Evaluation of Surgical Aid of Methylene Blue in Addition to Intraoperative Gamma Probe for Sentinel Lymph Node Extirpation in 116 Canine Mast Cell Tumors (2017–2022)
Abstract
:Simple Summary
Abstract
1. Introduction
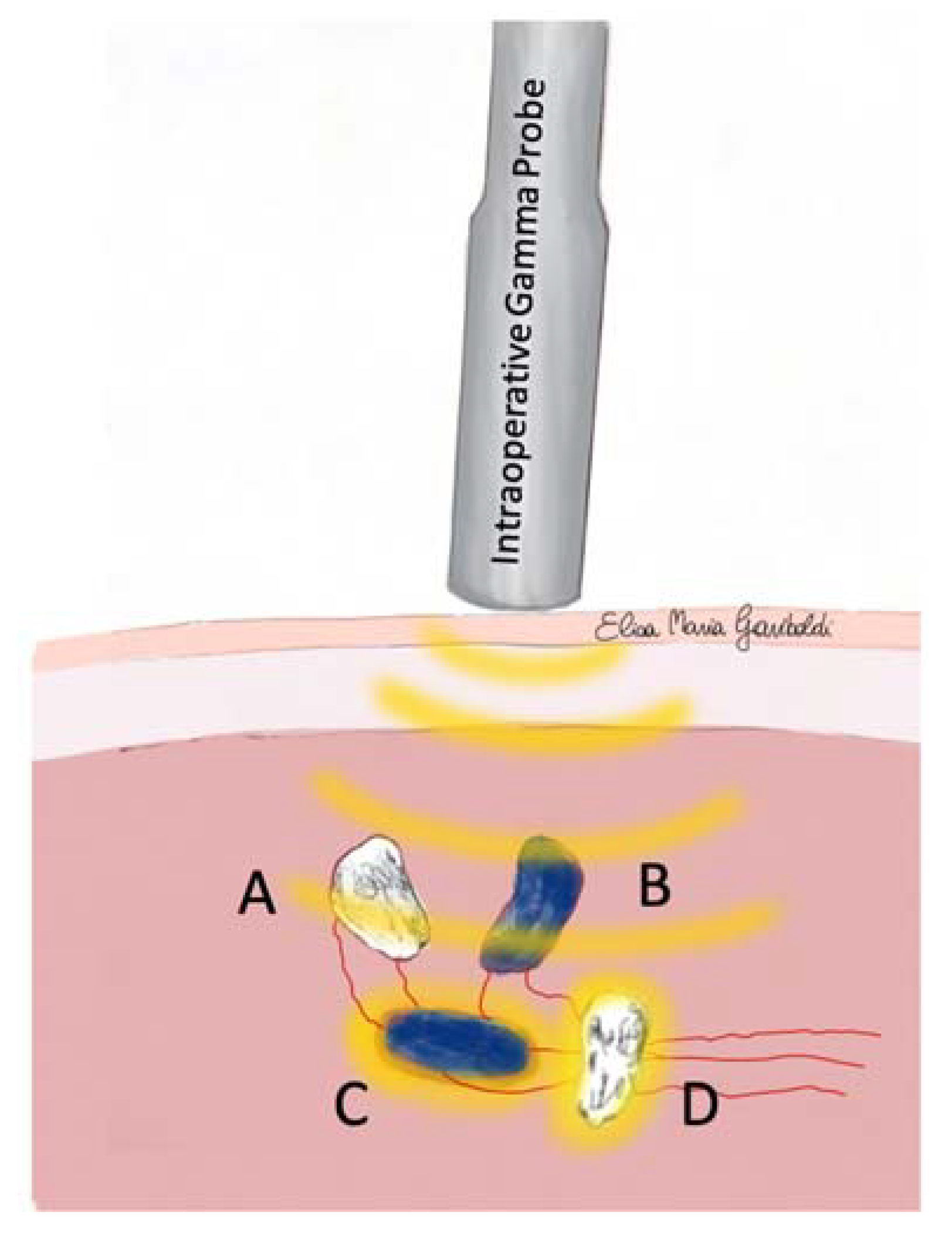
2. Materials and Methods
- “blue” if all its SLNs were stained blue;
- “non-blue” if all its SLNs were not stained blue;
- “mixed for blue’’ if both not blue and blue SLN were present in the SLC;
- “hot’’ if all SLNs were hot;
- “non-hot’’ if all SLNs were not hot;
- “mixed hot’’ if both non-hot and hot SLN were detected in the same SLC.
