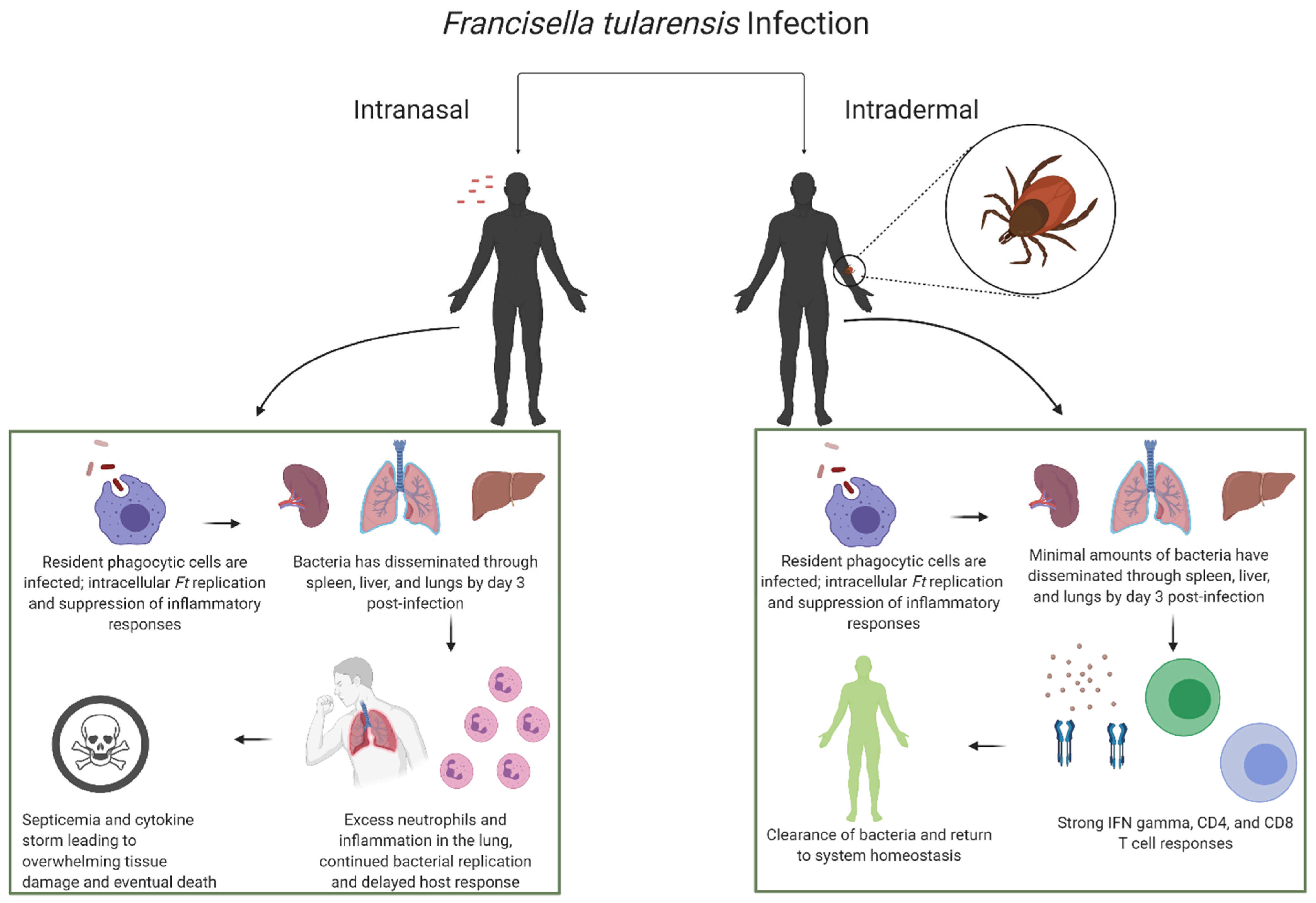
Differential Immune Response Following Intranasal and Intradermal Infection with Francisella tularensis: Implications for Vaccine Development
Abstract
:1. Introduction
2. Vector-Borne Intradermal Infections and Aerogenic Exposure
3. Intradermal and Intranasal Infection Models for LVS
3.1. Rabbits
3.1.1. Rabbits–Intradermal
3.1.2. Rabbits–Intranasal
3.2. Rodents
3.2.1. Rodents–Intradermal
3.2.2. Rodents–Intranasal
3.3. Non-Human Primates
3.3.1. Non-Human Primates–Intradermal
3.3.2. Non-Human Primates–Intranasal
3.4. Humans
3.4.1. Humans–Intradermal
3.4.2. Humans–Intranasal
3.5. Animal Model Overview
4. Immune Response and Vaccines
4.1. Primary Infection
4.2. Vaccination
| Species | % Protection (Respiratory Route) | % Protection (Non-Respiratory Route) | Non-Respiratory Vaccine Route | Refs. |
|---|---|---|---|---|
| Human | 100 | 54 | Scarification | [8] |
| Rhesus macaque | 88 | 63 | Intradermal | [61] |
| Guinea pig | 60 | 5 | Subcutaneous | [61] |
| Mouse (BALB/c) | 40 | 0 | Subcutaneous | [96] |
| Mouse (BALB/c) | 60 | 0 | Intradermal | [78] |
| Mouse (C57BL/6) | 100 * | n.d. | n.a. | [92] |
| Mouse (C57BL/6) | 0–10 * | 0–10 | Scarification, Intradermal, subcutaneous | [49,78,96,114] |
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Petersen, J.M.; Mead, P.S.; Schriefer, M.E. Francisella Tularensis: An Arthropod-Borne Pathogen. Veter. Res. 2009, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spickler, R. Tularemia. Available online: http://www.cfsph.iastate.edu/DiseaseInfo/factsheets.php (accessed on 25 March 2021).
