Untargeted Analysis of Serum Metabolomes in Dogs with Exocrine Pancreatic Insufficiency
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population and Sample Collection
2.2. Untargeted Serum Metabolomics
2.3. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data
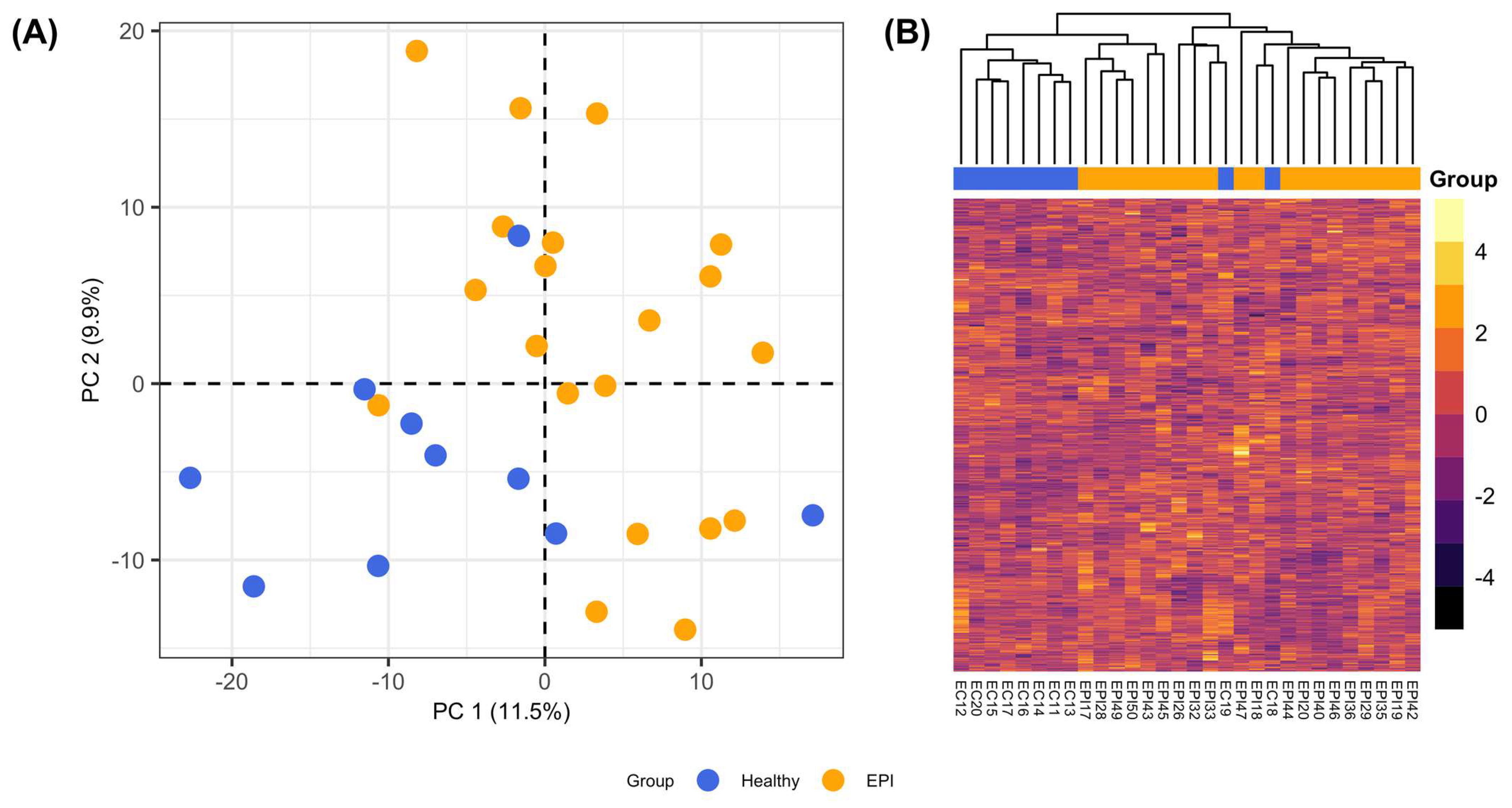
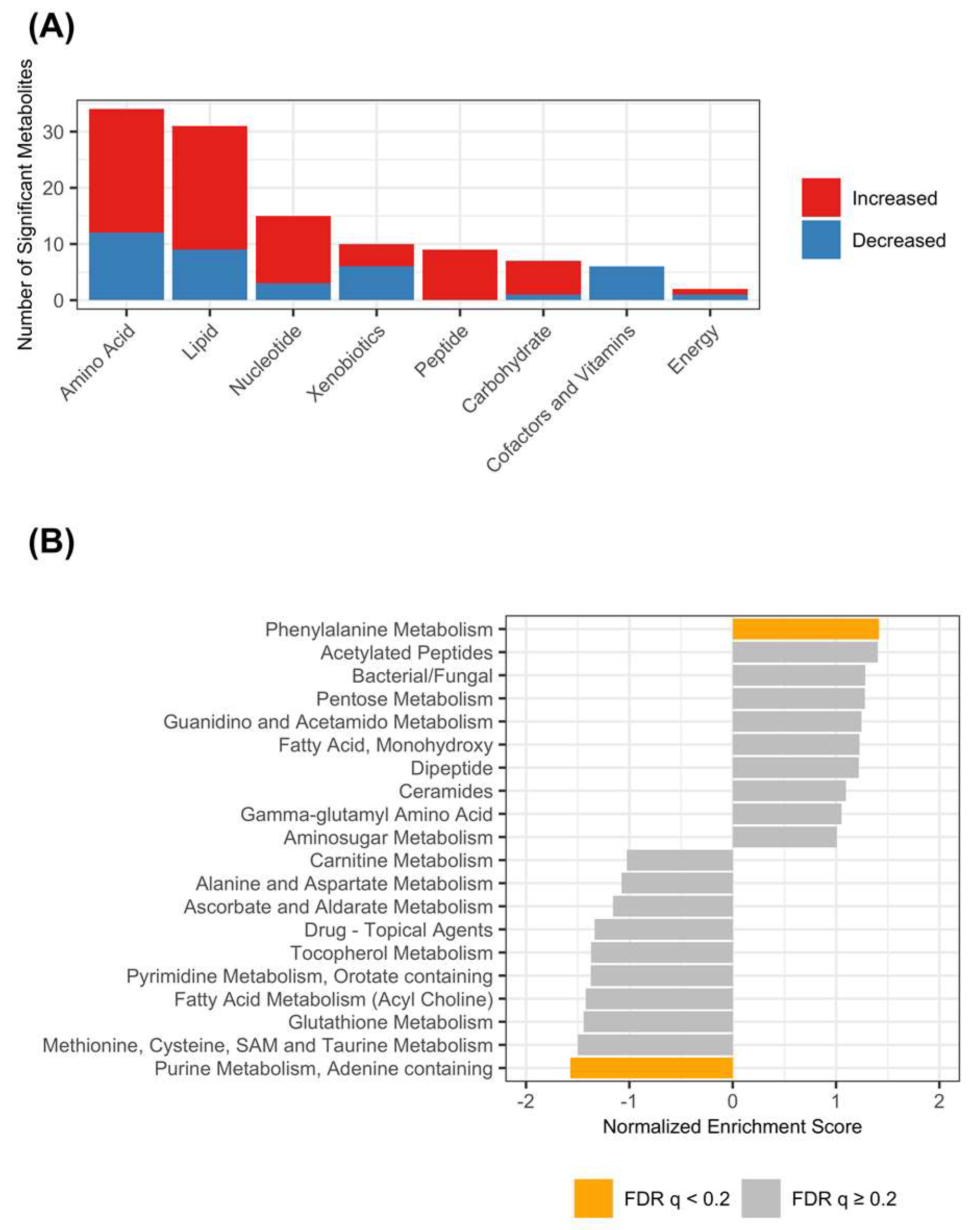
3.2. Untargeted Metabolomics Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Westermarck, E.; Wiberg, M. Exocrine Pancreatic Insufficiency in the Dog: Historical Background, Diagnosis, and Treatment. Top. Companion Anim. Med. 2012, 27, 96–103. [Google Scholar] [CrossRef]
- Batt, R.M. Exocrine Pancreatic Insufficiency. Vet. Clin. N. Am. Small Anim. Pract. 1993, 23, 595–608. [Google Scholar] [CrossRef]
- Barko, P.C.; Williams, D.A. Serum concentrations of lipid-soluble vitamins in dogs with exocrine pancreatic insufficiency treated with pancreatic enzymes. J. Vet. Intern. Med. 2018, 32, 1600–1608. [Google Scholar] [CrossRef]
- Soetart, N.; Rochel, D.; Drut, A.; Jaillardon, L. Serum cobalamin and folate as prognostic factors in canine exocrine pancreatic insufficiency: An observational cohort study of 299 dogs. Vet. J. 2019, 243, 15–20. [Google Scholar] [CrossRef]
- Chang, C.; Lidbury, J.A.; Suchodolski, J.S.; Steiner, J.M. Effect of oral or injectable supplementation with cobalamin in dogs with hypocobalaminemia caused by chronic enteropathy or exocrine pancreatic insufficiency. J. Vet. Intern. Med. 2022, 36, 1607–1621. [Google Scholar] [CrossRef]
- Wiberg, M.E.; Nurmi, A.-K.; Westermarck, E. Serum Trypsinlike Immunoreactivity Measurement for the Diagnosis of Subclinical Exocrine Pancreatic Insufficiency. J. Vet. Intern. Med. 1999, 13, 426–432. [Google Scholar] [CrossRef]
- Wiberg, M.E.; Westermarck, E. Subclinical exocrine pancreatic insufficiency in dogs. J. Am. Vet. Med. Assoc. 2002, 220, 1183–1187. [Google Scholar] [CrossRef]
- Wiberg, M. Pancreatic acinar atrophy in German shepherd dogs and rough-coated Collies. Etiopathogenesis, diagnosis and treatment. A review. Vet. Q. 2004, 26, 61–75. [Google Scholar] [CrossRef]
- Westermarck, E.; Batt, R.M.; Vaillant, C.; Wiberg, M. Sequential study of pancreatic structure and function during development of pancreatic acinar atrophy in a German shepherd dog. Am. J. Vet. Res. 1993, 54, 1088–1094. [Google Scholar]
- Williams, D.A.; Batt, R.M. Sensitivity and specificity of radioimmunoassay of serum trypsin-like immunoreactivity for the diagnosis of canine exocrine pancreatic insufficiency. J. Am. Vet. Med. Assoc. 1988, 192, 195–201. [Google Scholar]
