Lactobacillus plantarum and Lactobacillus reuteri as Functional Feed Additives to Prevent Diarrhoea in Weaned Piglets
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Species-Specific PCR
2.2. Minimal Inhibitory Concentration (MIC)
2.3. Gastric Acid and Simulated In Vitro Digestion Resistance
2.4. Small-Scale Fermentation and Freeze-Drying Resistance
2.5. Bacterial Fermentation for Experimental Trial Batch Production
2.6. Experimental Design, Animal Housing and Dietary Treatments
2.7. Animal Performance, Diarrhoea Occurrence and Biological Sample Collection
2.8. Microbiological and pH Evaluation of Faecal Samples
2.9. Serum Metabolites
2.10. Statistical Analysis
3. Results
3.1. Species-Specific PCR
3.2. Minimal Inhibitory Concentrations
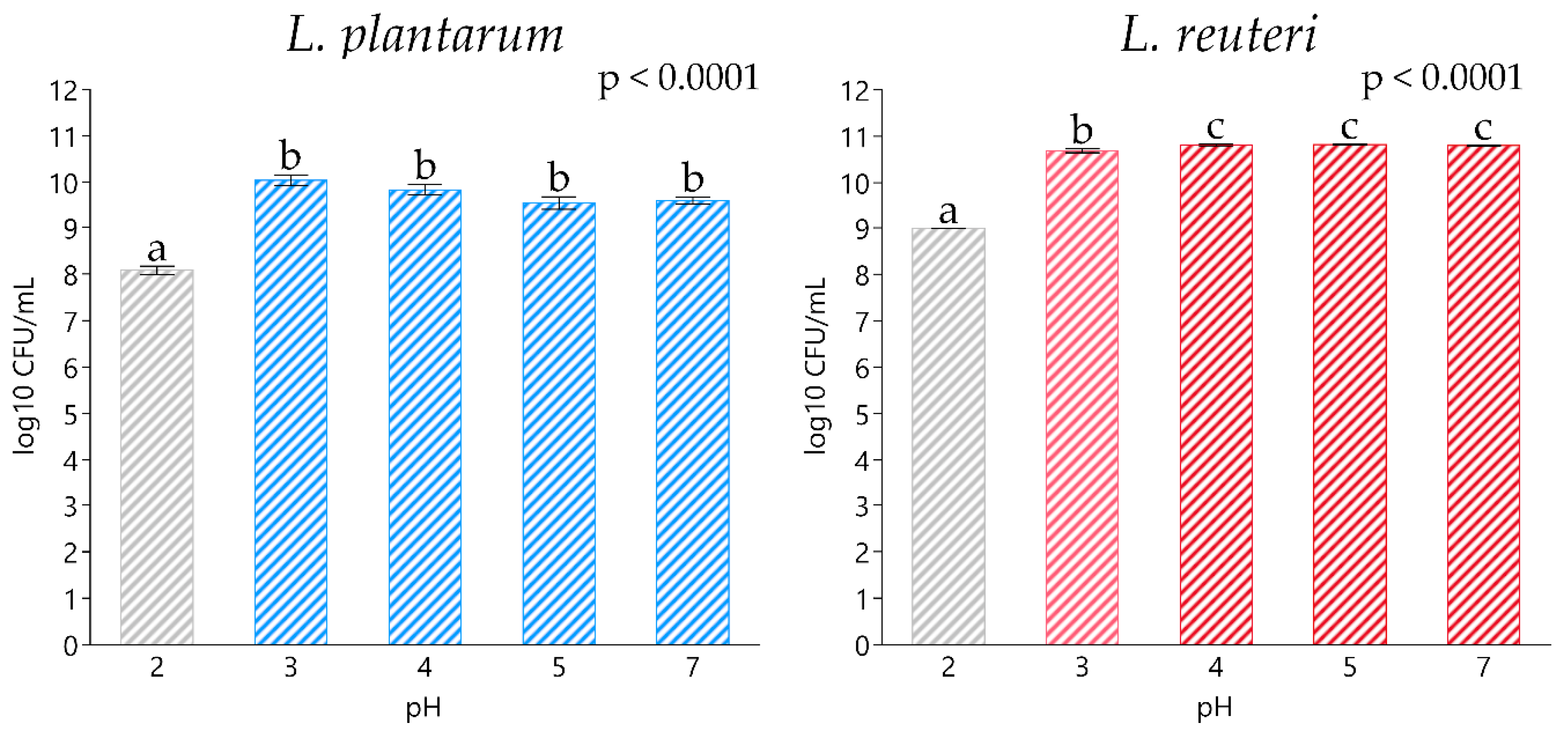
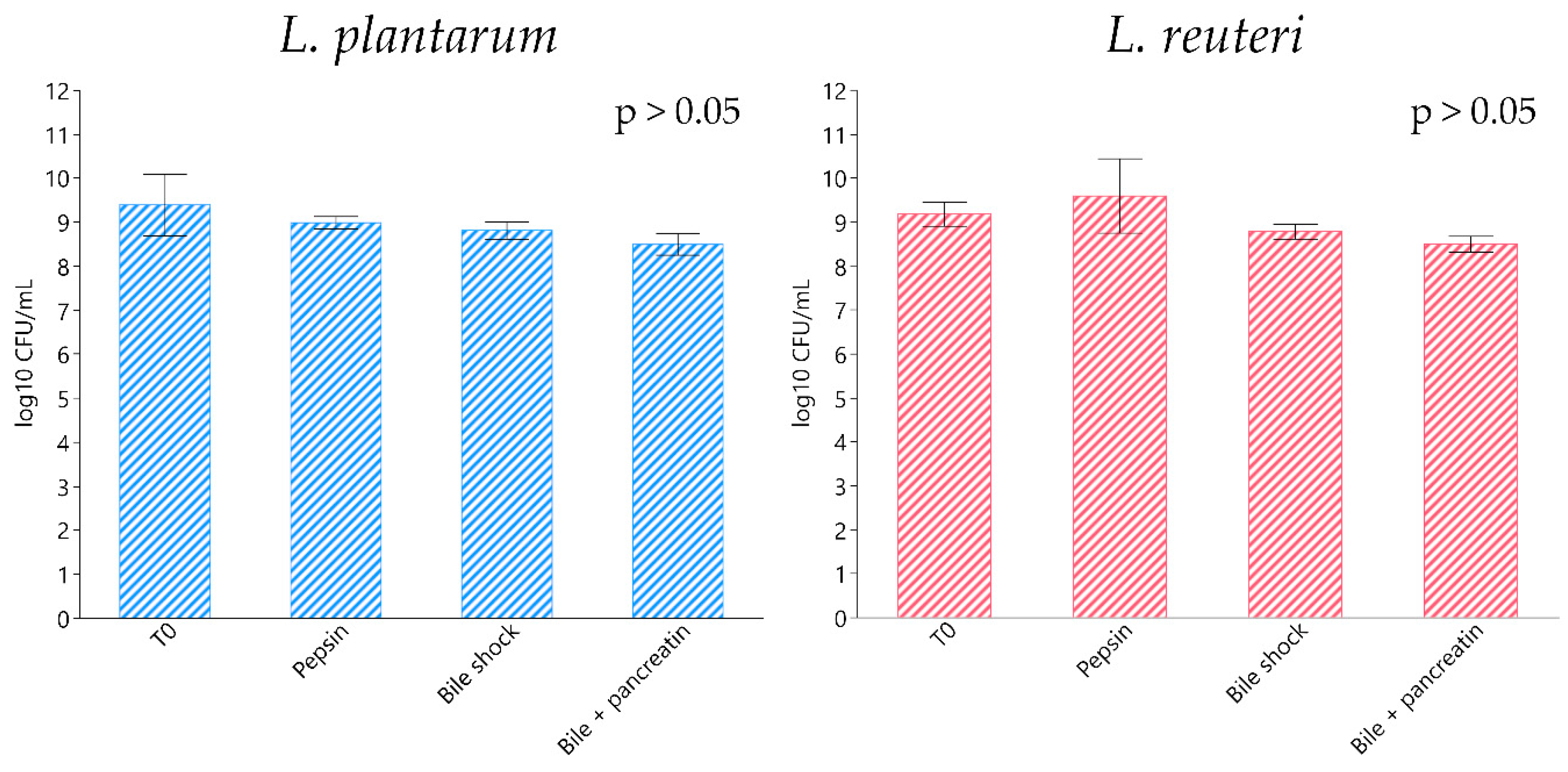
3.3. Acid and Simulated In Vitro Digestion Resistance
3.4. Small-Scale Fermentation and Freeze-Drying Resistance
3.5. Bacterial Fermentation for Experimental Trial Batch Production
3.6. Evaluation of Experimental Diets
3.7. Zootechnical Performance
3.8. Diarrhoea Occurrence
3.9. Microbiological Analysis and Faecal pH
3.10. Serum Metabolism
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arsène, M.M.; Davares, A.K.; Andreevna, S.L.; Vladimirovich, E.A.; Carime, B.Z.; Marouf, R.; Khelifi, I. The use of probiotics in animal feeding for safe production and as potential alternatives to antibiotics. Vet. World 2021, 14, 319. [Google Scholar] [CrossRef]
