Pre-Treatment of Swine Oviductal Epithelial Cells with Progesterone Increases the Sperm Fertilizing Ability in an IVF Model
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. SOECs Collection and Incubation
2.3. Cell Population Doubling Time
2.4. Phalloidin Staining
2.5. Tubulin Immunocytochemistry
2.6. Confocal Analysis of SOECr
2.7. Preparation and Incubation of Sperm Samples
2.8. In Vitro Fertilization
2.9. Gene Expression Analysis
2.10. Statistical Analysis
3. Results and Discussion
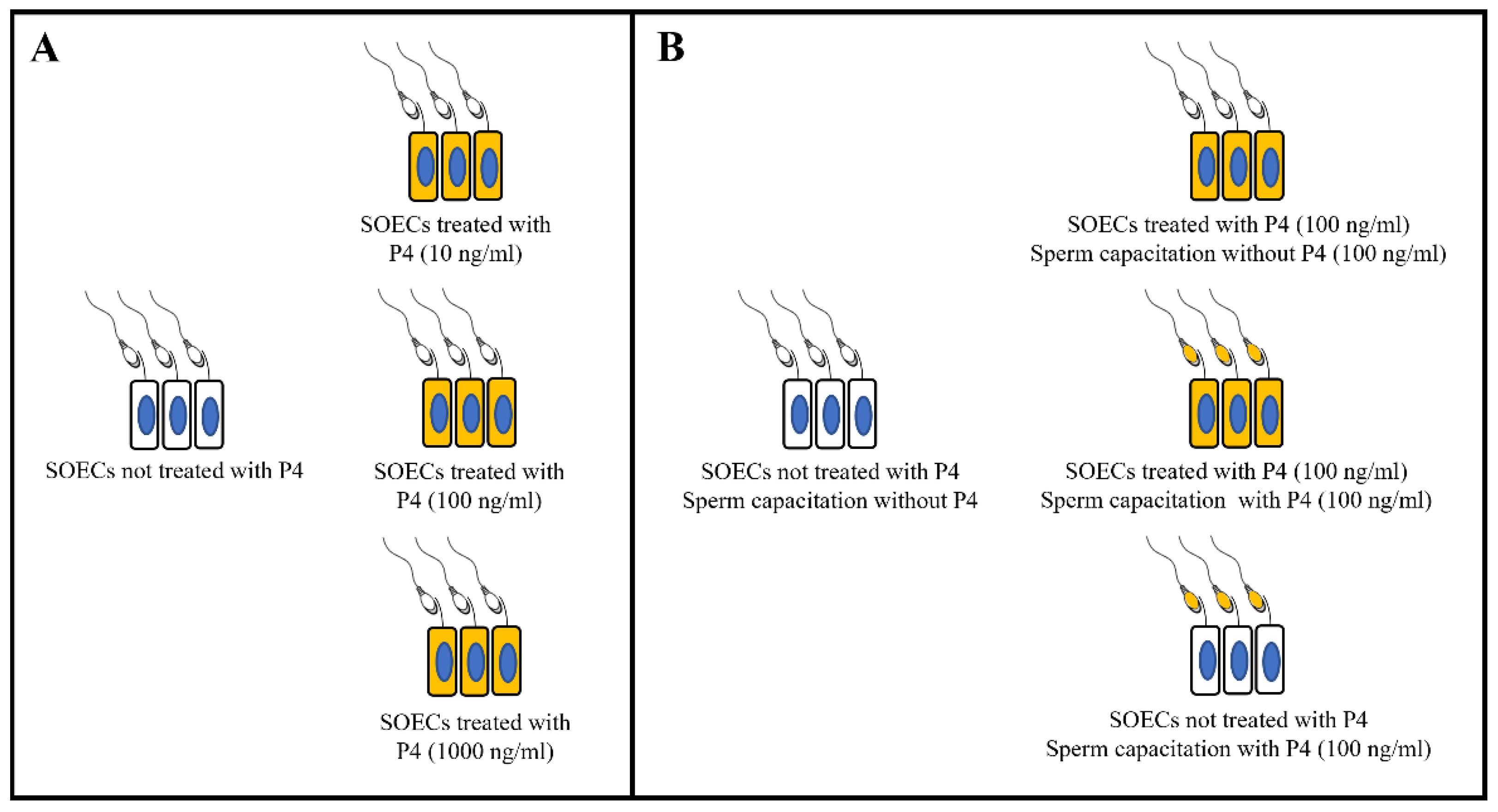
- Once the most favourable P4 concentration (100 ng/mL) was identified, we performed the comparison with further experimental conditions of interest (as shown in Figure 1B) to evaluate the sperm fertilizing ability, both with the SOECs treatment with or without P4 (100 ng/mL) and the addition or not of P4 (100 ng/mL) during capacitation.
