Microbiological and Molecular Investigation of Antimicrobial Resistance in Staphylococcus aureus Isolates from Western Romanian Dairy Farms: An Epidemiological Approach
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Description of Sampling
2.2. Samples and Staphylococcus aureus Isolation
2.3. Confirmation of Staphylococcus aureus and Detection of Antimicrobial Resistance
2.4. DNA Extraction and Detection of Resistance Genes viaq-PCR
2.5. Phenotypic and Genotypic Resistance
- (RG+): Phenotypically resistant and possessing the resistance gene.
- (RG−): Phenotypically resistant but lacking the resistance gene.
- (SG+): Phenotypically susceptible but with the resistance gene.
- (SG−): Phenotypically susceptible and without the resistance gene.
2.6. Statistical Analysis
3. Results
3.1. Epidemiological Results
3.2. Microbiological Antibiotic Resistance and Susceptibility Testing (AST)
3.3. Prevalence of Resistance Genes
3.4. Penetrance of the Resistance Genes
3.5. AST Diagnostic Odds Ratio of Positive Phenotypic Resistance (DOR)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Klaas, I.C.; Zadoks, R.N. An update on environmental mastitis: Challenging perceptions. Transbound. Emerg. Dis. 2018, 65 (Suppl. S1), 166–185. [Google Scholar] [CrossRef] [PubMed]
- Campos, B.; Pickering, A.C.; Rocha, L.S.; Aguilar, A.P.; Fabres-Klein, M.H.; de Oliveira Mendes, T.A.; Fitzgerald, J.R.; de Oliveira Barros Ribon, A. Diversity and pathogenesis of Staphylococcus aureus from bovine mastitis: Current understanding and future perspectives. BMC Vet. Res. 2022, 18, 115. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.; Henriques, M. Control of bovine mastitis: Old and recent therapeutic approaches. Curr. Microbiol. 2016, 72, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Petrovski, K.; Trajcev, M.; Buneski, G. A review of the factors affecting the costs of bovine mastitis: Review article. J. S. Afr. Vet. Assoc. 2006, 77, 52–60. [Google Scholar] [CrossRef]
- Hillerton, J.E.; Berry, E.A. Treating mastitis in the cow–a tradition or an archaism. J. Appl. Microbiol. 2005, 98, 1250–1255. [Google Scholar] [CrossRef] [PubMed]
- Huijps, K.; Lam, T.; Hogeveen, H. Costs of mastitis: Facts and perception. J. Dairy Res. 2008, 75, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Viguier, C.; Arora, S.; Gilmartin, N.; Welbeck, K.; O’Kennedy, R. Mastitis detection: Current trends and future perspectives. Trends Biotechnol. 2009, 27, 486–493. [Google Scholar] [CrossRef] [PubMed]
- Hogeveen, H.; Steeneveld, W.; Wolf, C.A. Production diseases reduce the efficiency of dairy production: A review of the results, methods, and approaches regarding the economics of mastitis. Annu. Rev. Resour. Econ. 2019, 11, 289–312. [Google Scholar] [CrossRef]
- Zhao, X.; Lacasse, P. Mammary tissue damage during bovine mastitis: Causes and control. J. Anim. Sci. 2008, 86, 57–65. [Google Scholar] [CrossRef]
- Cobirka, M.; Tancin, V.; Slama, P.E. Epidemiology and classification of mastitis. Animals 2020, 10, 2212. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lakew, B.T.; Fayera, T.; Ali, Y.M. Risk factors for bovine mastitis with the isolation and identification of Streptococcus agalactiae from farms in and around Haramaya district, eastern Ethiopia. Trop. Anim. Health Prod. 2019, 51, 1507–1513. [Google Scholar] [CrossRef]
- Schreiner, D.; Ruegg, P.L. E Effects of tail docking on milk quality and cow cleanliness. J Dairy Sci. 2002, 85, 2503–2511. [Google Scholar] [CrossRef] [PubMed]
