Influences of Semaphorin 3A Expression on Clinicopathological Features, Human Papillomavirus Status, and Prognosis in Oropharyngeal Carcinoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Tissue Samples
2.2. Immunohistochemistry
2.3. Evaluation of SEMA3A Immunoreactivity
2.4. Evaluation of CD34 Immunoreactivity
2.5. Statistical Analyses
3. Results
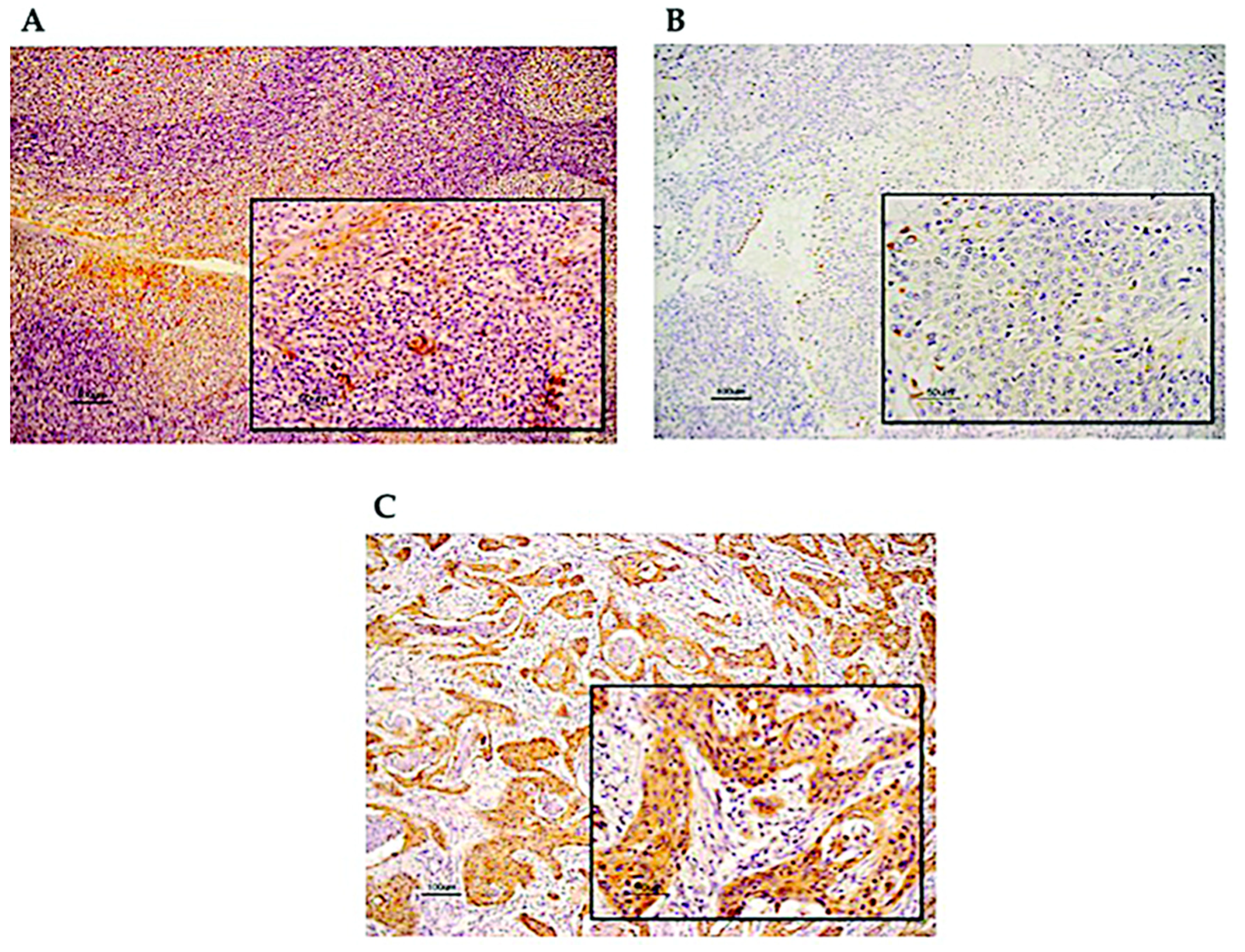
3.1. Immunohistochemical Analysis of SEMA3A Expression in OPC Tissues
3.2. Association between the Expression of SEMA3A and Various Clinicopathological Features
3.3. Association between the Expression of SEMA3A and Survival
3.4. Association between SEMA3A Expression and MVD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Jemal, A.; Lortet-Tieulent, J. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaturvedi, A.K.; Engels, E.A.; Pfeiffer, R.M.; Hernandez, B.Y.; Xiao, W.; Kim, E.; Jiang, B.; Goodman, M.T.; Sibug-Saber, M.; Cozen, W.; et al. Human Papillomavirus and Rising Oropharyngeal Cancer Incidence in the United States. J. Clin. Oncol. 2011, 29, 4294–4301. [Google Scholar] [CrossRef] [PubMed]
- Marur, S.; D’Souza, G.; Westra, W.H.; Forastiere, A.A. HPV-associated head and neck cancer: A virus-related cancer epidemic. Lancet Oncol. 2010, 11, 781–789. [Google Scholar] [CrossRef] [Green Version]
- Ramqvist, T.; Dalianis, T. Oropharyngeal Cancer Epidemic and Human Papillomavirus. Emerg. Infect. Dis. 2010, 16, 1671–1677. [Google Scholar] [CrossRef]
- Chaturvedi, A.K. Epidemiology and Clinical Aspects of HPV in Head and Neck Cancers. Head Neck Pathol. 2012, 6, 16–24. [Google Scholar] [CrossRef] [Green Version]
- Gillison, M.L.; Alemany, L.; Snijders, P.J.; Chaturvedi, A.; Steinberg, B.M.; Schwartz, S.; Castellsagué, X. Human Papillomavirus and Diseases of the Upper Airway: Head and Neck Cancer and Respiratory Papillomatosis. Vaccine 2012, 30, F34–F54. [Google Scholar] [CrossRef]
- Chaturvedi, A.K.; Engels, E.A.; Anderson, W.F.; Gillison, M.L. Incidence Trends for Human Papillomavirus-Related and -Unrelated Oral Squamous Cell Carcinomas in the United States. J. Clin. Oncol. 2008, 26, 612–619. [Google Scholar] [CrossRef] [Green Version]
- Auluck, A.; Hislop, G.; Bajdik, C.; Poh, C.; Zhang, L.; Rosin, M.P. Trends in oropharyngeal and oral cavity cancer incidence of human papillomavirus (HPV)-related and HPV-unrelated sites in a multicultural population. Br. Columbia Exp.Cancer 2010, 116, 2635–2644. [Google Scholar] [CrossRef]
- Chaturvedi, A.K.; Anderson, W.F.; Lortet-Tieulent, J.; Curado, M.P.; Ferlay, J.; Franceschi, S.; Rosenberg, P.S.; Bray, F.; Gillison, M.L. Worldwide Trends in Incidence Rates for Oral Cavity and Oropharyngeal Cancers. J. Clin. Oncol. 2013, 31, 4550–4559. [Google Scholar] [CrossRef] [Green Version]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Maxwell, J.H.; Kumar, B.; Feng, F.Y.; Worden, F.P.; Lee, J.S.; Eisbruch, A.; Wolf, G.T.; Prince, M.E.; Moyer, J.S.; Teknos, T.N.; et al. Tobacco use in human papillomavirus-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin. Cancer Res. 2010, 16, 1226–1235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dayyani, F.; Etzel, C.J.; Liu, M.; Ho, C.