Pathophysiology, Diagnosis, and Management of Canine Intestinal Lymphangiectasia: A Comparative Review
Abstract
Simple Summary
Abstract
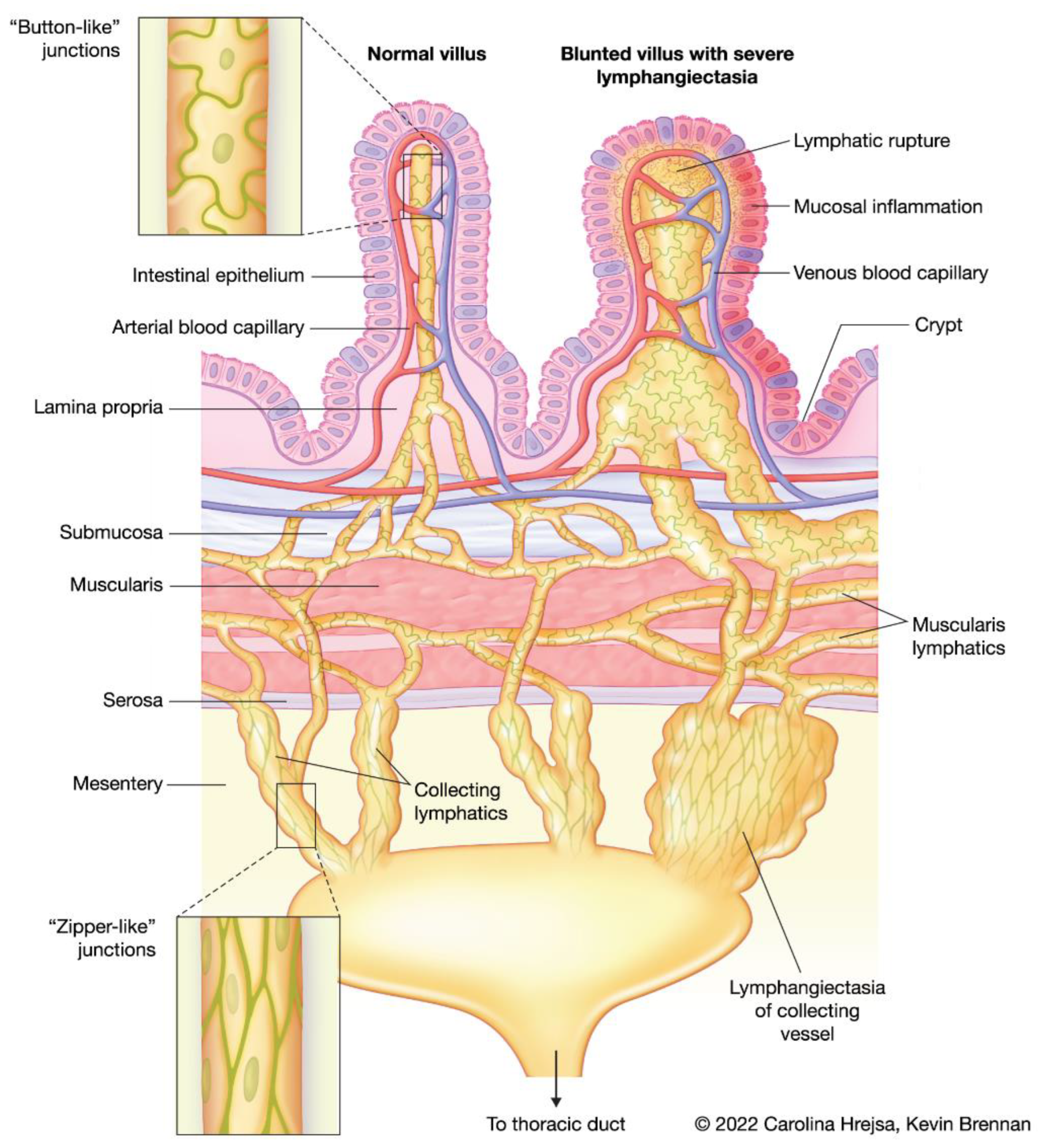
1. Overview of the Intestinal Lymphatic Vasculature
2. Pathophysiology
2.1. Lymphatic Disturbances and Consequences
2.2. Intestinal Lymphatic Disorders in Humans
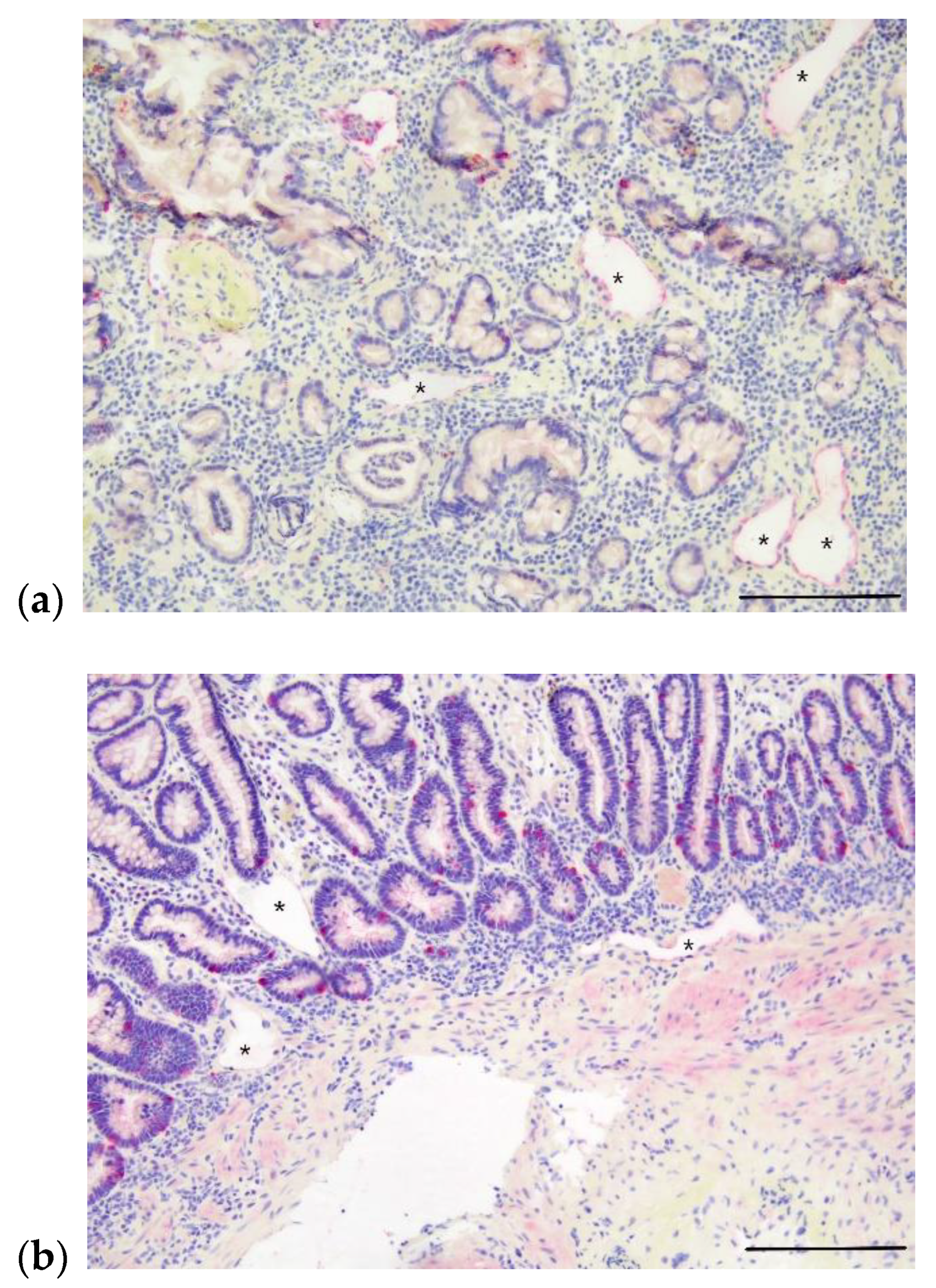
2.3. Intestinal Lymphatic Disorders in Dogs
3. Diagnosis
4. Management
4.1. Management of PIL in Humans
| Therapy | Mechanism of Action | Citations |
|---|---|---|
| Low-fat, high-protein, MCT diet | Decreases excessive lymphatic dilation and rupture | [23,91,92,93,94,95,96] |
| Octreotide | Decreased fat absorption | [97,115,116,117,118,119,120,121,122,123] |
| Inhibits GI vasoactive peptides Induces splanchnic vasoconstriction | ||
| Sirolimus or everolimus | Suppress lymphatic sprouting and proliferation | [124,125] |
| Propanolol | Reduces expression of vascular endothelial growth factor | [109,110] |
| Tranexamic acid | Normalization of fibrinolytic activity (increased fibrinolytic activity leads to protein loss) | [97,111] |
| Surgical resection | Direct removal of affected tissue | [100,101,102,103,104,105] |
| Lymphatic embolization | Address focal leakage of lymphatic vasculature | [64,106,107,108] |
4.2. Management of IL in Dogs
5. Conclusions and Future Directions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alexander, J.S.; Ganta, V.C.; Jordan, P.A.; Witte, M.H. Gastrointestinal Lymphatics in Health and Disease. Pathophysiol. Off. J. Int. Soc. Pathophysiol. 2010, 17, 315–335. [Google Scholar] [CrossRef] [PubMed]
- Goswami, A.K.; Khaja, M.S.; Downing, T.; Kokabi, N.; Saad, W.E.; Majdalany, B.S. Lymphatic Anatomy and Physiology. Semin. Interv. Radiol. 2020, 37, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.J.; McDole, J.R.; Newberry, R.D. Microanatomy of the Intestinal Lymphatic System. Ann. N. Y. Acad. Sci. 2010, 1207 (Suppl. S1), E21–E28. [Google Scholar] [CrossRef] [PubMed]
- Cifarelli, V.; Eichmann, A. The Intestinal Lymphatic System: Functions and Metabolic Implications. Cell Mol. Gastroenterol. Hepatol. 2019, 7, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Ohtani, O. Three-Dimensional Organization of Lymphatics and Its Relationship to Blood Vessels in Rat Small Intestine. Cell Tissue Res. 1987, 248, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Dixon, J.B. Lymphatic Lipid Transport: Sewer or Subway? Trends Endocrinol. Metab. Tem 2010, 21, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Li, Y.; Gong, J.; Zhu, W. Mesenteric Organ Lymphatics and Inflammatory Bowel Disease. Ann. Anat. Anat. Anz. Off. Organ Anat. Ges. 2018, 218, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Hokari, R.; Tomioka, A. The Role of Lymphatics in Intestinal Inflammation. Inflamm. Regen. 2021, 41, 25. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ocansey, D.K.W.; Liu, L.; Olovo, C.V.; Zhang, X.; Qian, H.; Xu, W.; Mao, F. Implications of Lymphatic Alterations in the Pathogenesis and Treatment of Inflammatory Bowel Disease. Biomed. Pharmacother. Biomed. Pharmacother. 2021, 140, 111752. [Google Scholar] [CrossRef]
- Oliver, G.; Sosa-Pineda, B.; Geisendorf, S.; Spana, E.P.; Doe, C.Q.; Gruss, P. Prox 1, a Prospero-Related Homeobox Gene Expressed during Mouse Development. Mech. Dev. 1993, 44, 3–16. [Google Scholar] [CrossRef]
- Podgrabinska, S.; Braun, P.; Velasco, P.; Kloos, B.; Pepper, M.S.; Skobe, M. Molecular Characterization of Lymphatic Endothelial Cells. Proc. Natl. Acad. Sci. USA. 2002, 99, 16069–16074. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.S.; Chaitanya, G.V.; Grisham, M.B.; Boktor, M. Emerging Roles of Lymphatics in Inflammatory Bowel Disease. Ann. N. Y. Acad. Sci. 2010, 1207 (Suppl. S1), E75–E85. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, S.; Davis, M.J.; Muthuchamy, M. Emerging Trends in the Pathophysiology of Lymphatic Contractile Function. Semin. Cell Dev. Biol. 2015, 38, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.B.; Kechele, D.O.; Blakeney, E.S.; Pawlak, J.B.; Caron, K.M. Lymphatic Deletion of Calcitonin Receptor-like Receptor Exacerbates Intestinal Inflammation. JCI Insight 2017, 2, e92465. [Google Scholar] [CrossRef] [PubMed]
