Exploiting the Advantages of Molecular Tools for the Monitoring of Fungal Indoor Air Contamination: First Detection of Exophiala jeanselmei in Indoor Air of Air-Conditioned Offices
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sampling
2.2. Classical Analysis
2.3. DNA Extraction
2.4. RT-PCR Screening
2.5. Massive Parallel Sequencing
2.6. Bioinformatics Analysis
3. Results
3.1. Classical Analysis by Culturing
3.2. RT-PCR Detection
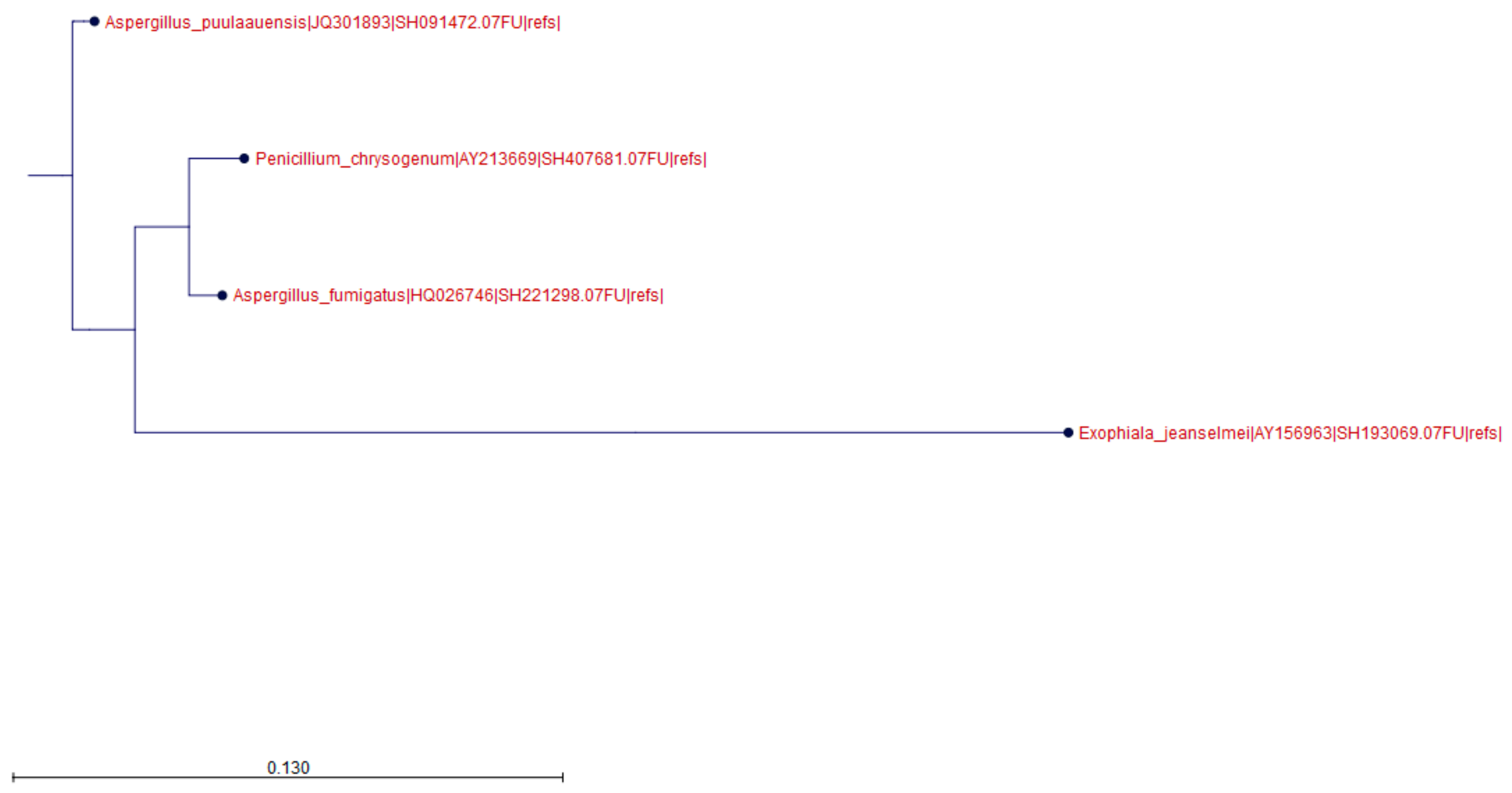
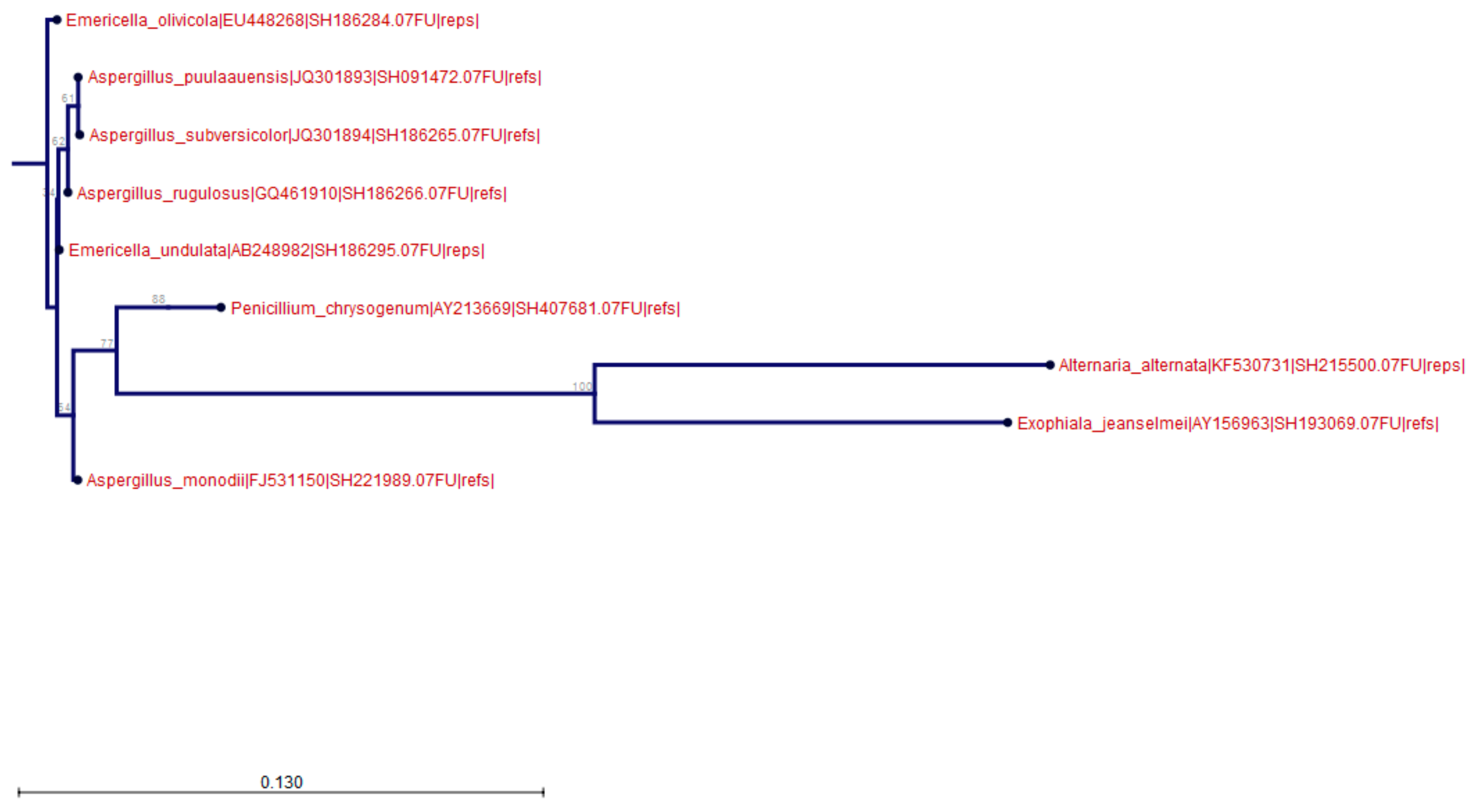
3.3. Massive Parallel Sequencing
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bellanger, A.P.; Reboux, G.; Roussel, S.; Grenouillet, F.; Didier-Scherer, E.; Dalphin, J.C.; Millon, L. Indoor fungal contamination of moisture-damaged and allergic patient housing analysed using real-time PCR. Lett. Appl. Microbiol. 2009, 49, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Mendell, M.J.; Mirer, A.G.; Cheung, K.; Tong, M.; Douwes, J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Env. Health Perspect. 2011, 119, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Packeu, A.; Chasseur, C.; Bladt, S.; Detandt, M. The role of indoor pollution in the development and maintenance of chronic airway inflammation in children. B-ENT 2012, 8, 73–79. [Google Scholar] [PubMed]
- Meheust, D.; Le Cann, P.; Reboux, G.; Millon, L.; Gangneux, J.P. Indoor fungal contamination: Health risks and measurement methods in hospitals, homes and workplaces. Crit. Rev. Microbiol. 2014, 40, 248–260. [Google Scholar] [CrossRef]
- Portnoy, J.M.; Jara, D. Molds allergy revisited. Ann. Allergy Asthma Immunol. 2015, 114, 83–89. [Google Scholar] [CrossRef]
- Dannemiller, K.C.; Gent, J.F.; Leaderer, B.P.; Peccia, J. Indoor microbial communities: Influence on asthma severity in atopic and nonatopic asthma. J. Allergy Clin. Immunol. 2016, 138, 76–83. [Google Scholar] [CrossRef] [Green Version]
- European Environment Agency. Indoor Air Quality. Available online: http://www.eea.europa.eu/signals/signals-2013/articles/indoor-air-quality (accessed on 15 October 2019).
- United States Environmental Protection Agency. An introduction to indoor air quality. Available online: https://www.epa.gov/indoor-air-quality-iaq (accessed on 15 October 2019).