- Williams, D.A.; Batt, R.M. Diagnosis of canine exocrine pancreatic insufficiency by the assay of serum trypsin-like immunoreactivity. J. Small Anim. Pract. 1983, 24, 583–588. [Google Scholar] [CrossRef]
- Batchelor, D.J.; Noble, P.-J.M.; Taylor, R.H.; Cripps, P.J.; German, A.J. Prognostic Factors in Canine Exocrine Pancreatic Insufficiency: Prolonged Survival is Likely if Clinical Remission is Achieved. J. Vet. Intern. Med. 2007, 21, 54–60. [Google Scholar] [CrossRef]
- German, A.J. Exocrine Pancreatic Insufficiency in the Dog: Breed Associations, Nutritional Considerations, and Long-term Outcome. Top. Companion Anim. Med. 2012, 27, 104–108. [Google Scholar] [CrossRef]
- Wiberg, M.; Lautala, H.; Westermarck, E. Response to long-term enzyme replacement treatment in dogs with exocrine pancreatic insufficiency—PubMed. J. Am. Vet. Med. Assoc. 1998, 213, 86–90. [Google Scholar]
- Wiberg, M.E.; Saari, S.A.; Westermarck, E.; Meri, S. Cellular and humoral immune responses in atrophic lymphocytic pancreatitis in German shepherd dogs and rough-coated collies. Vet. Immunol. Immunopathol. 2000, 76, 103–115. [Google Scholar] [CrossRef]
- Wiberg, M.E.; Saari, S.A.M.; Westermarck, E. Exocrine Pancreatic Atrophy in German Shepherd Dogs and Rough-coated Collies: An End Result of Lymphocytic Pancreatitis. Vet. Pathol. 1999, 36, 530–541. [Google Scholar] [CrossRef]
- Westermarck, E.; Saari, S.; Wiberg, M. Heritability of Exocrine Pancreatic Insufficiency in German Shepherd Dogs. J. Vet. Intern. Med. 2010, 24, 450–452. [Google Scholar] [CrossRef]
- Tsai, K.L.; Noorai, R.E.; Starr-Moss, A.N.; Quignon, P.; Rinz, C.J.; Ostrander, E.A.; Steiner, J.M.; Murphy, K.E.; Clark, L.A. Genome-wide association studies for multiple diseases of the German Shepherd Dog. Mamm. Genome 2011, 23, 203–211. [Google Scholar] [CrossRef]
- Evans, J.M.; Tsai, K.L.; Starr-Moss, A.N.; Steiner, J.M.; Clark, L.A. Association ofDLA-DQB1alleles with exocrine pancreatic insufficiency in Pembroke Welsh Corgis. Anim. Genet. 2015, 46, 462–465. [Google Scholar] [CrossRef]
- Tsai, K.L.; Starr-Moss, A.N.; Venkataraman, G.M.; Robinson, C.; Kennedy, L.J.; Steiner, J.M.; Clark, L.A. Alleles of the major histocompatibility complex play a role in the pathogenesis of pancreatic acinar atrophy in dogs. Immunogenetics 2013, 65, 501–509. [Google Scholar] [CrossRef]