- Liao, S.; von der Weid, P.-Y. Inflammation-Induced Lymphangiogenesis and Lymphatic Dysfunction. Angiogenesis 2014, 17, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.F.; MacNaughton, W.K.; von der Weid, P.-Y. Lymphatic Vessel Contractile Activity and Intestinal Inflammation. Mem. Inst. Oswaldo Cruz 2005, 100 (Suppl. S1), 107–110. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dossin, O.; Lavoué, R. Protein-Losing Enteropathies in Dogs. Vet. Clin. North Am. Small Anim. Pract. 2011, 41, 399–418. [Google Scholar] [CrossRef] [PubMed]
- Craven, M.D.; Washabau, R.J. Comparative Pathophysiology and Management of Protein-Losing Enteropathy. J. Vet. Intern. Med. 2019, 33, 383–402. [Google Scholar] [CrossRef]
- Kull, P.A.; Hess, R.S.; Craig, L.E.; Saunders, H.M.; Washabau, R.J. Clinical, Clinicopathologic, Radiographic, and Ultrasonographic Characteristics of Intestinal Lymphangiectasia in Dogs: 17 Cases (1996–1998). J. Am. Vet. Med. Assoc. 2001, 219, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.N.; Day, A.S. Primary Intestinal Lymphangiectasia in Children: A Review. J. Paediatr. Child Health 2020, 56, 1719–1723. [Google Scholar] [CrossRef] [PubMed]
- Magdo, H.S.; Stillwell, T.L.; Greenhawt, M.J.; Stringer, K.A.; Yu, S.; Fifer, C.G.; Russell, M.W.; Schumacher, K.R. Immune Abnormalities in Fontan Protein-Losing Enteropathy: A Case-Control Study. J. Pediatr. 2015, 167, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Fuss, I.J.; Strober, W.; Cuccherini, B.A.; Pearlstein, G.R.; Bossuyt, X.; Brown, M.; Fleisher, T.A.; Horgan, K. Intestinal Lymphangiectasia, a Disease Characterized by Selective Loss of Naive CD45RA+ Lymphocytes into the Gastrointestinal Tract. Eur. J. Immunol. 1998, 28, 4275–4285. [Google Scholar] [CrossRef]
- Huber, R.; Semmler, G.; Mayr, A.; Offner, F.; Datz, C. Primary Intestinal Lymphangiectasia in an Adult Patient: A Case Report and Review of Literature. World J. Gastroenterol. 2020, 26, 7707–7718. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Tang, Q.; Wu, J.; Wang, Y.; Cai, W. Primary Intestinal Lymphangiectasia: Four Case Reports and a Review of the Literature. Dig. Dis. Sci. 2010, 55, 3466–3472. [Google Scholar] [CrossRef]
- Waldmann, T.A.; Steinfeld, J.L.; Dutcher, T.F.; Davidson, J.D.; Gordon, R.S. The Role of the Gastrointestinal System in “Idiopathic Hypoproteinemia”. Gastroenterology 1961, 41, 197–207. [Google Scholar] [CrossRef]
- Braamskamp, M.J.A.M.; Dolman, K.M.; Tabbers, M.M. Clinical Practice. Protein-Losing Enteropathy in Children. Eur. J. Pediatr. 2010, 169, 1179–1185. [Google Scholar] [CrossRef]
- Hardikar, W.; Smith, A.L.; Chow, C.W. Neonatal Protein-Losing Enteropathy Caused by Intestinal Lymphatic Hypoplasia in Siblings. J. Pediatr. Gastroenterol. Nutr. 1997, 25, 217–221. [Google Scholar] [CrossRef]
- Cheslock, M.; Harrington, D.W. Yellow Nail Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Malek, N.P.; Ocran, K.; Tietge, U.J.; Maschek, H.; Gratz, K.F.; Trautwein, C.; Wagner, S.; Manns, M.P. A Case of the Yellow Nail Syndrome Associated with Massive Chylous Ascites, Pleural and Pericardial Effusions. Z. Gastroenterol. 1996, 34, 763–766. [Google Scholar]
- Ferrell, R.E.; Finegold, D.N. Research Perspectives in Inherited Lymphatic Disease: An Update. Ann. N. Y. Acad. Sci. 2008, 1131, 134–139. [Google Scholar] [CrossRef]
- Irrthum, A.; Karkkainen, M.J.; Devriendt, K.; Alitalo, K.; Vikkula, M. Congenital Hereditary Lymphedema Caused by a Mutation That Inactivates VEGFR3 Tyrosine Kinase. Am. J. Hum. Genet. 2000, 67, 295–301. [Google Scholar] [CrossRef]
- Atton, G.; Gordon, K.; Brice, G.; Keeley, V.; Riches, K.; Ostergaard, P.; Mortimer, P.; Mansour, S. The Lymphatic Phenotype in Turner Syndrome: An Evaluation of Nineteen Patients and Literature Review. Eur. J. Hum. Genet. 2015, 23, 1634–1639. [Google Scholar] [CrossRef] [PubMed]
- Hennekam, R.C.; Geerdink, R.A.; Hamel, B.C.; Hennekam, F.A.; Kraus, P.; Rammeloo, J.A.; Tillemans, A.A. Autosomal Recessive Intestinal Lymphangiectasia and Lymphedema, with Facial Anomalies and Mental Retardation. Am. J. Med. Genet. 1989, 34, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Umar, S.B.; DiBaise, J.K. Protein-Losing Enteropathy: Case Illustrations and Clinical Review. Am. J. Gastroenterol. 2010, 105, 43–49; quiz 50. [Google Scholar] [CrossRef] [PubMed]
- Feldt, R.H.; Driscoll, D.J.; Offord, K.P.; Cha, R.H.; Perrault, J.; Schaff, H.V.; Puga, F.J.; Danielson, G.K. Protein-Losing Enteropathy after the Fontan Operation. J. Thorac. Cardiovasc. Surg. 1996, 112, 672–680. [Google Scholar] [CrossRef]