- WHO Regional Office for Europe. WHO Guidelines for Indoor Air Quality: Dampness and Mould; World Health Organization: Copenhagen, Denmark, 2009. [Google Scholar]
- Shelton, B.G.; Kirkland, K.H.; Flanders, W.D.; Morris, G.K. Profiles of airborne fungi in buildings and outdoor environments in the United States. Appl. Env. Microbiol. 2002, 68, 1743–1753. [Google Scholar] [CrossRef] [Green Version]
- Horner, W.E.; Worthan, A.G.; Morey, P.R. Air- and dustborn mycoflora in houses free of water damage and fungal growth. Appl. Env. Microbiol. 2004, 70, 6394–6400. [Google Scholar] [CrossRef] [Green Version]
- Kelkar, U.; Bal, A.; Kulkarni, S. Fungal contamination of air conditionning units in operating theatres in India. JHI 2005, 60, 81–84. [Google Scholar] [CrossRef]
- Ponsoni, K.; Gonçalves Raddi, M.S. Indoor air quality related to occupancy at an air-conditioned public health. Braz. Arch Biol. Technol. 2010, 53, 99–103. [Google Scholar] [CrossRef] [Green Version]
- Adams, R.I.; Miletto, M.; Taylor, J.W.; Bruns, T.D. Dispersal in microbes: Fungi in indoor air are dominated by outdoor air and show dispersal limitation at short distances. ISME J. 2013, 7, 1262–1273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nucci, M.; Akiti, T.; Barreiros, G.; Silveira, F.; Revankar, S.; Sutton, D.; Patterson, T. Nosocomial fungemia due to Exophiala jeanselmei var. jeanselmei and a Rhinocladiella species: Newly described causes of bloodstream infection. J. Clin. Microbiol. 2001, 39, 514–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.; Yokoyama, K.; Miyaji, M.; Nishimura, K. Identification; classification; and phylogeny of the pathogenic species Exophiala jeanselmei and related species by mitochondrial cytochrome b gene analysis. J. Clin. Microbiol. 2001, 39, 4462–4467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nucci, M.; Akiti, T.; Barreiros, G.; Silveira, F.; Revankar, S.; Wickes, B.; Sutton, D.; Patterson, T. Nosocomial outbreak of Exophiala jeanselmei fungemia associated with contamination of hospital water. Clin. Infect Dis. 2002, 34, 1475–1480. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Sutton, D.; Fothergill, A.; Rinaldi, M.; Harrak, M.; de Hoog, G. Spectrum of clinically relevant Exophiala species in the United States. J. Clin. Microbiol. 2007, 45, 3713–3720. [Google Scholar] [CrossRef] [Green Version]