Statistical Analysis
3. Results
3.1. Canine Patients
3.2. Mast Cell Tumors
3.3. Sentinel Lymphocentrums
3.4. Sentinel Lymph Nodes
3.5. Surgical Data
3.6. Detection Technique Agreement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Worley, D.R. Incorporation of sentinel lymph node mapping in dogs with mast cell tumours: 20 consecutive procedures. Vet. Comp. Oncol. 2014, 12, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, R.; Chiti, L.E.; Manfredi, M.; Ravasio, G.; De Zani, D.; Zani, D.D.; Giudice, C.; Gambini, M.; Stefanello, D. Biopsy of sentinel lymph nodes after injection of methylene blue and lymphoscintigraphic guidance in 30 dogs with mast cell tumors. Vet. Surg. 2020, 49, 1099–1108. [Google Scholar] [CrossRef]
- Fournier, Q.; Thierry, F.; Longo, M.; Malbon, A.; Cazzini, P.; Bisson, J.; Woods, S.; Liuti, T.; Bavcar, S. Contrast-enhanced ultrasound for sentinel lymph node mapping in the routine staging of canine mast cell tumours: A feasibility study. Vet. Comp. Oncol. 2020, 19, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Lapsley, J.; Hayes, G.M.; Janvier, V.; Newman, A.W.; Peters-Kennedy, J.; Balkman, C.; Sumner, J.P.; Johnson, P. Influence of locoregional lymph node aspiration cytology vs sentinel lymph node mapping and biopsy on disease stage assignment in dogs with integumentary mast cell tumours. Vet. Surg. 2021, 50, 133–141. [Google Scholar] [CrossRef]
- Chiti, L.E.; Stefanello, D.; Manfredi, M.; Zani, D.D.; De Zani, D.; Boracchi, P.; Giudice, C.; Grieco, V.; Di Giancamillo, M.; Ferrari, R. To map or not to map the cN0 neck: Impact of sentinel lymph node biopsy in canine head and neck tumours. Vet. Comp. Oncol. 2021, 19, 661–670. [Google Scholar] [CrossRef]
- Weishaar, K.M.; Thamm, D.H.; Worley, D.R.; Kamstock, D.A. Correlation of nodal mast cells with clinical outcome in dogs with mast cell tumour and a proposed classification system for the evaluation of node metastasis. J. Comp. Pathol. 2014, 151, 329–338. [Google Scholar] [CrossRef]
- Marconato, L.; Polton, G.; Stefanello, D.; Morello, E.; Ferrari, R.; Henriques, J.; Tortorella, G.; Benali, S.L.; Bergottini, R.; Vasconi, M.E.; et al. Therapeutic impact of regional lymphadenectomy in canine stage II cutaneous mast cell tumours. Vet. Comp. Oncol. 2018, 16, 580–589. [Google Scholar] [CrossRef]
- Marconato, L.; Stefanello, D.; Kiupel, M.; Finotello, R.; Polton, G.; Massari, F.; Ferrari, R.; Agnoli, C.; Capitani, O.; Giudice, C.; et al. Adjuvant medical therapy provides no therapeutic benefit in the treatment of dogs with low-grade mast cell tumours and early nodal metastasis undergoing surgery. Vet. Comp. Oncol. 2020, 18, 409–415. [Google Scholar] [CrossRef]
- Guerra, D.; Faroni, E.; Sabattini, S.; Agnoli, C.; Chalfon, C.; Stefanello, D.; Del Magno, S.; Cola, V.; Grieco, V.; Marconato, L. Histologic grade has a higher-weighted value than nodal status as predictor of outcome in dogs with cutaneous mast cell tumours and overtly metastatic sentinel lymph nodes. Vet. Comp. Oncol. 2022, 20, 551–558. [Google Scholar] [CrossRef]