- Van Kruiningen, H.J.; Colombel, J.-F. The Forgotten Role of Lymphangitis in Crohn’s Disease. Gut 2008, 57, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.S.; Brobst, D.; Bisgard, G. Intestinal Lymphangiectasia in a Dog. J. Am. Vet. Med. Assoc. 1968, 153, 1051–1054. [Google Scholar]
- Allenspach, K.; Iennarella-Servantez, C. Canine Protein Losing Enteropathies and Systemic Complications. Vet. Clin. N. Am. Small Anim. Pract. 2021, 51, 111–122. [Google Scholar] [CrossRef]
- Olson, N.C.; Zimmer, J.F. Protein-Losing Enteropathy Secondary to Intestinal Lymphangiectasia in a Dog. J. Am. Vet. Med. Assoc. 1978, 173, 271–274. [Google Scholar]
- Jones, B.R.; Labuc, R.H.; Jones, J.M.; Pauli, J.V.; Arthur, D.E. Intestinal Lymphangiectasia in a Dog. N. Z. Vet. J. 1984, 32, 213–216. [Google Scholar] [CrossRef]
- Kleint, M. [Intestinal lymphangiectasis in the dog. A literature review with a case history]. Tierarztl. Prax. 1994, 22, 165–171. [Google Scholar]
- Mattheeuws, D.; De Rick, A.; Thoonen, H.; Van Der Stock, J. Intestinal Lymphangiectasia in a Dog. J. Small Anim. Pract. 1974, 15, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Milstein, M.; Sanford, S.E. Intestinal Lymphangiectasia in a Dog. Can. Vet. J. Rev. Veterinaire Can. 1977, 18, 127–130. [Google Scholar]
- Simmerson, S.M.; Armstrong, P.J.; Wünschmann, A.; Jessen, C.R.; Crews, L.J.; Washabau, R.J. Clinical Features, Intestinal Histopathology, and Outcome in Protein-Losing Enteropathy in Yorkshire Terrier Dogs. J. Vet. Intern. Med. 2014, 28, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Allenspach, K.; Lomas, B.; Wieland, B.; Harris, T.; Pressler, B.; Mancho, C.; Lees, G.E.; Vaden, S.L. Evaluation of Perinuclear Anti-Neutrophilic Cytoplasmic Autoantibodies as an Early Marker of Protein-Losing Enteropathy and Protein-Losing Nephropathy in Soft Coated Wheaten Terriers. Am. J. Vet. Res. 2008, 69, 1301–1304. [Google Scholar] [CrossRef] [PubMed]
- Littman, M.P.; Dambach, D.M.; Vaden, S.L.; Giger, U. Familial Protein-Losing Enteropathy and Protein-Losing Nephropathy in Soft Coated Wheaten Terriers: 222 Cases (1983–1997). J. Vet. Intern. Med. 2000, 14, 68–80. [Google Scholar] [CrossRef]
- Jablonski Wennogle, S.A.; Priestnall, S.L.; Webb, C.B. Histopathologic Characteristics of Intestinal Biopsy Samples from Dogs with Chronic Inflammatory Enteropathy with and without Hypoalbuminemia. J. Vet. Intern. Med. 2017, 31, 371–376. [Google Scholar] [CrossRef]
- García-Sancho, M.; Sainz, A.; Villaescusa, A.; Rodríguez, A.; Rodríguez-Franco, F. White Spots on the Mucosal Surface of the Duodenum in Dogs with Lymphocytic Plasmacytic Enteritis. J. Vet. Sci. 2011, 12, 165–169. [Google Scholar] [CrossRef]
- Okanishi, H.; Yoshioka, R.; Kagawa, Y.; Watari, T. The Clinical Efficacy of Dietary Fat Restriction in Treatment of Dogs with Intestinal Lymphangiectasia. J. Vet. Intern. Med. 2014, 28, 809–817. [Google Scholar] [CrossRef]
- Larson, R.N.; Ginn, J.A.; Bell, C.M.; Davis, M.J.; Foy, D.S. Duodenal Endoscopic Findings and Histopathologic Confirmation of Intestinal Lymphangiectasia in Dogs. J. Vet. Intern. Med. 2012, 26, 1087–1092. [Google Scholar] [CrossRef]
- Jablonski Wennogle, S.A.; Priestnall, S.L.; Suárez-Bonnet, A.; Webb, C.B. Comparison of Clinical, Clinicopathologic, and Histologic Variables in Dogs with Chronic Inflammatory Enteropathy and Low or Normal Serum 25-Hydroxycholecalciferol Concentrations. J. Vet. Intern. Med. 2019, 33, 1995–2004. [Google Scholar] [CrossRef]
- Lecoindre, A.; Lecoindre, P.; Cadoré, J.L.; Chevallier, M.; Guerret, S.; Derré, G.; Mcdonough, S.P.; Simpson, K.W. Focal Intestinal Lipogranulomatous Lymphangitis in 10 Dogs. J. Small Anim. Pract. 2016, 57, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Watson, V.E.; Hobday, M.M.; Durham, A.C. Focal Intestinal Lipogranulomatous Lymphangitis in 6 Dogs (2008–2011). J. Vet. Intern. Med. 2014, 28, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Van Kruiningen, H.J.; Lees, G.E.; Hayden, D.W.; Meuten, D.J.; Rogers, W.A. Lipogranulomatous Lymphangitis in Canine Intestinal Lymphangiectasia. Vet. Pathol. 1984, 21, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Malatos, J.M.; Kurpios, N.A.; Duhamel, G.E. Small Intestinal Lymphatic Hypoplasia in Three Dogs with Clinical Signs of Protein-Losing Enteropathy. J. Comp. Pathol. 2018, 160, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Fossum, T.W.; Sherding, R.G.; Zack, P.M.; Birchard, S.J.; Smeak, D.D. Intestinal Lymphangiectasia Associated with Chylothorax in Two Dogs. J. Am. Vet. Med. Assoc. 1987, 190, 61–64. [Google Scholar]
