Epidemiological and Clinical Aspects of Cutaneous and Mucosal Leishmaniases in Portugal: Retrospective Analysis of Cases Diagnosed in Public Hospitals and Reported in the Literature between 2010 and 2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics and Comorbidities
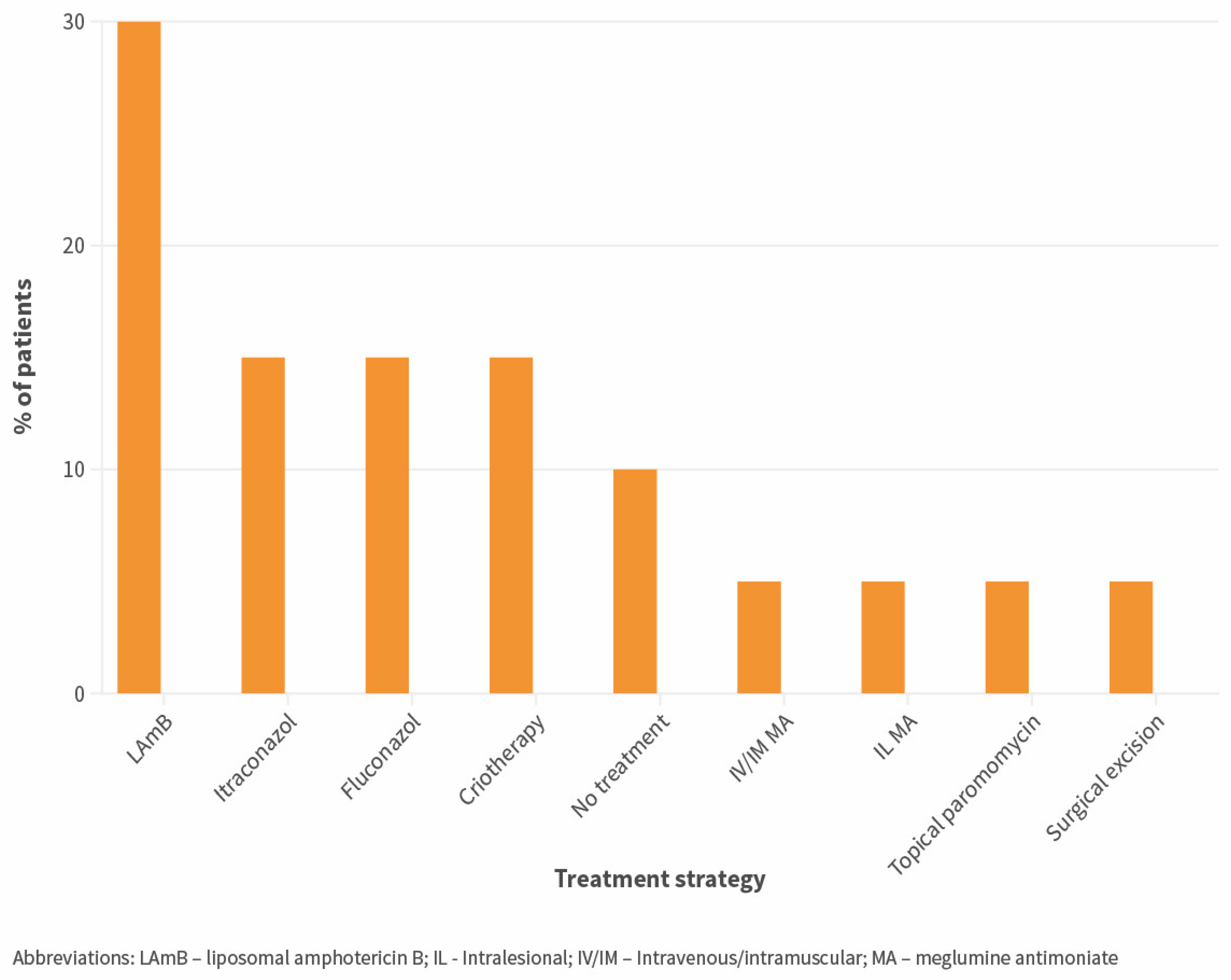
3.2. Clinical Aspects of CL
3.3. Clinical Aspects of ML
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Farrar, J.; Garcia, P.; Hotez, P.; Junghanss, T.; Kang, G.; Lalloo, D.; White, N. Manson’s Tropical Diseases, 24th ed.; Elsevier: Amsterdam, The Netherlands, 2024. [Google Scholar]
- ECDC. Surveillance, Prevention and Control of Leishmaniases in the European Union and Its Neighbouring Countries. Stockholm. 2022. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/leishmaniasis-surveillance-eu.pdf (accessed on 3 March 2024).