- Ng, W.J.; Shit, C.-S.; Ee, K.Y.; Chai, T.T. Plant Natural Products for Mitigation of Antibiotic Resistance. In Sustainable Agriculture Reviews 49; Springer: Berlin/Heidelberg, Germany, 2021; pp. 57–91. [Google Scholar]
- Tang, K.L.; Caffrey, N.P.; Nóbrega, D.B.; Cork, S.C.; Ronksley, P.E.; Barkema, H.W.; Polachek, A.J.; Ganshorn, H.; Sharma, N.; Kellner, J.D. Restricting the use of antibiotics in food-producing animals and its associations with antibiotic resistance in food-producing animals and human beings: A systematic review and meta-analysis. Lancet Planet. Health 2017, 1, e316–e327. [Google Scholar] [CrossRef]
- Cormican, M.; Hopkins, S.; Jarlier, V.; Reilly, J.; Simonsen, G.; Strauss, R.; Vandenberg, O.; Zabicka, D.; Zarb, P.; Catchpole, M.; et al. ECDC, EFSA and EMA Joint Scientific Opinion on a list of outcome indicators as regards surveillance of antimicrobial resistance and antimicrobial consumption in humans and food-producing animals. EFSA J. 2017, 15. [Google Scholar] [CrossRef]
- European Medicines Agency. EMA/394961/2017. European Medicines Agency, Questions and Answers on Veterinary Medicinal Products Containing Zinc Oxide to be Administered Orally to Food-Producing Species Outcome of a Referral Procedure under Article 35 of Directive 2001/82/EC (EMEA/V/A/118); EMA: London, UK, 2017.