- Wishart, D.S. Metabolomics for Investigating Physiological and Pathophysiological Processes. Physiol. Rev. 2019, 99, 1819–1875. [Google Scholar] [CrossRef]
- Sergushichev, A. Algorithm for cumulative calculation of gene set enrichment statistic. Sci. Technol. J. Inf. Technol. Mech. Opt. 2016, 16, 956. [Google Scholar] [CrossRef]
- Korotkevich, G.; Sukhov, V.; Budin, N.; Shpak, B.; Artyomov, M.N.; Sergushichev, A. Fast gene set enrichment analysis. bioRxiv 2021, 060012. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. Royal Statistical Soc. Ser. B Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Storey, J.D.; Bass, A.J.; Dabney, A.; Robinson, D. Qvalue: Q-Value Estimation for False Discovery Rate Control. 2020. Available online: http://github.com/jdstorey/qvalue (accessed on 28 June 2023).
- Hayashi, M.; Inagaki, A.; Novak, I.; Matsuda, H. The adenosine A2B receptor is involved in anion secretion in human pancreatic duct Capan-1 epithelial cells. Pflugers Arch. 2016, 468, 1171–1181. [Google Scholar] [CrossRef] [PubMed]
- Iwatsuki, K. Subtypes of adenosine receptors on pancreatic exocrine secretion in anaesthetized dogs. Fundam. Clin. Pharmacol. 2000, 14, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Hede, S.E.; Hansen, M.R. Adenosine receptors in rat and human pancreatic ducts stimulate chloride transport. Pflugers Arch. 2008, 456, 437–447. [Google Scholar] [CrossRef]
- Burnstock, G.; Novak, I. Purinergic signalling in the pancreas in health and disease. J. Endocrinol. 2012, 213, 123–141. [Google Scholar] [CrossRef]
- Hayashi, M. Expression of Adenosine Receptors in Rodent Pancreas. Int. J. Mol. Sci. 2019, 20, 5329. [Google Scholar] [CrossRef]
- Ye, J.H.; Rajendran, V.M. Adenosine: An immune modulator of inflammatory bowel diseases. World J. Gastroenterol. 2009, 15, 4491–4498. [Google Scholar] [CrossRef]
- Beloborodova, N.; Bairamov, I.; Olenin, A.; Shubina, V.; Teplova, V.; Fedotcheva, N. Effect of phenolic acids of microbial origin on production of reactive oxygen species in mitochondria and neutrophils. J. Biomed. Sci. 2012, 19, 89. [Google Scholar] [CrossRef]
- Li, X.; Jiang, B.; Pan, B.; Mu, W.; Zhang, T. Purification and Partial Characterization of Lactobacillus Species SK007 Lactate Dehydrogenase (LDH) Catalyzing Phenylpyruvic Acid (PPA) Conversion into Phenyllactic Acid (PLA). J. Agric. Food Chem. 2008, 56, 2392–2399. [Google Scholar] [CrossRef] [PubMed]