- Fossum, T.W.; Hodges, C.C.; Scruggs, D.W.; Fiske, R.A. Generalized Lymphangiectasis in a Dog with Subcutaneous Chyle and Lymphangioma. J. Am. Vet. Med. Assoc. 1990, 197, 231–236. [Google Scholar]
- Day, M.J.; Bilzer, T.; Mansell, J.; Wilcock, B.; Hall, E.J.; Jergens, A.; Minami, T.; Willard, M.; Washabau, R.; World Small Animal Veterinary Association Gastrointestinal Standardization Group. Histopathological Standards for the Diagnosis of Gastrointestinal Inflammation in Endoscopic Biopsy Samples from the Dog and Cat: A Report from the World Small Animal Veterinary Association Gastrointestinal Standardization Group. J. Comp. Pathol. 2008, 138 (Suppl. S1), S1–S43. [Google Scholar] [CrossRef]
- Procoli, F.; Mõtsküla, P.F.; Keyte, S.V.; Priestnall, S.; Allenspach, K. Comparison of Histopathologic Findings in Duodenal and Ileal Endoscopic Biopsies in Dogs with Chronic Small Intestinal Enteropathies. J. Vet. Intern. Med. 2013, 27, 268–274. [Google Scholar] [CrossRef]
- Jablonski Wennogle, S.A.; Priestnall, S.L.; Suárez-Bonnet, A.; Soontararak, S.; Webb, C.B. Lymphatic Endothelial Cell Immunohistochemical Markers for Evaluation of the Intestinal Lymphatic Vasculature in Dogs with Chronic Inflammatory Enteropathy. J. Vet. Intern. Med. 2019, 33, 1669–1676. [Google Scholar] [CrossRef]
- Kleinschmidt, S.; Meneses, F.; Nolte, I.; Hewicker-Trautwein, M. Retrospective Study on the Diagnostic Value of Full-Thickness Biopsies from the Stomach and Intestines of Dogs with Chronic Gastrointestinal Disease Symptoms. Vet. Pathol. 2006, 43, 1000–1003. [Google Scholar] [CrossRef]
- Sura, R.; Colombel, J.-F.; Van Kruiningen, H.J. Lymphatics, Tertiary Lymphoid Organs and the Granulomas of Crohn’s Disease: An Immunohistochemical Study. Aliment. Pharmacol. Ther. 2011, 33, 930–939. [Google Scholar] [CrossRef] [PubMed]
- Van Kruiningen, H.J.; Hayes, A.W.; Colombel, J.-F. Granulomas Obstruct Lymphatics in All Layers of the Intestine in Crohn’s Disease. APMIS 2014, 122, 1125–1129. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.; Kim, M.J. The Update of Treatment for Primary Intestinal Lymphangiectasia. Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Nagahara, T.; Ohno, K.; Nagao, I.; Nakagawa, T.; Goto-Koshino, Y.; Tsuboi, M.; Chambers, J.K.; Uchida, K.; Tomiyasu, H.; Tsujimoto, H. Evaluation of the Degree and Distribution of Lymphangiectasia in Full-Thickness Canine Small Intestinal Specimens Diagnosed with Lymphoplasmacytic Enteritis and Granulomatous Lymphangitis. J. Vet. Med. Sci. 2022, 84, 566–573. [Google Scholar] [CrossRef]
- Ohmiya, N.; Nakamura, M.; Yamamura, T.; Yamada, K.; Nagura, A.; Yoshimura, T.; Hirooka, Y.; Hirata, I.; Goto, H. Classification of Intestinal Lymphangiectasia with Protein-Losing Enteropathy: White Villi Type and Non-White Villi Type. Digestion 2014, 90, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Meng, M.-M.; Liu, K.-L.; Xue, X.-Y.; Hao, K.; Dong, J.; Yu, C.-K.; Liu, H.; Wang, C.-H.; Su, H.; Lin, W.; et al. Endoscopic Classification and Pathological Features of Primary Intestinal Lymphangiectasia. World J. Gastroenterol. 2022, 28, 2482–2493. [Google Scholar] [CrossRef] [PubMed]
- Jablonski Wennogle, S.A.; Stockman, J.; Webb, C.B. Prospective Evaluation of a Change in Dietary Therapy in Dogs with Steroid-Resistant Protein-Losing Enteropathy. J. Small Anim. Pract. 2021, 62, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Saygili, F.; Saygili, S.M.; Oztas, E. Examining the Whole Bowel, Double Balloon Enteroscopy: Indications, Diagnostic Yield and Complications. World J. Gastrointest. Endosc. 2015, 7, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Sarria, R.; López Albors, O.; Soria, F.; Ayala, I.; Pérez Cuadrado, E.; Esteban, P.; Latorre, R. Characterization of Oral Double Balloon Endoscopy in the Dog. Vet. J. Lond. Engl. 2013, 195, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Latorre, R.; Ayala, I.; Soria, F.; Carballo, F.; Ayala, M.D.; Pérez-Cuadrado, E. Double-Balloon Enteroscopy in Two Dogs. Vet. Rec. 2007, 161, 587–590. [Google Scholar] [CrossRef] [PubMed]
- Rivet, C.; Lapalus, M.-G.; Dumortier, J.; Le Gall, C.; Budin, C.; Bouvier, R.; Ponchon, T.; Lachaux, A. Use of Capsule Endoscopy in Children with Primary Intestinal Lymphangiectasia. Gastrointest. Endosc. 2006, 64, 649–650. [Google Scholar] [CrossRef] [PubMed]
