Overview of Bovine Mastitis: Application of Metabolomics in Screening Its Predictive and Diagnostic Biomarkers
Abstract
:Simple Summary
Abstract
1. Introduction
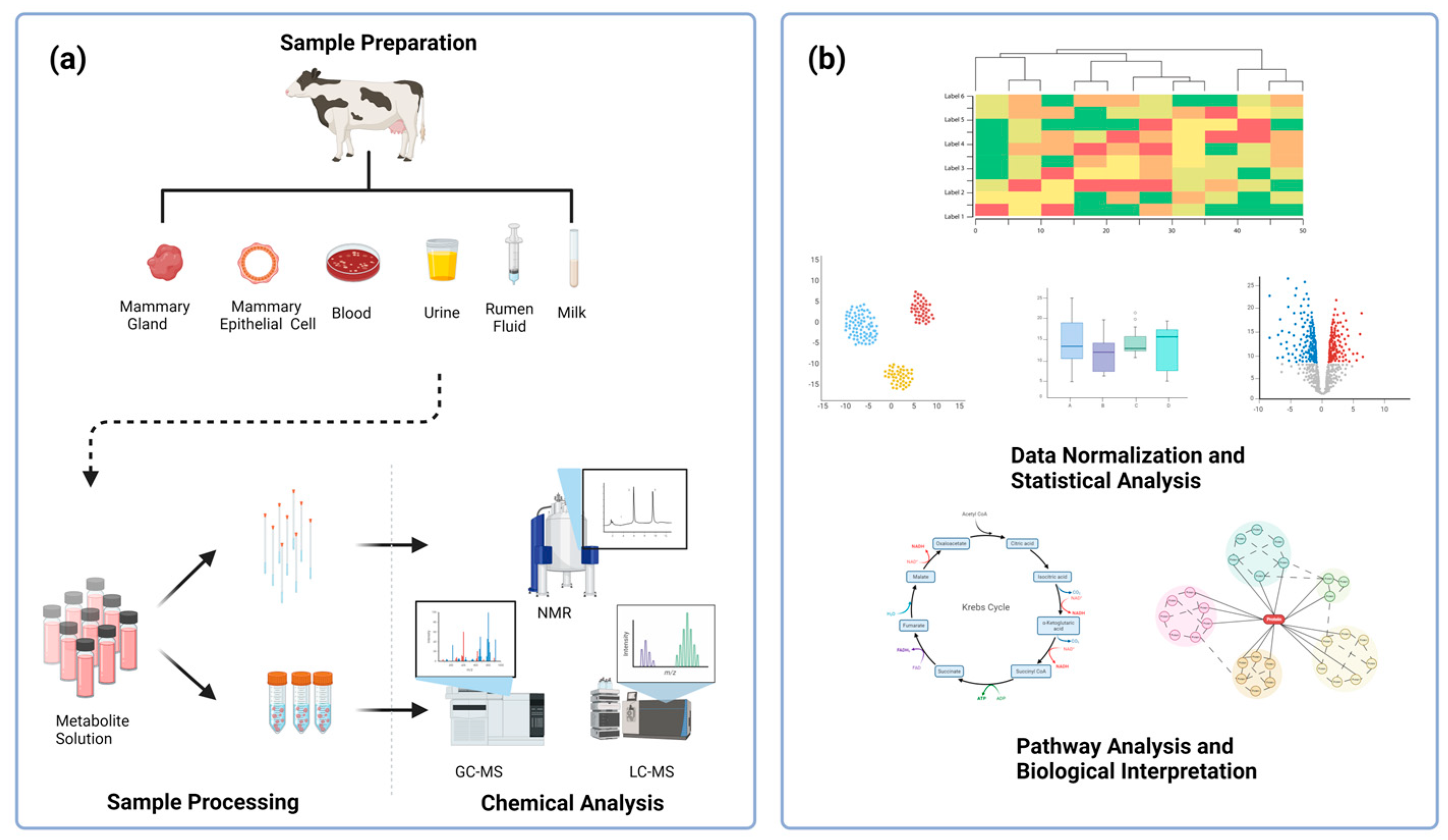
2. Methodology
3. Pathogenesis of Bovine Mastitis
4. Diagnosis of Bovine Mastitis
| Method | Strengths | Weakness | References |
|---|---|---|---|
| SCC |
|
| [59,60] |
| Bacterial culture |
|
| [61] |
| PCR |
|
| [62] |
| California Mastitis Test |
|
| [63] |
| Electrical conductivity test |
|
| [64] |
| Sensor |
|
| [65] |
| IRT |
|
| [66] |
5. Milk Metabolomics
| Method | Type of Mastitis | Key Differential Metabolites | Important Metabolic Pathway | Reference |
|---|---|---|---|---|
| NMR | CM | Dimethylamine, Tyr, lactate, Leu, Pro, Val, Arg, Ile, fumarate, lactose, maltose, 2-oxoglutarate, citrate, cis-aconitate, creatine, O-acetylcarnitine, Gly, creatinine, carnitine, choline, N-acetylglucosamine, trimethylamine N-oxide | Metabolism: Gly, Ser, Thr; biosynthesis: Phe, Tyr, Trp; TCA cycle | [77] |
| NMR | SCM CM | SCM: hippurate, valerate, N-acetylglucosamine, His, Ile, Leu, fumarate CM: acetate, formate, lactate, benzoate, hippurate, β-hydroxybutyrate, valerate, N-acetylamino acid, Ala, His, Ile, Leu, Phe, Thr, Val | / | [74] |
| NMR | / | Lactate, acetate, β-hydroxybutyrate, butyrate, isoleucine, lactose, hippurate, fumarate | / | [71] |
| NMR | SCM CM | Lactate, Ala, pyruvate, succinate, formate, sn-glycero-3-phosphocholine | His metabolism; glycolysis; gluconeogenesis; lipolysis; β-oxidation; TCA cycle | [85] |
| GC-TOFMS | SCM | phenylpyruvic acid, homogentisic acid, 4-hydroxyphenylpyruvic acid, xanthine, guanine, uridine, glycerol, pyrophosphate | Metabolism: galactose, starch, sucrose, Ala, Asp, D-Glu, D-Gln; biosynthesis: Arg, neomycin, kanamycin, gentamicin; pentose and glucuronate interconversion; TCA cycle | [78] |
| LC-MS | SCM CM | 2-Aminoethyl dihydrogen phosphate, 4,5-dihydroxyphthalic acid, O-succinyl-L-homoserine, isolithocholic acid, Tyr-Ile, dihydroxyacetone, D-fructofuranose, dichlorprop, fludrocortisone acetate, 2,4-dinitrotoluene | Metabolism: fructose, mannose, pyrimidine, 2-oxocarboxylic acid, nucleotides, glycerolipid, carbon; taste transduction; ABC transporters; bile secretion | [49] |
| LC-MS | SCM CM | Ceramide(d18:1/22:0), testosterone, glucuronide, 5-methyl-(THF), xanthine, 5-aminoimidazole ribonucleotide, thiamine, L-Arginine phosphate | Metabolism: sphingolipid, thiamine, purine, pyrimidine, glycerophospholipid, riboflavin, galactose, Cys, Met, Arg, Pro, Gly, Ser, Thr; biosynthesis: unsaturated fatty acids, steroid hormone; one-carbon pool by folate | [50] |
| LC-MS | / | Bile acids (taurochenodeoxycholic acid, taurocholic acid, glycocholate, glycodeoxycholate, cholate), hippurate, lactate, Leu, lactose, 2,3-dinor-8-iso PGF2α | Metabolism: Ala, Asp, Glu, pyrimidine, purine, ascorbate, aldarate, eicosanoids | [69] |
| LC-MS | CM | HODE, 13-HODE, 13-oxoODE, 9-HODE, 6-keto PGF1α, 11-HETE | Oxylipid biosynthesis | [86] |
6. Blood Metabolomics
| Method | Type of Mastitis | Key Differential Metabolites | Important Metabolic Pathway | Reference |
|---|---|---|---|---|
| NMR | SCM | His, lactose, acetate, Asn, dimethylamine, Val, Cit, methylguanidine, 3-hydroxybutyrate, acetone, allantoin, carnitine, citrate, ethanol | Ruminal fermentation, energy metabolism, urea synthesis and metabolism, immune and inflammatory response, mammary gland permeability | [100] |
| NMR | CM | Lactate, Ser, Phe, formate, Asn, citrate | / | [88] |
| NMR | SCM | His, lactose, acetate, Asp, dimethylamine, Val, carnitine, Cit, methylguanidine, 3-hydroxybutyrate, acetone, allantoin, ethanol, betaine, choline | Metabolism: Gly, Ser, Thr; biosynthesis: aminoacyl-tRNA, Phe, Tyr, Trp | [100] |
| NMR | SCM CM | Malonate, Phe, Ile, Histamine, Leu, glucose, Gly | His metabolism; glycolysis; gluconeogenesis; lipolysis; β-oxidation; citric acid cycle | [85] |
| NMR | CM | Lactose, Lactate, 3-hydroxybutyrate, acetoacetate, butyrate, acetate, citrate, propionate | / | [99] |
| GC-MS | SCM | Val, Ser, Tyr, Phe, Ile, Pro | Metabolism: propanoate, sphingolipid, Met, Phe, Tyr, Asp, Gly, Ser, Thr, porphyrin, glutathione; degradation: sphingolipid, Val, Leu, Ile; biosynthesis: protein, bile acid; ammonia recycling | [93] |