- Sterflinger, K. Black yeasts and meristemactic fungi: Ecology; diversity and identification. In Biodiversity and Ecophysiology of Yeasts; Péter, G., Rosa, C., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; Volume 20, pp. 501–514. [Google Scholar]
- Kirtsideli, I.Y.; Vlasov, D.Y.; Abakumov, E.V.; Barantsevich, E.P.; Novozhilov, Y.K.; Krylenkov, V.A.; Sokolov, V.T. Airborne fungi in arctic settlement Tiksi (Russian Arctic, coast of the Laptev Sea). Czech Polar Rep. 2017, 7, 300–310. [Google Scholar] [CrossRef]
- Nishimura, K.; Miyaji, M.; Taguchi, H.; Tanaka, R. Fungi in bathwater and sludge of bathroom drainpipes. Frequent isolation of Exophiala species. Mycopathologia 1987, 97, 17–23. [Google Scholar] [CrossRef]
- Badali, H.; Chander, J.; Bayat, M.; Seyedmousavi, S.; Sidhu, S.; Rani, H.; Attri, A.; Handa, U.; Meis, J.; de Hoog, G. Multiple subcutaneous cysts due to Exophiala spinifera in an immunocompetent patient. Med. Mycol. 2012, 50, 207–213. [Google Scholar] [CrossRef] [Green Version]
- Pitkaranta, M.; Meklin, T.; Hyvarinen, A.; Nevalainen, A.; Paulin, L.; Auvinen, P.; Lignell, U.; Rintala, H. Molecular profiling of fungal communities in moisture damaged buildings before and after remediation—A comparison of culture-dependent and culture-independent methods. BMC Microbiol. 2011, 11, 235. [Google Scholar] [CrossRef] [Green Version]
- Vesper, S.J. Traditional mould analysis compared to a DNA-based method of mould analysis. Crit. Rev. Microbiol. 2011, 37, 15–24. [Google Scholar] [CrossRef]
- Anaissie, E.J.; Stratton, S.L.; Dignagi, M.C.; Lee, C.K.; Summerbell, R.C.; Rex, J.H.; Monson, T.P.; Walsh, T.J. Pathogenic molds (including Aspergillus species) in hospital water distribution systems: A 3-year prospective study and clinical implications for patients with hematologic malignancies. Blood 2003, 101, 2542–2546. [Google Scholar] [CrossRef] [PubMed]
- Haugland, R.A.; Varma, M.; Wymer, L.J.; Vesper, S.J. Quantitative PCR analysis of selected Aspergillus; Penicillium and Paecilomyces species. Syst. Appl. Microbiol. 2004, 27, 198–210. [Google Scholar] [CrossRef] [PubMed]
- Timothy, D.; Betancourt, D.; Menetrez, M. A rapid DNA extraction method for PCR identification of fungal indoor air contaminants. J. Microbiol. Methods 2004, 56, 431–434. [Google Scholar]