- van der Reijden, S.M.; van Wijk, M.P.; Jacobs, M.A.J.M.; de Meij, T.G.J. Video Capsule Endoscopy to Diagnose Primary Intestinal Lymphangiectasia in a 14-Month-Old Child. J. Pediatr. Gastroenterol. Nutr. 2017, 64, e161. [Google Scholar] [CrossRef] [PubMed]
- Ersoy, O.; Akin, E.; Demirezer, A.; Yilmaz, E.; Solakoglu, T.; Irkkan, C.; Yurekli, O.T.; Buyukasik, S. Evaluation of Primary Intestinal Lymphangiectasia by Capsule Endoscopy. Endoscopy 2013, 45 (Suppl. S2), E61–E62. [Google Scholar] [CrossRef] [PubMed]
- Chavhan, G.B.; Amaral, J.G.; Temple, M.; Itkin, M. MR Lymphangiography in Children: Technique and Potential Applications. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc 2017, 37, 1775–1790. [Google Scholar] [CrossRef]
- Brownell, J.N.; Biko, D.M.; Mamula, P.; Krishnamurthy, G.; Escobar, F.; Srinivasan, A.; Laje, P.; Piccoli, D.A.; Pinto, E.; Smith, C.L.; et al. Dynamic Contrast Magnetic Resonance Lymphangiography Localizes Lymphatic Leak to the Duodenum in Protein-Losing Enteropathy. J. Pediatr. Gastroenterol. Nutr. 2022, 74, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Kudo, T.; Endo, J.; Hashida, K.; Tachibana, N.; Murakoshi, T.; Hasebe, T. Transnodal Lymphangiography and Post-CT for Protein-Losing Enteropathy in Noonan Syndrome. Minim. Invasive Ther. Allied Technol. MITAT Off. J. Soc. Minim. Invasive Ther. 2015, 24, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Pascal, P.; Malloizel, J.; Lairez, O.; de Volontat, M.D.; Bournet, B. Primary Intestinal Lymphangiectasia: Diagnostic Accuracy of 99mTc-Labeled Human Serum Albumin Nanocolloid SPECT/CT Before Biopsy. Clin. Nucl. Med. 2021, 46, e34–e35. [Google Scholar] [CrossRef] [PubMed]
- Sutherland-Smith, J.; Penninck, D.G.; Keating, J.H.; Webster, C.R.L. Ultrasonographic Intestinal Hyperechoic Mucosal Striations in Dogs Are Associated with Lacteal Dilation. Vet. Radiol. Ultrasound Off. J. Am. Coll. Vet. Radiol. Int. Vet. Radiol. Assoc. 2007, 48, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Pollard, R.E.; Johnson, E.G.; Pesavento, P.A.; Baker, T.W.; Cannon, A.B.; Kass, P.H.; Marks, S.L. Effects of Corn Oil Administered Orally on Conspicuity of Ultrasonographic Small Intestinal Lesions in Dogs with Lymphangiectasia. Vet. Radiol. Ultrasound Off. J. Am. Coll. Vet. Radiol. Int. Vet. Radiol. Assoc. 2013, 54, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Engelmann, N.; Ondreka, N.; von Pückler, K.; Mohrs, S.; Sicken, J.; Neiger, R. Applicability of 99m Tc-Labeled Human Serum Albumin Scintigraphy in Dogs with Protein-Losing Enteropathy. J. Vet. Intern. Med. 2017, 31, 365–370. [Google Scholar] [CrossRef]
- Heilmann, R.M.; Parnell, N.K.; Grützner, N.; Mansell, J.; Berghoff, N.; Schellenberg, S.; Reusch, C.E.; Suchodolski, J.S.; Steiner, J.M. Serum and Fecal Canine A1-Proteinase Inhibitor Concentrations Reflect the Severity of Intestinal Crypt Abscesses and/or Lacteal Dilation in Dogs. Vet. J. Lond. Engl. 2016, 207, 131–139. [Google Scholar] [CrossRef]
- Rossi, G.; Cerquetella, M.; Antonelli, E.; Pengo, G.; Magi, G.E.; Villanacci, V.; Rostami-Nejad, M.; Spaterna, A.; Bassotti, G. The Importance of Histologic Parameters of Lacteal Involvement in Cases of Canine Lymphoplasmacytic Enteritis. Gastroenterol. Hepatol. Bed Bench 2015, 8, 33–41. [Google Scholar] [PubMed]
- Rossi, G.; Gavazza, A.; Vincenzetti, S.; Mangiaterra, S.; Galosi, L.; Marchegiani, A.; Pengo, G.; Sagratini, G.; Ricciutelli, M.; Cerquetella, M. Clinicopathological and Fecal Proteome Evaluations in 16 Dogs Presenting Chronic Diarrhea Associated with Lymphangiectasia. Vet. Sci. 2021, 8, 242. [Google Scholar] [CrossRef] [PubMed]
- Nagahara, T.; Ohno, K.; Nagao, I.; Nakagawa, T.; Goto-Koshino, Y.; Tsuboi, M.; Chambers, J.K.; Uchida, K.; Tomiyasu, H.; Tsujimoto, H. Association between Intestinal Lymphangiectasia and Expression of Inducible Nitric Oxide Synthase in Dogs with Lymphoplasmacytic Enteritis. J. Vet. Med. Sci. 2022, 84, 20–24. [Google Scholar] [CrossRef] [PubMed]
- D’Alessio, S.; Correale, C.; Tacconi, C.; Gandelli, A.; Pietrogrande, G.; Vetrano, S.; Genua, M.; Arena, V.; Spinelli, A.; Peyrin-Biroulet, L.; et al. VEGF-C-Dependent Stimulation of Lymphatic Function Ameliorates Experimental Inflammatory Bowel Disease. J. Clin. Investig. 2014, 124, 3863–3878. [Google Scholar] [CrossRef]
- D’Alessio, S.; Tacconi, C.; Danese, S. Targeting Lymphatics in Inflammatory Bowel Disease. Oncotarget 2015, 6, 34047–34048. [Google Scholar] [CrossRef]