- Ellis, J.; Oyston, P.C.F.; Green, M.; Titball, R.W. Tularemia. Clin. Microbiol. Rev. 2002, 15, 631–646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maurin, M.; Gyuranecz, M. Tularaemia: Clinical Aspects in Europe. Lancet Infect. Dis. 2016, 16, 113–124. [Google Scholar] [CrossRef]
- Roberts, L.M.; Powell, D.A.; Frelinger, J.A. Adaptive Immunity to Francisella Tularensis and Considerations for Vaccine Development. Front. Cell. Infect. Microbiol. 2018, 8, 115. [Google Scholar] [CrossRef] [Green Version]
- Hong, K.-J.; Park, P.-G.; Seo, S.-H.; Rhie, G.-E.; Hwang, K.-J. Current Status of Vaccine Development for Tularemia Preparedness. Clin. Exp. Vaccine Res. 2013, 2, 34. [Google Scholar] [CrossRef] [PubMed]
- Conlan, J.W.; Oyston, P.C. Vaccines Against Francisella Tularensis. Ann. New York Acad. Sci. 2007, 1105, 325–350. [Google Scholar] [CrossRef]
- Hornick, R.B.; Eigelsbach, H.T. Aerogenic Immunization of Man with Live Tularemia Vaccine. Bacteriol. Rev. 1966, 30, 532–538. [Google Scholar] [CrossRef]
- Cowley, S.C.; Elkins, K.L. Immunity to Francisella. Front. Microbiol. 2011, 2, 26. [Google Scholar] [CrossRef] [Green Version]
- Munseri, P.J.; Kroidl, A.; Nilsson, C.; Geldmacher, C.; Mann, P.; Moshiro, C.; Aboud, S.; Lyamuya, E.; Maboko, L.; Missanga, M.; et al. Priming with a Simplified Intradermal HIV-1 DNA Vaccine Regimen followed by Boosting with Recombinant HIV-1 MVA Vaccine Is Safe and Immunogenic: A Phase IIa Randomized Clinical Trial. PLoS ONE 2015, 10. [Google Scholar] [CrossRef]
- Sánchez, V.R.; Fenoy, I.M.; Picchio, M.S.; Soto, A.S.; Arcon, N.; Goldman, A.; Martin, V. Homologous Prime-Boost Strategy with TgPI-1 Improves the Immune Response and Protects Highly Susceptible Mice against Chronic Toxoplasma Gondii Infection. Acta Trop. 2015, 150, 159–165. [Google Scholar] [CrossRef]
- Foil, L.D. Tabanids as Vectors of Disease Agents. Parasitol. Today 1989, 5, 88–96. [Google Scholar] [CrossRef]
- Jellison, W.L. Tularemia Geographical Distribution of “Deerfly Fever” and the BitingFly, Chrysops Discalis Williston. Public Health Rep. 1950, 65, 1321–1329. [Google Scholar] [CrossRef]
- Krinsky, W.L. Animal Disease Agents Transmitted by Horse Flies and Deer Flies (Diptera: Tabanidae). J. Med. Entomol. 1976, 13, 225–275. [Google Scholar] [CrossRef]
- Eliasson, H.; Bäck, E. Tularaemia in An Emergent Area in Sweden: An Analysis of 234 Cases in Five Years. Scand. J. Infect. Dis. 2007, 39, 880–889. [Google Scholar] [CrossRef] [PubMed]
- Movert, E.; Wu, Y.; Lambeau, G.; Kahn, F.; Touqui, L.; Areschoug, T. Using Patient Pathways to Accelerate the Drive to Ending Tuberculosis. J. Infect. Dis. 2013, 208, 2025–2035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopla, C. Multiplication of Tularemia Organisms in the Lone Star Tick. Can. J. Comp. Med. Vet. Sci. 1955, 19, 255. [Google Scholar]
- Saliba, G.S.; Harmston, F.C.; Diamond, B.E.; Zymet, C.L.; Goldenberg, M.I.; Chin, T.D. An Outbreak of Human Tularemia Associated with the American Dog Tick, Dermacentor Variabilis. Am. J. Trop. Med. Hyg. 1966, 15, 531–538. [Google Scholar] [CrossRef]
- Markowitz, L.E.; Hynes, N.A.; Cruz, P.; Campos, E.; Barbaree, J.M.; Plikaytis, B.D.; Mosier, D.; Kaufmann, A.F. Tick-Borne Tularemia: An Outbreak of Lymphadenopathy in Children. JAMA 1985, 254, 2922–2925. [Google Scholar] [CrossRef] [PubMed]
- Feldman, K.A.; Enscore, R.E.; Lathrop, S.L.; Matyas, B.T.; McGuill, M.; Schriefer, M.E.; Stiles-Enos, D.; Dennis, D.T.; Petersen, L.R.; Hayes, E.B. An Outbreak of Primary Pneumonic Tularemia on Martha’s Vineyard. N. Engl. J. Med. 2001, 345, 1601–1606. [Google Scholar] [CrossRef]
- Dahlstrand, S.; Ringertz, O.; Zetterberg, B. Airborne Tularemia in Sweden. Scand. J. Infect. Dis. 1971, 3, 7–16. [Google Scholar] [CrossRef]
- Teutsch, S.M.; Martone, W.J.; Brink, E.W.; Potter, M.E.; Eliot, G.; Hoxsie, R.; Craven, R.B.; Kaufmann, A.F. Pneumonic Tularemia on Martha’s Vineyard. N. Engl. J. Med. 1979, 301, 826–828. [Google Scholar] [CrossRef]
- Pittman, B.; Shaw, E.J.; Cherry, W. Isolation of Francisella Tularensis from Infected Frozen Human Blood. J. Clin. Microbiol. 1977, 5, 621–624. [Google Scholar]
- Halsted, C.; Kulasinghe, H. Tularemia Pneumonia in Urban Children. Pediatrics 1978, 61, 660–662. [Google Scholar]