- Chalfon, C.; Sabattini, S.; Finotello, R.; Faroni, E.; Guerra, D.; Pisoni, L.; Ciammaichella, L.; Vasconi, M.E.; Annoni, M.; Marconato, L. Lymphadenectomy improves outcome in dogs with resected Kiupel high-grade cutaneous mast cell tumours and overtly metastatic regional lymph nodes. J. Small Anim. Pract. 2022, 63, 661–669. [Google Scholar] [CrossRef]
- Brissot, H.N.; Edery, E.G. Use of indirect lymphography to identify sentinel lymph node in dogs: A pilot study in 30 tumours. Vet. Comp. Oncol. 2017, 15, 740–753. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F.; Körner, M.; Suárez, J.; Carozzi, G.; Meier, V.S.; Roos, M.; Rohrer Bley, C. Computed tomographic-lymphography as a complementary technique for lymph node staging in dogs with malignant tumors of various sites. Vet. Radiol. Ultrasound 2018, 59, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Beer, P.; Rohrer-Bley, C.; Nolff, M.C. Near-infrared fluorescent image-guided lymph node dissection compared with locoregional lymphadenectomies in dogs with mast cell tumours. J. Small Anim. Pract. 2022, 63, 670–678. [Google Scholar] [CrossRef]
- Manfredi, M.; De Zani, D.; Chiti, L.E.; Ferrari, R.; Stefanello, D.; Giudice, C.; Pettinato, V.; Longo, M.; Di Giancamillo, M.; Zani, D.D. Preoperative planar lymphoscintigraphy allows for sentinel lymph node detection in 51 dogs improving staging accuracy: Feasibility and pitfalls. Vet. Radiol. Ultrasound 2021, 62, 602–609. [Google Scholar] [CrossRef]
- Wan, J.; Oblak, M.L.; Ram, A.; Singh, A.; Nykamp, S. Determining agreement between preoperative computed tomography lymphography and indocyanine green near infrared fluorescence intraoperative imaging for sentinel lymph node mapping in dogs with oral tumours. Vet. Comp. Oncol. 2021, 19, 295–303. [Google Scholar] [CrossRef]
- Alvarez-Sanchez, A.; Townsend, K.L.; Newsom, L.; Milovancev, M.; Gorman, E.; Russell, D.S. Comparison of indirect computed tomographic lymphography and near-infrared fluorescence sentinel lymph node mapping for integumentary canine mast cell tumors. Vet. Surg. 2023, 52, 416–427. [Google Scholar] [CrossRef] [PubMed]
- Goyal, A. New Technologies for Sentinel Lymph Node Detection. Breast Care 2018, 13, 349–353. [Google Scholar] [CrossRef]
- Inubushi, M.; Tatsumi, M.; Yamamoto, Y.; Kato, K.; Tsujikawa, T.; Nishii, R. European research trends in nuclear medicine. Ann. Nucl. Med. 2018, 32, 579–582. [Google Scholar] [CrossRef] [Green Version]
- Morton, D.L.; Thompson, J.F.; Essner, R.; Elashoff, R.; Stern, S.L.; Nieweg, O.E.; Roses, D.F.; Karakousis, C.P.; Mozzillo, N.; Reintgen, D.; et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: A multicenter trial. Multicenter Selective Lymphadenectomy Trial Group. Ann. Surg. 1999, 230, 453–465. [Google Scholar] [CrossRef]