- Sigall Boneh, R.; Sarbagili Shabat, C.; Yanai, H.; Chermesh, I.; Ben Avraham, S.; Boaz, M.; Levine, A. Dietary Therapy with the Crohn’s Disease Exclusion Diet Is a Successful Strategy for Induction of Remission in Children and Adults Failing Biological Therapy. J. Crohns Colitis 2017, 11, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Khayat, A.A. Primary Intestinal Lymphangiectasia Presenting as Limb Hemihyperplasia: A Case Report and Literature Review. BMC Gastroenterol. 2021, 21, 225. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.P.; Guvenc, B.H.; Carachi, R. Evidence for Medium Chain Triglycerides in the Treatment of Primary Intestinal Lymphangiectasia. Eur. J. Pediatr. Surg. Off. J. Austrian Assoc. Pediatr. Surg. Al Z. Kinderchir. 2009, 19, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Greco, F.; Piccolo, G.; Sorge, A.; Pavone, P.; Triglia, T.; Spina, M.; Sorge, G. [Early-onset of primary intestinal lymphangiectasia. A case report and diet treatment]. Minerva Pediatr. 2003, 55, 615–619. [Google Scholar]
- Isa, H.M.; Al-Arayedh, G.G.; Mohamed, A.M. Intestinal Lymphangiectasia in Children. A Favorable Response to Dietary Modifications. Saudi Med. J. 2016, 37, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.; Yu, T.; Qiao, X.-Y.; Zhao, L.-N.; Chen, Q.-K. Primary Intestinal Lymphangiectasia Diagnosed by Double-Balloon Enteroscopy and Treated by Medium-Chain Triglycerides: A Case Report. J. Med. Case Reports 2013, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Liu, X.; He, Y.; Li, Q.; Ji, L.; Shen, W.; Tong, G. Nutritional Therapy and Effect Assessment of Infants with Primary Intestinal Lymphangiectasia: Case Reports. Medicine 2017, 96, e9240. [Google Scholar] [CrossRef] [PubMed]
- Martín, C.C.; García, A.F.-A.; Restrepo, J.M.R.; Pérez, A.S. [Sucessful dietetic-therapy in primary intestinal lymphangiectasia and recurrent chylous ascites: A case report]. Nutr. Hosp. 2007, 22, 723–725. [Google Scholar] [PubMed]
- Ohno, S.; Nakahara, S.; Kasahara, K.; Murakami, R.; Mitsuuchi, M.; Makiguchi, Y.; Takahashi, H.; Adachi, M.; Endo, T.; Imai, K.; et al. [A case report of primary intestinal lymphangiectesia successfully treated with low fat diet]. Nihon Shokakibyo Gakkai Zasshi Jpn. J. Gastro-Enterol. 1997, 94, 767–771. [Google Scholar]
- Prasad, D.; Srivastava, A.; Tambe, A.; Yachha, S.K.; Sarma, M.S.; Poddar, U. Clinical Profile, Response to Therapy, and Outcome of Children with Primary Intestinal Lymphangiectasia. Dig. Dis. Basel Switz. 2019, 37, 458–466. [Google Scholar] [CrossRef]
- Vignes, S.; Bellanger, J. Primary Intestinal Lymphangiectasia (Waldmann’s Disease). Orphanet J. Rare Dis. 2008, 3, 5. [Google Scholar] [CrossRef]
- Aoyagi, K.; Iida, M.; Matsumoto, T.; Sakisaka, S. Enteral Nutrition as a Primary Therapy for Intestinal Lymphangiectasia: Value of Elemental Diet and Polymeric Diet Compared with Total Parenteral Nutrition. Dig. Dis. Sci. 2005, 50, 1467–1470. [Google Scholar] [CrossRef]
- Chen, C.-P.; Chao, Y.; Li, C.-P.; Lo, W.-C.; Wu, C.-W.; Tsay, S.-H.; Lee, R.-C.; Chang, F.-Y. Surgical Resection of Duodenal Lymphangiectasia: A Case Report. World J. Gastroenterol. 2003, 9, 2880–2882. [Google Scholar] [CrossRef]
- Connor, F.L.; Angelides, S.; Gibson, M.; Larden, D.W.; Roman, M.R.; Jones, O.; Currie, B.G.; Day, A.S.; Bohane, T.D. Successful Resection of Localized Intestinal Lymphangiectasia Post-Fontan: Role of (99m)Technetium-Dextran Scintigraphy. Pediatrics 2003, 112, e242–e247. [Google Scholar] [CrossRef]
- Zhu, L.; Cai, X.; Mou, Y.; Zhu, Y.; Wang, S.; Wu, J. Partial Enterectomy: Treatment for Primary Intestinal Lymphangiectasia in Four Cases. Chin. Med. J. 2010, 123, 760–764. [Google Scholar] [PubMed]
- Huber, T.; Paschold, M.; Eckardt, A.J.; Lang, H.; Kneist, W. Surgical Therapy of Primary Intestinal Lymphangiectasia in Adults. J. Surg. Case Rep. 2015, 2015, rjv081. [Google Scholar] [CrossRef] [PubMed]
- Kneist, W.; Drescher, D.G.; Hansen, T.; Kreitner, K.F.; Lang, H. [Surgical therapy of segmental jejunal, primary intestinal lymphangiectasia]. Z. Gastroenterol. 2013, 51, 576–579. [Google Scholar] [CrossRef] [PubMed]
- Mari, J.; Kovacs, T.; Pasztor, G.; Tiszlavicz, L.; Bereczki, C.; Szucs, D. Pediatric Localized Intestinal Lymphangiectasia Treated with Resection. Int. Med. Case Rep. J. 2019, 12, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.; Kim, E.S.; Choe, Y.H.; Hyun, D.; Kim, M.J. Therapeutic Lymphatic Embolization in Pediatric Primary Intestinal Lymphangiectasia. Yonsei Med. J. 2021, 62, 470–473. [Google Scholar] [CrossRef] [PubMed]