3.1. P4 Supplementation Does Not Affect the Cells Growing Rate
3.2. P4 Supplementation Does Not Modify the SOECs Cytoskeleton
3.3. Sperm Capacitation on SOECs Previously Supplemented with P4 100 ng/mL Significantly Increases the IVF Outcomes
3.4. Pre-Treatment of SOECs with P4 but Not Sperm Capacitation Supplementation Improves IVF Outcomes
3.5. P4 Induces a Downregulation of the Expression of OVGP1, SPP1 and DMBT1 Genes
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mascarenhas, M.N.; Flaxman, S.R.; Boerma, T.; Vanderpoel, S.; Stevens, G.A. National, Regional, and Global Trends in Infertility Prevalence Since 1990: A Systematic Analysis of 277 Health Surveys. PLoS Med. 2012, 9, e1001356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boivin, J.; Bunting, L.; Collins, J.A.; Nygren, K.G. International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum. Reprod. 2007, 22, 1506–1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ardon, F.; Markello, R.D.; Hu, L.; Deutsch, Z.I.; Tung, C.-K.; Wu, M.; Suarez, S.S. Dynamics of Bovine Sperm Interaction with Epithelium Differ Between Oviductal Isthmus and Ampulla. Biol. Reprod. 2016, 95, 90. [Google Scholar] [CrossRef] [PubMed]
- Suarez, S.S. Mammalian sperm interactions with the female reproductive tract. Cell Tissue Res. 2016, 363, 185–194. [Google Scholar] [CrossRef] [Green Version]
- Tienthai, P. The porcine sperm reservoir in relation to the function of hyaluronan. J. Reprod. Dev. 2015, 61, 245–250. [Google Scholar] [CrossRef] [Green Version]
- Ellington, J.E.; Samper, J.C.; Jones, A.E.; Oliver, S.A.; Burnett, K.M.; Wright, R.W. In vitro interactions of cryopreserved stallion spermatozoa and oviduct (uterine tube) epithelial cells or their secretory products. Anim. Reprod. Sci. 1999, 56, 51–65. [Google Scholar] [CrossRef]
- Yeste, M.; Lloyd, R.E.; Badia, E.; Briz, M.; Bonet, S.; Holt, W.V. Direct contact between boar spermatozoa and porcine oviductal epithelial cell (OEC) cultures is needed for optimal sperm survival in vitro. Anim. Reprod. Sci. 2009, 113, 263–278. [Google Scholar] [CrossRef]
- Tuckey, R.C. Progesterone synthesis by the human placenta. Placenta 2005, 26, 273–281. [Google Scholar] [CrossRef]
- Miller, W.L.; Bose, H.S. Early steps in steroidogenesis: Intracellular cholesterol trafficking. J. Lipid Res. 2011, 52, 2111–2135. [Google Scholar] [CrossRef] [Green Version]
- Taraborrelli, S. Physiology, production and action of progesterone. Acta Obstet. Gynecol. Scand. 2015, 94, 8–16. [Google Scholar] [CrossRef]
- Einer-Jensen, N.; Hunter, R.H.F. Counter-current transfer in reproductive biology. Reproduction 2005, 129, 9–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fujinoki, M.; Takei, G.L.; Kon, H. Non-genomic regulation and disruption of spermatozoal in vitro hyperactivation by oviductal hormones. J. Physiol. Sci. 2016, 66, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Lishko, P.V.; Botchkina, I.L.; Kirichok, Y. Progesterone activates the principal Ca2+ channel of human sperm. Nature 2011, 471, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Teves, M.E.; Barbano, F.; Guidobaldi, H.A.; Sanchez, R.; Miska, W.; Giojalas, L.C. Progesterone at the picomolar range is a chemoattractant for mammalian spermatozoa. Fertil. Steril. 2006, 86, 745–749. [Google Scholar] [CrossRef]