- Jia, J.; Mu, W.; Zhang, T.; Jiang, B. Bioconversion of Phenylpyruvate to Phenyllactate: Gene Cloning, Expression, and Enzymatic Characterization of d- and l1-Lactate Dehydrogenases from Lactobacillus plantarum SK002. Appl. Biochem. Biotechnol. 2010, 162, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Preidis, G.A.; Ajami, N.J.; Wong, M.C.; Bessard, B.C.; Conner, M.E.; Petrosino, J.F. Microbial-Derived Metabolites Reflect an Altered Intestinal Microbiota during Catch-Up Growth in Undernourished Neonatal Mice. J. Nutr. 2016, 146, 940–948. [Google Scholar] [CrossRef] [PubMed]
- Nierop Groot, M.N.; de Bont, J.A.M. Conversion of Phenylalanine to Benzaldehyde Initiated by an Aminotransferase in Lactobacillus plantarum. Appl. Environ. Microbiol. 1998, 64, 3009–3013. [Google Scholar] [CrossRef]
- Visconti, A.; Le Roy, C.I.; Rosa, F.; Rossi, N.; Martin, T.C.; Mohney, R.P.; Li, W.; de Rinaldis, E.; Bell, J.T.; Venter, J.C.; et al. Interplay between the human gut microbiome and host metabolism. Nat. Commun. 2019, 10, 4505. [Google Scholar] [CrossRef]
- Isaiah, A.; Parambeth, J.C.; Steiner, J.M.; Lidbury, J.A.; Suchodolski, J.S. The fecal microbiome of dogs with exocrine pancreatic insufficiency. Anaerobe 2017, 45, 50–58. [Google Scholar] [CrossRef]
- Dekkers, K.F.; Sayols-Baixeras, S.; Baldanzi, G.; Nowak, C.; Hammar, U.; Nguyen, D.; Varotsis, G.; Brunkwall, L.; Nielsen, N.; Eklund, A.C.; et al. An online atlas of human plasma metabolite signatures of gut microbiome composition. Nat. Commun. 2022, 13, 5370. [Google Scholar] [CrossRef]
- Yadav, M.; Lomash, A.; Kapoor, S.; Pandey, R.; Chauhan, N.S. Mapping of the benzoate metabolism by human gut microbiome indicates food-derived metagenome evolution. Sci. Rep. 2021, 11, 5561. [Google Scholar] [CrossRef]
- Williams, D.A.; Batt, R.M.; McLean, L. Bacterial overgrowth in the duodenum of dogs with exocrine pancreatic insufficiency. J. Am. Vet. Med. Assoc. 1987, 191, 201–206. [Google Scholar]
- Simpson, K.; Morton, D.; Sørensen, S.; McLEAN, L.; Riley, J.; Batt, R. Biochemical changes in the jejunal mucosa of dogs with exocrine pancreatic insufficiency following pancreatic duct ligation. Res. Vet. Sci. 1989, 47, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Simpson, K.W.; Batt, R.M.; Jones, D.; Morton, D.B. Effects of exocrine pancreatic insufficiency and replacement therapy on the bacterial flora of the duodenum in dogs. Am. J. Vet. Res. 1990, 51, 203–206. [Google Scholar] [PubMed]
