Use of Spinal Anaesthesia with Anaesthetic Block of Intercostal Nerves Compared to a Continuous Infusion of Sufentanyl to Improve Analgesia in Cats Undergoing Unilateral Mastectomy
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Pre-Surgery Procedure
2.2. Spinal Anaesthesia with an Anaesthetic Block of Intercostal Nerves
2.3. Surgical Procedure
2.4. Post-Surgery Pain Evaluation
2.5. Ethics
2.6. Data Analysis
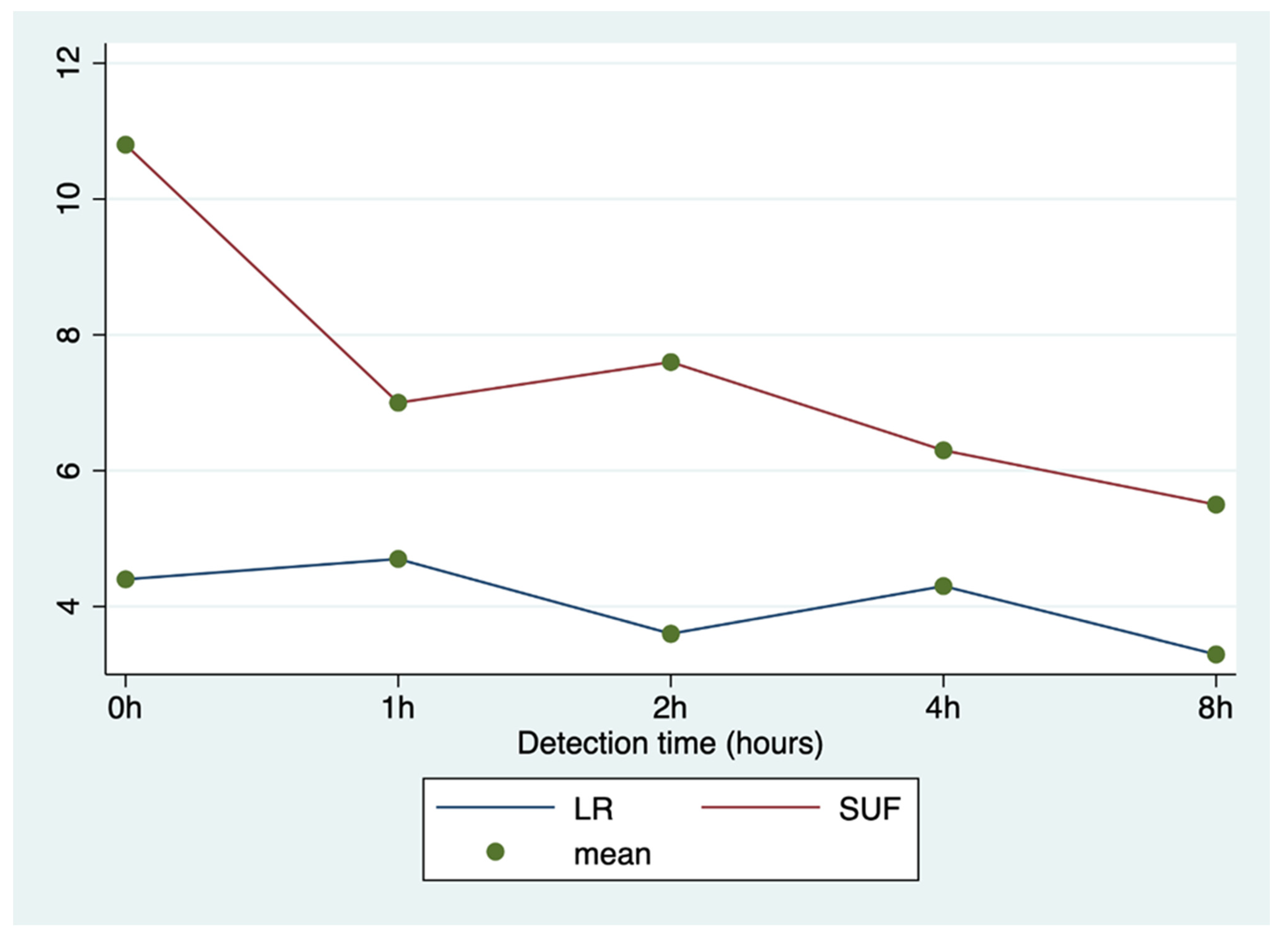
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yilmaz, Ö.T.; Toydemir, T.S.; Kirşan, İ.; Dokuzeylul, B.; Gunay, Z. Effects of surgical wound infiltration with bupivacaine on postoperative analgesia in cats undergoing bilateral mastectomy. J. Vet. Med. Sci. 2014, 76, 1595–1601. [Google Scholar] [CrossRef]
- Cassali, G.; De Campos, C.; Bertagnolli, A.; Estrela-Lima, A.; Lavalle, G.; Damasceno, K.; De Nardi, A.; Cogliati, B.; Da Costa, F.; Sobral, R.; et al. Consensus for the diagnosis, prognosis and treatment of feline mammary tumors. Braz. J. Vet. Res. Anim. Sci. 2018, 55, 1–17. [Google Scholar] [CrossRef]
- McKelvey, D.; Hollingshead, K.W. Analgesia. In Veterinary Anesthesia and Analgesia; McKelvey, D., Hollingshead, K.W., Eds.; Mosby: St Louis, MI, USA, 2000; pp. 315–346. [Google Scholar]
- Hansen, B.D. Analgesia and sedation in the critically ill. J. Vet. Emerg. Crit. Care 2005, 15, 285–294. [Google Scholar] [CrossRef]
- Clarissa, M.R.; Moreira, R.L.S.; Oliveira, G.A.; Costa, K.B.; Corgozinho, S.P.L.; Luna, H.J.M. Souza Evaluation of tumescent local anesthesia in cats undergoing unilateral mastectomy. Vet. Anaest. Analg. 2021, 48, 134–141. [Google Scholar]
- Otero, P.E.; Campoy, L. Epidural and spinal anesthesia. In Small Animals and Regional Anesthesia and Analgesia; Campoy, L., Read, M., Eds.; Wiley-Blackwell: New York NY, USA, 2013; pp. 227–231. [Google Scholar]
- Sarotti, D.; Cattai, A.; Franci, P. Combined spinal and general anaesthesia in 58 cats undergoing various surgical procedures: Description of technique and retrospective perioperative evaluation. J. Feline Med. Surg. 2018, 21, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Beilin, Y.; Guinn, N.; Bernstein, H.; Zahn, J.; Hossain, S.; Bodian, C. Local anesthetics and mode of delivery: Bupivacaine versus ropivacaine versus levobupivacaine. Anesth. Analg. 2007, 105, 756–763. [Google Scholar] [CrossRef]
- Torske, K.E.; Dyson, D.H. Epidural analgesia and anesthesia. Vet. Clin. N. Am. Small Anim. Pr. 2000, 30, 859–874. [Google Scholar] [CrossRef]