- Hutu, I.; Chis, C.; Tulcan, C.; Mircu, C. Associated factors to mastitis in cows voluntary milking system. J. Biotechnol. 2014, 185, S50–S51. [Google Scholar] [CrossRef]
- Kibebew, K. Bovine mastitis: A review of causes and epidemiological point of view. J. Biol. Agric. Healthc. 2017, 7, 1–14. [Google Scholar]
- Abril, G.A.G.; Villa, T.; Barros-Velázquez, J.; Cañas, B.; Sánchez-Pérez, A.; Calo-Mata, P.; Carrera, M. Staphylococcus aureus exotoxins and their detection in the dairy industry and mastitis. Toxins 2020, 12, 537. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lowy, F.D. Staphylococcus aureus Infections. New Engl. J. Med. 1998, 339, 520–532. [Google Scholar] [CrossRef] [PubMed]
- Sukumar, D.; Vanan, T.T.; Thennarasu, A.; Kumar, T. T The Effect of teat protect spray and potassium permanganate teat dip in curing subclinical mastitis in crossbred cows of Villupuram district of Tamilnadu. J. Appl. Nat. Sci. 2019, 11, 738–742. [Google Scholar] [CrossRef]
- Vissio, C.; Mella, A.; Amestica, L.; Pol, M. Noninferiority study evaluating the efficacy of a teat disinfectant containing copper and zinc for prevention of naturally occurring intramammary infections in an automatic milking system. J. Dairy Sci. 2019, 103, 1776–1784. [Google Scholar] [CrossRef] [PubMed]
- Miseikiene, R.; Tusas, S.; Biziene, R.; Kerziene, S.; Miciński, J.; Matusevicius, P. Influence of teat disinfection with iodine preparation on bacterial contamination of teats, hygenic quality and content of iodine in milk. J. Elem. 2020, 25, 225–236. [Google Scholar]
- Zadoks, R.N.; Allore, H.G.; Barkema, H.W.; Sampimon, O.C.; Wellenberg, G.J.; Gröhn, Y.T.; Schukken, Y.H. Cow- and quarter-level risk factors for Streptococcus uberis and Staphylococcus aureus mastitis. J. Dairy Sci. 2001, 84, 2649–2663. [Google Scholar] [CrossRef]
- Gleeson, D.; Flynn, J.; Brien, B.O. Effect of pre-milking teat disinfection on new mastitis infection rates of dairy cows. Ir. Veter J. 2018, 71, 11. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, S.R.; Garvey, M.; Flynn, J.; O’Brien, B.; Gleeson, D. Effect of pre-milking teat foam disinfection on the prevention of new mastitis rates in early lactation. Animals 2021, 11, 2582. [Google Scholar] [CrossRef]
- Sharun, K.; Dhama, K.; Tiwari, R.; Gugjoo, M.B.; Yatoo, M.I.; Patel, S.K.; Pathak, M.; Karthik, K.; Khurana, S.K.; Singh, R.; et al. Advances in therapeutic and managemental approaches of bovine mastitis: A comprehensive review. Vet. Q. 2021, 41, 107–136. [Google Scholar] [CrossRef] [PubMed]
- Nale, J.Y.; McEwan, N.R. Bacteriophage therapy to control bovine mastitis: A review. Antibiotics 2023, 12, 1307. [Google Scholar] [CrossRef] [PubMed]
- Jamali, H.; Radmehr, B.; Ismail, S. Short communication: Prevalence and antibiotic resistance of Staphylococcus aureus isolated from bovine clinical mastitis. J. Dairy Sci. 2014, 97, 2226–2230. [Google Scholar] [CrossRef]
- Jagielski, T.; Puacz, E.; Lisowski, A.; Siedlecki, P.; Dudziak, W.; Międzobrodzki, J.; Krukowski, H. Short communication: Antimicrobial susceptibility profiling and genotyping of Staphylococcus aureus isolates from bovine mastitis in Poland. J. DairySci. 2014, 97, 6122–6128. [Google Scholar] [CrossRef]