- Blake, A.B.; Guard, B.C.; Honneffer, J.B.; Lidbury, J.A.; Steiner, J.M.; Suchodolski, J.S. Altered microbiota, fecal lactate, and fecal bile acids in dogs with gastrointestinal disease. PLoS ONE 2019, 14, e0224454. [Google Scholar] [CrossRef] [PubMed]
- Geever, E.F.; Seifter, E.; Levenson, S.M. Pancreatic pathology, chemically defined liquid diets and bacterial flora in the rat. Br. J. Exp. Pathol. 1970, 51, 341–347. [Google Scholar] [PubMed]
- Levenson, S.M.M.; Kan, D.M.; Gruber, C.B.; Crowley, L.B.; Jaffe, E.R.M.; Nakao, K.M.; Geever, E.F.M.; Seifter, E. Hemolytic Anemia and Pancreatic Acinar Atrophy and Fibrosis Conditioned by “Elemental” Liquid Diets and the Ordinary Intenstinal Microflora. Ann. Surg. 1971, 174, 469–510. [Google Scholar] [CrossRef]
- Kondoh, H.; Teruya, T.; Yanagida, M. Metabolomics of human fasting: New insights about old questions. Open Biol. 2020, 10, 200176. [Google Scholar] [CrossRef]
- Haq, S.; Grondin, J.A.; Khan, W.I. Tryptophan-derived serotonin-kynurenine balance in immune activation and intestinal inflammation. FASEB J. 2021, 35, e21888. [Google Scholar] [CrossRef]
- Gupta, N.K.; Thaker, A.I.; Kanuri, N.; Riehl, T.E.; Rowley, C.W.; Stenson, W.F.; Ciorba, M.A. Serum Analysis of Tryptophan Catabolism Pathway: Correlation with Crohn’s Disease Activity. Inflamm. Bowel Dis. 2012, 18, 1214–1220. [Google Scholar] [CrossRef]
- Sofia, M.A.; Ciorba, M.A.; Meckel, K.; Lim, C.K.; Guillemin, G.J.; Weber, C.R.; Bissonnette, M.; Pekow, J.R. Tryptophan Metabolism through the Kynurenine Pathway is Associated with Endoscopic Inflammation in Ulcerative Colitis. Inflamm. Bowel Dis. 2018, 24, 1471–1480. [Google Scholar] [CrossRef]
- Nikolaus, S.; Schulte, B.; Al-Massad, N.; Thieme, F.; Schulte, D.M.; Bethge, J.; Rehman, A.; Tran, F.; Aden, K.; Häsler, R.; et al. Increased Tryptophan Metabolism Is Associated with Activity of Inflammatory Bowel Diseases. Gastroenterology 2017, 153, 1504–1516. [Google Scholar] [CrossRef]
- Deng, P.; Jones, J.C.; Swanson, K.S. Effects of dietary macronutrient composition on the fasted plasma metabolome of healthy adult cats. Metabolomics 2013, 10, 638–650. [Google Scholar] [CrossRef]
- Lyu, Y.; Liu, D.; Nguyen, P.; Peters, I.; Heilmann, R.M.; Fievez, V.; Hemeryck, L.Y.; Hesta, M. Differences in Metabolic Profiles of Healthy Dogs Fed a High-Fat vs. a High-Starch Diet. Front. Vet. Sci. 2022, 9, 801863. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.D.; Compher, C.; Chen, E.Z.; Smith, S.A.; Shah, R.D.; Bittinger, K.; Chehoud, C.; Albenberg, L.G.; Nessel, L.; Gilroy, E.; et al. Comparative metabolomics in vegans and omnivores reveal constraints on diet-dependent gut microbiota metabolite production. Gut 2016, 65, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Puurunen, J.; Ottka, C.; Salonen, M.; Niskanen, J.E.; Lohi, H. Age, breed, sex and diet influence serum metabolite profiles of 2000 pet dogs. R. Soc. Open Sci. 2022, 9, 211642. [Google Scholar] [CrossRef]
- Yue, T.; Tan, H.; Shi, Y.; Xu, M.; Luo, S.; Weng, J.; Xu, S. Serum Metabolomic Profiling in Aging Mice Using Liquid Chromatography—Mass Spectrometry. Biomolecules 2022, 12, 1594. [Google Scholar] [CrossRef]
- Yu, Z.; Zhai, G.; Singmann, P.; He, Y.; Xu, T.; Prehn, C.; Römisch-Margl, W.; Lattka, E.; Gieger, C.; Soranzo, N.; et al. Human serum metabolic profiles are age dependent. Aging Cell 2012, 11, 960–967. [Google Scholar] [CrossRef]
- Ritz, S.; Hahn, D.; Wami, H.T.; Tegelkamp, K.; Dobrindt, U.; Schnekenburger, J. Gut microbiome as a response marker for pancreatic enzyme replacement therapy in a porcine model of exocrine pancreas insufficiency. Microb. Cell Factories 2020, 19, 221. [Google Scholar] [CrossRef]
- Whittemore, J.C.; Price, J.M.; Moyers, T.; Suchodolski, J.S. Effects of Synbiotics on the Fecal Microbiome and Metabolomic Profiles of Healthy Research Dogs Administered Antibiotics: A Randomized, Controlled Trial. Front. Vet. Sci. 2021, 8, 665713. [Google Scholar] [CrossRef]
- Stavroulaki, E.M.; Suchodolski, J.S.; Xenoulis, P.G. Effects of antimicrobials on the gastrointestinal microbiota of dogs and cats. Vet. J. 2023, 291, 105929. [Google Scholar] [CrossRef]
- Garcia-Mazcorro, J.F.; Suchodolski, J.S.; Jones, K.R.; Clark-Price, S.C.; Dowd, S.E.; Minamoto, Y.; Markel, M.; Steiner, J.M.; Dossin, O. Effect of the proton pump inhibitor omeprazole on the gastrointestinal bacterial microbiota of healthy dogs. FEMS Microbiol Ecol. 2012, 80, 624–636. [Google Scholar] [CrossRef]
| Healthy | EPI | p-Value | |
|---|---|---|---|
| Age (years) | 0.36 | ||
| Mean (SD) | 5.0 (± 1.74) | 4.3 (± 2.0) | |
| Breed | 0.62 | ||
| Akita | 0 (0%) | 1 (5%) | |
| Australian Shepherd | 0 (0%) | 2 (10%) | |
| Border Collie | 0 (0%) | 1 (5%) | |
| Cavalier King Charles Spaniels | 0 (0%) | 1 (5%) | |
| German Shepherd | 4 (40%) | 9 (45%) | |
| Labrador Retriever | 1 (10%) | 1 (5%) | |
| Mixed Breed | 4 (40%) | 4 (20%) | |
| Pit Bull Terrier | 1 (10%) | 0 (0%) | |
| West Highland White Terrier | 0 (0%) | 1 (5%) | |
| Sex | 0.16 | ||