- Hejna, M.; Onelli, E.; Moscatelli, A.; Bellotto, M.; Cristiani, C.; Stroppa, N.; Rossi, L. Heavy-Metal Phytoremediation from Livestock Wastewater and Exploitation of Exhausted Biomass. Int. J. Environ. Res. Public Health 2021, 18, 2239. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, A.; Tugnoli, B.; Piva, A.; Grilli, E. Towards Zero Zinc Oxide: Feeding Strategies to Manage Post-Weaning Diarrhea in Piglets. Animals 2021, 11, 642. [Google Scholar] [CrossRef] [PubMed]
- EU Commission. Regulation EC 1831/2003. of the European Parliament and of the Council, of 22 September 2003 on Additives for Use in Animal Nutrition (Text with EEA Relevance); EU Commission: Brussels, Belgium, 2003. [Google Scholar]
- Hejna, M.; Gottardo, D.; Baldi, A.; Dell’Orto, V.; Cheli, F.; Zaninelli, M.; Rossi, L. Nutritional ecology of heavy metals. Animal 2018, 12, 2156–2170. [Google Scholar] [CrossRef] [Green Version]
- Hejna, M.; Moscatelli, A.; Onelli, E.; Baldi, A.; Pilu, S.; Rossi, L. Evaluation of concentration of heavy metals in animal rearing system. Ital. J. Anim. Sci. 2019, 18, 1372–1384. [Google Scholar] [CrossRef] [Green Version]
- Hejna, M.; Moscatelli, A.; Stroppa, N.; Onelli, E.; Pilu, S.; Baldi, A.; Rossi, L. Bioaccumulation of heavy metals from wastewater through a Typha latifolia and Thelypteris palustris phytoremediation system. Chemosphere 2020, 241. [Google Scholar] [CrossRef]
- Rossi, L.; Dell′Orto, V.; Vagni, S.; Sala, V.; Reggi, S.; Baldi, A. Protective effect of oral administration of transgenic tobacco seeds against verocytotoxic Escherichia coli strain in piglets. Vet. Res. Commun. 2014, 38, 39–49. [Google Scholar] [CrossRef]
- Lu, C.W.; Wang, S.E.; Wu, W.J.; Su, L.Y.; Wang, C.H.; Wang, P.H.; Wu, C.H. Alternative antibiotic feed additives alleviate pneumonia with inhibiting ACE-2 expression in the respiratory system of piglets. Food Sci. Nutr. 2021, 9, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- Chelakkot, C.; Ghim, J.; Ryu, S.H. Mechanisms regulating intestinal barrier integrity and its pathological implications. Exp. Mol. Med. 2018, 50, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Sarkar, A.; Yoo, J.Y.; Valeria Ozorio Dutra, S.; Morgan, K.H.; Groer, M. The association between early-life gut microbiota and long-term health and diseases. J. Clin. Med. 2021, 10, 459. [Google Scholar] [CrossRef]
- Domínguez Díaz, L.; Fernández-Ruiz, V.; Cámara, M. The frontier between nutrition and pharma: The international regulatory framework of functional foods, food supplements and nutraceuticals. Crit. Rev. Food Sci. Nutr. 2020, 60, 1738–1746. [Google Scholar] [CrossRef]
- Lallès, J.P.; Montoya, C.A. Dietary alternatives to in-feed antibiotics, gut barrier function and inflammation in piglets post-weaning: Where are we now? Anim. Feed Sci. Technol. 2021, 114836. [Google Scholar] [CrossRef]
- Tomičić, Z.; Čabarkapa, I.; Čolović, R.; Đuragić, O.; Tomičić, R. Salmonella in the feed industry: Problems and potential solutions. J. Agron. 2018, 22, 2019. [Google Scholar]
- Hori, T.; Matsuda, K.; Oishi, K. Probiotics: A Dietary Factor to Modulate the Gut Microbiome, Host Immune System, and Gut–Brain Interaction. Microorganisms 2020, 8, 1401. [Google Scholar] [CrossRef]
- Guevarra, R.B.; Lee, J.H.; Lee, S.H.; Seok, M.J.; Kim, D.W.; Kang, B.N.; Johnson, T.J.; Isaacson, R.E.; Kim, H.B. Piglet gut microbial shifts early in life: Causes and effects. J. Anim. Sci. Biotechnol. 2019, 10, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, F.; Wang, A.; Zeng, X.; Hou, C.; Liu, H.; Qiao, S. Lactobacillus reuteri I5007 modulates tight junction protein expression in IPEC-J2 cells with LPS stimulation and in newborn piglets under normal conditions. BMC Microbiol. 2015, 15, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Śliżewska, K.; Chlebicz-Wójcik, A.; Nowak, A. Probiotic Properties of New Lactobacillus Strains Intended to Be Used as Feed Additives for Monogastric Animals. Probiotics Antimicrob. Proteins 2021, 13, 146–162. [Google Scholar] [CrossRef]