- O’dea, M.; Abraham, R.J.; Sahibzada, S.; Lee, T.; Jordan, D.; Laird, T.; Pang, S.; Buller, N.; Stegger, M.; Coombs, G.W.; et al. Antimicrobial resistance and genomic insights into bovine mastitis-associated Staphylococcus aureus in Australia. Vet. Microbiol. 2020, 250, 108850. [Google Scholar] [CrossRef]
- Bolte, J.; Zhang, Y.; Wente, N.; Mahmmod, Y.S.; Svennesen, L.; Krömker, V. Comparison of phenotypic and genotypic antimicrobial resistance patterns associated with Staphylococcus aureus mastitis in German and Danish dairy cows. J. Dairy Sci. 2020, 103, 3554–3564. [Google Scholar] [CrossRef]
- Naranjo-Lucena, A.; Slowey, R. Invited review: Antimicrobial resistance in bovine mastitis pathogens: A review of genetic determinants and prevalence of resistance in European countries. J. Dairy Sci. 2023, 106, 1–23. [Google Scholar] [CrossRef]
- Hendriksen, R.S.; Mevius, D.J.; Schroeter, A.; Teale, C.; Meunier, D.; Butaye, P.; Franco, A.; Utinane, A.; Amado, A.; Moreno, M.; et al. Prevalence of antimicrobial resistance among bacterial pathogens isolated from cattle in different European countries 2002-2004. Acta Vet. Scand. 2008, 50, 28. [Google Scholar] [CrossRef]
- Vintov, J.; Aarestrup, F.M.; Zinn, C.E.; Olsen, J.E. Association between phage types and antimicrobial resistance among bovine Staphylococcus aureus from 10 countries. Vet. Microbiol. 2003, 95, 133–147. [Google Scholar] [CrossRef] [PubMed]
- Molineri, A.I.; Camussone, C.; Zbrun, M.V.; Archilla, G.S.; Cristiani, M.; Neder, V.; Calvinho, L.; Signorini, M. Antimicrobial resistance of Staphylococcus aureus isolated from bovine mastitis: Systematic review and meta-analysis. Prev. Vet. Med. 2021, 188, 105261. [Google Scholar] [CrossRef] [PubMed]
- Pol, M.; Ruegg, P.L. Relationship between antimicrobial drug usage and antimicrobial susceptibility of gram-positive mastitis pathogens. J. Dairy Sci. 2007, 90, 262–273. [Google Scholar] [CrossRef]
- Nielsen, C. Economic Impact of Mastitis in Dairy Cows. Ph.D. Thesis, Swedish University of Agricultural Sciences, Uppsala, Sweden, 2009. [Google Scholar]
- Oliver, S.P.; Murinda, S.E.; Jayarao, B.M. Impact of antibiotic use in adult dairy cows on antimicrobial resistance of veterinary and human pathogens: A comprehensive review. Foodborne Pathog. Dis. 2011, 8, 337–355. [Google Scholar] [CrossRef] [PubMed]
- Beyene, T.J.; Hayishe, H.; Gizaw, F.; Beyi, A.F.; Abunna, F.; Mammo, B.; Ayana, D.; Waktole, H.; Abdi, R.D. Prevalence and antimicrobial resistance profile of Staphylococcus in dairy farms, abattoir and humans in Addis Ababa, Ethiopia. BMC Res. Notes 2017, 10, 171. [Google Scholar] [CrossRef] [PubMed]
- Pascu, C.; Herman, V.; Iancu, I.; Costinar, L. Etiology of mastitis and antimicrobial resistance in dairy cattle farms in the Western part of Romania. Antibiotics 2022, 11, 57. [Google Scholar] [CrossRef] [PubMed]
- Barrow, P.; Lungu, B.; Brzoska, H.; Mircu, C.; Hutu, I. Antibiotic resistance in enteric infections—Exploring a new approach. Rev. Rom. Med.Vet. 2022, 32, 83–88. [Google Scholar]
- Scherr, T.D.; Hanke, M.L.; Huang, O.; James, D.B.A.; Horswill, A.R.; Bayles, K.W.; Fey, P.D.; Torres, V.J.; Kielian, T. Staphylococcus aureus biofilms induce macrophage dysfunction through leukocidin AB and alpha-toxin. mBio 2015, 6, e01021-15. [Google Scholar] [CrossRef] [PubMed]
- Huijbers, P.M.C. Transmission of Antibiotic Resistance from Animals to Humans: Broilers as a Reservoir of ESBL-Producing Bacteria; Wageningen University: Wageningen, NL, USA, 2016; Available online: https://edepot.wur.nl/366347 (accessed on 25 November 2023).