| LC-MS | SCM CM | 20-Trihydroxy-leukotriene-B4, 13,14-dihydro-15-keto-PGE2, 9,10-dihydroxylinoleicacids, deoxycholic acid, 12-ketolithocholic acid, 3-hydroxyisovalerylcarnitine, citric acid, uric acid, inosine | Metabolism: arachidonic acid, linoleic acid, purine, carnitine, Ala, Asp, Glu; biosynthesis: primary bile acid, secondary bile acid; citrate cycle | [101] |
| LC-MS/MS | SCM | Leu, Ala, Orn, betaine, methylmalonate, lactate, pyruvate | Metabolism: Gly, Ser, Met, betaine, selenoamino acid; glucose–AlacCycle | [94] |
| LC-MS/MS | SCM | Kynurenine, sphingomyelin C26:0, Lys, Leu, Ile | Metabolism: biotin, Cys, Met, glutathione; degradation: Lys, Val, Leu, Ile; biosynthesis: Val, Leu, Ile, aminoacyl -tRNA | [95] |
| UPLC-MSE | CM | 3′-Sialyllactose, N-methylethanolamine phosphate, choline, phosphorylcholine, free carnitine, trimethyl lysine, Tyr, Pro | Metabolism: carnitine, AA, water-soluble phospholipid | [98] |
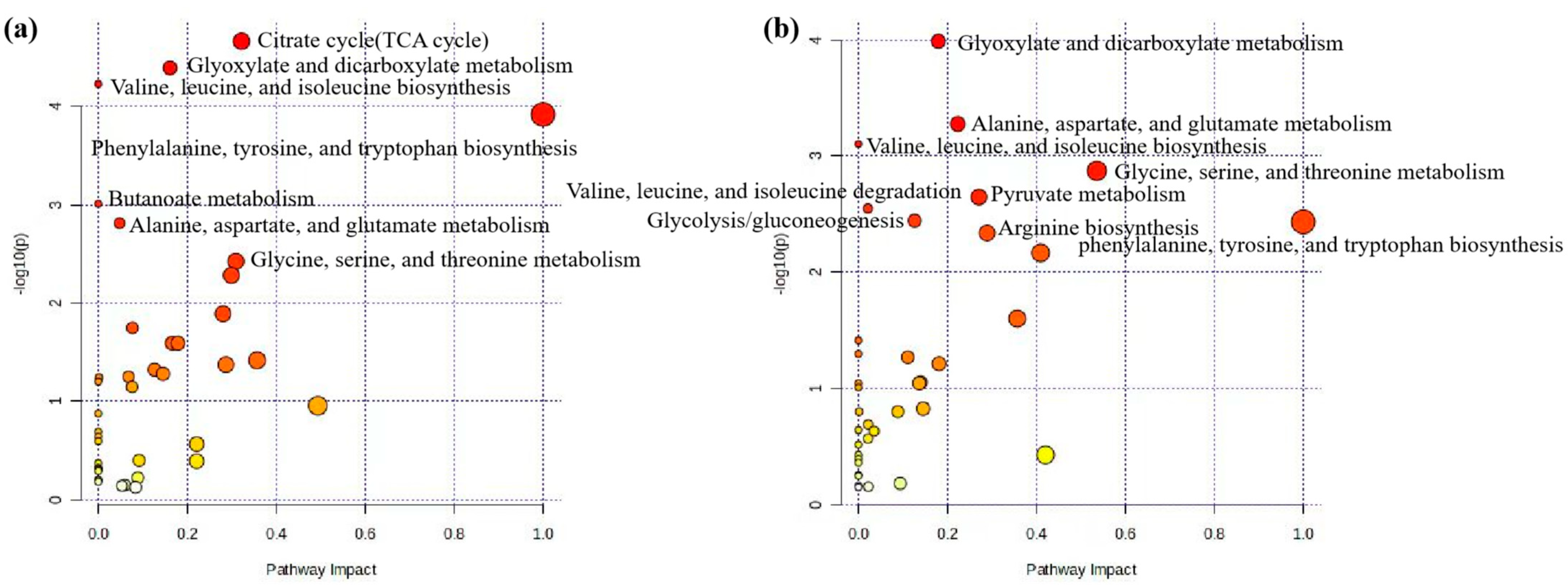
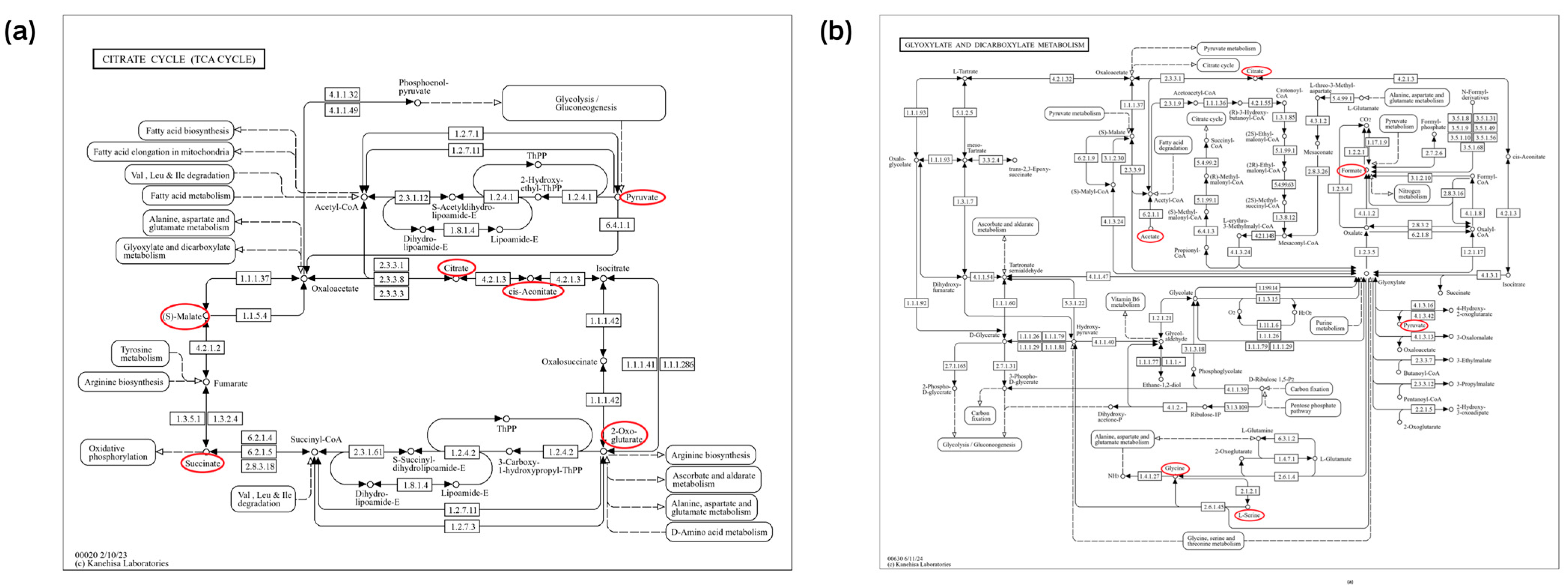
7. Milk Metabolomics and Blood Metabolomics Pathway Analysis
8. Metabolomics in Other Sample Types
| Sample Type | Method | Type of Mastitis | Key Differential Metabolites | Important Metabolic Pathway | Reference |
|---|---|---|---|---|---|
| mammary gland | LC-MS | CM | 6-Keto prostaglandin F1α, prostaglandin E2, prostaglandin F2α, 5-oxoeicosatetraenoic acid, 9-hydroxyoctadecadienoic acid, 13-hydroxyoctadecadienoic acid, 9-oxooctadecadienoic acid | Oxylipid biosynthesis | [86] |
| urine | NMR | CM | Citrate, lactose, taurine, methylamine, N-acetylaspartate, galactose, 3-phenylpropionate | / | [88] |
| DI/LC-MS/MS | SCM | acylcarnitines (C3:1, C3-OH, C5-DC (C6-OH), C5-M-DC, C14:1, C18:2, C12, C14, C16:2), phosphatidylcholines (PC aa C34:2, PC ae C42:1, PC ae C36:4), AA (Asp, Glu, His, Thr), biogenic amines (carnosine, symmetric dimethylarginine), hexose | Metabolism: selenoamino acid, Asp, arachidonic acid, Cys, Tyr, Met, sphingolipid; biosynthesis: phosphatidylethanolamine, fatty acids; ammonia recycling; malate–aspartate shuttle; homocysteine degradation | [104] | |
| feces | NMR | CM | Propionate, acetate, pyruvate, acetoacetate, 2,3-butanediol, ethanol, glycine, O-acetylcholine, glutamine, O-phosphocholine, | / | [88] |
| LC-MS | SCM CM | 20-trihydroxy-leukotriene-B4, 13,14-dihydro-15-keto-PGE2, 9,10-dihydroxylinoleicacids, deoxycholic acid, 12-ketolithocholic acid, 3-hydroxyisovalerylcarnitine, citric acid, uric acid, inosine | Metabolism: arachidonic acid, linoleic acid, purine, carnitine, Ala, Asp, Glu; biosynthesis: primary bile acid, secondary bile acid; citrate cycle | [101] | |
| rumen fluid | LC-MS/MS | SCM CM | SCM: methenamine, 5-hydroxymethyl-2-furancarboxaldehyde, 6-methoxymellein CM: 12-oxo-20-dihydroxy-leukotriene B4, 10beta-hydroxy-6beta-isobutyrylfuranoeremophilane, 2-phenylbutyric acid | Metabolism: arachidonic acid, butanoate; degradation: limonene, pinene, furfural; biosynthesis: formaldehyde, plant secondary metabolites | [106] |
9. Existing Knowledge Gap and Future Recommendations
10. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hogeveen, H.; Steeneveld, W.; Wolf, C.A. Production diseases reduce the efficiency of dairy production: A review of the results, methods, and approaches regarding the economics of mastitis. Annu. Rev. Resour. Econ. 2019, 11, 289–312. [Google Scholar] [CrossRef]
- Tommasoni, C.; Fiore, E.; Lisuzzo, A.; Gianesella, M. Mastitis in dairy cattle: On-Farm diagnostics and future perspectives. Animals 2023, 13, 2538. [Google Scholar] [CrossRef] [PubMed]
- Laliotis, G.P.; Koutsouli, P.; Sotirakoglou, K.; Savoini, G.; Politis, I. Association of Oxidative Stress Biomarkers and Clinical Mastitis Incidence in Dairy Cows During the Periparturient Period. J. Vet. Res. 2020, 64, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Cobirka, M.; Tancin, V.; Slama, P. Epidemiology and classification of mastitis. Animals 2020, 10, 2212. [Google Scholar] [CrossRef]
- Suzuki, N.; Kurose, T.; Kaneko, S.; Haraguchi, A.; Isobe, N. Outcome prediction from the first examination in clinical mastitis using ultrasonography in dairy cows. Anim. Sci. J. 2020, 91, e13452. [Google Scholar] [CrossRef]