- Kedrzycki, M.S.; Leiloglou, M.; Ashrafian, H.; Jiwa, N.; Thiruchelvam, P.T.R.; Elson, D.S.; Leff, D.R. Meta-analysis comparing fluorescence imaging with radioisotope and blue dye-guided sentinel node identification for breast cancer surgery. Ann. Surg. Oncol. 2021, 28, 3738–3748. [Google Scholar] [CrossRef]
- Sanidas, E.S.; de Bree, E.; Tsiftsis, D.D. How many cases are enough for accreditation in sentinel lymph node biopsy in breast cancer? Am. J. Surg. 2003, 185, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Albertini, J.J.; Cruse, C.W.; Rapaport, D.; Wells, K.; Ross, M.; DeConti, R.; Berman, C.G.; Jared, K.; Messina, J.; Lyman, G.; et al. Intraoperative radiolymphoscintigraphy improves sentinel lymph node identification for patients with melanoma. Ann. Surg. 1996, 223, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.-Q.; Zhang, G.-J.; Jansen, L.; de Vries, J.; Schröder, C.P.; de Vries, E.G.E.; van Dam, G.M. Evolution in sentinel lymph node biopsy in breast cancer. Crit. Rev. Oncol. Hematol. 2018, 123, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Randall, E.K.; Jones, M.D.; Kraft, S.L.; Worley, D.R. The development of an indirect computed tomography lymphography protocol for sentinel lymph node detection in head and neck cancer and comparison to other sentinel lymph node mapping techniques. Vet. Comp. Oncol. 2020, 18, 634–644. [Google Scholar] [CrossRef]
- Verbeek, F.P.; Troyan, S.L.; Mieog, J.S.; Liefers, G.J.; Moffitt, L.A.; Rosenberg, M.; Hirshfield-Bartek, J.; Gioux, S.; Van de Velde, C.J.; Vahrmeijer, A.L.; et al. Near-infrared fluorescence sentinel lymph node mapping in breast cancer: A multicenter experience. Breast Cancer Res. Treat. 2014, 143, 333–342. [Google Scholar] [CrossRef] [Green Version]
- Van der Vorst, J.R.; Schaafsma, B.E.; Verbeek, F.P.; Hutteman, M.; Mieog, J.S.; Lowik, C.W.; Liefers, G.J.; Frangioni, J.V.; van de Velde, C.J.; Vahrmeijer, A.L. Randomized comparison of near-infrared fluorescence imaging using indocyanine green and 99 (m) technetium with or without patent blue for the sentinel lymph node procedure in breast cancer patients. Ann. Surg. Oncol. 2012, 19, 4104–4111. [Google Scholar] [CrossRef] [Green Version]
- Argon, A.M.; Duygun, U.; Acar, E.; Daglioz, G.; Yenjay, L.; Zekioglu, O.; Kapkac, M. The use of periareolar intradermal Tc-99m tin colloid and peritumoral intraparenchymal isosulfan blue dye injections for determination of the sentinel lymph node. Clin. Nucl. Med. 2006, 31, 795–800. [Google Scholar] [CrossRef]
- Beer, P.; Pozzi, A.; Rohrer Bley, C.; Bacon, N.; Pfammatter, N.S.; Venzin, C. The role of sentinel lymph node mapping in small animal veterinary medicine: A comparison with current approaches in human medicine. Vet. Comp. Oncol. 2018, 16, 178–187. [Google Scholar] [CrossRef]