- Lee, C.S.; Kim, S.H. Anti-inflammatory and anti-osteoporotic potential of lactobacillus plantarum A41 and L. fermentum SRK414 as probiotics. Probiotics Antimicrob. Proteins 2020, 12, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Liu, Y.; Ma, F.; Sun, M.; Song, Y.; Xu, D.; Mu, G.; Tuo, Y. Lactobacillus plantarum Y44 alleviates oxidative stress by regulating gut microbiota and colonic barrier function in Balb/C mice with subcutaneous D-galactose injection. Food Funct. 2021, 12, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Jiang, Z.; Zheng, C.; Wang, L.; Yang, X. Effect of Lactobacillus plantarum on diarrhea and intestinal barrier function of young piglets challenged with enterotoxigenic Escherichia coli K88. J. Anim. Sci. 2014, 92, 1496–1503. [Google Scholar] [CrossRef] [Green Version]
- EU Commission. Regulation EU 451/2012. COMMISSION IMPLEMENTING REGULATION (EU) No 451/2012 on the Withdrawal from the Market of Certain Feed Additives Belonging to the Functional Group of Silage Additives (Text with EEA Relevance); EU Commission: Brussels, Belgium, 2012. [Google Scholar]
- EFSA BIOHAZ Panel; Koutsoumanis, K.; Allende, A.; Alvarez-Ordonez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; Davies, R.; De Cesare, A.; Hilbert, F.; et al. The list of QPS status recommended biological agents for safety risk assessments carried out by EFSA. EFSA J. 2021. [Google Scholar] [CrossRef]
- Chen, X.Y.; Woodward, A.; Zijlstra, R.T.; Gänzle, M.G. Exopolysaccharides synthesized by Lactobacillus reuteri protect against enterotoxigenic Escherichia coli in piglets. Appl. Environ. Microbiol. 2014, 80, 5752–5760. [Google Scholar] [CrossRef] [Green Version]
- Hou, C.; Zeng, X.; Yang, F.; Liu, H.; Qiao, S. Study and use of the probiotic Lactobacillus reuteri in pigs: A review. J. Anim. Sci. Biotechnol. 2015, 6, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghini, V.; Tenori, L.; Pane, M.; Amoruso, A.; Marroncini, G.; Squarzanti, D.; Azzimonti, B.; Rolla, R.; Savoia, P.; Tarocchi, M.; et al. Effects of Probiotics Administration on Human Metabolic Phenotype. Metabolites 2020, 10, 396. [Google Scholar] [CrossRef] [PubMed]
- Khare, A.; Gaur, S. Cholesterol-Lowering Effects of Lactobacillus Species. Curr. Microbiol. 2020, 77, 638–644. [Google Scholar] [CrossRef]
- Fang, T.; Guo, J.; Lin, M.; Lee, M.; Chen, Y.; Lin, W. Protective effects of Lactobacillus plantarum against chronic alcohol-induced liver injury in the murine model. Appl. Microbiol. Biotechnol. 2019, 103, 8597–8608. [Google Scholar] [CrossRef] [PubMed]
- Chapman, C.; Gibson, G.; Rowland, I. In vitro evaluation of single- and multi-strain probiotics: Inter-species inhibition between probiotic strains, and inhibition of pathogens. Anaerobe 2012, 18, 405–413. [Google Scholar] [CrossRef]
- Torriani, S.; Felis, G.E.; Dellaglio, F. Differentiation of Lactobacillus plantarum, L. pentosus, and L. paraplantarum by recA gene sequence analysis and multiplex PCR assay with recA gene-derived primers. Appl. Environ. Microbiol. 2001, 67, 3450–3454. [Google Scholar] [CrossRef] [Green Version]
- Song, Y.L.; Kato, N.; Liu, C.X.; Matsumiya, Y.; Kato, H.; Watanabe, K. Rapid identification of 11 human intestinal Lactobacillus species by multiplex PCR assays using group-and species-specific primers derived from the 16S–23S rRNA intergenic spacer region and its flanking 23S rRNA. FEMS Microbiol. Lett. 2000, 187, 167–173. [Google Scholar] [CrossRef]
- Warke, R.; Kamat, A.; Kamat, M.; Thomas, P. Incidence of pathogenic psychrotrophs in ice creams sold in some retail outlets in Mumbai, India. Food Control 2000, 11, 77–83. [Google Scholar] [CrossRef]
- Charteris, W.; Kelly, P.; Morelli, L.; Collins, J. Development and application of an in vitro methodology to determine the transit tolerance of potentially probiotic Lactobacillus and Bifidobacterium species in the upper human gastrointestinal tract. J. Appl. Microbiol. 1998, 84, 759–768. [Google Scholar] [CrossRef]
- Jensen, H.; Grimmer, S.; Naterstad, K.; Axelsson, L. In vitro testing of commercial and potential probiotic lactic acid bacteria. Int. J. Food Microbiol. 2012, 153, 216–222. [Google Scholar] [CrossRef]
- Commission Directive EU 6/2010 amending Annex I to Directive 2002/32/EC of the European Parliament and of the Council as regards mercury, free gossypol, nitrites and Mowrah, Bassia, Madhuca (Text with EEA relevance). Off. J. Eur. Uni. 2002, 140, 1–10.