- Martone, W.J. Tularemia Pneumonia in Washington, DC: A Report of Three Cases with Possible Common-Source Exposures. JAMA 1979, 242, 2315–2317. [Google Scholar] [CrossRef]
- Hepburn, M.J.; Purcell, B.K.; Lawler, J.V.; Coyne, S.R.; Petitt, P.L.; Sellers, K.D.; Norwood, D.A.; Ulrich, M.P. Live Vaccine Strain Francisella Tularensis Is Detectable at the Inoculation Site but Not in Blood after Vaccination against Tularemia. Clin. Infect. Dis. 2006, 43, 711–716. [Google Scholar] [CrossRef] [Green Version]
- Poquet, Y.; Kroca, M.; Halary, F.; Stenmark, S.; Peyrat, M.A.; Bonneville, M.; Fournié, J.J.; Sjöstedt, A. Expansion of Vγ9Vδ2 T Cells is Triggered by Francisella Tularensis—Derived Phosphoantigens in Tularemia but not after Tularemia Vaccination. Infect. Immun. 1998, 66, 2107–2114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schricker, R.L.; Eigelsbach, H.T.; Mitten, J.Q.; Hall, W.C. Pathogenesis of Tularemia in Monkeys Aerogenically Exposed to Francisella Tularensis 425. Infect. Immun. 1972, 5, 734–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eigelsbach, H.; Downs, C. Prophylactic Effectiveness of Live and Killed Tularemia Vaccines. I. Production of Vaccine and Evaluation in the White Mouse and Guinea Pig-PubMed. J. Immunol. 1961, 87, 415–425. [Google Scholar] [PubMed]
- Stenmark, S.; Sunnemark, D.; Bucht, A.; Sjöstedt, A. Rapid Local Expression of Interleukin-12, Tumor Necrosis Factor Alpha, and Gamma Interferon after Cutaneous Francisella tularensis Infection in Tularemia-Immune Mice. Infect. Immun. 1999, 67, 1789–1797. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.R.; Adney, D.R.; Bielefeldt-Ohmann, H.; Gordy, P.W.; Felix, T.A.; Olea-Popelka, F.J.; Bowen, R.A. Pathogenesis and Immune Responses of Francisella Tularensis Strains in Wild-Caught Cottontail Rabbits (Sylvilagus Spp.). J. Wildl. Dis. 2015, 51, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Saslaw, S.; Eigelsbach, H.T.; Prior, J.A.; Wilson, H.E.; Carhart, S. Tularemia Vaccine Study. II. Respiratory Challenge. Arch. Intern. Med. 1961, 107, 702–714. [Google Scholar] [CrossRef]
- Saslaw, S.; Eigelsbach, H.T.; Wilson, H.E.; Prior, J.A.; Carhart, S. Tularemia Vaccine Study. I. Intracutaneous Challenge. Arch. Intern. Med. 1961, 107, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Molins, C.R.; DeLorey, M.J.; Yockey, B.M.; Young, J.W.; Sheldon, S.W.; Reese, S.M.; Schriefer, M.E.; Petersen, J.M. Virulence Differences Among Francisella Tularensis Subsp. Tularensis Clades in Mice. PLoS ONE 2010, 5, 10205. [Google Scholar] [CrossRef]
- Molins, C.R.; DeLorey, M.J.; Yockey, B.M.; Young, J.W.; Belisle, J.T.; Schriefer, M.E.; Petersen, J.M. Virulence Difference between the Prototypic Schu S4 Strain (A1a) and Francisella TularensisA1a, A1b, A2 and Type B Strains in a Murine Model of Infection. BMC Infect. Dis. 2014, 14, 67. [Google Scholar] [CrossRef]
- Reed, D.S.; Smith, L.P.; Cole, K.S.; Santiago, A.E.; Mann, B.J.; Barry, E.M. Live Attenuated Mutants of Francisella tularensis Protect Rabbits against Aerosol Challenge with a Virulent Type A Strain. Infect. Immun. 2014, 82, 2098–2105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pasetti, M.F.; Cuberos, L.; Horn, T.L.; Shearer, J.D.; Matthews, S.J.; House, R.V.; Sztein, M.B. An Improved Francisella Tularensis Live Vaccine Strain (LVS) is Well Tolerated and Highly Immunogenic when Administered to Rabbits in Escalating Doses Using Various Immunization Routes. Vaccine 2008, 26, 1773–1785. [Google Scholar] [CrossRef] [Green Version]
- Stinson, E.; Smith, L.P.; Cole, K.S.; Barry, E.M.; Reed, D.S. Respiratory and Oral Vaccination Improves Protection Conferred by the Live Vaccine Strain against Pneumonic Tularemia in the Rabbit Model. Pathog. Dis. 2016, 74. [Google Scholar] [CrossRef] [Green Version]
- O’Malley, K.J.; Bowling, J.L.; Stinson, E.; Cole, K.S.; Mann, B.J.; Namjoshi, P.; Hazlett, K.R.O.; Barry, E.M.; Reed, D.S. Aerosol Prime-Boost Vaccination provides Strong Protection in Outbred Rabbits against Virulent type A Francisella Tularensis. PLoS ONE 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Ray, H.J.; Chu, P.; Wu, T.H.; Lyons, C.R.; Murthy, A.K.; Guentzel, M.N.; Klose, K.E.; Arulanandam, B.P. The Fischer 344 Rat Reflects Human Susceptibility to Francisella Pulmonary Challenge and Provides a New Platform for Virulence and Protection Studies. PLoS ONE 2010, 5. [Google Scholar] [CrossRef] [Green Version]