- Tuohy, J.L.; Worley, D.R. Pulmonary lymph node charting in normal dogs with blue dye and scintigraphic lymphatic mapping. Res. Vet. Sci. 2014, 97, 148–155. [Google Scholar] [CrossRef]
- Rossanese, M.; Pierini, A.; Pisani, G.; Freeman, A.; Burrow, R.; Booth, M.; Marchetti, V.; Finotello, R. Ultrasound-guided placement of an anchor wire or injection of methylene blue to aid in the intraoperative localization and excision of peripheral lymph nodes in dogs and cats. J. Am. Vet. Med. Assoc. 2021, 260 (Suppl. S1), S75–S82. [Google Scholar] [CrossRef]
- Patnaik, A.K.; Ehler, W.J.; MacEwen, E.G. Canine cutaneous mast cell tumor: Morphologic grading and survival time in 83 dogs. Vet. Pathol. 1984, 21, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Kiupel, M.; Webster, J.D.; Bailey, K.L.; Best, S.; DeLay, J.; Detrisac, C.J.; Fitzgerald, S.D.; Gamble, D.; Ginn, P.E.; Goldschmidt, M.H.; et al. Proposal of a 2-tier histologic grading system for canine cutaneous mast cell tumors to more accurately predict biological behavior. Vet. Pathol. 2011, 48, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.J.; Pearl, D.L.; Yager, J.A.; Best, S.J.; Coomber, B.L.; Foster, R.A. Canine subcutaneous mast cell tumor: Characterization and prognostic indices. Vet. Pathol. 2011, 48, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Dores, C.B.; Milovancev, M.; Russell, D.S. Comparison of histologic margin status in low-grade cutaneous and subcutaneous canine mast cell tumours examined by radial and tangential sections. Vet. Comp. Oncol. 2018, 16, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Giudice, C.; Stefanello, D.; Sala, M.; Cantatore, M.; Russo, F.; Romussi, S.; Travetti, O.; Di Giancamillo, M.; Grieco, V. Feline injection-site sarcoma: Recurrence, tumour grading and surgical margin status evaluated using the three-dimensional histological technique. Vet. J. 2010, 186, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C., 2nd; Edwards, M.J.; Wong, S.L.; Tuttle, T.M.; Carlson, D.J.; Brown, C.M.; Noyes, R.D.; Glaser, R.L.; Vennekotter, D.J.; Turk, P.S.; et al. Practical guidelines for optimal gamma probe detection of sentinel lymph nodes in breast cancer: Results of a multi-institutional study. For the University of Louisville Breast Cancer Study Group. Surgery 2000, 128, 139–144. [Google Scholar] [CrossRef]
- Suami, H.; Yamashita, S.; Soto-Miranda, M.A.; Chang, D.W. Lymphatic territories (lymphosomes) in a canine: An animal model for investigation of postoperative lymphatic alterations. PLoS ONE 2013, 8, e69222. [Google Scholar] [CrossRef] [Green Version]
- Baum, H. The Lymphatic System of the Dog; Mayer, M.; Bettin, L.; Bellamy, K.; Stamm, I., Translators; University of Saskatchewan: Saskatoon, SK, Canada, 2021; pp. 26–34. Available online: https://openpress.usask.ca/k9lymphaticsystem/ (accessed on 1 January 2021).