- Kylat, R.I.; Witte, M.H.; Barber, B.J.; Dori, Y.; Ghishan, F.K. Resolution of Protein-Losing Enteropathy after Congenital Heart Disease Repair by Selective Lymphatic Embolization. Pediatr. Gastroenterol. Hepatol. Nutr. 2019, 22, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Li, A.A.; Raghu, P.; Chen, A.; Triadafilopoulos, G.; Park, W. Sticky Situation: Bleeding Duodenal Lymphangiectasias Treated with Lymphatic Glue Embolization. Dig. Dis. Sci. 2022, 67, 71–74. [Google Scholar] [CrossRef]
- Poralla, C.; Specht, S.; Born, M.; Müller, A.; Bartmann, P.; Müller, A. Treatment of Congenital Generalized Lymphangiectasia with Propranolol in a Preterm Infant. Pediatrics 2014, 133, e439–e442. [Google Scholar] [CrossRef]
- Liviskie, C.J.; Brennan, C.C.; McPherson, C.C.; Vesoulis, Z.A. Propranolol for the Treatment of Lymphatic Malformations in a Neonate-A Case Report and Review of Literature. J. Pediatr. Pharmacol. Ther. 2020, 25, 155–162. [Google Scholar] [CrossRef]
- MacLean, J.E.; Cohen, E.; Weinstein, M. Primary Intestinal and Thoracic Lymphangiectasia: A Response to Antiplasmin Therapy. Pediatrics 2002, 109, 1177–1180. [Google Scholar] [CrossRef]
- Thacker, D.; Patel, A.; Dodds, K.; Goldberg, D.J.; Semeao, E.; Rychik, J. Use of Oral Budesonide in the Management of Protein-Losing Enteropathy after the Fontan Operation. Ann. Thorac. Surg. 2010, 89, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Hoashi, T.; Ichikawa, H.; Ueno, T.; Kogaki, S.; Sawa, Y. Steroid Pulse Therapy for Protein-Losing Enteropathy after the Fontan Operation. Congenit. Heart Dis. 2009, 4, 284–287. [Google Scholar] [CrossRef] [PubMed]
- Fleisher, T.A.; Strober, W.; Muchmore, A.V.; Broder, S.; Krawitt, E.L.; Waldmann, T.A. Corticosteroid-Responsive Intestinal Lymphangiectasia Secondary to an Inflammatory Process. N. Engl. J. Med. 1979, 300, 605–606. [Google Scholar] [CrossRef] [PubMed]
- Al Sinani, S.; Rawahi, Y.A.; Abdoon, H. Octreotide in Hennekam Syndrome-Associated Intestinal Lymphangiectasia. World J. Gastroenterol. 2012, 18, 6333–6337. [Google Scholar] [CrossRef]
- Alshikho, M.J.; Talas, J.M.; Noureldine, S.I.; Zazou, S.; Addas, A.; Kurabi, H.; Nasser, M. Intestinal Lymphangiectasia: Insights on Management and Literature Review. Am. J. Case Rep. 2016, 17, 512–522. [Google Scholar] [CrossRef]
- Bac, D.J.; Van Hagen, P.M.; Postema, P.T.; ten Bokum, A.M.; Zondervan, P.E.; van Blankenstein, M. Octreotide for Protein-Losing Enteropathy with Intestinal Lymphangiectasia. Lancet Lond. Engl. 1995, 345, 1639. [Google Scholar] [CrossRef]
- Ballinger, A.B.; Farthing, M.J. Octreotide in the Treatment of Intestinal Lymphangiectasia. Eur. J. Gastroenterol. Hepatol. 1998, 10, 699–702. [Google Scholar]
- Filik, L.; Oguz, P.; Koksal, A.; Koklu, S.; Sahin, B. A Case with Intestinal Lymphangiectasia Successfully Treated with Slow-Release Octreotide. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2004, 36, 687–690. [Google Scholar] [CrossRef]
- Kuroiwa, G.; Takayama, T.; Sato, Y.; Takahashi, Y.; Fujita, T.; Nobuoka, A.; Kukitsu, T.; Kato, J.; Sakamaki, S.; Niitsu, Y. Primary Intestinal Lymphangiectasia Successfully Treated with Octreotide. J. Gastroenterol. 2001, 36, 129–132. [Google Scholar] [CrossRef]
- Sari, S.; Baris, Z.; Dalgic, B. Primary Intestinal Lymphangiectasia in Children: Is Octreotide an Effective and Safe Option in the Treatment? J. Pediatr. Gastroenterol. Nutr. 2010, 51, 454–457. [Google Scholar] [CrossRef]
- Suehiro, K.; Morikage, N.; Murakami, M.; Yamashita, O.; Hamano, K. Late-Onset Primary Intestinal Lymphangiectasia Successfully Managed with Octreotide: A Case Report. Ann. Vasc. Dis. 2012, 5, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Troskot, R.; Jurčić, D.; Bilić, A.; Gomerčić Palčić, M.; Težak, S.; Brajković, I. How to Treat an Extensive Form of Primary Intestinal Lymphangiectasia? World J. Gastroenterol. 2015, 21, 7320–7325. [Google Scholar] [CrossRef] [PubMed]
- Pollack, S.F.; Geffrey, A.L.; Thiele, E.A.; Shah, U. Primary Intestinal Lymphangiectasia Treated with Rapamycin in a Child with Tuberous Sclerosis Complex (TSC). Am. J. Med. Genet. A. 2015, 167, 2209–2212. [Google Scholar] [CrossRef] [PubMed]
- Ozeki, M.; Hori, T.; Kanda, K.; Kawamoto, N.; Ibuka, T.; Miyazaki, T.; Fukao, T. Everolimus for Primary Intestinal Lymphangiectasia with Protein-Losing Enteropathy. Pediatrics 2016, 137, e20152562. [Google Scholar] [CrossRef] [PubMed]