- Jemski, J.V. Respiratory Tularemia: Comparison of Selected Routes of Vaccination in Fischer 344 Rats. Infect. Immun. 1981, 34, 766–772. [Google Scholar] [CrossRef] [Green Version]
- Conlan, J.W.; Sjöstedt, A.; North, R.J. CD4+ and CD8+ T-Cell-Dependent and -Independent Host Defense Mechanisms can Operate to Control and Resolve Primary and Secondary Francisella Tularensis LVS Infection in Mice. Infect. Immun. 1994, 62, 5603–5607. [Google Scholar] [CrossRef] [Green Version]
- Eneslätt, K.; Normark, M.; Björk, R.; Rietz, C.; Zingmark, C.; Wolfraim, L.A.; Stöven, S.; Sjöstedt, A. Signatures of T Cells as Correlates of Immunity to Francisella tularensis. PLoS ONE 2012, 7, e32367. [Google Scholar] [CrossRef] [PubMed]
- Elkins, K.L.; Colombini, S.M.; Meierovics, A.I.; Chu, M.C.; Chou, A.Y.; Cowley, S.C. Survival of Secondary Lethal Systemic Francisella LVS Challenge depends Largely on Interferon Gamma. Microbes Infect. 2010, 12, 28–36. [Google Scholar] [CrossRef]
- Cowley, S.C.; Goldberg, M.F.; Ho, J.A.; Elkins, K.L. The Membrane Form of Tumor Necrosis Factor Is Sufficient to Mediate Partial Innate Immunity to Francisella Tularensis Live Vaccine Strain. J. Infect. Dis. 2008, 198, 284–292. [Google Scholar] [CrossRef] [Green Version]
- Roberts, L.M.; Davies, J.S.; Sempowski, G.D.; Frelinger, J.A. IFN-γ, but not IL-17A, is required for survival during secondary pulmonary Francisella tularensis Live Vaccine Stain infection. Vaccine 2014, 32, 3595–3603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conlan, J.W.; Zhao, X.; Harris, G.; Shen, H.; Bolanowski, M.; Rietz, C.; Sjostedt, A.; Chen, W. Molecular Immunology of Experimental Primary Tularemia in Mice infected by Respiratory or Intradermal Routes with Type A Francisella Tularensis. Mol. Immunol. 2008, 45, 2962–2969. [Google Scholar] [CrossRef] [Green Version]
- Kurtz, S.L.; Bosio, C.M.; De Pascalis, R.; Elkins, K.L. GM-CSF has Disparate Roles during Intranasal and Intradermal Francisella Tularensis Infection. Microbes Infect. 2016, 18, 758–767. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Shen, H.; Webb, A.; KuoLee, R.; Conlan, J.W. Tularemia in BALB/c and C57Bl/6 Mice Vaccinated with Francisella Tularensis LVS and Challenged Intradermally, or by Aerosol with Virulent Isolates of the Pathogen: Protection Varies Depending on Pathogen Virulence, Route of Exposure, and Host Genetic Back. Vaccine 2003, 21, 3690–3700. [Google Scholar] [CrossRef]
- Henry, T.; Kirimanjeswara, G.S.; Ruby, T.; Jones, J.W.; Peng, K.; Perret, M.; Ho, L.; Sauer, J.-D.; Iwakura, Y.; Metzger, D.W.; et al. Type I IFN Signaling Constrains IL-17A/F Secretion by γδ T Cells during Bacterial Infections. J. Immunol. 2010, 184, 3755–3767. [Google Scholar] [CrossRef] [Green Version]
- Stanley, S.A.; Johndrow, J.E.; Manzanillo, P.; Cox, J.S. The Type I IFN Response to Infection with Mycobacterium tuberculosis Requires ESX-1-Mediated Secretion and Contributes to Pathogenesis. J. Immunol. 2007, 178, 3143–3152. [Google Scholar] [CrossRef] [Green Version]
- Carrero, J.A.; Calderon, B.; Unanue, E.R. Lymphocytes are Detrimental during the Early Innate Immune Response against Listeria Monocytogenes. J. Exp. Med. 2006, 203, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Fan, Y.; Joyee, A.G.; Wang, S.; Han, X.; Bai, H.; Jiao, L.; Van Rooijen, N.; Yang, X. Type I IFNs Enhance Susceptibility toChlamydia muridarumLung Infection by Enhancing Apoptosis of Local Macrophages. J. Immunol. 2008, 181, 2092–2102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagarajan, U.M.; Prantner, D.; Sikes, J.D.; Andrews, C.W.; Goodwin, A.M.; Nagarajan, S.; Darville, T. Type I Interferon Signaling Exacerbates Chlamydia muridarum Genital Infection in a Murine Model. Infect. Immun. 2008, 76, 4642–4648. [Google Scholar] [CrossRef] [Green Version]
- O’Connell, R.M.; Saha, S.K.; Vaidya, S.A.; Bruhn, K.W.; Miranda, G.A.; Zarnegar, B.; Perry, A.K.; Nguyen, B.O.; Lane, T.F.; Taniguchi, T.; et al. Type I Interferon Production Enhances Susceptibility to Listeria monocytogenes Infection. J. Exp. Med. 2004, 200, 437–445. [Google Scholar] [CrossRef] [Green Version]