- Brondani, J.T.; Luna, S.P.L.; Minto, B.W.; Santos, B.P.R.; Beier, S.L.; Matsubara, L.M.; Padovani, C.R. Validity and responsiveness of a multidimensional composite scale to assess postoperative pain in cats. Arq. Bras. Med. Vet. Zootec. 2012, 64, 1529–1538. [Google Scholar] [CrossRef]
- Owen, L.N. TNM Classification of Tumors in Domestic Animals; WHO: Geneva, Switzerland; Available online: apps.who.int/iris/bitstream/10665/68618/1/VPH_CMO_80.20_eng.pdf (accessed on 22 January 2014).
- Langley-Hobbs, S.L.; Demetriou, J.L.; Ladlow, J.F. Mammary Glands. In Feline Soft Tissue and General Surgery; Saunders Elsevier Ltd: London, UK, 2014; Chapter 21; pp. 219–232. [Google Scholar]
- Brondani, J.; Mama, K.R.; Luna, S.P.L.; Wright, B.D.; Niyom, S.; Ambrosio, J.; Vogel, P.R.; Padovani, C.R. Validation of the English version of the UNESP-Botucatu multidimensional composite pain scale for assessing postoperative pain in cats. BMC Vet. Res. 2013, 9, 143. [Google Scholar] [CrossRef] [PubMed]
- Egger, C.M.; Glerum, L.E.; Allen, S.W.; Haag, B. Plasma fentanyl concentrations in awake cats and cats undergoing anesthesia and ovariohysterectomy using transdermal administration. Vet. Anaesth. Analg. 2003, 30, 229–236. [Google Scholar] [CrossRef]
- Della, R.G.; Catanzaro, A.; Conti, M.B.; Bufalari, A.; De Monte, V.; Di Salvo, A.; Tabarelli, B.J.; Pacca, S.; Luna, L. Validation of the Italian version of the UNESP-Botucatu multidimensional composite pain scale for the assessment of postoperative pain in cats. Vet. Ital. 2018, 54, 49–61. [Google Scholar]
- Robertson, S.A. Taylor PM Pain management in cats—Past, present and future. Part 2. Treatment of pain—clinical pharmacology. J. Feline Med. Surg. 2004, 6, 321–333. [Google Scholar] [CrossRef]
- Grubb, T.; Sager, J.; Gaynor, J.S.; Montgomery, E.; Parkerm, J.A.; Shafford, H.; Tearney, C. AAHA Anesthesia and Monitoring Guidelines for Dogs and Cats. J. Am. Anim Hosp. Assoc. 2020, 56, 59–82. [Google Scholar] [CrossRef]
- Robertson, S.A. Managing pain in feline patients. Vet. Clin. N. Am. Small Anim. Pract. 2008, 38, 1267–1290. [Google Scholar] [CrossRef] [PubMed]
- Thurmon, J.C.; Tranquilli, W.J.; Benson, G.J. Perioperative Pain and Its Management. In Essentials of Small Animal Anesthesia and Analgesia; Thurmon, J.C., Tranquilli, W.J., Benson, G.J., Eds.; Lippincott Williams&Wilkins: Philadelphia, PA, USA, 1996; pp. 28–59. [Google Scholar]
- Grubb, T.; Lobprise, H. Local and regional anaesthesia in dogs and cats: Overview of concepts and drugs (Part 1). Vet. Med. Sci. 2000, 6, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Grubb, T.; Lobprise, H. Local and regional anaesthesia in dogs and cats: Descriptions of specific local and regional techniques (Part 2). Vet. Med. Sci. 2000, 2020, 2218–2234. [Google Scholar] [CrossRef]