- Michealsen, A.; Pinzari, F.; Ripka, K.; Lubitz, W.; Piñar, G. Application of molecular techniques for identification of fungal communities colonising paper materials. Int. Biodeter. Biodegrad. 2006, 58, 133–141. [Google Scholar] [CrossRef]
- Reboux, G.; Bellanger, A.P.; Roussel, S.; Grenouillet, F.; Sornin, S.; Piarroux, R.; Dalphin, J.C.; Millon, L. Indoor mold concentration in Eastern France. Indoor Air. 2009, 19, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Hospodsky, D.; Yamamoto, N.; Peccia, J. Accuracy; precision; and method detection limits of quantitative PCR for airborne bacteria and fungi. Appl. Env. Microbiol. 2010, 76, 7004–7012. [Google Scholar] [CrossRef] [Green Version]
- Libert, X.; Chasseur, C.; Packeu, A.; Bureau, F.; Roosens, N.H.; De Keersmaecker, S.C.J. A molecular approach for the rapid; selective and sensitive detection of Exophiala jeanselmei in environmental samples: Development and performance assessment of a real-time PCR assay. Appl. Microbiol. Biotechnol. 2016, 100, 1377–1392. [Google Scholar] [CrossRef] [Green Version]
- Nolard, N.; Chasseur, C.; Marlier, M.; Lognay, G. Validation des Méthodes Microbiologiques et Chimiques de Contrôle des Lieux de Travail. 2004. Available online: http://www.belspo.be/belspo/organisation/publ/pub_ostc/PS/rPS19r_fr.pdf (accessed on 15 October 2019).
- Libert, X.; Chasseur, C.; Bladt, S.; Packeu, A.; Bureau, F.; Roosens, N.; De Keersmaecker, S.C.J. Development and validation of a qualitative SYBR®green real-time PCR assay for the detection of Aspergillus versicolor from indoor air. Appl. Microbiol. Biotechnol. 2015, 99, 7267–7282. [Google Scholar] [CrossRef] [Green Version]
- White, T.; Bruns, T.; Lee, S.; Taylor, J. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In PCR Protocols: A Guide to Methods and Applications; Innis, M., Gelfand, D., Shinsky, J., White, T., Eds.; Academic Press: Amsterdam, The Netherlands, 1990; pp. 315–322. [Google Scholar]
- Andrews, S. FastQC: A Quality Control Tool for High Throughput Sequence Data. [Babraham Bioinformatics Website]. October 2010. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc (accessed on 10 September 2019).