- Auerbuch, V.; Brockstedt, D.G.; Meyer-Morse, N.; O’Riordan, M.; Portnoy, D.A. Mice Lacking the Type I Interferon Receptor Are Resistant to Listeria Monocytogenes. J. Exp. Med. 2004, 200, 527–533. [Google Scholar] [CrossRef] [Green Version]
- Sjostedt, A.; Conlan, J.W.; North, R.J. Neutrophils are Critical for Host Defense against Primary Infection with the Facultative Intracellular Bacterium Francisella Tularensis in Mice and Participate in Defense against Reinfection. Infect. Immun. 1994, 62, 2779–2783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, L.M.; Tuladhar, S.; Steele, S.P.; Riebe, K.J.; Chen, C.J.; Cumming, R.; Seay, S.; Frothingham, R.; Sempowski, G.D.; Kawula, T.H.; et al. Identification of Early Interactions between Francisella and the Host. Infect. Immun. 2014, 82, 2504–2510. [Google Scholar] [CrossRef] [Green Version]
- Wu, T.H.; Zsemlye, J.L.; Statom, G.L.; Hutt, J.A.; Schrader, R.M.; Scrymgeour, A.A.; Lyons, C.R. Vaccination of Fischer 344 Rats against Pulmonary Infections by Francisella Tularensis Type A Strains. Vaccine 2009, 27, 4684–4693. [Google Scholar] [CrossRef] [Green Version]
- Hutt, J.A.; Lovchik, J.A.; Dekonenko, A.; Hahn, A.C.; Wu, T.H. The Natural History of Pneumonic Tularemia in Female Fischer 344 Rats after Inhalational Exposure to Aerosolized Francisella Tularensis Subspecies Tularensis Strain SCHU S4. Am. J. Pathol. 2017, 187, 252–267. [Google Scholar] [CrossRef] [Green Version]
- Eigelsbach, H.T.; Tulis, J.J.; Overholt, E.L.; Griffith, W.R. Aerogenic Immunization of the Monkey and Guinea Pig with Live Tularemia Vaccine. Proc. Soc. Exp. Biol. Med. 1961, 108, 732–734. [Google Scholar] [CrossRef] [PubMed]
- Sellers, R.S.; Clifford, C.B.; Treuting, P.M.; Brayton, C. Immunological Variation between Inbred Laboratory Mouse Strains: Points to Consider in Phenotyping Genetically Immunomodified Mice. Vet. Pathol. 2012, 49, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Martínez, F.O. Regulators of Macrophage Activation. Eur. J. Immunol. 2011, 41, 1531–1534. [Google Scholar] [CrossRef] [PubMed]
- Day, W.C.; Berendt, R.F. Experimental Tularemia in Macaca Mulatta: Relationship of Aerosol Particle Size to the Infectivity of Airborne Pasteurella Tularensis. Infect. Immun. 1972, 5, 77–82. [Google Scholar] [CrossRef] [Green Version]
- Tulis, J.J.; Eigelsbach, H.T.; Kerpsack, R.W. Host-Parasite Relationship in Monkeys Administered Live Tularemia Vaccine. Am. J. Pathol. 1970, 58, 329–336. [Google Scholar]
- Nelson, M.; Lever, M.S.; Savage, V.L.; Salguero, F.J.; Pearce, P.C.; Stevens, D.J.; Simpson, A.J.H. Establishment of Lethal Inhalational Infection with Francisella Tularensis (Tularaemia) in the Common Marmoset (Callithrix Jacchus). Int. J. Exp. Pathol. 2009, 90, 109–118. [Google Scholar] [CrossRef]
- Rick Lyons, C.; Wu, T.H. Animal Models of Francisella Tularensis Infection. Ann. New York Acad. Sci. 2007, 1105, 238–265. [Google Scholar] [CrossRef] [PubMed]
- Kadull, P.J.; Reames, H.R.; Coriell, L.L.; Foshay, L. Studies on Tularemia. V. Immunization of Man. J. Immunol. 1950, 65, 425–435. [Google Scholar]
- Foshay, L.; Hesselbrock, W.H.; Wittenberg, H.J.; Rodenberg, A.H. Vaccine Prophylaxis against Tularemia in Man. Am. J. Public Health Nations Health 1942, 32, 1131–1145. [Google Scholar] [CrossRef] [PubMed]
- El Sahly, H.M.; Atmar, R.L.; Patel, S.M.; Wells, J.M.; Cate, T.; Ho, M.; Guo, K.; Pasetti, M.F.; Lewis, D.E.; Sztein, M.B.; et al. Safety, Reactogenicity and Immunogenicity of Francisella Tularensis Live Vaccine Strain in Humans. Vaccine 2009, 27, 4905–4911. [Google Scholar] [CrossRef] [Green Version]
- Tärnvik, A. Nature of Protective Immunity to Francisella Tularensis. Rev. Infect. Dis. 1989, 11, 440–451. [Google Scholar] [CrossRef]
- Burke, D. Immunization against Tularemia: Analysis of the Effectiveness of Live Francisella tularensis Vaccine in Prevention of Laboratory-Acquired Tularemia. J. Infect. Dis. 1976, 135, 55–60. [Google Scholar] [CrossRef]
- Binesse, J.; Lindgren, H.; Conlan, W.; Sjöstedt, A. Roles of Reactive Oxygen Species-Degrading Enzymes of Francisella Tularensis SCHU S4. Infect. Immun. 2015, 83, 2255–2263. [Google Scholar] [CrossRef] [Green Version]