- Campagnol, D.; Teixeira-Neto, F.J.; Monteiro, E.R.; Restitutti, F.; Minto, B.W. Effect of intraperitoneal or incisional bupivacaine on pain and the analgesic requirement after ovariohysterectomy in dogs. Vet. Anaesth. Analg. 2012, 39, 426–430. [Google Scholar] [CrossRef]
- Mwangi, W.E.; Mogoa, E.M.; Mwangi, J.N.; Mbuthia, P.G.; Mbugua, S.W. A systematic review of analgesia practices in dogs undergoing ovariohysterectomy. Vet. World 2018, 11, 1725–1735. [Google Scholar] [CrossRef]
- Tranquilli, W.; Grimm, K.; Lamont, L. Pain Management, 2nd ed.; Tranquilli, W., Grimm, K., Lamont, L., Jackson, W.Y., Eds.; Teton New Media: Jackson, WY, USA, 2004; pp. 30–38. [Google Scholar]
- Smith, L. Balanced anesthetic techniques. Navta. J. Spring 2006, 14, 36–39. [Google Scholar]
- Pavlidou, K.; Papazoglou, L.; Savvas, I.; Kazakos, G. Analgesia for small animal thoracic surgery. Compend. Contin. Educ. Vet. 2009, 31, 432–436. [Google Scholar] [PubMed]
- Matteson, V. Block that pain—Local anesthesia in dogs and cats. Vet. Tech. 2000, 21, 332–339. [Google Scholar]
- Hellyer, P.; Rodan, I.; Brunt, J.; Downing, R.; Hagedorn, J.E.; Robertson, S.A. AAHA/AAFP Pain Management Guidelines Task Force Members. AAHA/AAFP pain management guidelines for dogs and cats. J. Feline Med. Surg. 2007, 9, 466–480. [Google Scholar] [CrossRef] [PubMed]
- Waterman-Pearson AE Analgesia. In BSAVA Manual of Small Animal Anesthesia and Analgesia; Seymour, C., Gleed, R., Eds.; British Small Animal Veterinary Association: Gloucester, UK, 2016; pp. 59–71. [Google Scholar]
- Epstein, M.E. Postsurgical assessment of pain in dogs and cats. In Proceedings of the 82nd Annual Westerns Veterinary Conference, Las Vegas, NV, USA, 14–18 February 2010. [Google Scholar]
- Grimm, K.A. Pain Management for Small Animals. In Veterinary Anesthesia and Pain Management Secrets; Greene, S.A., Ed.; Hanley& Belfus: Philadelphia, PA, USA, 2002; pp. 327–329. [Google Scholar]
- Lambertini, C.; Kluge, K.; Lanza-Perea, M.; Bruhl-Day, R.; Kalchofner Guerrero, K.S. Comparison of intraperitoneal ropivacaine and bupivacaine for postoperative analgesia in dogs undergoing ovariohysterectomy. Vet. Anaesth. Analg. 2018, 45, 865–870. [Google Scholar] [CrossRef] [PubMed]
| Variable | Group | Total (n = 20) | p-Value | |
|---|---|---|---|---|
| LR (n = 10) | SUF (n = 10) | |||
| Age (years) | 13.0 ± 1.2 (11–15) | 14.2 ± 2.0 (11–16) | 13.6 ± 1.7 (11–16) | 0.118 |
| Weight (kg) | 3.3 ± 0.5 (2–4) | 3.1 ± 0.6 (2–4) | 3.2 ± 0.5 (2–4) | 0.341 |
| Variable | LR (n = 10) | SUF (n = 10) | Total (n = 20) | p-Value |