- Shaheen, T.; Ahmad, S.B.; Rehman, M.U.; Muzamil, S.; Bhat, R.R.; Hussain, I.; Bashir, N.; Mir, M.U.R.; Paray, B.A.; Dawood, M.A.O. Investigations on cytokines and proteins in lactating cows with and without naturally occurring mastitis. J. King Saud. Univ. Sci. 2020, 32, 2863–2867. [Google Scholar] [CrossRef]
- Rienesl, L.; Khayatzdadeh, N.; Koeck, A.; Egger-Danner, C.; Gengler, N.; Grelet, C.; Dale, L.M.; Werner, A.; Auer, F.; Leblois, J.; et al. Prediction of Acute and Chronic Mastitis in Dairy Cows Based on Somatic Cell Score and Mid-Infrared Spectroscopy of Milk. Animals 2022, 12, 1830. [Google Scholar] [CrossRef]
- Li, X.; Xu, C.; Liang, B.; Kastelic, J.P.; Han, B.; Tong, X.; Gao, J. Alternatives to antibiotics for treatment of mastitis in dairy cows. Front. Vet. Sci. 2023, 10, 1160350. [Google Scholar] [CrossRef] [PubMed]
- Rollin, E.; Dhuyvetter, K.C.; Overton, M.W. The cost of clinical mastitis in the first 30 days of lactation: An economic modeling tool. Prev. Vet. Med. 2015, 122, 257–264. [Google Scholar] [CrossRef]
- Halasa, T.; Huijps, K.; Osteras, O.; Hogeveen, H. Economic effects of bovine mastitis and mastitis management: A review. Vet. Q. 2007, 29, 18–31. [Google Scholar] [CrossRef]
- Zhao, X.; Lacasse, P. Mammary tissue damage during bovine mastitis: Causes and control. J. Anim. Sci. 2008, 86, 57–65. [Google Scholar] [CrossRef]
- Blum, S.E.; Heller, E.D.; Leitner, G. Long term effects of Escherichia coli mastitis. Vet. J. 2014, 201, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Aghamohammadi, M.; Haine, D.; Kelton, D.F.; Barkema, H.W.; Hogeveen, H.; Keefe, G.P.; Dufour, S. Herd-Level mastitis-associated costs on canadian dairy farms. Front. Vet. Sci. 2018, 5, 100. [Google Scholar] [CrossRef] [PubMed]
- Mbindyo, C.M.; Gitao, G.C.; Mulei, C.M. Prevalence, etiology, and risk factors of mastitis in dairy cattle in embu and kajiado counties, kenya. Vet. Med. Int. 2020, 2020, 8831172. [Google Scholar] [CrossRef]
- Califf, R.M. Biomarker definitions and their applications. Exp. Biol. Med. 2018, 243, 213–221. [Google Scholar] [CrossRef]
- Chen, X.X.; Xu, Y.M.; Lau, A. Metabolic effects of long-term cadmium exposure: An overview. Environ. Sci. Pollut. Res. 2022, 29, 89874–89888. [Google Scholar] [CrossRef] [PubMed]
- Porto, V.A.; Da, R.J.E.; Ursulino, J.S.; Porto, R.S.; Da, S.M.; de Jesus, L.; Oliveira, J.M.; Crispim, A.C.; Santos, J.; Aquino, T.M. NMR-based metabolomics applied to ecotoxicology with zebrafish (Danio rerio) as a prominent model for metabolic profiling and biomarker discovery: Overviewing the most recent approaches. Sci. Total Environ. 2023, 868, 161737. [Google Scholar] [CrossRef]
- Sille, F.; Hartung, T. Metabolomics in preclinical drug safety assessment: Current status and future trends. Metabolites 2024, 14, 98. [Google Scholar] [CrossRef]
- Yu, J.W.; Song, M.H.; Lee, J.H.; Song, J.H.; Hahn, W.H.; Keum, Y.S.; Kang, N.M. Urinary metabolomic differentiation of infants fed on human breast milk and formulated milk. Metabolites 2024, 14, 128. [Google Scholar] [CrossRef]
- Gao, Y.; Hou, L.; Gao, J.; Li, D.; Tian, Z.; Fan, B.; Wang, F.; Li, S. Metabolomics approaches for the comprehensive evaluation of fermented foods: A review. Foods 2021, 10, 2294. [Google Scholar] [CrossRef]
- Legrand, E.; Basu, N.; Hecker, M.; Crump, D.; Xia, J.; Chandramouli, B.; Butler, H.; Head, J.A. Targeted metabolomics to assess exposure to environmental chemicals of concern in japanese quail at two life stages. Metabolites 2021, 11, 850. [Google Scholar] [CrossRef]
- Wishart, D.S.; Cheng, L.L.; Copie, V.; Edison, A.S.; Eghbalnia, H.R.; Hoch, J.C.; Gouveia, G.J.; Pathmasiri, W.; Powers, R.; Schock, T.B.; et al. NMR and metabolomics—A roadmap for the future. Metabolites 2022, 12, 678. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, M.S.; Carvalho, M.; Bastos, M.L.; Guedes, D.P.P. Metabolomics analysis for biomarker discovery: Advances and challenges. Curr. Med. Chem. 2013, 20, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, Å.; Persson Waller, K.; Svennersten-Sjaunja, K.; Haugen, J.; Lundby, F.; Lind, O. Detection of mastitic milk using a gas-sensor array system (electronic nose). Int. Dairy J. 2005, 15, 1193–1201. [Google Scholar] [CrossRef]
- Sadat, A.; Farag, A.M.M.; Elhanafi, D.; Awad, A.; Elmahallawy, E.K.; Alsowayeh, N.; El-khadragy, M.F.; Elshopakey, G.E. Immunological and Oxidative Biomarkers in Bovine Serum from Healthy, Clinical, and Sub-Clinical Mastitis Caused by Escherichia coli and Staphylococcus aureus Infection. Animals 2023, 13, 892. [Google Scholar] [CrossRef]