- Guidobaldi, H.A.; Teves, M.E.; Uñates, D.R.; Anastasía, A.; Giojalas, L.C. Progesterone from the Cumulus Cells Is the Sperm Chemoattractant Secreted by the Rabbit Oocyte Cumulus Complex. PLoS ONE 2008, 3, e3040. [Google Scholar] [CrossRef] [PubMed]
- Bronson, R.A.; Peresleni, T.; Golightly, M. Progesterone promotes the acrosome reaction in capacitated human spermatozoa as judged by flow cytometry and CD46 staining. Mol. Hum. Reprod. 1999, 5, 507–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldi, E.; Luconi, M.; Muratori, M.; Marchiani, S.; Tamburrino, L.; Forti, G. Nongenomic activation of spermatozoa by steroid hormones: Facts and fictions. Mol. Cell. Endocrinol. 2009, 308, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Foresta, C.; Rossato, M.; Mioni, R.; Zorzi, M. Progesterone induces capacitation in human spermatozoa. Andrologia 2009, 24, 33–35. [Google Scholar] [CrossRef]
- López-Torres, A.S.; Chirinos, M. Modulation of Human Sperm Capacitation by Progesterone, Estradiol, and Luteinizing Hormone. Reprod. Sci. 2017, 24, 193–201. [Google Scholar] [CrossRef]
- Chen, S.; Einspanier, R.; Schoen, J. In vitro mimicking of estrous cycle stages in porcine oviduct epithelium cells: Estradiol and progesterone regulate differentiation, gene expression, and cellular function. Biol. Reprod. 2013, 89, 54. [Google Scholar] [CrossRef]
- Pérez-Cerezales, S.; Ramos-Ibeas, P.; Acuna, O.S.; Avilés, M.; Coy, P.; Rizos, D.; Gutieŕrez-Adán, A. The oviduct: From sperm selection to the epigenetic landscape of the embryo. Biol. Reprod. 2018, 98, 262–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Hagen, D.E.; Ji, T.; Bakhtiarizadeh, M.R.; Frederic, W.M.; Traxler, E.M.; Kalish, J.M.; Rivera, R.M. Altered microRNA expression profiles in large offspring syndrome and Beckwith-Wiedemann syndrome. Epigenetics 2019, 14, 850–876. [Google Scholar] [CrossRef] [PubMed]
- Grace, K.S.; Sinclair, K.D. Assisted reproductive technology, epigenetics, and long-term health: A developmental time bomb still ticking. Semin. Reprod. Med. 2009, 27, 409–416. [Google Scholar] [CrossRef] [PubMed]
- La Rovere, M.; Franzago, M.; Stuppia, L. Epigenetics and Neurological Disorders in ART. Int. J. Mol. Sci. 2019, 20, 4169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ludwig, M.; Katalinic, A.; Groß, S.; Sutcliffe, A.; Varon, R.; Horsthemke, B. Increased prevalence of imprinting defects in patients with Angelman syndrome born to subfertile couples. J. Med. Genet. 2005, 42, 289–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eroglu, A.; Layman, L.C. Role of ART in Imprinting Disorders. Semin. Reprod. Med. 2007, 83, 255–262. [Google Scholar] [CrossRef] [Green Version]
- Soriano-Úbeda, C.; Avilés-López, K.; García-Vázquez, F.A.; Romero-Aguirregomezcorta, J.; Matás, C. Epididymal and ejaculated sperm functionality is regulated differently by periovulatory oviductal fluid in pigs. Andrology 2021, 9, 426–439. [Google Scholar] [CrossRef]
- París-Oller, E.; Navarro-Serna, S.; Soriano-Úbeda, C.; Lopes, J.S.; Matás, C.; Ruiz, S.; Latorre, R.; López-Albors, O.; Romar, R.; Cánovas, S.; et al. Reproductive fluids, used for the in vitro production of pig embryos, result in healthy offspring and avoid aberrant placental expression of PEG3 and LUM. J. Anim. Sci. Biotechnol. 2021, 12, 32. [Google Scholar] [CrossRef]