- Tolbert, M.K.; Murphy, M.; Gaylord, L.; Witzel-Rollins, A. Dietary Management of Chronic Enteropathy in Dogs. J. Small Anim. Pract. 2022, 63, 425–434. [Google Scholar] [CrossRef]
- Rudinsky, A.J.; Howard, J.P.; Bishop, M.A.; Sherding, R.G.; Parker, V.J.; Gilor, C. Dietary Management of Presumptive Protein-Losing Enteropathy in Yorkshire Terriers. J. Small Anim. Pract. 2017, 58, 103–108. [Google Scholar] [CrossRef]
- Nagata, N.; Ohta, H.; Yokoyama, N.; Teoh, Y.B.; Nisa, K.; Sasaki, N.; Osuga, T.; Morishita, K.; Takiguchi, M. Clinical Characteristics of Dogs with Food-Responsive Protein-Losing Enteropathy. J. Vet. Intern. Med. 2020, 34, 659–668. [Google Scholar] [CrossRef]
- Jensen, G.L.; McGarvey, N.; Taraszewski, R.; Wixson, S.K.; Seidner, D.L.; Pai, T.; Yeh, Y.Y.; Lee, T.W.; DeMichele, S.J. Lymphatic Absorption of Enterally Fed Structured Triacylglycerol vs Physical Mix in a Canine Model. Am. J. Clin. Nutr. 1994, 60, 518–524. [Google Scholar] [CrossRef]
- Economu, L.; Chang, Y.-M.; Priestnall, S.L.; Kathrani, A. The Effect of Assisted Enteral Feeding on Treatment Outcome in Dogs with Inflammatory Protein-Losing Enteropathy. J. Vet. Intern. Med. 2021, 35, 1297–1305. [Google Scholar] [CrossRef]
- Tanner, A.R.; Halliday, J.W.; Powell, L.W. Serum Prednisolone Levels in Crohn’s Disease and Coeliac Disease Following Oral Prednisolone Administration. Digestion 1981, 21, 310–315. [Google Scholar] [CrossRef]
- Allenspach, K.; Rizzo, J.; Jergens, A.E.; Chang, Y.M. Hypovitaminosis D Is Associated with Negative Outcome in Dogs with Protein Losing Enteropathy: A Retrospective Study of 43 Cases. BMC Vet. Res. 2017, 13, 96. [Google Scholar] [CrossRef] [PubMed]
- Salavati Schmitz, S.; Gow, A.; Bommer, N.; Morrison, L.; Mellanby, R. Diagnostic Features, Treatment, and Outcome of Dogs with Inflammatory Protein-Losing Enteropathy. J. Vet. Intern. Med. 2019, 33, 2005–2013. [Google Scholar] [CrossRef] [PubMed]
- deLaforcade, A.; Bacek, L.; Blais, M.-C.; Boyd, C.; Brainard, B.M.; Chan, D.L.; Cortellini, S.; Goggs, R.; Hoareau, G.L.; Koenigshof, A.; et al. 2022 Update of the Consensus on the Rational Use of Antithrombotics and Thrombolytics in Veterinary Critical Care (CURATIVE) Domain 1-Defining Populations at Risk. J. Vet. Emerg. Crit. Care 2001 2022, 32, 289–314. [Google Scholar] [CrossRef] [PubMed]


| Authors (Citation) Study Type | Dogs | Results |
|---|---|---|
| Okanishi et al. JVIM 2014;28:809–817 [49] Retrospective | 24 dogs with unresponsive or relapsed histologically confirmed IL | 19/24 (79%) dogs responded satisfactorily to dietary fat restriction |
| Rudinsky et al. JSAP 2017;58:103–108 [127] Retrospective | 11 Yorkshire terriers with PLE, 4 with histologically confirmed IL | Clinical signs resolved completely in 8 dogs with dietary therapy alone |
| Nagata et al. JVIM 2020;34:659–668 [128] Retrospective | 33 dogs with PLE, 25 with histologically confirmed IL | 17/21 IL dogs treated with ultra-low fat diet had partial or complete response |
| Jablonski Wennogle et al. JSAP 2021;62:756–764 [68] Prospective | 12 dogs with steroid-refractory PLE, 4 with histologically confirmed IL | 8/10 dogs had complete remission with dietary change; 7/8 had dietary fat lowered |
| Olson and Zimmer. JAVMA 1978;173:271–274 [39] Case report | 1.5 year old, female, Doberman pincher with IL and PLE | Remission of clinical signs and improvement of serum albumin with dietary therapy |
| Jones et al. NZ Vet J 1984;32:213–216 [40] Case report | 8 month old, female, mixed breed dog with IL and PLE | Full recovery with dietary management alone |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jablonski, S.A. Pathophysiology, Diagnosis, and Management of Canine Intestinal Lymphangiectasia: A Comparative Review. Animals 2022, 12, 2791. https://doi.org/10.3390/ani12202791
Jablonski SA. Pathophysiology, Diagnosis, and Management of Canine Intestinal Lymphangiectasia: A Comparative Review. Animals. 2022; 12(20):2791. https://doi.org/10.3390/ani12202791
Chicago/Turabian StyleJablonski, Sara A. 2022. "Pathophysiology, Diagnosis, and Management of Canine Intestinal Lymphangiectasia: A Comparative Review" Animals 12, no. 20: 2791. https://doi.org/10.3390/ani12202791
APA StyleJablonski, S. A. (2022). Pathophysiology, Diagnosis, and Management of Canine Intestinal Lymphangiectasia: A Comparative Review. Animals, 12(20), 2791. https://doi.org/10.3390/ani12202791