- NRC. Nutrient Requirements of Swine, 7th ed.; National Research Council: Washington, DC, USA; The National Academies Press: Washington, DC, USA, 2012. [Google Scholar]
- AOAC. Official Methods of Analysis, 21st ed.; Association of Official Analytical Chemists: Washington, DC, USA, 2019. [Google Scholar]
- Christie, W.W.; Han, X. Lipid Analysis, Isolation, Separation, Identification and Lipidomic Analysis. Oily Press Lipid Libr. Ser. 2012, 181–211. [Google Scholar] [CrossRef]
- Shewale, R.N.; Sawale, P.D.; Khedkar, C.; Singh, A. Selection criteria for probiotics: A review. Int. J. Probiotics Prebiotics 2014, 9, 17. [Google Scholar]
- Yun, J.H.; Lee, K.B.; Sung, Y.K.; Kim, E.B.; Lee, H.G.; Choi, Y.J. Isolation and characterization of potential probiotic lactobacilli from pig feces. J. Basic Microbiol. 2009, 49, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Lukacova, D.; Karovicova, J.; Greifova, M.; Greif, G.; Sovcikova, A.; Kohajdova, Z. In vitro testing of selected probiotic characteristics of Lactobacillus plantarum and Bifidobacterium longum. J. Food Nutr. Res. 2006, 45, 77–83. [Google Scholar]
- Singh, T.; Kaur, G.; Malik, R.; Schillinger, U.; Guigas, C.; Kapila, S. Characterization of Intestinal Lactobacillus reuteri Strains as Potential Probiotics. Probiotics Antimicrob. Proteins 2012, 4, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Vamanu, E. Effect of gastric and small intestinal digestion on lactic acid bacteria activity in a GIS1 simulator. Saudi J. Biol. Sci. 2017, 24, 1453–1457. [Google Scholar] [CrossRef] [Green Version]
- Bove, P.; Russo, P.; Capozzi, V.; Gallone, A.; Spano, G.; Fiocco, D. Lactobacillus plantarum passage through an oro-gastro-intestinal tract simulator: Carrier matrix effect and transcriptional analysis of genes associated to stress and probiosis. Microbiol. Res. 2013, 168, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Suo, C.; Yin, Y.; Wang, X.; Lou, X.; Song, D.; Wang, X.; Gu, Q. Effects of Lactobacillus plantarum ZJ316 on pig growth and pork quality. BMC Vet. Res. 2012, 8, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betancur, C.; Martínez, Y.; Merino-Guzman, R.; Hernandez-Velasco, X.; Castillo, R.; Rodríguez, R.; Tellez-Isaias, G. Evaluation of oral administration of Lactobacillus plantarum CAM6 strain as an alternative to antibiotics in weaned pigs. Animals 2020, 10, 1218. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wu, H.; Lu, L.; Jiang, L.; Yu, Q. Lactobacillus reuteri promotes intestinal development and regulates mucosal immune function in newborn piglets. Front. Vet. Sci. 2020, 7, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Yang, L.; Tang, X.; Cai, L.; Liu, G.; Kong, X.; Blachier, F.; Yin, Y. Dietary supplementation with high-dose Bacillus subtilis or Lactobacillus reuteri modulates cellular and humoral immunities and improves performance in weaned piglets. J. Food Agric. Environ. 2011, 9, 181–187. [Google Scholar]
- EFSA; Rychen, G.; Aquilina, G.; Azimonti, G.; Bampidis, V.; Bastos, M.d.L.; Bories, G.; Chesson, A.; Cocconcelli, P.S.; Flachowsky, G. EFSA Panel on Additives and Products or Substances used in Animal Feed: Guidance on the assessment of the efficacy of feed additives. EFSA J. 2018, 16, e05274. [Google Scholar]
- Wu, Y.; Zhu, C.; Chen, Z.; Chen, Z.; Zhang, W.; Ma, X.; Wang, L.; Yang, X.; Jiang, Z. Protective effects of Lactobacillus plantarum on epithelial barrier disruption caused by enterotoxigenic Escherichia coli in intestinal porcine epithelial cells. Vet. Immunol. Immunopathol. 2016, 172, 55–63. [Google Scholar] [CrossRef]