- Ferraz, M.A.M.M.; Henning, H.H.W.; Costa, P.F.; Malda, J.; Melchels, F.P.; Wubbolts, R.; Stout, T.A.E.; Vos, P.L.A.M.; Gadella, B.M. Improved bovine embryo production in an oviduct-on-a-chip system: Prevention of poly-spermic fertilization and parthenogenic activation. Lab Chip 2017, 17, 905–916. [Google Scholar] [CrossRef] [Green Version]
- Lamy, J.; Corbin, E.; Blache, M.C.; Garanina, A.S.; Uzbekov, R.; Mermillod, P.; Saint-Dizier, M. Steroid hormones regulate sperm–oviduct interactions in the bovine. Reproduction 2017, 154, 497–508. [Google Scholar] [CrossRef] [Green Version]
- Ramal-Sanchez, M.; Bernabo, N.; Tsikis, G.; Blache, M.C.; Labas, V.; Druart, X.; Mermillod, P.; Saint-Dizier, M. Progesterone induces sperm release from oviductal epithelial cells by modifying sperm proteomics, lipidomics and membrane fluidity. Mol. Cell. Endocrinol. 2020, 504, 110723. [Google Scholar] [CrossRef] [PubMed]
- Romero-Aguirregomezcorta, J.; Cronin, S.; Donnellan, E.; Fair, S. Progesterone induces the release of bull spermatozoa from oviductal epithelial cells. Reprod. Fertil. Dev. 2019, 31, 1463–1472. [Google Scholar] [CrossRef] [PubMed]
- Maccarrone, M.; Barboni, B.; Paradisi, A.; Bernabò, N.; Gasperi, V.; Pistilli, M.G.; Fezza, F.; Lucidi, P.; Mattioli, M. Characterization of the endocannabinoid system in boar spermatozoa and implications for sperm capacitation and acrosome reaction. J. Cell Sci. 2005, 118, 4393–4404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernabò, N.; Machado-simoes, J.; Valbonetti, L.; Ramal-sanchez, M.; Capacchietti, G.; Fontana, A.; Zappacosta, R.; Palestini, P.; Botto, L.; Marchisio, M.; et al. Graphene Oxide increases mammalian spermatozoa fertilizing ability by extracting cholesterol from their membranes and promoting capacitation. Sci. Rep. 2019, 9, 8155. [Google Scholar] [CrossRef]
- Bernabò, N.; Fontana, A.; Sanchez, M.R.; Valbonetti, L.; Capacchietti, G.; Zappacosta, R.; Greco, L.; Marchisio, M.; Lanuti, P.; Ercolino, E.; et al. Graphene oxide affects in vitro fertilization outcome by interacting with sperm membrane in an animal model. Carbon N. Y. 2018, 129, 428–437. [Google Scholar] [CrossRef]
- Bernabò, N.; Tettamanti, E.; Pistilli, M.G.; Nardinocchi, D.; Berardinelli, P.; Mattioli, M.; Barboni, B. Effects of 50 Hz extremely low frequency magnetic field on the morphology and function of boar spermatozoa capacitated in vitro. Theriogenology 2007, 67, 801–815. [Google Scholar] [CrossRef]
- Abeydeera, L.R.; Day, B.N. Fertilization and subsequent development in vitro of pig oocytes inseminated in a modified Tris-buffered medium with frozen-thawed ejaculated spermatozoa. Biol. Reprod. 1997, 57, 729–734. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Einspanier, R.; Schoen, J. Long-term culture of primary porcine oviduct epithelial cells: Validation of a comprehensive invitro model for reproductive science. Theriogenology 2013, 80, 862–869. [Google Scholar] [CrossRef] [Green Version]
- Thornton, B.; Basu, C. Real-time PCR (qPCR) primer design using free online software. Biochem. Mol. Biol. Educ. 2011, 39, 145–154. [Google Scholar] [CrossRef]