- De Jong, A.; ElGarch, F.; Simjee, S.; Moyaert, H.; Rose, M.; Youala, M.; Siegwart, E.M. Monitoring of antimicrobial susceptibility of udder pathogens recovered from cases of clinical mastitis in dairy cows across Europe. Vet. Microbiol. 2018, 213, 73–81. [Google Scholar] [CrossRef]
- Kozarsky, P.E.; Rimland, D.; Terry, P.M.; Wachsmuth, K. Plasmid analysis of simultaneous nosocomial outbreaks of methicillin resistant Staphylococcus aureus. Infect. Control 1986, 7, 577–581. [Google Scholar] [CrossRef]
- Cafini, F.; Le, T.T.N.; Higashide, M.; Román, F.; Prieto, J.; Morikawa, K.J. Horizontal gene transmission of the cfr gene to MRSA and Enterococcus: Role of Staphylococcus epidermidis as a reservoir and alternative pathways for the spread of linezolid resistance. Antimicrob. Chemother. 2016, 71, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Varga, M.; Pantu Ček, R.; Žičková, V.R.; Doškar, J. Molecular characterisation of a new efficiently transducing bacteriophage identified in methicillin-resistant Staphylococcus aureus. J. Genet. Virol. 2016, 97, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Mulders, M.N.; Haenen, A.P.J.; Geenen, P.L.; Vesseur, P.C.; Poldervaart, E.S.; Bosch, T.; Huijsdens, X.W.; Hengeveld, P.D.; Dam-Deisz, W.D.C.; Graat, E.A.M.; et al. Prevalence of livestock-associated MRSA in broiler flocks and risk factors for slaughterhouse personnel in the Netherlands. Epidemiol. Infect. 2010, 138, 743–755. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Global Action Plan on Antimicrobial Resistance; World Health Organisation: Geneva, Switzerland, 2015.
- Moruzi, R.F.; Tirziu, E.; Muselin, F.; Dumitrescu, E.; Huțu, I.; Mircu, C.; Tulcan, C.; Doma, A.O.; Degi, J.; Degi, D.M.; et al. The importance of databases to manage the phenomenon of resistance to antimicrobials for veterinary use. Rev. Rom. Med. Vet. 2019, 29, 40–57. [Google Scholar]
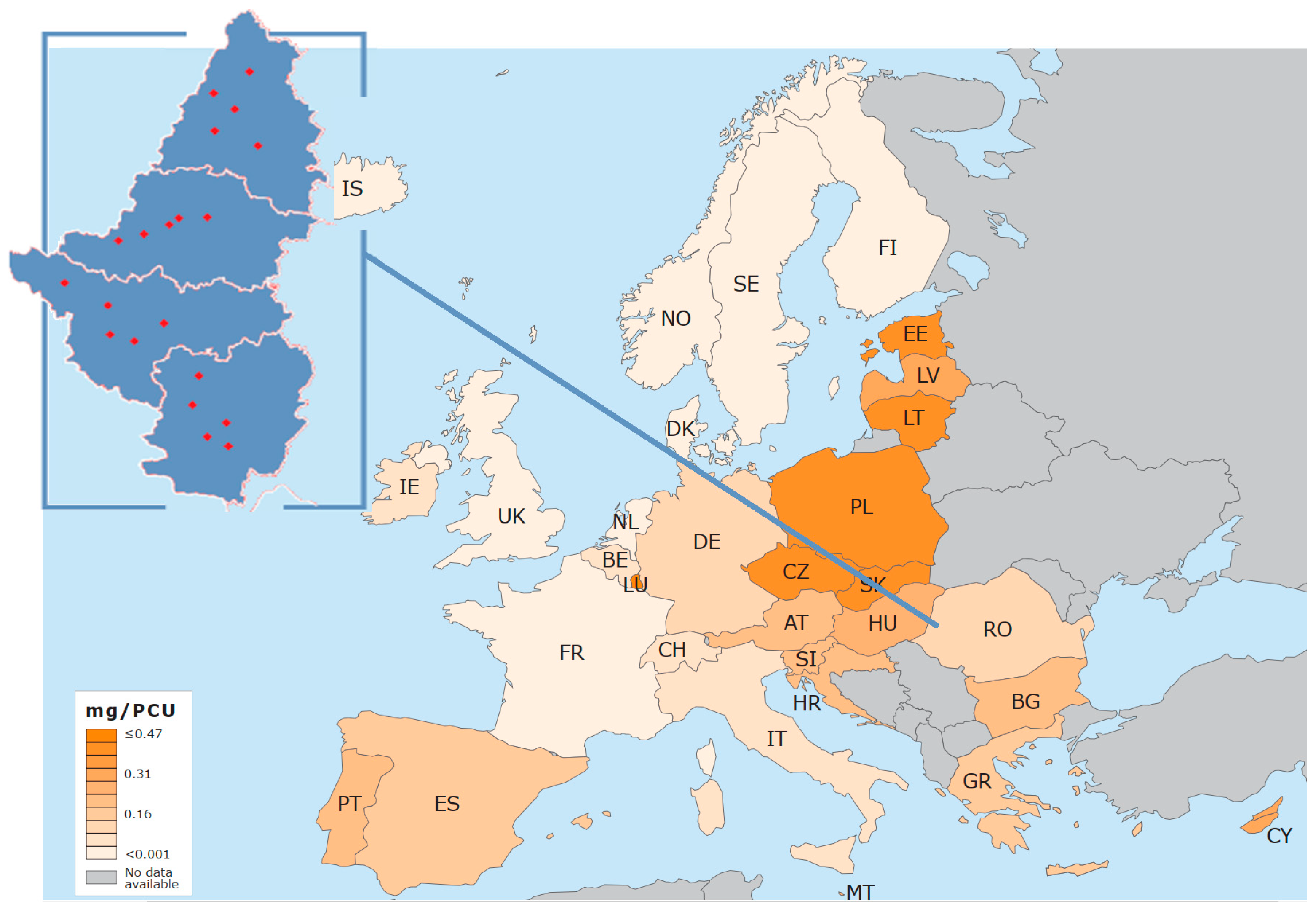
- European Medicines Agency. Available online: https://www.ema.europa.eu/en/documents/report/romania-sales-trends-mgpcu-antibiotic-veterinary-medicinal-products-food-producing-animals-2010-2021_en.pdf (accessed on 20 October 2023).
- European Medicines Agency. Sales of Veterinary Antimicrobial agents in 31 European Countries in 2022-Trends from 2010 to 2022-Thirteenth ESVAC Report. Available online: https://european-union.europa.eu/index_en (accessed on 20 October 2023).