- Edwards, J.A.; Rockx-Brouwer, D.; Nair, V.; Celli, J. Restricted Cytosolic Growth of Francisella Tularensis Subsp. Tularensis by IFN-γ Activation of Macrophages. Microbiology 2010, 156, 327–339. [Google Scholar] [CrossRef] [Green Version]
- Lopez, M.C.; Duckett, N.S.; Baron, S.D.; Metzger, D.W. Early Activation of NK Cells after Lung Infection with the Intracellular Bacterium, Francisella Tularensis LVS. Cell. Immunol. 2004, 232, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Henry, T.; Brotcke, A.; Weiss, D.S.; Thompson, L.J.; Monack, D.M. Type I Interferon Signaling is Required for Activation of the Inflammasome during Francisella Infection. J. Exp. Med. 2007, 204, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Skyberg, J.A.; Rollins, M.F.; Samuel, J.W.; Sutherland, M.D.; Belisle, J.T.; Pascual, D.W. Interleukin-17 Protects against the Francisella Tularensis Live Vaccine Strain but Not against a Virulent F. Tularensis Type A Strain. Infect. Immun. 2013, 81, 3099–3105. [Google Scholar] [CrossRef] [Green Version]
- Conlan, J.W.; Shen, H.; Kuo Lee, R.; Zhao, X.; Chen, W. Aerosol-, but not Intradermal-Immunization with the Live Vaccine Strain of Francisella Tularensis Protects Mice against Subsequent Aerosol Challenge with a Highly Virulent Type A Strain of the Pathogen by an αβ T Cell- and Interferon Gamma- Dependent Mechanism. Vaccine 2005, 23, 2477–2485. [Google Scholar] [CrossRef]
- Anderson, R.V.; Crane, D.D.; Bosio, C.M. Long lived Protection against Pneumonic Tularemia is correlated with Cellular Immunity in Peripheral, not Pulmonary, Organs. Vaccine 2010, 28, 6562–6572. [Google Scholar] [CrossRef] [Green Version]
- Melillo, A.A.; Foreman, O.; Bosio, C.M.; Elkins, K.L. T-bet Regulates Immunity to Francisella Tularensis Live Vaccine Strain Infection, Particularly in Lungs. Infect. Immun. 2014, 82, 1477–1490. [Google Scholar] [CrossRef] [Green Version]
- Melillo, A.A.; Foreman, O.; Elkins, K.L. IL-12Rβ2 is Critical for Survival of Primary Francisella Tularensis LVS Infection. J. Leukoc. Biol. 2013, 93, 657–667. [Google Scholar] [CrossRef] [Green Version]
- Kurtz, S.L.; Foreman, O.; Bosio, C.M.; Anver, M.R.; Elkins, K.L. Interleukin-6 Is Essential for Primary Resistance to Francisella tularensis Live Vaccine Strain Infection. Infect. Immun. 2012, 81, 585–597. [Google Scholar] [CrossRef] [Green Version]
- Cowley, S.C.; Sedgwick, J.D.; Elkins, K.L. Differential Requirements by CD4+ and CD8+ T Cells for Soluble and Membrane TNF in Control of Francisella Tularensis Live Vaccine Strain Intramacrophage Growth. J. Immunol. 2007, 179, 7709–7719. [Google Scholar] [CrossRef] [Green Version]
- Kirimanjeswara, G.S.; Olmos, S.; Bakshi, C.S.; Metzger, D.W. Humoral and Cell-Mediated Immunity to the Intracellular Pathogen Francisella Tularensis. Immunol. Rev. 2008, 225, 244–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen, W.P. Immunity against Tularemia: Passive Protection of Mice by Transfer of Immune Tissues. J. Exp. Med. 1962, 115, 411–420. [Google Scholar] [CrossRef]
- Fulop, M.; Mastroeni, P.; Green, M.; Titball, R.W. Role of Antibody to Lipopolysaccharide in Protection against Low- and High-Virulence Strains of Francisella Tularensis. Vaccine 2001, 19, 4465–4472. [Google Scholar] [CrossRef]
- Place, D.E.; Williamson, D.R.; Yuzefpolskiy, Y.; Katkere, B.; Sarkar, S.; Kalia, V.; Kirimanjeswara, G.S. Development of a Novel Francisella Tularensis Live Vaccine Strain Expressing Ovalbumin Provides Insight into Antigen-Specific CD8+ T Cell Responses. PLoS ONE 2017, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twine, S.M.; Petit, M.D.; Shen, H.; Mykytczuk, N.C.S.; Kelly, J.F.; Conlan, J.W. Immunoproteomic Analysis of the Murine Antibody Response to Successful and failed Immunization with Live Anti-Francisella Vaccines. Biochem. Biophys. Res. Commun. 2006, 346, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Elkins, K.L.; Rhinehart-Jones, T.R.; Culkin, S.J.; Yee, D.; Winegar, R.K. Minimal Requirements for Murine Resistance to Infection with Francisella Tularensis LVS. Infect. Immun. 1996, 64, 3288–3293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woolard, M.D.; Hensley, L.L.; Kawula, T.H.; Frelinger, J.A. Respiratory Francisella Tularensis Live Vaccine Strain Infection Induces Th17 Cells and Prostaglandin E2, Which Inhibits Generation of Gamma Interferon-Positive T Cells. Infect. Immun. 2008, 76, 2651–2659. [Google Scholar] [CrossRef] [Green Version]