- Bernabò, N.; Valbonetti, L.; Raspa, M.; Fontana, A.; Palestini, P.; Botto, L.; Paoletti, R.; Fray, M.; Allen, S.; Machado-Simoes, J.; et al. Graphene Oxide Improves in vitro Fertilization in Mice with No Impact on Embryo Development and Preserves the Membrane Microdomains Architecture. Front. Bioeng. Biotechnol. 2020, 8, 629. [Google Scholar] [CrossRef]
- Oraiopoulou, M.E.; Tzamali, E.; Tzedakis, G.; Vakis, A.; Papamatheakis, J.; Sakkalis, V. In Vitro/In silico study on the role of doubling time heterogeneity among primary glioblastoma cell lines. Biomed Res. Int. 2017, 2017, 8569328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korzyńska, A.; Zychowicz, M. A method of estimation of the cell doubling time on basis of the cell culture monitoring data. Biocybern. Biomed. Eng. 2008, 28, 75–82. [Google Scholar]
- Lindström, H.J.G.; Friedman, R. Inferring time-dependent population growth rates in cell cultures undergoing adaptation. BMC Bioinform. 2020, 21, 583. [Google Scholar] [CrossRef] [PubMed]
- Tzur, A.; Kafri, R.; LeBleu, V.S.; Lahav, G.; Kirschner, M.W. Cell Growth and Size Homeostasis in Proliferating Animal Cells. Science 2009, 325, 167. [Google Scholar] [CrossRef] [Green Version]
- Sun, B.; Fang, Y.; Li, Z.; Chen, Z.; Xiang, J. Role of cellular cytoskeleton in epithelial-mesenchymal transition process during cancer progression. Biomed. Rep. 2015, 3, 603–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tojkander, S.; Gateva, G.; Lappalainen, P. Actin stress fibers-Assembly, dynamics and biological roles. J. Cell Sci. 2012, 125, 1855–1864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Svitkina, T. The Actin Cytoskeleton and Actin-Based Motility. Cold Spring Harb. Perspect. Biol. 2018, 10, a018267. [Google Scholar] [CrossRef] [Green Version]
- Goodson, H.V.; Jonasson, E.M. Microtubules and Microtubule-Associated Proteins. Cold Spring Harb. Perspect. Biol. 2018, 10, a022608. [Google Scholar] [CrossRef]
- Etienne-Manneville, S. Actin and Microtubules in Cell Motility: Which One is in Control? Traffic 2004, 5, 470–477. [Google Scholar] [CrossRef]
- Parker, A.L.; Kavallaris, M.; McCarroll, J.A. Microtubules and their role in cellular stress in cancer. Front. Oncol. 2014, 4, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-Lasso, D.C.; Romá-Mateo, C.; Pallardó, F.V.; Gonzalez-Cabo, P. Much More Than a Scaffold: Cytoskeletal Proteins in Neurological Disorders. Cells 2020, 9, 358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magliocca, V.; Petrini, S.; Franchin, T.; Borghi, R.; Niceforo, A.; Abbaszadeh, Z.; Bertini, E.; Compagnucci, C. Identifying the dynamics of actin and tubulin polymerization in iPSCs and in iPSC-derived neurons. Oncotarget 2017, 8, 111096–111109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suarez, S.S.; Pacey, A.A. Sperm transport in the female reproductive tract. Hum. Reprod. Update 2006, 12, 23–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, D.J. Review: The epic journey of sperm through the female reproductive tract. Animal 2018, 12, s110–s120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reshi, Q.U.A.; Viil, J.; Ord, J.; Lättekivi, F.; Godakumara, K.; Hasan, M.M.; Nõmm, M.; Jääger, K.; Velthut-Meikas, A.; Jaakma, Ü.; et al. Spermatozoa induce transcriptomic alterations in bovine oviductal epithelial cells prior to initial contact. J. Cell Commun. Signal. 2020, 14, 439–451. [Google Scholar] [CrossRef]