- Gaspari, V.; Gritti, T.; Ortalli, M.; Santi, A.; Galletti, G.; Rossi, A.; Rugna, G.; Mattivi, A.; Matteo, G.; Belloli, G.L.; et al. Tegumentary Leishmaniasis in Northeastern Italy from 2017 to 2020: A Neglected Public Health Issue. Int. J. Environ. Res. Public Health 2022, 19, 16047. [Google Scholar] [CrossRef] [PubMed]
- Phlebotomine sandflies maps. European Centre for Disease Prevention and Control and European Food Safety Authority. Stockholm: ECDC. Available online: https://ecdc.europa.eu/en/disease-vectors/surveillance-and-disease-data/phlebotomine-maps (accessed on 3 March 2024).
- Maia, C.; Dantas-Torres, F.; Campino, L. Parasite Biology: The Reservoir Hosts. In The Leishmaniases: Old Neglected Tropical Diseases; Springer International Publishing: Cham, Germany, 2018; pp. 79–106. [Google Scholar]
- Campino, L.; Abranches, P. Leishmaniose cutânea: Uma doença rara em Portugal? Acta. Med. Port. 2002, 15, 387–390. [Google Scholar] [PubMed]
- Borges-Costa, J.; Pacheco, D.; Soares-Almeida, L.; Sacramento-Marques, M. Pápulas marrones y violáceas localizadas en la espalda de un paciente con infección por el virus de la inmunodeficiencia humana. Enferm. Infecc. Microbiol. Clin. 2013, 31, 410–411. [Google Scholar] [CrossRef] [PubMed]
- Costin, A.; Bonito, F.; Alves, J.; Barreiros, H. Tratamiento de la leishmaniasis localizada mediante el antimoniato de meglumina intralesional y la terapia fotodinámica. Actas Dermosifiliogr. 2020, 111, 897–899. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelos, J.; Torres, J.; Granado, J.; Baptista, T.; Mansinho, K. Cutaneous leishmaniasis in non-endemic countries: An emerging yet neglected problem. IDCases 2019, 17, e00570. [Google Scholar] [CrossRef] [PubMed]
- Marques, N.; Bustorff, M.; Cordeiro Da Silva, A.; Pinto, A.I.; Santarém, N.; Ferreira, F.; Nunes, A.; Cerqueira, A.; Rocha, A.; Ferreira, I.; et al. Visceral Dissemination of Mucocutaneous Leishmaniasis in a Kidney Transplant Recipient. Pathogens 2020, 10, 18. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.; Vasconcelos, P.; Borges-Costa, J.; Soares-Almeida, L.; Campino, L.; Filipe, P. An atypical case of cutaneous leishmaniasis caused by Leishmania infantum in Portugal. Dermatol. Online J. 2013, 19, 20407. [Google Scholar] [CrossRef] [PubMed]
- Matos, A.L.; Figueiredo, C.; Alves, F.; Pereira, N.; Gonçalo, M. Mucocutaneous leishmaniasis complicating systemic lupus erythematosus and responding to high dose amphotericin B. J. Eur. Acad. Dermatol. Venereol. 2021, 35, pe756. [Google Scholar] [CrossRef] [PubMed]
- Van der Auwera, G.; Davidsson, L.; Buffet, P.; Ruf, M.T.; Gramiccia, M.; Varani, S.; Chicharro, C.; Bart, A.; Harms, G.; Chiodini, P.L.; et al. Surveillance of leishmaniasis cases from 15 European centres, 2014 to 2019: A retrospective analysis. Eurosurveillance 2022, 27, 2002028. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, N. Leishmaniose cutânea na Beira Interior: Um Diagnóstico Diferencial Obrigatório. Master’s Thesis, Universidade da Beira Interior, Covilhã, Portugal, 2009. [Google Scholar]
- Fundação Francisco Manuel dos Santos. PORDATA Base de Dados de Portugal Contemporâneo. População Residente Estrangeira Segundo os Censos: Total e por País de Nacionalidade. 2023. Available online: https://www.pordata.pt/portugal/populacao+residente+estrangeira+segundo+os+censos+total+e+por+pais+de+nacionalidade-3786 (accessed on 3 March 2024).