|---|---|---|---|---|
| Drug administration, n (%) | 4 (40.0) | 10 (100.0) | 14 (70.0) | 0.011 |
| Number of doses, n (%) | 0.505 | |||
| 1 | 4/4 (100.0) | 7/10 (70.0) | 11/14 (78.6) | |
| 2 | 0/4 (0.0) | 3/10 (30.0) | 3/14 (21.4) | |
| Administration dose 1, n (%) | 0.203 | |||
| 0 | 1/4 (25.0) | 7/10 (70.0) | 8/14 (57.1) | |
| 1 | 2/4 (50.0) | 2/10 (20.0) | 4/14 (28.6) | |
| 2 | 0/4 (0.0) | 1/10 (10.0) | 1/14 (7.1) | |
| 4 | 1/4 (25.0) | 0/10 (0.0) | 1/14 (7.1) | |
| Administration dose 2, n (%) | - | |||
| 2 | - | 2/3 (66.7) | 2/3 (66.7) | |
| 4 | - | 1/3 (33.3) | 1/3 (33.3) |
| Determinant | aOR | 95% CI | p-Value |
|---|---|---|---|
| Weight | 3.3 | 0.2–54.0 | 0.400 |
| Age | 0.2 | 0.1–0.9 | 0.043 |
| Group (SUF vs. LR) | 34.3 | 0.5–2340.9 | 0.100 |
| Determinant | aOR | 95% CI | p-Value |
|---|---|---|---|
| Weight | 6.2 | 0.4–106.5 | 0.212 |
| Age | 1.1 | 0.3–3.8 | 0.830 |
| Group (SUF vs. LR) * | 1 | - | 0.100 |
| Determinant | Correlation Coefficient | 95% CI | p-Value |
|---|---|---|---|
| Weight | 1.6 | −1.5 to 4.6 | 0.293 |
| Age | −0.4 | −1.4 to 0.6 | 0.435 |
| Group (SUF vs. LR) | −3.4 | −6.9 to 0.2 | 0.061 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cicirelli, V.; Debidda, P.; Maggio, N.; Caira, M.; Mrenoshki, D.; Aiudi, G.G.; Lacalandra, G.M. Use of Spinal Anaesthesia with Anaesthetic Block of Intercostal Nerves Compared to a Continuous Infusion of Sufentanyl to Improve Analgesia in Cats Undergoing Unilateral Mastectomy. Animals 2021, 11, 887. https://doi.org/10.3390/ani11030887
Cicirelli V, Debidda P, Maggio N, Caira M, Mrenoshki D, Aiudi GG, Lacalandra GM. Use of Spinal Anaesthesia with Anaesthetic Block of Intercostal Nerves Compared to a Continuous Infusion of Sufentanyl to Improve Analgesia in Cats Undergoing Unilateral Mastectomy. Animals. 2021; 11(3):887. https://doi.org/10.3390/ani11030887
Chicago/Turabian StyleCicirelli, Vincenzo, Pasquale Debidda, Nicola Maggio, Michele Caira, Daniela Mrenoshki, Giulio G. Aiudi, and Giovanni M. Lacalandra. 2021. "Use of Spinal Anaesthesia with Anaesthetic Block of Intercostal Nerves Compared to a Continuous Infusion of Sufentanyl to Improve Analgesia in Cats Undergoing Unilateral Mastectomy" Animals 11, no. 3: 887. https://doi.org/10.3390/ani11030887
APA StyleCicirelli, V., Debidda, P., Maggio, N., Caira, M., Mrenoshki, D., Aiudi, G. G., & Lacalandra, G. M. (2021). Use of Spinal Anaesthesia with Anaesthetic Block of Intercostal Nerves Compared to a Continuous Infusion of Sufentanyl to Improve Analgesia in Cats Undergoing Unilateral Mastectomy. Animals, 11(3), 887. https://doi.org/10.3390/ani11030887