- Mahé, C.; Zlotkowska, A.M.; Reynaud, K.; Tsikis, G.; Mermillod, P.; Druart, X.; Schoen, J.; Saint-Dizier, M. Sperm migration, selection, survival, and fertilizing ability in the mammalian oviduct. Biol. Reprod. 2021, 105, 317–331. [Google Scholar] [CrossRef]
- Chang, H.; Suarez, S.S. Unexpected flagellar movement patterns and epithelial binding behavior of mouse sperm in the oviduct. Biol. Reprod. 2012, 86, 140. [Google Scholar] [CrossRef]
- Gualtieri, R.; Talevi, R. In vitro-cultured bovine oviductal cells bind acrosome-intact sperm and retain this ability upon sperm release. Biol. Reprod. 2000, 62, 1754–1762. [Google Scholar] [CrossRef] [Green Version]
- Fazeli, A.; Elliott, R.M.A.; Duncan, A.E.; Moore, A.; Watson, P.F.; Holt, W.V. In Vitro Maintenance of Boar Sperm Viability by a Soluble Fraction Obtained from Oviductal Apical Plasma Membrance Prepations. Available online: https://pubmed.ncbi.nlm.nih.gov/12683921/ (accessed on 23 November 2021).
- Coy, P.; García-Vázquez, F.A.; Visconti, P.E.; Avilés, M. Roles of the oviduct in mammalian fertilization. Reproduction 2012, 144, 649–660. [Google Scholar] [CrossRef] [Green Version]
- Hunter, R.H.F.; Petersen, H.H.; Greve, T. Ovarian follicular fluid, progesterone and Ca2+ ion influences on sperm release from the Fallopian tube reservoir. Mol. Reprod. Dev. 1999, 54, 283–291. [Google Scholar] [CrossRef]
- Gervasi, M.G.; Osycka-Salut, C.; Sanchez, T.; Alonso, C.A.I.; Llados, C.; Castellano, L.; Franchi, A.M.; Villalõn, M.; Perez-Martinez, S. Sperm Release From the Oviductal Epithelium Depends on Ca(2+) Influx Upon Activation of CB1 and TRPV1 by Anandamide. J. Cell. Biochem. 2016, 117, 320–333. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Saito, Y.; Kagawa, N.; Yang, X. In vitro fertilization and polyspermy in the pig: Factors affecting fertilization rates and cytoskeletal reorganization of the oocyte. Microsc. Res. Tech. 2003, 61, 327–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abeydeera, L.R.; Funahashi, H.; Kim, N.H.; Day, B.N. Chlortetracycline fluorescence patterns and in vitro fertilisation of frozen-thawed boar spermatozoa incubated under various bicarbonate concentrations. Zygote 1997, 5, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Hunter, R.H.F.; Nichol, R. Capacitation potential of the fallopian tube: A study involving surgical insemination and the subsequent incidence of polyspermy. Gamete Res. 1988, 21, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Almiñana, C.; Tsikis, G.; Labas, V.; Uzbekov, R.; Silveira, J.C.; Bauersachs, S.; Mermillod, P. Deciphering the oviductal extracellular vesicles content across the estrous cycle: Implications for the gametes-oviduct interactions and the environment of the potential embryo. BMC Genom. 2018, 19, 622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franchi, A.; Moreno-Irusta, A.; Domínguez, E.M.; Adre, A.J.; Giojalas, L.C. Extracellular vesicles from oviductal isthmus and ampulla stimulate the induced acrosome reaction and signaling events associated with capacitation in bovine spermatozoa. J. Cell. Biochem. 2019, 121, 2877–2888. [Google Scholar] [CrossRef] [PubMed]