- Kõljalg, U.; Larsson, K.H.; Abarenkov, K.; Nilsson, R.H.; Alexander, I.J.; Eberhardt, U.; Erland, S.; Høiland, K.; Kjøller, R.; Larsson, E.; et al. UNITE: A database providing web-based methods for the molecular identification of ectomycorrhizal fungi. New Phytol. 2005, 166, 1063–1068. [Google Scholar]
- Beguin, H.; Nolard, N. Mould biodiversity in homes. I. Air and surface analysis of 130 dwellings. Aerobiologia 1994, 10, 157–166. [Google Scholar] [CrossRef]
- Heinemann, S.; Beguin, H.; Nolard, N. Biocontamination in air-conditioning. In Health Implication of Fungi in Indoor Environment; Samson, R.A., Flannigan, B., Flannigan, M.E., Verhoeff, A.P., Adan, O.C.G., Hoekstra, E.S., Eds.; Elsevier: Amsterdam, The Netherlands, 1994; pp. 179–186. [Google Scholar]
- Parat, S.; Fricker-Hidalgo, H.; Perdrix, A.; Bemer, D.; Pelissier, N.; Grillot, R. Airborne fungal contamination in air-conditionning systems: Effect of filtering and humidifying devices. AIHA J. 1996, 57, 996–1001. [Google Scholar] [CrossRef]
- Afanou, K.A.; Straumfors, A.; Skogstad, A.; Nayak, A.P.; Skaar, I.; Hejeljord, L.; Transmo, A.; Eduard, W.; Green, B.J. Indirect immunodetection of fungal fragments by field emission scanning electron microscopy. Appl. Env. Microbiol. 2015, 1, 5794–5803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, W.C.; Lu, Y.H.; Lin, Z.G.; Su, W.L. Sauna lung: Hypersensitivity pneumonitis due to Exophiala jeanselmei. Respiro Case Rep. 2010, 15, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Gurvich, O.L.; Skoblov, M. Real-Time PCR and Multiplex Approaches. Methods Mol. Biol. 2011, 2, 1–13. [Google Scholar] [CrossRef]
| Sample ID * | Pulse Group | Office | Sample Type | Analysis Method | ||
|---|---|---|---|---|---|---|
| Culture | RT-PCR | |||||
| CFU/mL 1 | Tm (°C) 2 | Cq 3 | ||||
| PG1 4 | 1 | Water 5 | 0 | N/A | N/A | |
| PG1-1 | 1 | 1 | Air | 0 | N/A | N/A |
| PG1-2 | 1 | 2 | Air | 0 | N/A | N/A |
| PG1-3 | 1 | 3 | Air | 0 | N/A | N/A |
| PG2 | 2 | Water 5 | 10 | 79.53 ± 0.12 | 28.00 ± 1.35 | |
| PG2-1 | 2 | 1 | Air | 0 | N/A | N/A |
| PG2-2 | 2 | 2 | Air | 0 | N/A | N/A |
| PG2-3 | 2 | 3 | Air | 0 | N/A | N/A |
| PG3 | 3 | Water 5 | 10 | 79.79 ± 0.32 | 28.39 ± 0.93 | |
| PG3-1 | 3 | 1 | Air | 0 | N/A | N/A |
| PG3-2 | 3 | 2 | Air | 0 | N/A | N/A |
| PG3-3 | 3 | 3 | Air | 0 | N/A | N/A |
| PG4 | 4 | Water 5 | 100 | 79.93 ± 0.05 | 20.32 ± 1.98 | |
| PG4-1 | 4 | 1 | Air | 0 | 79.44 ± 0.10 | 23.79 ± 0.92 |