-H.; Lippman, S.M.; Tsao, A.S. Meta-analysis of the impact of human papillomavirus (HPV) on cancer risk and overall survival in head and neck squamous cell carcinomas (HNSCC). Head Neck Oncol. 2010, 2, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.; Nguyen-Tan, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human Papillomavirus and Survival of Patients with Oropharyngeal Cancer. N. Engl. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fakhry, C.; Westra, W.H.; Li, S.; Cmelak, A.; Ridge, J.A.; Pinto, H.; Forastiere, A.; Gillison, M.L. Improved Survival of Patients With Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma in a Prospective Clinical Trial. J. Natl. Cancer Inst. 2008, 100, 261–269. [Google Scholar] [CrossRef] [Green Version]
- Dahlstrand, H.M.; Lindquist, D.; Björnestål, L.; Ohlsson, A.; Dalianis, T.; Munck-Wikland, E.; Elmberger, G. P16(INK4a) correlates to human papillomavirus presence, response to radiotherapy and clinical outcome in tonsillar carcinoma. Anticancer. Res. 2005, 25, 4375–4383. [Google Scholar]
- Worden, F.; Kumar, B.; Lee, J.S.; Wolf, G.T.; Cordell, K.G.; Taylor, J.M.; Urba, S.G.; Eisbruch, A.; Teknos, T.N.; Chepeha, D.B.; et al. Chemoselection As a Strategy for Organ Preservation in Advanced Oropharynx Cancer: Response and Survival Positively Associated With HPV16 Copy Number. J. Clin. Oncol. 2008, 26, 3138–3146. [Google Scholar] [CrossRef]
- Lin, B.M.; Wang, H.; D’Souza, G.; Zhang, Z.; Fakhry, C.; Joseph, A.W.; Drake, V.E.; Sanguineti, G.; Westra, W.H.; Pai, S.I. Long term prognosis and risk factors among HPV-associated oropharyngeal squamous cell carcinoma patients. Cancer 2014, 119, 3462–3471. [Google Scholar] [CrossRef]
- Tamagnone, L.; Comoglio, P.M. To move or not to move? Semaphorin signalling in cell migration. EMBO Rep. 2004, 5, 356–361. [Google Scholar] [CrossRef]
- Kruger, R.P.; Aurandt, J.; Guan, K.-L. Semaphorins command cells to move. Nat. Rev. Mol. Cell Biol. 2005, 6, 789–800. [Google Scholar] [CrossRef]
- Li, K.; Chen, M.K.; Li, L.Y.; Lu, M.H.; Shao, C.K.; Su, Z.L.; He, D.; Pang, J.; Gao, X. The predictive value of semaphorins 3 expression in biopsies for biochemical recurrence of patients with low- and intermediate-risk prostate cancer. Neoplasma 2013, 60, 683–689. [Google Scholar] [CrossRef] [Green Version]