- Asaadi, A.; Dolatabad, N.A.; Atashi, H.; Raes, A.; van Damme, P.; Hoelker, M.; Hendrix, A.; Pascottini, O.B.; Van Soom, A.; Kafi, M.; et al. Extracellular vesicles from follicular and ampullary fluid isolated by density gradient ultracentrifugation improve bovine embryo development and quality. Int. J. Mol. Sci. 2021, 22, 578. [Google Scholar] [CrossRef]
- Coy, P.; Yanagimachi, R. The Common and Species-Specific Roles of Oviductal Proteins in Mammalian Fertilization and Embryo Development. Bioscience 2015, 65, 973–984. [Google Scholar] [CrossRef] [Green Version]
- Choudhary, S.; Janjanam, J.; Kumar, S.; Kaushik, J.K.; Mohanty, A.K. Structural and functional characterization of buffalo oviduct-specific glycoprotein (OVGP1) expressed during estrous cycle. Biosci. Rep. 2019, 39, BSR20191501. [Google Scholar] [CrossRef] [Green Version]
- Algarra, B.; Han, L.; Soriano-Úbeda, C.; Avilés, M.; Coy, P.; Jovine, L.; Jiménez-Movilla, M. The C-terminal region of OVGP1 remodels the zona pellucida and modifies fertility parameters. Sci. Rep. 2016, 6, 32556. [Google Scholar] [CrossRef] [Green Version]
- Lamy, J.; Nogues, P.; Combes-Soia, L.; Tsikis, G.; Labas, V.; Mermillod, P.; Druart, X.; Saint-Dizier, M. Identification by proteomics of oviductal sperm-interacting proteins. Reproduction 2018, 155, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhao, Y.; Yang, X.; Kan, F.W.K. Recombinant hamster oviductin is biologically active and exerts positive effects on sperm functions and sperm-oocyte binding. PLoS ONE 2015, 10, e0123003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalves, R.F.; Wolinetz, C.D.; Killian, G.J. Influence of arginine-glycine-aspartic acid (RGD), integrins (αV and α5) and osteopontin on bovine sperm-egg binding, and fertilization in vitro. Theriogenology 2007, 67, 468–474. [Google Scholar] [CrossRef] [PubMed]
- Gabler, C.; Chapman, D.A.; Killian, G.J. Expression and presence of osteopontin and integrins in the bovine oviduct during the oestrous cycle. Reproduction 2003, 126, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.X.; Denhardt, D.T. Osteopontin: Role in immune regulation and stress responses. Cytokine Growth Factor Rev. 2008, 19, 333–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madsen, J.; Sorensen, G.L.; Nielsen, O.; Tornøe, I.; Thim, L.; Fenger, C.; Mollenhauer, J.; Holmskov, U. A Variant Form of the Human Deleted in Malignant Brain Tumor 1 (DMBT1) Gene Shows Increased Expression in Inflammatory Bowel Diseases and Interacts with Dimeric Trefoil Factor 3 (TFF3). PLoS ONE 2013, 8, e64441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, H.S.; Kim, B.C.; Yeo, H.Y.; Kim, K.H.; Yoo, B.C.; Park, J.W.; Chang, H.J. Deleted in malignant brain tumor 1 is a novel prognostic marker in colorectal cancer. Oncol. Rep. 2018, 39, 2279–2287. [Google Scholar] [CrossRef] [PubMed]
- Müller, H.; Nagel, C.; Weiss, C.; Mollenhauer, J.; Poeschl, J. Deleted in malignant brain tumors 1 (DMBT1) elicits increased VEGF and decreased IL-6 production in type II lung epithelial cells. BMC Pulm. Med. 2015, 15, 32. [Google Scholar] [CrossRef] [Green Version]
- Neville, M.C.; Zhang, P. Lactoferrin secretion into milk: Comparison between ruminant, murine, and human milk. J. Anim. Sci. 2000, 78, 26. [Google Scholar] [CrossRef]