- Fundação Francisco Manuel dos Santos. PORDATA. O que são NUTS? Available online: https://www.pordata.pt/o+que+sao+nuts (accessed on 3 March 2024).
- Instituto Nacional de Estatística. Censos 2021 Resultados Definitivos—Portugal, Lisboa; Instituto Nacional de Estatística: Lisbon, Portugal, 2022.
- Fundação Francisco Manuel dos Santos. PORDATA Base de Dados de Portugal Contemporâneo. SNS: Hospitais por Tipo—Continente. 2022. Available online: https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_publicacoes&PUBLICACOESpub_boui=66196836&PUBLICACOESmodo=2 (accessed on 3 March 2024).
- World Health Organisation. Status of Endemicity of Cutaneous Leishmaniasis: 2022. 2023. Available online: https://apps.who.int/neglected_diseases/ntddata/leishmaniasis/leishmaniasis.html (accessed on 8 October 2023).
- Nemhauser, J. Travelers with Additional Considerations. In CDC Yellow Book 2024; Oxford University Press: New York, NY, USA, 2023; pp. 139–180. [Google Scholar]
- Gradoni, L.; López-Vélez, R.; Mokni, M. Manual on Case Management and Surveillance of the Leishmaniasis in the WHO European Region; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Daly, L.E. Confidence Limits Made Easy: Interval Estimation Using a Substitution Method. Am. J. Epidemiol. 1998, 147, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Antunes, J.; da Costa, J.B.; Guimarães, M.; Vaz-Pinto, I.; Soares-Almeida, L.; Filipe, P. Post-Kala-azar dermal leishmaniasis due to Leishmania donovani in Europe—Case report. Int. J. Dermatol. 2013, 52, 1584–1586. [Google Scholar] [CrossRef] [PubMed]
- Maia, C.; Conceição, C.; Pereira, A.; Rocha, R.; Ortuño, M.; Muñoz, C.; Jumakanova, Z.; Pérez-Cutillas, P.; Özbel, Y.; Töz, S.; et al. The estimated distribution of autochthonous leishmaniasis by Leishmania infantum in Europe in 2005–2020. PLoS Negl. Trop. Dis. 2023, 17, e0011497. [Google Scholar] [CrossRef] [PubMed]
- Maia, C.; Campino, L. Leishmaniose em Portugal no início do século XXI. An. Inst. Hig. Med. Trop. 2014, 13, 25–28. [Google Scholar]
- Humanes-Navarro, A.M.; Herrador, Z.; Redondo, L.; Cruz, I.; Fernández-Martínez, B. Estimating human leishmaniasis burden in Spain using the capture-recapture method, 2016–2017. PLoS ONE 2021, 16, e0259225. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, G.; Demar, M.; Lami, P.; Zribi, A.; Marty, P.; Buffet, P.; Desbois-Nogard, N.; Gangneux, J.P.; Simon, S.; Blaizot, R.; et al. Leishmaniasis epidemiology in endemic areas of metropolitan France and its overseas territories from 1998 to 2020. PLoS Negl. Trop. Dis. 2022, 16, e0010745. [Google Scholar] [CrossRef]
- Campino, L.; Pratlong, F.; Abranches, P.; Rioux, J.A.; Santos-Gomes, G.; Alves-Pires, C.; Cortes, S.; Ramada, J.; Cristovão, J.M.; Afonso, M.O.; et al. Leishmaniasis in Portugal: Enzyme polymorphism of Leishmania infantum based on the identification of 213 strains. Trop. Med. Int. Health 2006, 11, 1708–1714. [Google Scholar] [CrossRef] [PubMed]
- Giavedoni, P.; Iranzo, P.; Fuertes, I.; Estrach, T.; Alsina Gibert, M. Leishmaniasis cutánea. Experiencia de 20 años en un hospital español de tercer nivel. Actas Dermosifiliogr. 2015, 106, 310–316. [Google Scholar] [CrossRef]
- Pan American Health Organization. Guideline for the Treatment of Leishmaniasis in the Americas, 2nd ed.; Pan American Health Organization: Washington, DC, USA, 2022. [Google Scholar]
- Rocha, R.; Pereira, A.; Maia, C. Non-Endemic Leishmaniases Reported Globally in Humans between 2000 and 2021—A Comprehensive Review. Pathogens 2022, 11, 921. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Phlebotomus sergenti-Current Known Distribution: August 2023. 2023. Available online: https://www.ecdc.europa.eu/en/publications-data/phlebotomus-sergenti-current-known-distribution-august-2023 (accessed on 13 October 2023).