- Huang, C.; Qiao, S.; Li, D.; Piao, X.; Ren, J. Effects of Lactobacilli on the performance, diarrhea incidence, VFA concentration and gastrointestinal microbial flora of weaning pigs. Asian-Australas J. Anim. Sci. 2004, 17, 401–409. [Google Scholar] [CrossRef]
- Pieper, R.; Janczyk, P.; Schumann, R.; Souffrant, W. The intestinal microflora of piglets around weaning with emphasis on lactobacilli. Arch. Zootech. 2006, 9, 28–40. [Google Scholar]
- De Angelis, M.; Siragusa, S.; Caputo, L.; Ragni, A.; Burzigotti, R.; Gobbetti, M. Survival and persistence of Lactobacillus plantarum 4.1 and Lactobacillus reuteri 3S7 in the gastrointestinal tract of pigs. Vet. Microbiol. 2007, 123, 133–144. [Google Scholar] [CrossRef]
- Castillo, M.; Martín-Orúe, S.M.; Manzanilla, E.G.; Badiola, I.; Martín, M.; Gasa, J. Quantification of total bacteria, enterobacteria and lactobacilli populations in pig digesta by real-time PCR. Vet. Microbiol. 2006, 114, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Zhang, N.; Zhou, M.; Tu, Y.; Deng, K.; Diao, Q. Effects of dietary probiotics on growth performance, faecal microbiota and serum profiles in weaned piglets. Anim. Prod. Sci. 2014, 54, 616–621. [Google Scholar] [CrossRef]
- Wang, W.; Chen, J.; Zhou, H.; Wang, L.; Ding, S.; Wang, Y.; Song, D.; Li, A. Effects of microencapsulated Lactobacillus plantarum and fructooligosaccharide on growth performance, blood immune parameters, and intestinal morphology in weaned piglets. Food Agric. Immunol. 2018, 29, 84–94. [Google Scholar] [CrossRef] [Green Version]
- Naqid, I.A.; Owen, J.P.; Maddison, B.C.; Gardner, D.S.; Foster, N.; Tchórzewska, M.A.; La Ragione, R.M.; Gough, K.C. Prebiotic and probiotic agents enhance antibody-based immune responses to Salmonella Typhimurium infection in pigs. Anim. Feed Sci. Technol. 2015, 201, 57–65. [Google Scholar] [CrossRef]
- Belik, S.N.; Gorlov, I.F.; Slozhenkina, M.I.; Zlobina, E.Y.; Pavlenko, A.S. Morpho-functional state of the liver of the rats fed the rations with meat of the pigs grown with antimicrobials. Pak. Vet. J. 2015, 35, 325–328. [Google Scholar]
- Klem, T.B.; Bleken, E.; Morberg, H.; Thoresen, S.I.; Framstad, T. Hematologic and biochemical reference intervals for Norwegian crossbreed grower pigs. Vet. Clin. Pathol. 2010, 39, 221–226. [Google Scholar] [CrossRef]
- Friendship, R.M.; Lumsden, J.H.; McMillan, I.; Wilson, M.R. Hematology and Biochemistry Reference Values for Ontario Swine. Can. J. Comp. Med. 1984, 48, 390–393. [Google Scholar]
- Caprarulo, V.; Hejna, M.; Giromini, C.; Liu, Y.; Dell’Anno, M.; Sotira, S.; Reggi, S.; Sgoifo-Rossi, C.A.; Callegari, M.L.; Rossi, L. Evaluation of Dietary Administration of Chestnut and Quebracho Tannins on Growth, Serum Metabolites and Fecal Parameters of Weaned Piglets. Animals 2020, 10, 1945. [Google Scholar] [CrossRef]
- IZSLER. Parametri di Chimica Clinica: Valori Osservati in Suini di Diversa Età. Available online: https://www.izsler.it/pls/izs_bs/v3_s2ew_consultazione.mostra_pagina?id_pagina=1494 (accessed on 18 March 2021).
- Pereg, D.; Kotliroff, A.; Gadoth, N.; Hadary, R.; Lishner, M.; Kitay-Cohen, Y. Probiotics for patients with compensated liver cirrhosis: A double-blind placebo-controlled study. Nutrition 2011, 27, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Metzler, B.; Mosenthin, R. A review of interactions between dietary fiber and the gastrointestinal microbiota and their consequences on intestinal phosphorus metabolism in growing pigs. Asian-Australas. J. Anim. Sci. 2008, 21, 603–615. [Google Scholar] [CrossRef]
- Wang, J.; Wu, C.; Feng, J. Effect of dietary antibacterial peptide and zinc-methionine on performance and serum biochemical parameters in piglets. Czech J. Anim. Sci. 2011, 56, 30–36. [Google Scholar] [CrossRef] [Green Version]