- Ram, A.S.; Matuszewska, K.; Petrik, J.; Singh, A.; Oblak, M.L. Quantitative and Semi-quantitative Methods for Assessing the Degree of Methylene Blue Staining in Sentinel Lymph Nodes in Dogs. Front. Vet. Sci. 2021, 8, 758295. [Google Scholar] [CrossRef]
- Mukaka, M.M. Statistics Corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- McMasters, K.M.; Wong, S.L.; Tuttle, T.M.; Carlson, D.J.; Brown, C.M.; Noyes, R.D.; Glaser, R.L.; Vennekotter, D.J.; Turk, P.S.; Tate, P.S.; et al. Preoperative lymphoscintigraphy for breast cancer does not improve the ability to identify axillary sentinel lymph nodes. Ann. Surg. 2000, 231, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Krag, D.N.; Anderson, S.J.; Julian, T.B.; Brown, A.M.; Harlow, S.P.; Ashikaga, T.; Weaver, D.L.; Miller, B.J.; Jalovec, L.M.; Frazier, T.G.; et al. National Surgical Adjuvant Breast and Bowel Project. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: Results from the NSABP B-32 randomised phase III trial. Lancet Oncol. 2007, 8, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Mathew, M.A.; Saha, A.K.; Saleem, T.; Saddozai, N.; Hutchinson, I.F.; Nejim, A. Pre-operative lymphoscintigraphy before sentinel lymph node biopsy for breast cancer. Breast 2010, 19, 28–32. [Google Scholar] [CrossRef] [PubMed]
- He, P.S.; Li, F.; Li, G.H.; Guo, C.; Chen, T.J. The combination of blue dye and radioisotope versus radioisotope alone during sentinel lymph node biopsy for breast cancer: A systematic review. BMC Cancer 2016, 16, 107. [Google Scholar] [CrossRef] [Green Version]
- Chiti, L.E.; Gariboldi, E.M.; Ferrari, R.; Luconi, E.; Boracchi, P.; De Zani, D.; Zani, D.; Manfredi, M.; Spediacci, C.; Grieco, V.; et al. Surgical complications following sentinel lymph node biopsy guided by γ-probe and methylene blue in 113 tumour-bearing dogs. Vet. Comp. Oncol. 2023, 21, 62–72. [Google Scholar] [CrossRef]
- Derossis, A.M.; Fey, J.; Yeung, H.; Yeh, S.D.; Heerdt, A.S.; Petrek, J.; VanZee, K.J.; Montgomery, L.L.; Borgen, P.I.; Cody, H.S., 3rd. A trend analysis of the relative value of blue dye and isotope localization in 2,000 consecutive cases of sentinel node biopsy for breast cancer. J. Am. Coll. Surg. 2001, 193, 473–478. [Google Scholar] [CrossRef]
- Bines, S.; Kopkash, K.; Ali, A.; Fogg, L.; Wool, N. The use of radioisotope combined with isosulfan Blue dye is not superior to radioisotope alone for the identification of sentinel lymph nodes in patients with breast cancer. Surgery 2008, 144, 606–610. [Google Scholar] [CrossRef]
- Van den Berg, N.S.; Brouwer, O.R.; Klop, W.M.; Karakullukcu, B.; Zuur, C.L.; Tan, I.B.; Balm, A.J.; Van den Brekel, M.W.; Valdés Olmos, R.A.; Van Leeuwen, F.W. Concomitant radio- and fluorescence-guided sentinel lymph node biopsy in squamous cell carcinoma of the oral cavity using ICG-(99m)Tc-nanocolloid. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 1128–1136. [Google Scholar] [CrossRef]
- Goyal, A.; Douglas-Jones, A.G.; Newcombe, R.G.; Mansel, R.E. Effect of lymphatic tumor burden on sentinel lymph node biopsy in breast cancer. Breast J. 2005, 11, 188–194. [Google Scholar] [CrossRef]