- Koskela, P.; Herva, E. Cell-Mediated and Humoral Immunity Induced by A Live Francisella Tularensis Vaccine. Infect. Immun. 1982, 36, 983–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffin, A.J.; Crane, D.D.; Wehrly, T.D.; Bosio, C.M. Successful Protection against Tularemia in C57BL/6 Mice Is Correlated with Expansion of Francisella Tularensis-Specific Effector T Cells. Clin. Vaccine Immunol. 2014, 22, 119–128. [Google Scholar] [CrossRef] [Green Version]
- Collazo, C.M.; Meierovics, A.I.; De Pascalis, R.; Wu, T.H.; Lyons, C.R.; Elkins, K.L. T Cells from Lungs and Livers of Francisella Tularensis-Immune Mice Control the Growth of Intracellular Bacteria. Infect. Immun. 2009, 77, 2010–2021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Pascalis, R.; Chou, A.Y.; Bosio, C.M.; Huang, C.-Y.; Follmann, D.A.; Elkins, K.L. Development of Functional and Molecular Correlates of Vaccine-Induced Protection for a Model Intracellular Pathogen, F. tularensis LVS. PLoS Pathog. 2012, 8, e1002494. [Google Scholar] [CrossRef]
- De Pascalis, R.; Mittereder, L.; Chou, A.Y.; Kennett, N.J.; Elkins, K.L. Francisella tularensis Vaccines Elicit Concurrent Protective T- and B-Cell Immune Responses in BALB/cByJ Mice. PLoS ONE 2015, 10, e0126570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, T.H.; Hutt, J.A.; Garrison, K.A.; Berliba, L.S.; Zhou, Y.; Lyons, C.R. Intranasal Vaccination Induces Protective Immunity against Intranasal Infection with Virulent Francisella Tularensis Biovar A. Infect. Immun. 2005, 73, 2644–2654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, N.; Bevan, M.J. CD8+ T Cells: Foot Soldiers of the Immune System. Immunity 2011, 35, 161–168. [Google Scholar] [CrossRef] [Green Version]
- Voskoboinik, I.; Whisstock, J.C.; Trapani, J.A. Perforin and Granzymes: Function, Dysfunction and Human Pathology. Nat. Rev. Immunol. 2015, 15, 388–400. [Google Scholar] [CrossRef]
- Chavezgalan, L.; Arenas-Del Angel, M.C.; Zenteno, E.; Chavez, R.; Lascurain, R. Cell Death Mechanisms Induced by Cytotoxic Lymphocytes. Cell. Mol. Immunol. 2009, 6, 15–25. [Google Scholar] [CrossRef]
- Mittrücker, H.W.; Visekruna, A.; Huber, M. Heterogeneity in the Differentiation and Function of CD8+ T Cells. Arch. Immunol. Ther. Exp. 2014, 62, 449–458. [Google Scholar] [CrossRef]
- Butler, N.S.; Nolz, J.C.; Harty, J.T. Immunologic Considerations for Generating Memory CD8 T Cells through Vaccination. Cell. Microbiol. 2011, 13, 925–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaech, S.M.; Cui, W. Transcriptional Control of Effector and Memory CD8+ T Cell Differentiation. Nat. Rev. Immunol. 2012, 12, 749–761. [Google Scholar] [CrossRef]
- Shane, H.L.; Klonowski, K.D. Every Breath You Take: The Impact of Environment on Resident Memory CD8 T Cells in the Lung. Front. Immunol. 2014, 5, 320. [Google Scholar] [CrossRef] [Green Version]
- Cowley, S.C.; Hamilton, E.; Frelinger, J.A.; Su, J.; Forman, J.; Elkins, K.L. CD4−CD8− T Cells Control Intracellular Bacterial Infections both in Vitro and in Vivo. J. Exp. Med. 2005, 202, 309–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cowley, S.C.; Meierovics, A.I.; Frelinger, J.A.; Iwakura, Y.; Elkins, K.L. Lung CD4−CD8−Double-Negative T Cells Are Prominent Producers of IL-17A and IFN-γ during Primary Respiratory Murine Infection with Francisella Tularensis Live Vaccine Strain. J. Immunol. 2010, 184, 5791–5801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valentino, M.D.; Hensley, L.L.; Skrombolas, D.; McPherson, P.L.; Woolard, M.D.; Kawula, T.H.; Frelinger, J.A.; Frelinger, J.G. Identification of a Dominant CD4 T Cell Epitope in the Membrane Lipoprotein Tul4 from Francisella Tularensis LVS. Mol. Immunol. 2009, 46, 1830–1838. [Google Scholar] [CrossRef] [Green Version]
- Valentino, M.D.; Maben, Z.J.; Hensley, L.L.; Woolard, M.D.; Kawula, T.H.; Frelinger, J.A.; Frelinger, J.G. Identification of T-Cell Epitopes in Francisella Tularensis using an Ordered Protein Array of Serological Targets. Immunology 2011, 132, 348–360. [Google Scholar] [CrossRef]