- Ambruosi, B.; Accogli, G.; Douet, C.; Canepa, S.; Pascal, G.; Monget, P.; Moros, C.; Holmskov, U.; Mollenhauer, J.; Robbe-Masselot, C.; et al. Deleted in malignant brain tumor 1 is secreted in the oviduct and involved in the mechanism of fertilization in equine and porcine species. Reproduction 2013, 146, 119–133. [Google Scholar] [CrossRef]
- Roldán, M.L.; Marini, P.E. First evidence of the interaction between deleted in malignant brain tumor 1 and galectin-3 in the mammalian oviduct. Histochem. Cell Biol. 2014, 141, 181–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saint-Dizier, M.; Schoen, J.; Chen, S.; Banliat, C.; Mermillod, P. Composing the early embryonic microenvironment: Physiology and regulation of oviductal secretions. Int. J. Mol. Sci. 2020, 21, 223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valero, A.; Roldán, M.L.; Ruiz, M.F.; Teijeiro, J.M.; Marquez, S.B.; Marini, P.E. Deleted in Malignant Brain Tumor 1 (DMBT1) Expression Pattern in Normal Cervix and at Different Stages of Squamous Intraepithelial Lesions. Open Biomark. J. 2018, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Liu, Q.; Xie, Q.Z.; Zhou, Y.; Yang, J. Osteopontin is expressed in the oviduct and promotes fertilization and preimplantation embryo development of mouse. Zygote 2014, 760. [Google Scholar] [CrossRef] [PubMed]
- Briton-Jones, C.; Hung Lok, I.; Mo Yuen, P.; Tak Yu Chiu, T.; Ping Cheung, L.; Haines, C. Regulation of human oviductin mRNA expression in vivo. Fertil. Steril. 2001, 75, 942–946. [Google Scholar] [CrossRef]





| Gene Symbol | Primer Sequence (5′–3′) | Fragment Size (bp) | Anneling Temperature (°C) | References |
|---|---|---|---|---|
| GAPDH | Forward: ATTCCACCCACGGCAAGTTC | |||
| Reverse: AAGGGGCAGAGATGATGACC | 225 | 60 | [38] | |
| OVGP1 | Forward: TACTTGAAGAGCTCCTGCTTGCCT | [38] | ||
| Reverse:TCTTCCCAGAAGGCGCACATCATA | 134 | 60 | ||
| DMBT1 | Forward: GAAATAGAGGTGAACTCCGGCTA- | 165 | 60 | Primer-BLAST |
| Reverse: TGTGAATATCTGGCTGGTGTGAT | ||||
| SPP1 | Forward: GCCCTTCCAGTTAAACAGACTAAT | |||
| Reverse: AGGGTCTCTTGTTTGAAGTCGT | 176 | 60 | Primer-BLAST |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cimini, C.; Moussa, F.; Taraschi, A.; Ramal-Sanchez, M.; Colosimo, A.; Capacchietti, G.; Mokh, S.; Valbonetti, L.; Tagaram, I.; Bernabò, N.; et al. Pre-Treatment of Swine Oviductal Epithelial Cells with Progesterone Increases the Sperm Fertilizing Ability in an IVF Model. Animals 2022, 12, 1191. https://doi.org/10.3390/ani12091191
Cimini C, Moussa F, Taraschi A, Ramal-Sanchez M, Colosimo A, Capacchietti G, Mokh S, Valbonetti L, Tagaram I, Bernabò N, et al. Pre-Treatment of Swine Oviductal Epithelial Cells with Progesterone Increases the Sperm Fertilizing Ability in an IVF Model. Animals. 2022; 12(9):1191. https://doi.org/10.3390/ani12091191
Chicago/Turabian StyleCimini, Costanza, Fadl Moussa, Angela Taraschi, Marina Ramal-Sanchez, Alessia Colosimo, Giulia Capacchietti, Samia Mokh, Luca Valbonetti, Israiel Tagaram, Nicola Bernabò, and et al. 2022. "Pre-Treatment of Swine Oviductal Epithelial Cells with Progesterone Increases the Sperm Fertilizing Ability in an IVF Model" Animals 12, no. 9: 1191. https://doi.org/10.3390/ani12091191