- Faucher, B.; Pomares, C.; Fourcade, S.; Benyamine, A.; Marty, P.; Pratlong, L.; Faraut, F.; Mary, C.; Piarroux, R.; Dedet, J.P.; et al. Mucosal Leishmania infantum leishmaniasis: Specific pattern in a multicentre survey and historical cases. J. Infect. 2011, 63, 76–82. [Google Scholar] [CrossRef] [PubMed]

| Global | CL | ML | p-Value | |
|---|---|---|---|---|
| Number | 50 | 43 | 7 | |
| Median age, years (IQI) | 48 | 47 | 66 | 0.026 * |
| [33–61.25] | [33–59] | [50–75] | (U = 71.0) | |
| Male sex (%) | 68.0 | 69.8 | 57.1 | 0.666 |
| (34/50) | (30/43) | (4/7) | (FET) | |
| Country of birth (%) | ||||
| Native | 75.6 | 72.5 | 100 | 0.313 (FET) |
| (34/45) | (29/40) | (5/5) | ||
| Migrant | 24.4 | 27.5 | 0 | |
| (11/45) | (11/40) a | (0/5) | ||
| Origin of infection (%) | ||||
| Autochthonous | 86.0 | 83.7 | 100 | 0.573 (FET) |
| (43/50) | (36/43) | (7/7) | ||
| Imported | 14.0 | 16.3 | 0 | |
| (7/50) | (7/43) b | (0/7) | ||
| Immunosuppression (%) | ||||
| Yes | 48.0 | 46.5 | 57.1 | 0.697 |
| (24/50) | (20/43) | (4/7) | (FET) | |
| Unknown/Not reported | 2.0 | 0 | 14.3 | |
| (1/50) | (0/43) | (1/7) | ||
| HIV infection/AIDS | ||||
| Yes (%) | 32.7 | 34.9 | 16.7 | 0.649 |
| (16/49) | (15/43) | (1/6) | (FET) | |
| CD4 cell count <200/µL (%) | 78.6 | 84.6 | 0 | 0.214 |
| (11/14) | (11/13) | (0/1) | (FET) | |
| Chronic pharmacologic immunosuppression (%) | ||||
| Inflammatory/autoimmune diseases c | 12.2 | 9.3 | 33.3 | 0.151 |
| (6/49) | (4/43) d | (2/6) e | (FET) | |
| Other | 4.1 | 2.3 | 16.7 | |
| (2/49) | (1/43) f | (1/6) g | ||
| Chronic dysfunction/condition (%) | ||||
| Yes | 28.6 | 19.4 | 83.3 | 0.005 * |
| (12/42) | (7/36) h | (5/6) i | (FET) | |
| a Brazil: n = 4; Cape Verde: n = 2; Guinea-Bissau: n = 1; Morocco: n = 1; São Tomé e Príncipe: n = 1; Senegal: n = 1; unknown: n = 1 | ||||
| b Brazil: n = 3; Morocco: n = 2; Mexico: n = 1; Tunisia: n = 1 | ||||
| c Systemic lupus erythematosus: n = 2; ankylosing spondylitis: n = 1; Crohn’s disease: n = 1; psoriasis: n = 1; rheumatoid arthritis: n = 1 | ||||
| d Adalimumab: n = 1; adalimumab + methotrexate: n = 1, methotrexate: n = 1; methotrexate + prednisolone: n = 1 | ||||
| e Methotrexate: n = 1; mycophenolate mofetil + prednisolone: n = 1 | ||||
| f Lymphoma: n = 1 | ||||
| g Kidney transplant: n = 1 h Chronic kidney disease n = 6; chronic heart failure n = 1; chronic obstructive respiratory disease n = 1; chronic hepatic disease n = 1; diabetes mellitus n =1 | ||||
| i Chronic kidney disease: n = 2; chronic heart failure: n = 1; chronic obstructive respiratory disease: n = 1; diabetes mellitus: n = 3 * Statistically significant | ||||