- Abdolmaleki, Z.; Mashak, Z.; Dehkordi, F.S. Phenotypic and genotypic characterization of antibiotic resistance in the methicillin-resistant Staphylococcus aureus strains isolated from hospital cockroaches. Antimicrob. Resist. Infect. Control. 2019, 8, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kehrenberg, C.; Schwarz, S. Distribution of florfenicol resistance genes fexA and cfr among chloramphenicol-resistant Staphylococcus isolates. Antimicrob. Agents Chemother. 2006, 50, 1156–1163. [Google Scholar] [CrossRef]
- Malhotra-Kumar, S.; Lammens, C.; Piessens, J.; Goossens, H. Multiplex PCR for simultaneous detection of macrolide and tetracycline resistance determinants in streptococci. Antimicrob Agents Chemother. 2005, 49, 4798–4800. [Google Scholar] [CrossRef] [PubMed]
- Klare, I.; Konstabel, C.; Werner, G.; Huys, G.; Vankerckhoven, V.; Kahlmeter, G.; Hildebrandt, B.; Müller-Bertling, S.; Witte, W.; Goossens, H. Antimicrobial susceptibilities of Lactobacillus, Pediococcus and Lactococcus human isolates and cultures intended for probiotic or nutritional use. J. Antimicrob. Chemother. 2007, 59, 900–912. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H. Methicillin (Oxacillin)-resistant Staphylococcus aureus strains isolated from major food animals and their potential transmission to humans. Appl. Environ. Microbiol. 2003, 69, 6489–6494. [Google Scholar] [CrossRef]
- Nassar, M.S.M.; Hazzah, W.A.; Bakr, W.M.K. Evaluation of antibiotic susceptibility test results: How guilty a laboratory could be? J. Egypt. Public Health Assoc. 2019, 94, 1–5. [Google Scholar] [CrossRef]
- Lungu, B.C.; Hutu, I.; Barrow, P.A. Molecular characterisation of antimicrobial resistance in e. coli isolates from piglets in the West Region of Romania. Antibiotics 2023, 12, 1544. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, L.E.; Rosenberg, D.D. Chapter 5: Transmission of Genes. In Human Genes and Genomes; Rosenberg, L.E., Rosenberg, D.D., Eds.; Academic Press: Cambridge, MA, USA, 2012; pp. 51–73. [Google Scholar]
- Eldar, A.L.; Chary, V.K.; Xenopoulos, P.; Fontes, M.E.; Losón, O.C.; Dworkin, J.; Piggot, P.J.; Elowitz, M.B. Partial penetrance facilitates developmental evolution in bacteria. Nature 2009, 460, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Leinyuy, J.F.; Ali, I.M.; Ousenu, K.; Tume, C.B. Molecular characterization of antimicrobial resistance related genes in E. coli, Salmonella and Klebsiella isolates from broilers in the West Region of Cameroon. PLoS ONE 2023, 18, e0280150. [Google Scholar] [CrossRef]
- Krumperman, P.H. Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl. Environ. Microbiol. 1983, 46, 165–170. [Google Scholar] [CrossRef]
- Silva, N.C.C.; Guimarães, F.F.; DeManzi, M.D.; Gómez-Sanz, E.; Gómez, P.; Araújo-Júnior, J.P.; Langoni, H.; Rall, V.L.M.; Torres, C. Characterization of methicillin-resistant coagulase-negative staphylococci in milk from cows with mastitis in Brazil. Antonie Leeuwenhoek 2014, 106, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Thomson, P.; García, P.; Miles, J.; Isla, D.; Yáñez, C.; Santibáñez, R.; Núñez, A.; Flores-Yáñez, C.; DelRío, C.; Cuadra, F. Isolation and Identification of Staphylococcus Species Obtained from Healthy Companion Animals and Humans. Vet. Sci. 2022, 9, 79. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nobrega, D.B.; De Buck, J.; Naqvi, S.A.; Liu, G.; Naushad, S.; Saini, V.; Barkema, H.W. Comparison of treatment records and inventory of empty drug containers to quantify antimicrobial usage in dairy herds. J. Dairy Sci. 2017, 100, 9736–9745. [Google Scholar] [CrossRef] [PubMed]