- Campos, B.; Pickering, A.C.; Rocha, L.S.; Aguilar, A.P.; Fabres-Klein, M.H.; de Oliveira, M.T.; Fitzgerald, J.R.; de Oliveira, B.R.A. Diversity and pathogenesis of Staphylococcus aureus from bovine mastitis: Current understanding and future perspectives. BMC Vet. Res. 2022, 18, 115. [Google Scholar] [CrossRef]
- Benic, M.; Macesic, N.; Cvetnic, L.; Habrun, B.; Cvetnic, Z.; Turk, R.; Duricic, D.; Lojkic, M.; Dobranic, V.; Valpotic, H.; et al. Bovine mastitis: A persistent and evolving problem requiring novel approaches for its control—A review. Vet. Arh. 2018, 88, 535–557. [Google Scholar] [CrossRef]
- Aitken, S.L.; Corl, C.M.; Sordillo, L.M. Immunopathology of mastitis: Insights into disease recognition and resolution. J. Mammary Gland. Biol. Neoplasia 2011, 16, 291–304. [Google Scholar] [CrossRef]
- Girma, A.; Tamir, D. Prevalence of Bovine Mastitis and its associated risk factors among dairy cows in ethiopia during 2005-2022: A systematic review and meta-analysis. Vet. Med. Int. 2022, 2022, 7775197. [Google Scholar] [CrossRef]
- Cheng, W.N.; Han, S.G. Bovine mastitis: Risk factors, therapeutic strategies, and alternative treatments—A review. Asian Australas. J. Anim. Sci. 2020, 33, 1699–1713. [Google Scholar] [CrossRef]
- Khan, M.Z.; Khan, A.; Xiao, J.; Ma, J.; Ma, Y.; Chen, T.; Shao, D.; Cao, Z. Overview of research development on the role of nf-kappab signaling in mastitis. Animals 2020, 10, 1625. [Google Scholar] [CrossRef] [PubMed]
- Taponen, S.; Pyorala, S. Coagulase-negative staphylococci as cause of bovine mastitis—Not so different from Staphylococcus aureus? Vet. Microbiol. 2009, 134, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Xie, X.; Du, T.; Jiang, X.; Miao, W.; Wang, T. Lactococcus lactis, a bacterium with probiotic functions and pathogenicity. World J. Microbiol. Biotechnol. 2023, 39, 325. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Xiang, W.; Wang, Q.; Yin, J.; Tian, T.; Yang, Q.; Zhang, M.; Ge, G.; Li, J.; Diao, N.; et al. Prevalence and risk factors of Klebsiella spp. in milk samples from dairy cows with mastitis-A global systematic review. Front. Vet. Sci. 2023, 10, 1143257. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Fang, Z.; Mu, T.; Wang, Z.; Ma, Y.; Ma, Y. Application of metabolomics in diagnosis of cow mastitis: A review. Front. Vet. Sci. 2021, 8, 747519. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Sun, H.; Zhao, Y.; Feng, L.; Wu, K.; Shang, S.; Xu, J.; Shan, R.; Duan, S.; Qiu, M.; et al. Hexadecanamide alleviates Staphylococcus aureus-induced mastitis in mice by inhibiting inflammatory responses and restoring blood-milk barrier integrity. PLoS Pathog. 2023, 19, e1011764. [Google Scholar] [CrossRef] [PubMed]
- Müller, U.; Neu-Zahren, A.; Sauerwein, H. Milking-induced changes of the teat canal: Review of investigation methods and first results from testing teat canal penetrability. Milchwissenschaft 2006, 6, 242–245. [Google Scholar]
- Rainard, P.; Riollet, C. Innate immunity of the bovine mammary gland. Vet. Res. 2006, 37, 369–400. [Google Scholar] [CrossRef] [PubMed]
- Haxhiaj, K.; Wishart, D.S.; Ametaj, B.N. Mastitis: What it is, current diagnostics, and the potential of metabolomics to dentify new predictive biomarkers. Dairy 2022, 3, 722–746. [Google Scholar] [CrossRef]
- Hettinga, K.A.; van Valenberg, H.J.; Lam, T.J.; van Hooijdonk, A.C. Detection of mastitis pathogens by analysis of volatile bacterial metabolites. J. Dairy. Sci. 2008, 91, 3834–3839. [Google Scholar] [CrossRef]
- Kelsey, J.A.; Bayles, K.W.; Shafii, B.; Mcguire, M.A. Fatty acids and monoacylglycerols inhibit growth of Staphylococcus aureus. Lipids 2006, 41, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Bhattarai, D.; Worku, T.; Dad, R.; Rehman, Z.U.; Gong, X.; Zhang, S. Mechanism of pattern recognition receptors (PRRs) and host pathogen interplay in bovine mastitis. Microb. Pathog. 2018, 120, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Turk, R.; Koledic, M.; Macesic, N.; Benic, M.; Dobranic, V.; Duricic, D.; Cvetnic, L.; Samardzija, M. The role of oxidative stress and inflammatory response in the pathogenesis of mastitis in dairy cows. Mljekarstvo 2017, 67, 91–101. [Google Scholar] [CrossRef]