- Nolz, J.C.; Harty, J.T. Protective Capacity of Memory CD8+ T Cells Is Dictated by Antigen Exposure History and Nature of the Infection. Immunity 2011, 34, 781–793. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.T.; Harty, J.T. Impact of Inflammatory Cytokines on Effector and Memory CD8+ T Cells. Front. Immunol. 2014, 5, 295. [Google Scholar] [CrossRef] [Green Version]
- Verbist, K.C.; Field, M.B.; Klonowski, K.D. Cutting Edge: IL-15–Independent Maintenance of Mucosally Generated Memory CD8 T Cells. J. Immunol. 2011, 186, 6667–6671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, T.; Hu, Y.; Lee, Y.-T.; Bouchard, K.R.; Benechet, A.; Khanna, K.; Cauley, L.S. Lung-Resident Memory CD8 T Cells (T RM) are Indispensable for Optimal Cross-Protection against Pulmonary Virus Infection. J. Leukoc. Biol. 2014, 95, 215–224. [Google Scholar] [CrossRef] [Green Version]
- De Bree, G.J.; Van Leeuwen, E.M.M.; Out, T.A.; Jansen, H.M.; Jonkers, R.E.; Van Lier, R.A.W. Selective Accumulation of Differentiated CD8+ T Cells Specific for Respiratory Viruses in the Human Lung. J. Exp. Med. 2005, 202, 1433–1442. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.S.; Gorski, S.A.; Hahn, S.; Murphy, K.M.; Braciale, T.J. Distinct Dendritic Cell Subsets Dictate the Fate Decision between Effector and Memory CD8+ T Cell Differentiation by a CD24-Dependent Mechanism. Immunity 2014, 40, 400–413. [Google Scholar] [CrossRef] [Green Version]
- Green, M.; Choules, G.; Rogers, D.; Titball, R.W. Efficacy of the Live Attenuated Francisella Tularensis Vaccine (LVS) in a Murine Model of Disease. Vaccine 2005, 23, 2680–2686. [Google Scholar] [CrossRef] [PubMed]
- Lai, R.; Afkhami, S.; Haddadi, S.; Jeyanathan, M.; Xing, Z. Mucosal Immunity and Novel Tuberculosis Vaccine Strategies: Route of Immunisation-Determined T-Cell Homing to Restricted Lung Mucosal Compartments. Eur. Respir. Rev. 2015, 24, 356–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beverley, P.C.L.; Sridhar, S.; Lalvani, A.; Tchilian, E.Z. Harnessing Local and Systemic Immunity for Vaccines against Tuberculosis. Mucosal Immunol. 2013, 7, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, N.; Kanekiyo, M.; Hagiwara, Y.; Okamura, T.; Someya, K.; Matsuo, K.; Ami, Y.; Sato, S.; Yamamoto, N.; Honda, M. Intradermal Delivery of Recombinant Vaccinia Virus Vector DIs Induces Gut-Mucosal Immunity. Scand. J. Immunol. 2010, 72, 98–105. [Google Scholar] [CrossRef]
- Manam, S.; Chaganty, B.K.R.; Evani, S.J.; Zafiratos, M.T.; Ramasubramanian, A.K.; Arulanandam, B.P.; Murthy, A.K. Intranasal Vaccination with Chlamydia Pneumoniae Induces Cross-Species Immunity against Genital Chlamydia Muridarum Challenge in Mice. PLoS ONE 2013, 8, e64917. [Google Scholar] [CrossRef]
- Neutra, M.R.; Kozlowski, P.A. Mucosal Vaccines: The Promise and the Challenge. Nat. Rev. Immunol. 2006, 6, 148–158. [Google Scholar] [CrossRef]
- Hu, K.; Luo, S.; Tong, L.; Huang, X.; Jin, W.; Huang, W.; Du, T.; Yan, Y.; He, S.; Griffin, G.E.; et al. CCL19 and CCL28 Augment Mucosal and Systemic Immune Responses to HIV-1 gp140 by Mobilizing Responsive Immunocytes into Secondary Lymph Nodes and Mucosal Tissue. J. Immunol. 2013, 191, 1935–1947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicol, M.J.; Williamson, D.R.; Place, D.E.; Kirimanjeswara, G.S. Differential Immune Response Following Intranasal and Intradermal Infection with Francisella tularensis: Implications for Vaccine Development. Microorganisms 2021, 9, 973. https://doi.org/10.3390/microorganisms9050973
Nicol MJ, Williamson DR, Place DE, Kirimanjeswara GS. Differential Immune Response Following Intranasal and Intradermal Infection with Francisella tularensis: Implications for Vaccine Development. Microorganisms. 2021; 9(5):973. https://doi.org/10.3390/microorganisms9050973
Chicago/Turabian StyleNicol, McKayla J., David R. Williamson, David E. Place, and Girish S. Kirimanjeswara. 2021. "Differential Immune Response Following Intranasal and Intradermal Infection with Francisella tularensis: Implications for Vaccine Development" Microorganisms 9, no. 5: 973. https://doi.org/10.3390/microorganisms9050973
APA StyleNicol, M. J., Williamson, D. R., Place, D. E., & Kirimanjeswara, G. S. (2021). Differential Immune Response Following Intranasal and Intradermal Infection with Francisella tularensis: Implications for Vaccine Development. Microorganisms, 9(5), 973. https://doi.org/10.3390/microorganisms9050973