- Li, C.; Nie, S.P.; Ding, Q.; Zhu, K.X.; Wang, Z.J.; Xiong, T.; Gong, J.; Xie, M.Y. Cholesterol-lowering effect of Lactobacillus plantarum NCU116 in a hyperlipidaemic rat model. J. Funct. Foods 2014, 8, 340–347. [Google Scholar] [CrossRef]
- Taranto, M.P.; Medici, M.; Perdigon, G.; Holgado, A.R.; Valdez, G. Effect of Lactobacillus reuteri on the prevention of hypercholesterolemia in mice. J. Dairy Sci. 2000, 83, 401–403. [Google Scholar] [CrossRef]
- Park, Y.; Kim, J.; Shin, Y.; Kim, S.; Whang, K. Effect of dietary inclusion of Lactobacillus acidophilus ATCC 43121 on cholesterol metabolism in rats. J. Microbiol. Biotechnol. 2007, 17, 655–662. [Google Scholar]
- Xie, N.; Cui, Y.; Yin, Y.; Zhao, X.; Yang, J.; Wang, Z.; Fu, N.; Tang, Y.; Wang, X.; Liu, X.; et al. Effects of two Lactobacillus strains on lipid metabolism and intestinal microflora in rats fed a high-cholesterol diet. BMC Complementary Altern. Med. 2011, 11. [Google Scholar] [CrossRef] [Green Version]




| Ingredients, % as Fed Basis | CTRL | TRT | |
|---|---|---|---|
| Barley, meal | 26.84 | 26.84 | |
| Wheat, meal | 12.45 | 10.45 | |
| Corn, flakes | 11.63 | 11.63 | |
| Corn, meal | 10.00 | 10.00 | |
| Barley, flakes | 7.50 | 7.50 | |
| Soy protein concentrates | 5.00 | 5.00 | |
| Biscuits, meal | 4.00 | 4.00 | |
| Soybean, meal | 4.00 | 4.00 | |
| Dextrose monohydrate | 3.50 | 3.50 | |
| Sweet milk whey | 3.20 | 3.20 | |
| Herring, meal | 2.00 | 2.00 | |
| Plasma, meal | 2.00 | 2.00 | |
| Organic acids 1 | 1.70 | 1.70 | |
| Coconut oil | 1.00 | 1.00 | |
| Soy oil | 1.00 | 1.00 | |
| Arbocel 2 | 0.70 | 0.70 | |
| Dicalcium phosphate | 0.60 | 0.60 | |
| L-Lysine | 0.60 | 0.60 | |
| Benzoic acid | 0.50 | 0.50 | |
| Vitamin and mineral premix 3 | 0.50 | 0.50 | |
| DL-Methionine | 0.39 | 0.39 | |
| L-Threonine | 0.35 | 0.35 | |
| Sodium Chloride | 0.27 | 0.27 | |
| L-Valine (96.5%) | 0.12 | 0.12 | |
| Enzymes 4 | 0.10 | 0.10 | |
| L-Tryptophan | 0.05 | 0.05 | |
| Experimental mix 5 | - | 2.00 | |
| Calculated Chemical Composition 6 | |||
| Crude protein (%) | 17.00 | 17.00 | |
| Fat (%) | 4.20 | 4.20 | |
| Crude fibre (%) | 2.90 | 2.90 | |
| Ashes (%) | 5.20 | 5.20 | |
| DE 7 (Mc/Kg) | 3.92 | 3.83 | |
| Analyte | CTRL | PLA | REU | P+R |
| DM | 90.89 | 91.14 | 91.14 | 90.78 |
| CP | 16.34 | 17.01 | 16.38 | 16.64 |
| EE | 3.98 | 3.78 | 3.74 | 3.80 |
| CF | 3.60 | 3.65 | 3.34 | 3.40 |
| Ashes | 4.59 | 4.49 | 4.54 | 4.25 |
| FA Composition (% Total FAMEs) | CTRL | TRT | ||
| Caproic acid, C6:0 | 0.04 | 0.04 | ||
| Caprylic acid, C8:0 | 1.00 | 1.10 | ||
| Capric acid, C10:0 | 1.12 | 1.21 | ||
| Undecanoic acid, C11:0 | 0.00 | 0.00 | ||
| Lauric acid, C12:0 | 10.85 | 11.69 | ||
| Tridecanoic acid, C13:0 | 0.01 | 0.01 | ||
| Myristic acid, C14:0 | 5.23 | 5.45 | ||
| Mysticoleic acid, C14:1 | 0.01 | 0.01 | ||
| Pentadecanoic acid, C 15:0 | 0.05 | 0.06 | ||
| cis-10 Heptadecenoic acid, C 17:0 | 0.00 | 0.00 | ||
| Stearic acid, C 18:0 | 15.17 | 14.95 | ||
| Elaidic acid, C 18:1 n9t | 0.23 | 0.22 | ||
| Oleic acid, C 18:1 n9c | 0.09 | 0.08 | ||
| Linolelaidic acid, C18:2 n6t | 0.00 | 0.00 | ||
| Linoleic acid, C 18:2 n6c | 4.34 | 4.07 | ||
| γ-Linolenic acid, C 18:3 n6 | 0.05 | 0.04 | ||
| α-Linolenic acid, C18:3 n3 | 22.71 | 22.50 | ||
| Arachidic acid, C 20:0 | 0.00 | 0.00 | ||
| Cis-11 Eicosenoic acid, C20:1 | 34.42 | 33.92 | ||
| Cis-11,14 Eicosenoic acid, C20:2 | 0.04 | 0.04 | ||
| Cis-8,11,14 Eicosatrienoic acid, C20:3 n6 | 2.65 | 2.74 | ||
| Cis-11,14,17 Eicosatrienoic acid, C20:3 n3 | 0.31 | 0.29 | ||
| Arachidonic acid, C20:4 n6 | 0.43 | 0.40 | ||
| Cis-5,8,11,14,17 Eicosapentaenoic acid, C20:5 n3 | 0.05 | 0.04 | ||
