 44, 2. [Google Scholar] [CrossRef]
- Masouris, I.; Manz, K.; Pfirrmann, M.; Dreyling, M.; Angele, B.; Straube, A.; Langer, S.; Huber, M.; Koedel, U.; Von Baumgarten, L. CXCL13 and CXCL9 CSF Levels in Central Nervous System Lymphoma-Diagnostic, Therapeutic, and Prognostic Relevance. Front. Neurol. 2021, 12, 654543. [Google Scholar] [CrossRef] [PubMed]
- Erhart, D.K.; Klose, V.; Schäper, T.; Tumani, H.; Senel, M. CXCL13 in Cerebrospinal Fluid: Clinical Value in a Large Cross-Sectional Study. Int. J. Mol. Sci. 2023, 25, 425. [Google Scholar] [CrossRef]
- Kim, J.S. Protein biomarkers in multiple sclerosis. Encephalitis 2023, 3, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Liba, Z.; Nohejlova, H.; Capek, V.; Krsek, P.; Sediva, A.; Kayserova, J. Utility of chemokines CCL2, CXCL8, 10 and 13 and interleukin 6 in the pediatric cohort for the recognition of neuroinflammation and in the context of traditional cerebrospinal fluid neuroinflammatory biomarkers. PLoS ONE 2019, 14, e0219987. [Google Scholar] [CrossRef]
- Ma, Y.; Wang, J.; Guo, S.; Meng, Z.; Ren, Y.; Xie, Y.; Wang, M. Cytokine/chemokine levels in the CSF and serum of anti-NMDAR encephalitis: A systematic review and meta-analysis. Front. Immunol. 2023, 13, 1064007. [Google Scholar] [CrossRef]
- Hoffman, K.W.; Lee, J.J.; Foster, G.A.; Krysztof, D.; Stramer, S.L.; Lim, J.K. Sex differences in cytokine production following West Nile virus infection: Implications for symptom manifestation. Pathog. Dis. 2019, 77, ftz016. [Google Scholar] [CrossRef] [PubMed]

| Parameter | All Patients (N = 62) | Patients with TBEV (N = 31) | Patients with WNV (N = 31) | |
|---|---|---|---|---|
| Demographics | Male sex | 38 (61%) | 21 (68%) | 17 (55%) |
| Age (median, range; years) | 58 (12–88) | 46 (12–74) | 63 (13–88) | |
| Clinical characteristics and outcome | Meningitis | 31 (50%) | 15 (48%) | 16 (52%) |
| Meningoencephalitis | 23 (37%) | 12 (39%) | 11 (36%) | |
| Febrile headache | 4 (7%) | 3 (10%) | 1 (3%) | |
| Myelitis | 2 (3%) | 1 (3%) | 1 (3%) | |
| Poliradiculoneuritis | 2 (3%) | 0 (0%) | 2 (7%) | |
| Fatal outcome | 3 (5%) | 0 (0%) | 3 (10%) |
| Chemokine | Coefficient | Standard Error | p-Value |
|---|---|---|---|
| CCL11 | 0.135 | 0.043 | <0.001 |
| CXCL5 | −0.144 | 0.034 | <0.001 |
| CXCL10 | −0.043 | 0.015 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zidovec-Lepej, S.; Bodulić, K.; Bogdanic, M.; Gorenec, L.; Savic, V.; Grgic, I.; Sabadi, D.; Santini, M.; Radmanic Matotek, L.; Kucinar, J.; et al. Proinflammatory Chemokine Levels in Cerebrospinal Fluid of Patients with Neuroinvasive Flavivirus Infections. Microorganisms 2024, 12, 657. https://doi.org/10.3390/microorganisms12040657
Zidovec-Lepej S, Bodulić K, Bogdanic M, Gorenec L, Savic V, Grgic I, Sabadi D, Santini M, Radmanic Matotek L, Kucinar J, et al. Proinflammatory Chemokine Levels in Cerebrospinal Fluid of Patients with Neuroinvasive Flavivirus Infections. Microorganisms. 2024; 12(4):657. https://doi.org/10.3390/microorganisms12040657
Chicago/Turabian StyleZidovec-Lepej, Snjezana, Kristian Bodulić, Maja Bogdanic, Lana Gorenec, Vladimir Savic, Ivana Grgic, Dario Sabadi, Marija Santini, Leona Radmanic Matotek, Jasmina Kucinar, and et al. 2024. "Proinflammatory Chemokine Levels in Cerebrospinal Fluid of Patients with Neuroinvasive Flavivirus Infections" Microorganisms 12, no. 4: 657. https://doi.org/10.3390/microorganisms12040657
APA StyleZidovec-Lepej, S., Bodulić, K., Bogdanic, M., Gorenec, L., Savic, V., Grgic, I., Sabadi, D., Santini, M., Radmanic Matotek, L., Kucinar, J., Barbic, L., Zmak, L., Ferenc, T., Stevanovic, V., Antolasic, L., Milasincic, L., Hruskar, Z., Vujica Ferenc, M., & Vilibic-Cavlek, T. (2024). Proinflammatory Chemokine Levels in Cerebrospinal Fluid of Patients with Neuroinvasive Flavivirus Infections. Microorganisms, 12(4), 657. https://doi.org/10.3390/microorganisms12040657