- Zhang, K.; Zhang, M.; Su, H.; Zhao, F.; Wang, D.; Zhang, Y.; Cao, G.; Zhang, Y. Regulation of Inflammatory Responses of Cow Mammary Epithelial Cells through MAPK Signaling Pathways of IL-17A Cytokines. Animals 2024, 14, 1572. [Google Scholar] [CrossRef] [PubMed]
- Sordillo, L.M.; Streicher, K.L. Mammary gland immunity and mastitis susceptibility. J. Mammary Gland. Biol. Neoplasia 2002, 7, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Ezzat, A.M.; Quintela-Baluja, M.; Bohme, K.; Fernandez-No, I.; Caamano-Antelo, S.; Calo-Mata, P.; Barros-Velazquez, J. The immunology of mammary gland of dairy ruminants between healthy and inflammatory conditions. J. Vet. Med. 2014, 2014, 659801. [Google Scholar] [CrossRef]
- Damm, M.; Holm, C.; Blaabjerg, M.; Bro, M.N.; Schwarz, D. Differential somatic cell count-A novel method for routine mastitis screening in the frame of Dairy Herd Improvement testing programs. J. Dairy. Sci. 2017, 100, 4926–4940. [Google Scholar] [CrossRef] [PubMed]
- Wittek, T.; Mader, C.; Ribitsch, V.; Burgstaller, J. Measurement of oxygen concentration for detection of subclinical mastitis. Schweiz. Arch. Tierheilkd. 2019, 161, 659–665. [Google Scholar] [CrossRef] [PubMed]
- She, Y.; Liu, J.; Su, M.; Li, Y.; Guo, Y.; Liu, G.; Deng, M.; Qin, H.; Sun, B.; Guo, J.; et al. A study on differential biomarkers in the milk of holstein cows with different somatic cells count levels. Animals 2023, 13, 2446. [Google Scholar] [CrossRef]
- Wang, Y.; Nan, X.; Zhao, Y.; Wang, H.; Wang, M.; Jiang, L.; Zhang, F.; Xue, F.; Hua, D.; Li, K.; et al. Coupling 16S rDNA sequencing and untargeted mass spectrometry for milk microbial composition and metabolites from dairy cows with clinical and subclinical mastitis. J. Agric. Food. Chem. 2020, 68, 8496–8508. [Google Scholar] [CrossRef]
- Saila, S.; Bork, O.; Tucker, I.G.; Cranefield, S.; Bryan, M.A. Evaluation of an on-farm culture system for the detection of subclinical mastitis pathogens in dairy cattle. JDS Commun. 2023, 4, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Mansion-De, V.E.; Knorr, N.; Paduch, J.H.; Zinke, C.; Hoedemaker, M.; Kromker, V. A field study evaluation of petrifilm plates as a 24-h rapid diagnostic test for clinical mastitis on a dairy farm. Prev. Vet. Med. 2014, 113, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Kahya, D.S.; Yildiz, M.; Akkoc, A.; Mutlu, A.M.; Ardicli, O.; Aner, H. Comparison of bacteriological culture method and multiplex real-time PCR for detection of mastitis. Res. Vet. Sci. 2024, 172, 105237. [Google Scholar] [CrossRef] [PubMed]
- Bhutto, A.L.; Murray, R.D.; Woldehiwet, Z. California mastitis test scores as indicators of subclinical intra-mammary infections at the end of lactation in dairy cows. Res. Vet. Sci. 2012, 92, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Wollowski, L.; Bertulat, S.; Kossatz, A.; Heuwieser, W. Short communication: Diagnosis and classification of clinical and subclinical mastitis utilizing a dynamometer and a handheld infrared thermometer. J. Dairy Sci. 2019, 102, 6532–6539. [Google Scholar] [CrossRef] [PubMed]
- Mota-Rojas, D.; Pereira, A.M.F.; Wang, D.; Martínez-Burnes, J.; Ghezzi, M.; Hernández-Avalos, I.; Lendez, P.; Mora-Medina, P.; Casas, A.; Olmos-Hernández, A. Clinical Applications and Factors Involved in Validating Thermal Windows Used in Infrared Thermography in Cattle and River Buffalo to Assess Health and Productivity. Animals 2021, 11, 2247. [Google Scholar] [CrossRef]
- Carvalho-Sombra, T.; Fernandes, D.D.; Bezerra, B.; Nunes-Pinheiro, D. Systemic inflammatory biomarkers and somatic cell count in dairy cows with subclinical mastitis. Vet. Anim. Sci. 2021, 11, 100165. [Google Scholar] [CrossRef] [PubMed]
- Usui, M.; Akiyoshi, M.; Fukuda, A.; Iwano, H.; Kato, T. 16S rRNA nanopore sequencing for rapid diagnosis of causative bacteria in bovine mastitis. Res. Vet. Sci. 2023, 161, 45–49. [Google Scholar] [CrossRef]
- Schukken, Y.H.; Wilson, D.J.; Welcome, F.; Garrison-Tikofsky, L.; Gonzalez, R.N. Monitoring udder health and milk quality using somatic cell counts. Vet. Res. 2003, 34, 579–596. [Google Scholar] [CrossRef]
- Ruegg, P.L.; Pantoja, J.C.E. Understanding and using somatic cell counts to improve milk quality. Ir. J. Agric. Food Res. 2013, 52, 101–117. [Google Scholar]