| Region | Average Population in 2011–2021 * | Number of CL/ML Cases | Mean Annual CL/ML Incidence ** | 95% CI |
|---|---|---|---|---|
| Mainland Portugal | 9,951,765 | 39 | 0.036 | 0.024–0.047 |
| Norte | 3,638,134 | 7 | 0.017 | 0.006–0.033 |
| Alto Minho | 238,051 | 0 | 0 | NA |
| Cávado | 413,387 | 0 | 0 | NA |
| Ave | 421,933 | 0 | 0 | NA |
| Área Metropolitana do Porto | 1,747,876 | 4 | 0.021 | 0.003–0.046 |
| Alto Tâmega | 89,195 | 0 | 0 | NA |
| Tâmega e Sousa | 420,776 | 1 | 0.022 | 0.001–0.120 |
| Douro | 194,516 | 1 | 0.047 | 0.001–0.260 |
| Terras de Trás-os-Montes | 112,399 | 0 | 0 | NA |
| Centro | 1,695,204 | 13 | 0.070 | 0.037–0.119 |
| Região de Aveiro | 368,898 | 3 | 0.074 | 0.015–0.216 |
| Região de Coimbra | 448,500 | 0 | 0 | NA |
| Região de Leiria | 290,692 | 0 | 0 | NA |
| Viseu Dão Lafões | 260,205 | 2 | 0.070 | 0.008–0.252 |
| Beira Baixa | 103,597 | 1 | 0.088 | 0.002–0.489 |
| Beiras e Serra da Estrela | 223,312 | 5 | 0.204 | 0.066–0.475 |
| Oeste e Vale do Tejo | 823,948 | 0 | 0 | NA |
| Oeste | 363,025 | 0 | 0 | NA |
| Médio Tejo | 219,266 | 0 | 0 | NA |
| Lezíria do Tejo | 241,657 | 0 | 0 | NA |
| Grande Lisboa | 2,052,392 | 13 | 0.058 | 0.031–0.098 |
| Península de Setúbal | 793,651 | 3 | 0.034 | 0.007–0.100 |
| Alentejo | 489,259 | 1 | 0.019 | 0.000–0.069 |
| Alentejo Litoral | 97,183 | 0 | 0 | NA |
| Baixo Alentejo | 120,777 | 0 | 0 | NA |
| Alto Alentejo | 111,714 | 1 | 0.081 | 0.002–0.453 |
| Alentejo Central | 159,585 | 0 | 0 | NA |
| Algarve | 459,174 | 2 | 0.040 | 0.005–0.143 |
| Type of Lesion (%) | |
|---|---|
| Papule/Nodule | 62.1 |
| (18/29) | |
| Ulcer | 24.1 |
| (7/29) | |
| Macule/Plaque | 20.7 |
| (6/29) | |
| Multiple lesions (%) | 41.9 |
| (13/31) | |
| Median size of largest lesion, mm (IQI) | 30 |
| [10–40] | |
| Location of lesions (%) | |
| Head | 48.3 |
| (14/29) | |
| Upper limbs | 31.0 |
| (9/29) | |
| Lower limbs | 31.0 |
| (9/29) | |
| Trunk | 20.7 |
| (6/29) | |
| Disseminated cutaneous leishmaniasis (%) | 12.5 |
| (4/32) | |
| Local pain (%) | 25.0 |
| (5/20) | |
| Skin superinfection a (%) | 11.1 |
| (3/27) | |
| Simultaneous visceral leishmaniasis (%) | 38.9 |
| (14/36) | |
| Technique used in skin/mucosa sample (%) | |
| Microscopy | 100 |
| (31/31) | |
| Positive result | 100 |
| (30/30) | |
| Polymerase chain reaction | 28.6 |
| (8/28) | |
| Positive result | 85.7 |
| (6/7) | |
| Identification of species (%) | 19.4 |
| (6/31) | |
| Serology (%) | |
| Yes b | 34.6 |
| (9/26) | |
| % positive | 37.5 |
| (3/8) | |