| Spayed Female | 3 (30%) | 11 (55%) | |
| Intact Male | 0 (0%) | 2 (10%) | |
| Neutered Male | 7 (70%) | 7 (35%) | |
| Serum cTLI (RI: 5.7–45.2 µg/L) | <0.001 | ||
| Median (IQR) | 18.8 (15.7–29.1) | 1.0 (1.0–1.1) | |
| Serum cobalamin (RI: 251–908 ng/L) | 0.01 | ||
| Median (IQR) | 411 (297–593) | 231 (207–313) | |
| Serum folate (RI: 7.7–24.4 ng/L) | 0.39 | ||
| Mean (SD) | 12.1 (±5.2) | 13.9 (±4.5) |
| Biochemical | Subpathway | p-Value | q-Value | log2FC |
|---|---|---|---|---|
| Amino Acids | ||||
| Alpha-ketoglutaramate | Glutamate Metabolism | 0.001 | 0.019 | 0.99 |
| Cysteinylglycine Disulfide | Glutathione Metabolism | 0.001 | 0.023 | −1.31 |
| Cysteine-glutathione Disulfide | 0.003 | 0.043 | −0.93 | |
| 4-guanidinobutanoate | Guanidino and Acetamido Metabolism | 0.002 | 0.034 | 1.65 |
| Homocarnosine | Histidine Metabolism | 0.001 | 0.017 | 1.24 |
| 5-aminovalerate | Lysine Metabolism | 0.002 | 0.034 | 0.99 |
| N-acetyl-cadaverine | 0.001 | 0.024 | 1.19 | |
| Cystine | Methionine, Cysteine, s-Adenosylmethionine, and Taurine Metabolism | 0.000 | <0.001 | −2.29 |
| Phenyllactate | Phenylalanine Metabolism | <0.001 | 0.010 | 0.93 |
| Phenylpyruvate | <0.001 | 0.011 | 1.31 | |
| 4-hydroxyphenylacetate | <0.001 | 0.000 | 2.09 | |
| Phenol Sulfate | Tyrosine Metabolism | 0.003 | 0.042 | −1.93 |
| 4-hydroxyphenylpyruvate | 0.001 | 0.023 | 0.83 | |
| 4-hydroxyphenylacetatoylcarnitine | <0.001 | 0.001 | 3.61 | |
| Pro-hydroxy-pro | Urea cycle; Arginine and Proline Metabolism | 0.001 | 0.023 | −1.57 |
| Argininate | 0.001 | 0.014 | 0.66 | |
| 2-oxoarginine | <0.001 | 0.001 | 2.44 | |
| Carbohydrates | ||||
| 1,5-anhydroglucitol | Glycolysis, Gluconeogenesis, and Pyruvate Metabolism | <0.001 | 0.006 | −0.73 |
| Glycerate | <0.001 | 0.001 | 1.03 | |
| Ribose | Pentose Metabolism | <0.001 | <0.001 | 1.97 |
| Cofactors and Vitamins | ||||
| Threonate | Ascorbate and Aldarate Metabolism | <0.001 | 0.002 | −0.98 |
| Alpha-CEHC Sulfate | Tocopherol Metabolism | <0.001 | 0.010 | −2.03 |
| Pyridoxal | Vitamin B6 Metabolism | 0.002 | 0.028 | −0.79 |
| Lipids | ||||
| 2-hydroxydecanoate | Fatty Acid, Monohydroxy | 0.001 | 0.023 | 1.48 |
| 1-arachidonoyl-GPA (20:4) | Lysophospholipid | <0.001 | 0.008 | 1.02 |
| 1-oleoyl-GPA (18:1) | <0.001 | <0.001 | 2.27 | |
| 1-palmitoyl-GPA (16:0) | <0.001 | <0.001 | 2.38 | |
| Heptanoate (7:0) | Medium Chain Fatty Acid | 0.003 | 0.046 | 0.80 |
| Choline | Phospholipid Metabolism | <0.001 | 0.001 | 0.62 |