| PG4-2 | 4 | 2 | Air | 0 | 79.49 ± 0.03 | 24.49 ± 0.23 |
| PG4-3 | 4 | 3 | Air | 0 | 79.38 ± 0.03 | 34.05 ± 1.75 |
| PG5 | 4 | Water 5 | 15 | 79.34 ± 0.23 | 27.36 ± 1.12 | |
| PG5-1 | 5 | 1 | Air | 0 | 79.39 ± 0.02 | 27.62 ± 0.63 |
| PG5-2 | 5 | 2 | Air | 0 | N/A | N/A |
| PG5-3 | 5 | 3 | Air | 0 | N/A | N/A |
| Sample * | Classical Analysis 1 | NGS | ||
|---|---|---|---|---|
| Species | CFU/mL | Species | Abundance of Reads Per OTU 2 (%) | |
| PG1 | Penicillium chrysogenum | 5 | Penicillium chrysogenum | 100 |
| PG2 | Penicillium chrysogenum | 5 | Penicillium chrysogenum | 60.64 |
| Aspergillus puulaaeunsis | 1 | Aspergilluspuulaaeunsis | 11.27 | |
| Nonsporulating sp. | 1 | |||
| Aspergillus fumigatus | 4 | Aspergillus fumigatus | 36.34 | |
| PG3 | Penicilliumchrysogenum | 5 | Penicilliumchrysogenum | 30.15 |
| Nonsporulating sp. | 2 | |||
| Undetermined species | 1 | |||
| PG4 | Aspergillus fumigatus | 2 | Aspergillus fumigatus | 12.19 |
| PG5 | Penicillium chrysogenum | 3 | Penicillium chrysogenum | 23.30 |
| Aspergillus puulaaeunsis | 11.86 |
| Samples * | Classical Analysis 1 | NGS 2 | ||
|---|---|---|---|---|
| Species | CFU/mL | Species | Abundance of Reads Per OTU 2 (%) | |
| PG1-1 | Alternaria alternata | 5 | Alternaria alternata | 21.86 |
| Aspergillusversicolor | 3 | Aspergillus subversicolor | 11.49 | |
| Penicillium chrysogenum | 9 | Penicillium chrysogenum | 66.65 | |
| PG1-2 | Alternaria alternata | 3 | Alternaria alternata | 24.72 |
| Aspergillus sp. | 2 | Aspergillus monodii | 7.70 | |
| Nonsporulating sp. | 1 | Aspergillus rugulosus | 4.43 | |
| Penicillium chrysogenum | 7 | Penicillium chrysogenum | 62.40 | |
| PG1-3 | Alternaria alternata | 2 | Alternaria alternata | 31.28 |
| Undetermined species | 1 | Aspergillus monodii | 15.93 | |
| Nonsporulating sp. | 1 | Aspergillus rugulosus | 12.47 | |
| Penicillium chrysogenum | 7 | Penicillium chrysogenum | 39.58 | |
| PG2-1 | Undetermined sp. | 2 | Emericella olivicola | 16.22 |
| Penicillium chrysogenum | 6 | Penicillium chrysogenum | 71.44 | |
| Emericella undulata | 12.35 | |||
| PG2-2 | Alternaria alternata | 2 | Alternaria alternata | 24.59 |
| Penicillium chrysogenum | 6 | Penicillium chrysogenum | 75.41 | |
| PG2-3 | Alternaria alternata | 4 | Alternaria alternata | 32.28 |
| Aspergillus versicolor | 5 | Aspergillus subversicolor | 32.09 | |