- Bagaria, S.P.; Faries, M.B.; Morton, D.L. Sentinel node biopsy in melanoma: Technical considerations of the procedure as performed at the John Wayne Cancer Institute. J. Surg. Oncol. 2010, 101, 669–676. [Google Scholar] [CrossRef] [Green Version]
- McHugh, J.B.; Su, L.; Griffith, K.A.; Schwartz, J.L.; Wong, S.L.; Cimmino, V.; Chang, A.E.; Johnson, T.M.; Sabel, M.S. Significance of Multiple Lymphatic Basin Drainage in Truncal Melanoma Patients Undergoing Sentinel Lymph Node Biopsy. Ann. Surg. Oncol. 2006, 13, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.H.; Ozao-Choy, J.J.; Hiles, J.M.; Sim, M.-S.; Faries, M.B. Prognostic Value of Multiple Draining lymph node Basins in Melanoma: A Matched-Pair analysis Based on the John Wayne cancer institute experience. Front. Oncol. 2017, 7, 172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrari, R.; Marconato, L.; Buracco, P.; Boracchi, P.; Giudice, C.; Iussich, S.; Grieco, V.; Chiti, L.E.; Favretto, E.; Stefanello, D. The impact of extirpation of non-palpable/normal-sized regional lymph nodes on staging of canine cutaneous mast cell tumours: A multicentric retrospective study. Vet. Comp. Oncol. 2018, 16, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Burns, G.O.; Scrivani, P.V.; Thompson, M.S.; Erb, H.N. Relation between age, body weight, and medial retropharyngeal lymph node size in apparently healthy dogs. Vet. Radiol. Ultrasound 2008, 49, 277–281. [Google Scholar] [CrossRef]
- Teodori, S.; Aste, G.; Tamburro, R.; Morselli-Labate, A.M.; Simeoni, F.; Vignoli, M. Computed Tomography Evaluation of Normal Canine Abdominal Lymph Nodes: Retrospective Study of Size and Morphology According to Body Weight and Age in 45 Dogs. Vet. Sci. 2021, 8, 44. [Google Scholar] [CrossRef]
- Stan, F.; Gudea, A.; Damian, A.; Gal, A.F.; Papuc, I.; Pop, A.R.; Martonos, C. Ultrasonographic algorithm for the assessment of sentinel lymph nodes that drain the mammary carcinomas in female dogs. Animals 2020, 10, 2366. [Google Scholar] [CrossRef]
- Baginski, H.; Davis, G.; Bastian, R.P. The prognostic value of lymph node metastasis with grade 2 MCTs in dogs: 55 cases (2001–2010). J. Am. Anim. Hosp. Assoc. 2014, 50, 89–95. [Google Scholar] [CrossRef]
- Ferrari, R.; Boracchi, P.; Chiti, L.E.; Manfredi, M.; Giudice, C.; De Zani, D.; Spediacci, C.; Recordati, C.; Grieco, V.; Gariboldi, E.M.; et al. Assessing the Risk of Nodal Metastases in Canine Integumentary Mast Cell Tumors: Is Sentinel Lymph Node Biopsy Always Necessary? Animals 2021, 11, 2373. [Google Scholar] [CrossRef]
- du Bois, H.; Heim, T.A.; Lund, A.W. Tumor-draining lymph nodes: At the crossroads of metastasis and immunity. Sci. Immunol. 2021, 6, 3551. [Google Scholar] [CrossRef]

| Variables | N° of Tumors and % |
|---|---|
| Clinical presentation | |
| Anatomical localization | |
| Limbs | 37 (32%) |
| Trunk | 33 (28%) |
| Head and neck | 16 (14%) |
| Inguinal region | 15 (13%) |
| Digits | 8 (7%) |
| Mammary region | 5 (4%) |
| Tail | 2 (2%) |
| Ulceration | |
| Yes | 18 (16%) |
| No | 98 (84%) |
| Histopathological data | |
| Histopathological type | |
| Cutaneous | 80 (69%) |
| Patnaik | |
| I | 15 (19%) |
| II | 64 (80%) |
| III | 1 (1%) |
| Kiupel | |
| Low-grade | 78 (97%) |