| 1-(1-enyl-palmitoyl)-2-oleoyl-GPE (P-16:0/18:1) | Plasmalogen | <0.001 | 0.006 | 0.81 |
| 1-(1-enyl-stearoyl)-2-oleoyl-GPE (P-18:0/18:1) | <0.001 | 0.011 | 0.92 | |
| Sphingomyelin (d18:1/25:0, d19:0/24:1, d20:1/23:0, d19:1/24:0) | Sphingolipid Metabolism | 0.001 | 0.020 | −1.02 |
| Sphingomyelin (d18:1/14:0, d16:1/16:0) | 0.001 | 0.025 | 0.65 | |
| Nucleotides | ||||
| Xanthine | Purine Metabolism, (Hypo)Xanthine/Inosine-containing | <0.001 | 0.001 | 1.53 |
| Adenosine 5′-monophosphate | Purine Metabolism, Adenine-containing | <0.001 | 0.001 | −2.89 |
| Adenosine | <0.001 | 0.004 | −2.45 | |
| Dihydroorotate | Pyrimidine Metabolism, Orotate-containing | <0.001 | 0.001 | −1.17 |
| Uracil | Pyrimidine Metabolism, Uracil-containing | <0.001 | 0.008 | 1.33 |
| Peptides | ||||
| 4-hydroxyphenylacetylglutamine | Acetylated Peptides | <0.001 | 0.001 | 1.93 |
| Phenylacetylthreonine | 0.002 | 0.028 | 1.96 | |
| 4-hydroxyphenylacetylglycine | 0.000 | 0.001 | 2.10 | |
| Leucylglutamine | Dipeptide | 0.001 | 0.024 | 1.90 |
| Xenobiotics | ||||
| Tartronate (hydroxymalonate) | Bacterial/Fungal | <0.001 | 0.008 | 0.94 |
| Perfluorooctanesulfonic Acid | Chemical | 0.002 | 0.034 | −2.11 |
| S-(3-hydroxypropyl)mercapturic Acid | 0.001 | 0.026 | 0.76 | |
| Hydroquinone Sulfate | Drug–Topical Agents | 0.002 | 0.028 | −1.86 |
| Quinate | Food Component/Plant | <0.001 | 0.006 | 3.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barko, P.C.; Rubin, S.I.; Swanson, K.S.; McMichael, M.A.; Ridgway, M.D.; Williams, D.A. Untargeted Analysis of Serum Metabolomes in Dogs with Exocrine Pancreatic Insufficiency. Animals 2023, 13, 2313. https://doi.org/10.3390/ani13142313
Barko PC, Rubin SI, Swanson KS, McMichael MA, Ridgway MD, Williams DA. Untargeted Analysis of Serum Metabolomes in Dogs with Exocrine Pancreatic Insufficiency. Animals. 2023; 13(14):2313. https://doi.org/10.3390/ani13142313
Chicago/Turabian StyleBarko, Patrick C., Stanley I. Rubin, Kelly S. Swanson, Maureen A. McMichael, Marcella D. Ridgway, and David A. Williams. 2023. "Untargeted Analysis of Serum Metabolomes in Dogs with Exocrine Pancreatic Insufficiency" Animals 13, no. 14: 2313. https://doi.org/10.3390/ani13142313
APA StyleBarko, P. C., Rubin, S. I., Swanson, K. S., McMichael, M. A., Ridgway, M. D., & Williams, D. A. (2023). Untargeted Analysis of Serum Metabolomes in Dogs with Exocrine Pancreatic Insufficiency. Animals, 13(14), 2313. https://doi.org/10.3390/ani13142313