| Aspergillus sp. | 1 | Aspergillus monodii | 24.26 | |
| Nonsporulating sp. | 1 | Aspergillus puulaaeunsis | 11.37 | |
| PG3-1 | Alternaria alternata | 4 | Alternaria alternata | 53.50 |
| Penicillium chrysogenum | 5 | Penicillium chrysogenum | 46.50 | |
| PG3-2 | Alternaria alternata | 5 | Alternaria alternata | 71.96 |
| Undetermined sp. | 2 | Emericella olivicola | 16.41 | |
| Emericella undulata | 11.63 | |||
| PG3-3 | Aspergillus sp. | 2 | Aspergillus monodii | 11.18 |
| Aspergillus rugulosus | 19.56 | |||
| Aspergillus subversicolor | 20.40 | |||
| Penicillium chrysogenum | 6 | Penicillium chrysogenum | 48.85 | |
| PG4-1 | Alternaria alternata | 1 | Alternaria alternata | 26.18 |
| Aspergillus versicolor | 1 | Undertermined sp. | 13.07 | |
| Nonsporulating sp. | 1 | |||
| PG4-2 | Alternaria alternata | 3 | Alternaria alternata | 17.48 |
| Penicillium chrysogenum | 9 | Penicillium chrysogenum | 40.88 | |
| Undetermined sp. | ||||
| PG4-3 | Aspergillus versicolor | 4 | Aspergillus subversicolor | 29.12 |
| Nonsporulating sp. | 1 | Aspergillus puulaaeunsis | 24.38 | |
| Aspergillus monodii | 7.17 | |||
| PG5-1 | Penicillium chrysogenum | 7 | Penicillium chrysogenum | 64.57 |
| Undetermined sp. | 1 | Emericella undulata | 13.98 | |
| Nonsporulating sp. | 1 | Emericella olivicola | 10.46 | |
| PG5-2 | Alternaria alternata | 4 | Alternaria alternata | 31.33 |
| Aspergillus versicolor | 4 | Aspergillus subversicolor | 32.55 | |
| Aspergillus puulaaeunsis | 36.12 | |||
| Nonsporulating sp. | 2 | |||
| PG5-3 | Aspergillus versicolor | 6 | Aspergillus subversicolor | 39.24 |
| Penicillium chrysogenum | 8 | Penicillium chrysogenum | 60.76 |
| Pulse Group | Office 1 | Sample Type | Total Number of Reads 2 | Total of Reads Clustered 3 | % Reads Clustered 4 | Abundance of Reads into E. jeanselmei OTU 5 | % Reads into E. jeanselmei OTU (%) 6 | |
|---|---|---|---|---|---|---|---|---|
| PG1 7 | 1 | Water 8 | 13,124 | 11,602 | 88.40 | 0 | 0 | |
| PG1-1 | 1 | 1 | Air | 29,666 | 23,545 | 79.37 | 0 | 0 |
| PG1-2 | 1 | 2 | Air | 19,753 | 19,603 | 99.24 | 0 | 0 |
| PG1-3 | 1 | 3 | Air | 6352 | 6305 | 99.26 | 0 | 0 |
| PG2 | 2 | Water 8 | 9755 | 9741 | 99.86 | 2727 | 28.00 | |
| PG2-1 | 2 | 1 | Air | 28,487 | 20,928 | 73.47 | 0 | 0 |