- Staton, C.A.; Shaw, L.A.; Valluru, M.; Hoh, L.; Koay, I.; Cross, S.S.; Reed, M.; Brown, N. Expression of class 3 semaphorins and their receptors in human breast neoplasia. Histopathology 2011, 59, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Miao, H.-Q.; Soker, S.; Feiner, L.; Alonso, J.L.; Raper, J.A.; Klagsbrun, M. Neuropilin-1 mediates collapsin-1/semaphorin III inhibition of endothelial cell motility: Functional competition of collapsin-1 and vascular endothelial growth factor-165. J. Cell Biol. 1999, 146, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Guttmann-Raviv, N.; Shraga-Heled, N.; Varshavsky, A.; Guimaraes-Sternberg, C.; Kessler, O.; Neufeld, G. Semaphorin-3A and Semaphorin-3F Work Together to Repel Endothelial Cells and to Inhibit Their Survival by Induction of Apoptosis. J. Biol. Chem. 2007, 282, 26294–26305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barresi, V.; Vitarelli, E.; Cerasoli, S. Semaphorin3A immunohistochemical expression in human meningiomas: Correlation with the microvessel density. Virchows Arch. 2009, 454, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Ebru, T.; Caloglu, V.Y.; Durankus, N.K.; Sut, N.; Turkkan, G.; Can, N.; Puyan, F.O.; Caloglu, M. Survivin expression, HPV positivity and microvessel density in oropharyngeal carcinomas and relationship with survival time. Arch. Med. Sci. 2017, 13, 1467–1473. [Google Scholar] [CrossRef]
- Kondo, S.; Wakae, K.; Wakisaka, N.; Nakanishi, Y.; Ishikawa, K.; Komori, T.; Moriyama-Kita, M.; Endo, K.; Murono, S.; Wang, Z.; et al. APOBEC3A associates with human papillomavirus genome integration in oropharyngeal cancers. Oncogene 2017, 36, 1687–1697. [Google Scholar] [CrossRef]
- Conner, K.L.; Shaik, A.N.; Ekinci, E.; Kim, S.; Ruterbusch, J.J.; Cote, M.L.; Patrick, S.M. HPV induction of APOBEC3 enzymes mediate overall survival and response to cisplatin in head and neck cancer. DNA Repair 2020, 87, 102802. [Google Scholar] [CrossRef]
- Kano, M.; Kondo, S.; Wakisaka, N.; Wakae, K.; Aga, M.; Moriyama-Kita, M.; Ishikawa, K.; Ueno, T.; Nakanishi, Y.; Hatano, M.; et al. Expression of estrogen receptor alpha is associated with pathogenesis and prognosis of human papillomavirus-positive oropharyngeal cancer. Int. J. Cancer 2019, 145, 1547–1557. [Google Scholar] [CrossRef]
- The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986. [CrossRef]
- Kuzu, I.; Bicknell, R.; Harris, A.L.; Jones, M.; Gatter, K.C.; Mason, D.Y. Heterogeneity of vascular endothelial cells with relevance to diagnosis of vascular tumours. J. Clin. Pathol. 1992, 45, 143–148. [Google Scholar] [CrossRef] [Green Version]
- Elrefaey, S.; Massaro, M.; Chiocca, S.; Chiesa, F.; Ansarin, M. HPV in oropharyngeal cancer: The basics to know in clinical practice. Acta Otorhinolaryngol. Ital. 2014, 34, 299–309. [Google Scholar] [PubMed]
- Kreimer, A.R.; Johansson, M.; Waterboer, T.; Kaaks, R.; Chang-Claude, J.; Drogen, D.; Tjønneland, A.; Overvad, K.; Quirós, J.R.; González, C.A.; et al. Evaluation of Human Papillomavirus Antibodies and Risk of Subsequent Head and Neck Cancer. J. Clin. Oncol. 2013, 31, 2708–2715. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.; Hoffmann, M.; Scheunemann, D.; Fazel, A.; Görögh, T.; Kahn, T.; Gottschlich, S. Human papillomavirus and p53 polymorphism in codon 72 in head and neck squamous cell carcinoma. Oncol. Rep. 2009, 21, 809–814. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Qi, L.; Wang, F.; Sun, Z.; Huang, Z.; Xi, Q. Decreased semaphorin 3A expression is associated with a poor prognosis in patients with epithelial ovarian carcinoma. Int. J. Mol. Med. 2015, 35, 1374–1380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, C.; Gao, X.; Liu, H.; Jiang, T.; Zhai, X. Decreased expression of SEMA3A is associated with poor prognosis in gastric carcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 4782–4794. [Google Scholar]
- Song, X.; Zhang, W.; Zhang, Y.; Zhang, H.; Fu, Z.; Ye, J.; Liu, L.; Wu, Y. Expression of semaphorin 3A and neuropilin 1 with clinicopathological features and survival in human tongue cancer. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e962–e968. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Chen, J.; Zhang, W.; Zheng, Y.; Wang, Z.; Liu, L.; Wu, H.; Ye, J.; Qi, B.; Wu, Y.; et al. Axon guidance molecule semaphorin3A is a novel tumor suppressor in head and neck squamous cell carcinoma. Oncotarget 2016, 7, 6048–6062. [Google Scholar] [CrossRef]
- Bielenberg, D.R.; Zetter, B.R. The Contribution of Angiogenesis to the Process of Metastasis. Cancer J. Sudbury Mass 2015, 21, 267–273. [Google Scholar] [CrossRef] [Green Version]
- Ma, J.; Lu, H.; Wang, S.; Chen, B.; Liu, Z.; Ke, X.; Liu, T.; Fu, J. The anthraquinone derivative Emodin inhibits angiogenesis and metastasis through downregulating Runx2 activity in breast cancer. Int. J. Oncol. 2015, 46, 1619–1628. [Google Scholar] [CrossRef]
- Vassilakopoulou, M.; Psyrri, A.; Argiris, A. Targeting angiogenesis in head and neck cancer. Oral Oncol. 2015, 51, 409–415. [Google Scholar] [CrossRef]
- Zhang, X.; Yamashita, M.; Uetsuki, H.; Kakehi, Y. Angiogenesis in renal cell carcinoma: Evaluation of microvessel density, vascular endothelial growth factor and matrix metalloproteinases. Int. J. Urol. 2002, 9, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Raible, D.; Raper, J.A. Collapsin: A protein in brain that induces the collapse and paralysis of neuronal growth cones. Cell 1993, 75, 217–227. [Google Scholar] [CrossRef]
- Acevedo, L.M.; Barillas, S.; Weis, S.M.; Göthert, J.R.; Cheresh, D.A. Semaphorin 3A suppresses VEGF-mediated angiogenesis yet acts as a vascular permeability factor. Blood 2008, 111, 2674–2680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakurai, A.; Doci, C.; Gutkind, J.S. Semaphorin signaling in angiogenesis, lymphangiogenesis and cancer. Cell Res. 2012, 22, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Maione, F.; Capano, S.; Regano, D.; Zentilin, L.; Giacca, M.; Casanovas, O.; Bussolino, F.; Serini, G.; Giraudo, E. Semaphorin 3A overcomes cancer hypoxia and metastatic dissemination induced by antiangiogenic treatment in mice. J. Clin. Investig. 2012, 122, 1832–1848. [Google Scholar] [CrossRef] [Green Version]
- Shih, T.; Lindley, C. Bevacizumab: An angiogenesis inhibitor for the treatment of solid malignancies. Clin. Ther. 2006, 28, 1779–1802. [Google Scholar] [CrossRef]