| High-grade | 2 (3%) |
| Subcutaneous | 35 (30%) |
| Histological pattern | |
| Infiltrative | 19 (54%) |
| Circumscribed | 4 (12%) |
| Combined | 12 (34%) |
| Mucocutaneous | 1 (1%) |
| Surgical margins | |
| Clean | 90 (78%) |
| Clean but close | 3 (2%) |
| Infiltrated | 23 (20%) |
| Blue–Hot | Blue–Non-Hot | Blue –Mixed Hot | Non-Blue –Hot | Non-Blue –Non-Hot | Non-Blue–Mixed Hot | Mixed Blue –Hot | Mixed Blue–Non-Hot | Mixed Blue–Mixed Hot | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Non Metastatic | 60 (83%) | 1 (1.5%) | 0 | 5 (7%) | 2 (3%) | 1 (1.5%) | 0 | 0 | 3 (4%) | 72 (100%) |
| Metastatic | 53 (78%) | 3 (4%) | 5 (7.5%) | 2 (3%) | 1 (1.5%) | 1 (1.5%) | 1 (1.5%) | 0 | 2 (3%) | 68 (100%) |
| Total | 113 (80.7%) | 4 (2.9%) | 5 (3.6%) | 7 (5%) | 3 (2%) | 2 (1.4%) | 1 (0.7%) | 0 | 5 (3.6%) | 140 (100%) |
| Blue–Hot | Blue–Non-Hot | Non-Blue–Hot | Non-Blue–Non-Hot | Total | |
|---|---|---|---|---|---|
| HN0 | 56 (76.7%) | 4 (5.5%) | 6 (8.2%) | 7 (9.6%) | 73 (100%) |
| HN1 | 34 (91.9%) | 0 | 2 (5.4%) | 1 (2.7%) | 37 (100%) |
| HN2 | 56 (84.9%) | 6 (9.1%) | 2 (3%) | 2 (3%) | 66 (100%) |
| HN3 | 18 (90%) | 0 | 2 (10%) | 0 | 20 (100%) |
| Total | 164 (84%) | 10 (5%) | 12 (6%) | 10 (5%) | 196 (100%) |
| Blue–Hot | Blue–Non-Hot | Non-Blue–Hot | Non-Blue–Non-Hot | Total | |
|---|---|---|---|---|---|
| HN0-HN1 (non-metastatic) | 90 (82%) | 4 (4%) | 8 (7%) | 8 (7%) | 110 (100%) |
| HN2-HN3 (metastatic) | 74 (86%) | 6 (7%) | 4 (5%) | 2 (2%) | 86 (100%) |
| Total | 164 (84%) | 10 (5%) | 12 (6%) | 10 (5%) | 196 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gariboldi, E.M.; Ubiali, A.; Chiti, L.E.; Ferrari, R.; De Zani, D.; Zani, D.D.; Grieco, V.; Giudice, C.; Recordati, C.; Stefanello, D.; et al. Evaluation of Surgical Aid of Methylene Blue in Addition to Intraoperative Gamma Probe for Sentinel Lymph Node Extirpation in 116 Canine Mast Cell Tumors (2017–2022). Animals 2023, 13, 1854. https://doi.org/10.3390/ani13111854
Gariboldi EM, Ubiali A, Chiti LE, Ferrari R, De Zani D, Zani DD, Grieco V, Giudice C, Recordati C, Stefanello D, et al. Evaluation of Surgical Aid of Methylene Blue in Addition to Intraoperative Gamma Probe for Sentinel Lymph Node Extirpation in 116 Canine Mast Cell Tumors (2017–2022). Animals. 2023; 13(11):1854. https://doi.org/10.3390/ani13111854
Chicago/Turabian StyleGariboldi, Elisa Maria, Alessandra Ubiali, Lavinia Elena Chiti, Roberta Ferrari, Donatella De Zani, Davide Danilo Zani, Valeria Grieco, Chiara Giudice, Camilla Recordati, Damiano Stefanello, and et al. 2023. "Evaluation of Surgical Aid of Methylene Blue in Addition to Intraoperative Gamma Probe for Sentinel Lymph Node Extirpation in 116 Canine Mast Cell Tumors (2017–2022)" Animals 13, no. 11: 1854. https://doi.org/10.3390/ani13111854
APA StyleGariboldi, E. M., Ubiali, A., Chiti, L. E., Ferrari, R., De Zani, D., Zani, D. D., Grieco, V., Giudice, C., Recordati, C., Stefanello, D., & Auletta, L. (2023). Evaluation of Surgical Aid of Methylene Blue in Addition to Intraoperative Gamma Probe for Sentinel Lymph Node Extirpation in 116 Canine Mast Cell Tumors (2017–2022). Animals, 13(11), 1854. https://doi.org/10.3390/ani13111854