- Ashraf, A.; Imran, M. Diagnosis of bovine mastitis: From laboratory to farm. Trop. Anim. Health Prod. 2018, 50, 1193–1202. [Google Scholar] [CrossRef] [PubMed]
- Soltau, J.B.; Einax, E.; Klengel, K.; Katholm, J.; Failing, K.; Wehrend, A.; Donat, K. Within-herd prevalence thresholds for herd-level detection of mastitis pathogens using multiplex real-time PCR in bulk tank milk samples. J. Dairy. Sci. 2017, 100, 8287–8295. [Google Scholar] [CrossRef] [PubMed]
- Adkins, P.R.F.; Middleton, J.R. Methods for diagnosing mastitis. Vet. Clin. N. Am. Food. Anim. Pract. 2018, 34, 479. [Google Scholar] [CrossRef] [PubMed]
- Pyoeraelae, S.U.O.H. Indicators of inflammation in the diagnosis of mastitis. Vet. Res. 2003, 34, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Hogeveen, H.; Klaas, I.C.; Dalen, G.; Honig, H.; Zecconi, A.; Kelton, D.F.; Sanchez, M.M. Novel ways to use sensor data to improve mastitis management. J. Dairy. Sci. 2021, 104, 11317–11332. [Google Scholar] [CrossRef] [PubMed]
- Colak, A.; Polat, B.; Okumus, Z.; Kaya, M.; Yanmaz, L.E.; Hayirli, A. Short communication: Early detection of mastitis using infrared thermography in dairy cows. J. Dairy. Sci. 2008, 91, 4244–4248. [Google Scholar] [CrossRef] [PubMed]
- Goldansaz, S.A.; Guo, A.C.; Sajed, T.; Steele, M.A.; Plastow, G.S.; Wishart, D.S. Livestock metabolomics and the livestock metabolome: A systematic review. PLoS ONE 2017, 12, e0177675. [Google Scholar] [CrossRef] [PubMed]
- Foroutan, A.; Guo, A.C.; Vazquez-Fresno, R.; Lipfert, M.; Zhang, L.; Zheng, J.; Badran, H.; Budinski, Z.; Mandal, R.; Ametaj, B.N.; et al. Chemical composition of commercial cow’s milk. Agric. Food. Chem. 2019, 67, 4897–4914. [Google Scholar] [CrossRef] [PubMed]
- Thomas, F.C.; Mudaliar, M.; Tassi, R.; Mcneilly, T.N.; Burchmore, R.; Burgess, K.; Herzyk, P.; Zadoks, R.N.; Eckersall, P.D. Mastitomics, the integrated omics of bovine milk in an experimental model of Streptococcus uberis mastitis: 3. Untargeted metabolomics. Mol. Biosyst. 2016, 12, 2762–2769. [Google Scholar] [CrossRef]
- Bansal, B.K.; Hamann, J.; Grabowskit, N.T.; Singh, K.B. Variation in the composition of selected milk fraction samples from healthy and mastitic quarters, and its significance for mastitis diagnosis. J. Dairy. Res. 2005, 72, 144–152. [Google Scholar] [CrossRef]
- Sundekilde, U.K.; Poulsen, N.A.; Larsen, L.B.; Bertram, H.C. Nuclear magnetic resonance metabonomics reveals strong association between milk metabolites and somatic cell count in bovine milk. J. Dairy. Sci. 2013, 96, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Mudaliar, M.; Tassi, R.; Thomas, F.C.; Mcneilly, T.N.; Weidt, S.K.; Mclaughlin, M.; Wilson, D.; Burchmore, R.; Herzyk, P.; Eckersall, P.D.; et al. Mastitomics, the integrated omics of bovine milk in an experimental model of Streptococcus uberis mastitis: 2. Label-free relative quantitative proteomics. Mol. Biosyst. 2016, 12, 2748–2761. [Google Scholar] [CrossRef] [PubMed]
- Rios-Covian, D.; Ruas-Madiedo, P.; Margolles, A.; Gueimonde, M.; de Los Reyes-Gavilan, C.G.; Salazar, N. Intestinal short Chain fatty acids and their link with diet and human health. Front. Microbiol. 2016, 7, 180861. [Google Scholar] [CrossRef] [PubMed]
- Luangwilai, M.; Duangmal, K.; Chantaprasarn, N.; Settachaimongkon, S. Comparative metabolite profiling of raw milk from subclinical and clinical mastitis cows using 1H-NMR combined with chemometric analysis. Int. J. Food Sci. Technol. 2021, 56, 493–503. [Google Scholar] [CrossRef]
- Xi, X.; Kwok, L.Y.; Wang, Y.; Ma, C.; Mi, Z.; Zhang, H. Ultra-performance liquid chromatography-quadrupole-time of flight mass spectrometry MSE-based untargeted milk metabolomics in dairy cows with subclinical or clinical mastitis. J. Dairy. Sci. 2017, 100, 4884–4896. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Khan, M.Z.; Kou, X.; Chen, Y.; Liang, H.; Ullah, Q.; Khan, N.; Khan, A.; Chai, W.; Wang, C. Enhancing metabolism and milk production performance in periparturient dairy cattle through rumen-protected methionine and choline supplementation. Metabolites 2023, 13, 1080. [Google Scholar] [CrossRef]