- Meyer, M.; Meinrath, J.; Seehawer, J.; Lechner, A.; Odenthal, M.; Quaas, A.; Semrau, R.; Huebbers, C.; Marnitz, S.; Büttner, R.; et al. The relevance of the lymph node ratio as predictor of prognosis is higher in HPV-negative than in HPV-positive oropharyngeal squamous cell carcinoma. Clin. Otolaryngol. 2018, 43, 192–198. [Google Scholar] [CrossRef]
- Sedaghat, A.R.; Zhang, Z.; Begum, S.; Palermo, R.; Best, S.; Ulmer, K.M.; Levine, M.; Zinreich, E.; Messing, B.P.; Gold, D.; et al. Prognostic significance of human papillomavirus in oropharyngeal squamous cell carcinomas. Laryngoscope 2009, 119, 1542–1549. [Google Scholar] [CrossRef]


| No. | SEMA3A | |||
|---|---|---|---|---|
| Low | High | p | ||
| Tumor | 32 | 19 | 13 | 0.005 |
| Chronic tonsillitis | 17 | 3 | 14 | |
| Characteristic | SEMA3A | |||
|---|---|---|---|---|
| Low | High | p | ||
| Sex | 0.314 | |||
| Male | 25 | 16 | 9 | |
| Female | 7 | 3 | 4 | |
| Age (years) | 0.683 | |||
| ≤50 | 4 | 2 | 2 | |
| >50 | 28 | 17 | 11 | |
| Subsite | 0.722 | |||
| Lateral (tonsil and pillars) | 21 | 12 | 9 | |
| Frontal (base of tongue) Upper (soft palate, uvula) Posterior | 11 | 7 | 4 | |
| TNM stage | 0.654 | |||
| I-II | 14 | 9 | 5 | |
| III-IV | 16 | 9 | 7 | |
| Tumor stage | 0.757 | |||
| T1-2 (early) | 19 | 11 | 8 | |
| T3-4 (advanced) | 11 | 7 | 4 | |
| Lymph node metastasis | 0.543 | |||
| N0 (negative) | 12 | 8 | 4 | |
| N1-3 (positive) | 18 | 10 | 8 | |
| HPV | 0.821 | |||
| Positive | 14 | 8 | 6 | |
| Negative | 18 | 11 | 7 | |
| Smoking | 0.515 | |||
| Never | 12 | 8 | 4 | |
| Past and present | 20 | 11 | 9 | |
| Alcohol | 0.719 | |||
| Never | 16 | 10 | 6 | |
| Past and present | 16 | 9 | 7 | |
| Histological grade Poorly | 11 | 4 | 7 | 0.159 |
| Moderately Well | 14 7 | 10 5 | 4 2 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pham, H.T.; Kondo, S.; Endo, K.; Wakisaka, N.; Aoki, Y.; Nakanishi, Y.; Kase, K.; Mizokami, H.; Kano, M.; Ueno, T.; et al. Influences of Semaphorin 3A Expression on Clinicopathological Features, Human Papillomavirus Status, and Prognosis in Oropharyngeal Carcinoma. Microorganisms 2020, 8, 1286. https://doi.org/10.3390/microorganisms8091286
Pham HT, Kondo S, Endo K, Wakisaka N, Aoki Y, Nakanishi Y, Kase K, Mizokami H, Kano M, Ueno T, et al. Influences of Semaphorin 3A Expression on Clinicopathological Features, Human Papillomavirus Status, and Prognosis in Oropharyngeal Carcinoma. Microorganisms. 2020; 8(9):1286. https://doi.org/10.3390/microorganisms8091286
Chicago/Turabian StylePham, Hai Thanh, Satoru Kondo, Kazuhira Endo, Naohiro Wakisaka, Yoshitaka Aoki, Yosuke Nakanishi, Kina Kase, Harue Mizokami, Makoto Kano, Takayoshi Ueno, and et al. 2020. "Influences of Semaphorin 3A Expression on Clinicopathological Features, Human Papillomavirus Status, and Prognosis in Oropharyngeal Carcinoma" Microorganisms 8, no. 9: 1286. https://doi.org/10.3390/microorganisms8091286