| Treatment of primary episode (%) | |
| Yes | 93.8 |
| (30/32) | |
| Median time from diagnosis to treatment, days (IQI) | 4 |
| [0–31] | |
| Monotherapy | 93.3 |
| (28/30) | |
| Systemic | 80.0 |
| (24/30) | |
| Topical | 23.3 |
| (7/30) | |
| Side effects | 15.4 |
| (2/13) | |
| Outcome of treatment (%) | |
| Improvement at 7 days | 60.0 |
| (9/15) | |
| Improvement at 30 days | 76.2 |
| (16/21) | |
| Switch of treatment/retreatment (non-improvement) | 19.2 |
| (5/26) | |
| Relapse | 5.6 |
| (2/36) | |
| a methicillin-sensitive Staphylococcus aureus: n = 1; Pseudomonas aeruginosa: n = 1; non-identified n = 1 | |
| b immunofluorescent antibody test: n = 5; unknown: n = 4 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rocha, R.; Conceição, C.; Gonçalves, L.; Carvalho, A.C.; Maia, A.; Martins, A.; Carujo, A.; Maio, A.; Forra, C.; Melita, C.; et al. Epidemiological and Clinical Aspects of Cutaneous and Mucosal Leishmaniases in Portugal: Retrospective Analysis of Cases Diagnosed in Public Hospitals and Reported in the Literature between 2010 and 2020. Microorganisms 2024, 12, 819. https://doi.org/10.3390/microorganisms12040819
Rocha R, Conceição C, Gonçalves L, Carvalho AC, Maia A, Martins A, Carujo A, Maio A, Forra C, Melita C, et al. Epidemiological and Clinical Aspects of Cutaneous and Mucosal Leishmaniases in Portugal: Retrospective Analysis of Cases Diagnosed in Public Hospitals and Reported in the Literature between 2010 and 2020. Microorganisms. 2024; 12(4):819. https://doi.org/10.3390/microorganisms12040819
Chicago/Turabian StyleRocha, Rafael, Cláudia Conceição, Luzia Gonçalves, Ana Cláudia Carvalho, André Maia, André Martins, António Carujo, António Maio, Catarina Forra, Catarina Melita, and et al. 2024. "Epidemiological and Clinical Aspects of Cutaneous and Mucosal Leishmaniases in Portugal: Retrospective Analysis of Cases Diagnosed in Public Hospitals and Reported in the Literature between 2010 and 2020" Microorganisms 12, no. 4: 819. https://doi.org/10.3390/microorganisms12040819
APA StyleRocha, R., Conceição, C., Gonçalves, L., Carvalho, A. C., Maia, A., Martins, A., Carujo, A., Maio, A., Forra, C., Melita, C., Couto, D., Fernandes, D., Pereira, D., Leal, E., Sarmento, H., Sousa, I., Gonçalves, J.-P., Marinho, J., Vasconcelos, J., ... Maia, C. (2024). Epidemiological and Clinical Aspects of Cutaneous and Mucosal Leishmaniases in Portugal: Retrospective Analysis of Cases Diagnosed in Public Hospitals and Reported in the Literature between 2010 and 2020. Microorganisms, 12(4), 819. https://doi.org/10.3390/microorganisms12040819