- Zhu, C.; Tang, K.; Lu, X.; Tang, J.; Laghi, L. An untargeted metabolomics investigation of milk from dairy cows with clinical mastitis by 1H-NMR. Foods 2021, 10, 1707. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.; Zhang, H.; Zhang, Y.; Xiong, B.; Jiang, L. Microbiome and metabolome analyses of milk from dairy cows with subclinical streptococcus agalactiae mastitis-potential biomarkers. Front. Microbiol. 2019, 10, 2547. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.R.; Farr, V.C.; Prosser, C.G.; Nicholas, G.D.; Turner, S.A.; Lee, J.; Hart, A.L. Milk L-lactate concentration is increased during mastitis. J. Dairy Res. 2004, 71, 175–181. [Google Scholar] [CrossRef]
- Xi, X.M. Microbial Diversity and Metabolomics Studies on Milk during Bovine Mastitis. Doctoral Thesis, Inner Mongolia Agricultural University, Huhhot, China, 2016. [Google Scholar]
- Sundekilde, U.K.; Frederiksen, P.D.; Clausen, M.R.; Larsen, L.B.; Bertram, H.C. Relationship between the Metabolite Profile and Technological Properties of Bovine Milk from Two Dairy Breeds Elucidated by NMR-Based Metabolomics. J. Agric. Food Chem. 2011, 59, 7360–7367. [Google Scholar] [CrossRef]
- Zhou, L.; Wang, Q.; Yin, P.; Xing, W.; Wu, Z.; Chen, S.; Lu, X.; Zhang, Y.; Lin, X.; Xu, G. Serum metabolomics reveals the deregulation of fatty acids metabolism in hepatocellular carcinoma and chronic liver diseases. Anal. Bioanal. Chem. 2012, 403, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Caggiano, N.; Smirnoff, A.L.; Bottini, J.M.; De Simone, E.A. Protease activity and protein profile in milk from healthy dairy cows and cows with different types of mastitis. Int. Dairy J. 2019, 89, 1–5. [Google Scholar] [CrossRef]
- Wedholm, A.; Moller, H.S.; Lindmark-Mansson, H.; Rasmussen, M.D.; Andren, A.; Larsen, L.B. Identification of peptides in milk as a result of proteolysis at different levels of somatic cell counts using LC MALDI MS/MS detection. J. Dairy Res. 2008, 75, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Qu, K.C. 1H nuclear Magnetic Resonance-Based Metabonomics on Early-Stage Diagnosis of Dairy Cow Mastitis. Doctoral Thesis, Northeast Agricultural University, Haerbin, China, 2020. [Google Scholar]
- Ryman, V.E.; Pighetti, G.M.; Lippolis, J.D.; Gandy, J.C.; Applegate, C.M.; Sordillo, L.M. Quantification of bovine oxylipids during intramammary Streptococcus uberis infection. Prostaglandins Other Lipid Mediat. 2015, 121, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Demicheva, E.; Dordiuk, V.; Espino, F.P.; Ushenin, K.; Aboushanab, S.; Shevyrin, V.; Buhler, A.; Mukhlynina, E.; Solovyova, O.; Danilova, I.; et al. Advances in mass spectrometry-based blood metabolomics profiling for non-cancer diseases: A comprehensive review. Metabolites 2024, 14, 54. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Zhang, Q.; Zhao, X.; Yang, Z.; Yang, F.; Yang, Y.; Tang, J.; Laghi, L. Metabolomic analysis of multiple biological specimens (feces, serum, and urine) by (1)H-NMR spectroscopy from dairy cows with clinical mastitis. Animals 2023, 13, 741. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Zhang, Z.; Lu, H.; Jin, Y.; Yi, L.; Liang, Y. Joint MS-based platforms for comprehensive comparison of rat plasma and serum metabolic profiling. Biomed. Chromatogr. 2014, 28, 1235–1245. [Google Scholar] [CrossRef]
- Yu, Z.; Kastenmuller, G.; He, Y.; Belcredi, P.; Moller, G.; Prehn, C.; Mendes, J.; Wahl, S.; Roemisch-Margl, W.; Ceglarek, U.; et al. Differences between human plasma and serum metabolite profiles. PLoS ONE 2011, 6, e21230. [Google Scholar] [CrossRef] [PubMed]
- Hurley, W.L.; Theil, P.K. Perspectives on immunoglobulins in colostrum and milk. Nutrients 2011, 3, 442–474. [Google Scholar] [CrossRef]
- Khatun, M.; Clark, C.E.F.; Lyons, N.A.; Thomson, P.C.; Kerrisk, K.L.; Garcia, S.C. Early detection of clinical mastitis from electrical conductivity data in an automatic milking system. Anim. Prod. Sci. 2017, 57, 1226–1232. [Google Scholar] [CrossRef]
- Dervishi, E.; Zhang, G.; Dunn, S.M.; Mandal, R.; Wishart, D.S.; Ametaj, B.N. GC-MS metabolomics identifies metabolite alterations that precede subclinical mastitis in the blood of transition dairy cows. J. Proteome Res. 2017, 16, 433–446. [Google Scholar] [CrossRef]
- Haxhiaj, K.; Li, Z.; Johnson, M.; Dunn, S.M.; Wishart, D.S.; Ametaj, B.N. Blood metabolomic phenotyping of dry cows could predict the high milk somatic cells in early lactation—Preliminary results. Dairy 2022, 3, 59–77. [Google Scholar] [CrossRef]