| PG2-2 | 2 | 2 | Air | 15,193 | 15,093 | 99.34 | 0 | 0 |
| PG2-3 | 2 | 3 | Air | 28,338 | 25,260 | 89.14 | 0 | 0 |
| PG3 | 3 | Water 8 | 11,148 | 6797 | 60.97 | 2278 | 33.51 | |
| PG3-1 | 3 | 1 | Air | 9154 | 9003 | 98.35 | 0 | 0 |
| PG3-2 | 3 | 2 | Air | 9474 | 9434 | 99.58 | 0 | 0 |
| PG3-3 | 3 | 3 | Air | 9474 | 9165 | 96.74 | 0 | 0 |
| PG4 | 4 | Water 8 | 10,675 | 10,616 | 99.45 | 5700 | 53.69 | |
| PG4-1 | 4 | 1 | Air | 8402 | 8360 | 99.50 | 5078 | 60.74 |
| PG4-2 | 4 | 2 | Air | 16,838 | 16,837 | 99.99 | 7011 | 41.64 |
| PG4-3 | 4 | 3 | Air | 20,286 | 20,059 | 98.88 | 7888 | 39.32 |
| PG5 | 4 | Water 8 | 9302 | 8458 | 90.93 | 4453 | 52.65 | |
| PG5-1 | 5 | 1 | Air | 12,288 | 11,355 | 92.41 | 1248 | 10.99 |
| PG5-2 | 5 | 2 | Air | 16,337 | 7016 | 42.95 | 0 | 0 |
| PG5-3 | 5 | 3 | Air | 9328 | 9320 | 99.91 | 0 | 0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Libert, X.; Chasseur, C.; Packeu, A.; Bureau, F.; Roosens, N.H.; De Keersmaecker, S.C.J. Exploiting the Advantages of Molecular Tools for the Monitoring of Fungal Indoor Air Contamination: First Detection of Exophiala jeanselmei in Indoor Air of Air-Conditioned Offices. Microorganisms 2019, 7, 674. https://doi.org/10.3390/microorganisms7120674
Libert X, Chasseur C, Packeu A, Bureau F, Roosens NH, De Keersmaecker SCJ. Exploiting the Advantages of Molecular Tools for the Monitoring of Fungal Indoor Air Contamination: First Detection of Exophiala jeanselmei in Indoor Air of Air-Conditioned Offices. Microorganisms. 2019; 7(12):674. https://doi.org/10.3390/microorganisms7120674
Chicago/Turabian StyleLibert, Xavier, Camille Chasseur, Ann Packeu, Fabrice Bureau, Nancy H. Roosens, and Sigrid C. J. De Keersmaecker. 2019. "Exploiting the Advantages of Molecular Tools for the Monitoring of Fungal Indoor Air Contamination: First Detection of Exophiala jeanselmei in Indoor Air of Air-Conditioned Offices" Microorganisms 7, no. 12: 674. https://doi.org/10.3390/microorganisms7120674
APA StyleLibert, X., Chasseur, C., Packeu, A., Bureau, F., Roosens, N. H., & De Keersmaecker, S. C. J. (2019). Exploiting the Advantages of Molecular Tools for the Monitoring of Fungal Indoor Air Contamination: First Detection of Exophiala jeanselmei in Indoor Air of Air-Conditioned Offices. Microorganisms, 7(12), 674. https://doi.org/10.3390/microorganisms7120674