| Heneicosanoic acid, C21:0 | 0.00 | 0.00 | ||
| Behenic acid, C22:0 | 0.01 | 0.01 | ||
| Erucic acid, C22:1 n9 | 0.02 | 0.02 | ||
| Cis-13,16 Docosadienoic acid, C22:2 | 0.26 | 0.25 | ||
| Cis-4,7,10,13,16,19 Docosahexaenoic acid, C22:6 n3 | 0.02 | 0.02 | ||
| Lignoceric acid; C24:0 | 0.25 | 0.23 | ||
| Nervonic acid, C24:1 | 0.04 | 0.04 | ||
| SFA | 38.64 | 39.36 | ||
| MUFA | 23.52 | 23.25 | ||
| PUFA | 37.83 | 37.39 | ||
| Serum Metabolite | CTRL | PLA | REU | P+R | p-Value |
|---|---|---|---|---|---|
| Total protein content, g/L | 53.26 ± 1.23 | 54.85 ± 1.15 | 51.84 ± 1.15 | 52.09 ± 1.15 | 0.2576 |
| Albumin, g/L | 28.35 ± 0.74 | 26.00 ± 0.70 | 25.94 ± 0.70 | 26.77 ± 0.70 | 0.0916 |
| Globulin, g/L | 24.91 ± 1.09 a | 28.89 ± 1.03 b | 25.91 ± 1.03 a | 25.31 ± 1.03 a | 0.0455 |
| Albumin/Globulin (A/G) | 1.16 ± 0.05 a | 0.92 ± 0.05 b | 1.06 ± 0.05 a,b | 1.01 ± 0.05 a,b | 0.0287 |
| Urea, mmol/L | 1.06 ± 0.21 | 1.42 ± 0.20 | 0.96 ± 0.20 | 0.89 ± 0.20 | 0.2452 |
| Alanine aminotransferase (ALT-GPT), IU/L | 50.00 ± 2.89 a | 38.22 ± 2.73 b | 35.78 ± 2.73 b | 46.00 ± 2.73 a,b | 0.0034 |
| Total bilirubin, µmol/L | 1.84 ± 0.13 | 1.42 ± 0.12 | 1.45 ± 0.12 | 1.58 ± 0.12 | 0.1021 |
| Glucose, mmol/L | 6.36 ± 0.47 | 6.31 ± 0.44 | 5.36 ± 0.44 | 6.41 ± 0.44 | 0.2926 |
| Phosphorus, mmol/L | 3.19 ± 0.09 a,b | 2.87 ± 0.08 a | 2.98 ± 0.08 a | 3.30 ± 0.08 b | 0.0038 |
| Magnesium, mmol/L | 0.92 ± 0.04 a | 0.77 ± 0.11 b | 0.79 ± 0.12 a,b | 0.85 ± 0.13 a,b | 0.0196 |
| Creatinine, µmol/L | 70.75 ± 3.51 | 77.33 ± 3.31 | 76.00 ± 3.31 | 81.10 ± 3.31 | 0.2175 |
| Total cholesterol, mmol/L | 2.70 ± 0.14 a | 2.20 ± 0.13 b | 2.27 ± 0.13 b | 2.68 ± 0.13 a | 0.0195 |
| High density lipoprotein (HDL), mmol/L | 1.08 ± 0.06 a | 0.77 ± 0.06 b | 0.81 ± 0.06 b | 1.04 ± 0.06 a | 0.0011 |
| Low density lipoprotein (LDL), mmol/L | 1.50 ± 0.09 | 1.26 ± 0.09 | 1.31 ± 0.09 | 1.52 ± 0.09 | 0.1173 |
| Triglycerides, mmol/L | 0.58 ± 0.08 | 0.83 ± 0.07 | 0.70 ± 007 | 0.60 ± 0.07 | 0.0764 |
| Interleukin 3, pg/L | 17.80 ± 1.98 | 14.78 ± 2.17 | 17.28 ± 2.17 | 17.90 ± 2.17 | 0.7098 |
| Interleukin 6, pg/L | 166.47 ± 45.87 | 152.65 ± 45.87 | 155.06 ± 45.87 | 166.48 ± 45.87 | 0.9941 |
| Interleukin 10, pg/L | 10.67 ± 2.13 | 8.91 ± 2.13 | 8.49 ± 2.13 | 10.80 ± 2.13 | 0.8158 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dell’Anno, M.; Callegari, M.L.; Reggi, S.; Caprarulo, V.; Giromini, C.; Spalletta, A.; Coranelli, S.; Sgoifo Rossi, C.A.; Rossi, L. Lactobacillus plantarum and Lactobacillus reuteri as Functional Feed Additives to Prevent Diarrhoea in Weaned Piglets. Animals 2021, 11, 1766. https://doi.org/10.3390/ani11061766
Dell’Anno M, Callegari ML, Reggi S, Caprarulo V, Giromini C, Spalletta A, Coranelli S, Sgoifo Rossi CA, Rossi L. Lactobacillus plantarum and Lactobacillus reuteri as Functional Feed Additives to Prevent Diarrhoea in Weaned Piglets. Animals. 2021; 11(6):1766. https://doi.org/10.3390/ani11061766
Chicago/Turabian StyleDell’Anno, Matteo, Maria Luisa Callegari, Serena Reggi, Valentina Caprarulo, Carlotta Giromini, Ambra Spalletta, Simona Coranelli, Carlo Angelo Sgoifo Rossi, and Luciana Rossi. 2021. "Lactobacillus plantarum and Lactobacillus reuteri as Functional Feed Additives to Prevent Diarrhoea in Weaned Piglets" Animals 11, no. 6: 1766. https://doi.org/10.3390/ani11061766
APA StyleDell’Anno, M., Callegari, M. L., Reggi, S., Caprarulo, V., Giromini, C., Spalletta, A., Coranelli, S., Sgoifo Rossi, C. A., & Rossi, L. (2021). Lactobacillus plantarum and Lactobacillus reuteri as Functional Feed Additives to Prevent Diarrhoea in Weaned Piglets. Animals, 11(6), 1766. https://doi.org/10.3390/ani11061766