- Zhang, G.; Tobolski, D.; Zwierzchowski, G.; Mandal, R.; Wishart, D.S.; Ametaj, B.N. Identification of serum-predictive biomarkers for subclinical mastitis in dairy cows and new insights into the pathobiology of the disease. J. Agric. Food. Chem. 2022, 70, 1724–1746. [Google Scholar] [CrossRef]
- Nakamura, T.; Kawase, H.; Kimura, K.; Watanabe, Y.; Ohtani, M.; Arai, I.; Urashima, T. Concentrations of sialyloligosaccharides in bovine colostrum and milk during the prepartum and early lactation. J. Dairy. Sci. 2003, 86, 1315–1320. [Google Scholar] [CrossRef]
- Ten, B.S.; Bovee-Oudenhoven, I.M.; Feitsma, A.L.; van Hoffen, E.; Schoterman, M.H. Functional role and mechanisms of sialyllactose and other sialylated milk oligosaccharides. Nutr. Rev. 2014, 72, 377–389. [Google Scholar] [CrossRef]
- Zandkarimi, F.; Vanegas, J.; Fern, X.; Maier, C.S.; Bobe, G. Metabotypes with elevated protein and lipid catabolism and inflammation precede clinical mastitis in prepartal transition dairy cows. J. Dairy. Sci. 2018, 101, 5531–5548. [Google Scholar] [CrossRef]
- Johnzon, C.F.; Dahlberg, J.; Gustafson, A.M.; Waern, I.; Moazzami, A.A.; Ostensson, K.; Pejler, G. The effect of lipopolysaccharide-induced experimental bovine mastitis on clinical parameters, inflammatory markers, and the metabolome: A kinetic approach. Front. Immunol. 2018, 9, 1487. [Google Scholar] [CrossRef] [PubMed]
- Lisuzzo, A.; Laghi, L.; Fiore, E.; Cecchinato, A.; Bisutti, V.; Pegolo, S.; Giannuzzi, D.; Tessari, R.; Barberio, A.; Schiavon, E.; et al. Serum metabolome differences associated with subclinical intramammary infection caused by Streptococcus agalactiae and Prototheca spp. in multiparous dairy cows. J. Dairy. Sci. 2024, 107, 1656–1668. [Google Scholar] [CrossRef]
- Wang, Y.; Nan, X.; Zhao, Y.; Jiang, L.; Wang, H.; Zhang, F.; Hua, D.; Liu, J.; Yang, L.; Yao, J.; et al. Discrepancies among healthy, subclinical mastitic, and clinical mastitic cows in fecal microbiome and metabolome and serum metabolome. J. Dairy. Sci. 2022, 105, 7668–7688. [Google Scholar] [CrossRef]
- Hao, D.; Bai, J.; Du, J.; Wu, X.; Thomsen, B.; Gao, H.; Su, G.; Wang, X. Overview of metabolomic analysis and the integration with multi-omics for economic traits in cattle. Metabolites 2021, 11, 753. [Google Scholar] [CrossRef]
- Chen, J.; Amdanee, N.; Zuo, X.; Wang, Y.; Gong, M.; Yang, Y.; Li, H.; Zhang, X.; Zhang, C. Biomarkers of bipolar disorder based on metabolomics: A systematic review. J. Affect. Disord. 2024, 350, 492–503. [Google Scholar] [CrossRef] [PubMed]
- Zwierzchowski, G.; Zhang, G.; Mandal, R.; Wishart, D.S.; Ametaj, B.N. Mass-spec-based urinary metabotyping around parturition identifies screening biomarkers for subclinical mastitis in dairy cows. Res. Vet. Sci. 2020, 129, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Lunsin, R.; Wanapat, M.; Rowlinson, P. Effect of cassava hay and rice bran oil supplementation on rumen fermentation, milk yield and milk composition in lactating dairy cows. Asian Australas. J. Anim. Sci. 2012, 25, 1364–1373. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Nan, X.; Zhao, Y.; Jiang, L.; Wang, M.; Wang, H.; Zhang, F.; Xue, F.; Hua, D.; Liu, J.; et al. Rumen microbiome structure and metabolites activity in dairy cows with clinical and subclinical mastitis. J. Anim. Sci. Biotechnol. 2021, 12, 36. [Google Scholar] [CrossRef]
- Zhu, Y.; Bu, D.; Ma, L. Integration of multiplied omics, a step forward in systematic dairy research. Metabolites 2022, 12, 225. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Li, Z.; Deng, M.; Liu, D.; Sun, B.; Liu, J.; Guo, J.; Guo, Y. Overview of Bovine Mastitis: Application of Metabolomics in Screening Its Predictive and Diagnostic Biomarkers. Animals 2024, 14, 2264. https://doi.org/10.3390/ani14152264
Li M, Li Z, Deng M, Liu D, Sun B, Liu J, Guo J, Guo Y. Overview of Bovine Mastitis: Application of Metabolomics in Screening Its Predictive and Diagnostic Biomarkers. Animals. 2024; 14(15):2264. https://doi.org/10.3390/ani14152264
Chicago/Turabian StyleLi, Muyang, Zhongjie Li, Ming Deng, Dewu Liu, Baoli Sun, Jianying Liu, Jianchao Guo, and Yongqing Guo. 2024. "Overview of Bovine Mastitis: Application of Metabolomics in Screening Its Predictive and Diagnostic Biomarkers" Animals 14, no. 15: 2264. https://doi.org/10.3390/ani14152264