- Neelam, J.V.K.; Singh, M.; Joshi, V.G.; Chhabra, R.; Singh, K.; Rana, Y.S. Virulence and antimicrobial resistance gene profiles of Staphylococcus aureus associated with clinical mastitis in cattle. PLoS ONE 2022, 17, e0264762. [Google Scholar] [CrossRef] [PubMed]
- Cortimiglia, C.; Luini, M.; Bianchini, V.; Marzagalli, L.; Vezzoli, F.; Avisani, D.; Bertoletti, M.; Ianzano, A.; Franco, A.; Battisti, A. Prevalence of Staphylococcus aureus and of methicillin-resistant S. aureus clonal complexes in bulk tank milk from dairy cattle herds in Lombardy Region (Northern Italy). Epidemiol. Infect. 2016, 144, 3046–3051. [Google Scholar] [CrossRef]
- Tenhagen, B.A.; Köster, G.; Wallmann, J.; Heuwieser, W. Prevalence of Mastitis Pathogens and Their Resistance Against Antimicrobial gents in Dairy Cows in Brandenburg, Germany. J. Dairy Sci. 2006, 89, 2542–2551. [Google Scholar] [CrossRef]
- Cervinkova, D.; Vlkova, H.; Borodacova, I.; Makovcova, J.; Babak, V.; Lorencova, A.; Vrtkova, I.; Marosevic, D.; Jaglic, Z. Prevalence of mastitis pathogens in milk from clinically healthy cows. Vet. Med. 2013, 58, 567–575. [Google Scholar] [CrossRef]
- Patel, K.; Godden, S.M.; Royster, E.E. Prevalence, antibiotic resistance, virulence and genetic diversity of Staphylococcus aureus isolated from bulk tank milk samples of U.S. dairy herds. BMC Genom. 2021, 22, 367. [Google Scholar] [CrossRef] [PubMed]
- Rüegsegger, F.; Ruf, J.; Tschuor, A.; Sigrist, Y.; Rosskopf, M.; Hässig, M. Antimicrobial susceptibility of mastitis pathogens of dairy cows in Switzerland. Schweiz. Arch. Tierheilkd. 2014, 156, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Kotzamanidis, C.; Vafeas, G.; Giantzi, V.; Anastasiadou, S.; Mygdalias, S.; Malousi, A.; Loukia, E.; Daniel, S.; Zdragas, A. Staphylococcus aureus isolated from ruminants with mastitis in Northern Greece dairy herds: Genetic relatedness and phenotypic and genotypic characterization. Toxins 2021, 13, 176. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Holmes, M.A.; Zadoks, R.N. Methicillin resistant S. aureus in human and bovine mastitis. J. Mammary Gland. Biol. Neoplasia 2011, 16, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Vanderhaeghen, W.; Cerpentier, T.; Adriaensen, C.; Vicca, J.; Hermans, K.; Butaye, P. Methicillin-resistant Staphylococcus aureus (MRSA) ST398 associated with clinical and subclinical mastitis in Belgian cows. Veter Microbiol. 2010, 144, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Obaidat, M.M.; Salman, A.E.B.; Roess, A.A. High prevalence and antimicrobial resistance of mecA Staphylococcus aureus in dairy cattle, sheep, and goat bulk tank milk in Jordan. Trop. Anim. Health Prod. 2017, 50, 405–412. [Google Scholar] [CrossRef]
- Papadopoulos, P.; Angelidis, A.S.; Papadopoulos, T.; Kotzamanidis, C.; Zdragas, A.; Papa, A.; Filioussis, G.; Sergelidis, D. Staphylococcus aureus and methicillin-resistant S. aureus (MRSA) in bulk tank milk, livestock and dairy-farm personnel in north-central and north-eastern Greece: Prevalence, characterization and genetic relatedness. Food Microbiol. 2019, 84, 103249. [Google Scholar] [CrossRef]
- Keyvan, E.; Yurdakul, O.; Demirtas, A.; Yalcin, H.; Bilgen, N. Identification of methicillin-resistant Staphylococcus aureus in bulk tank milk. Food Sci. Technol. 2020, 40, 150–156. [Google Scholar] [CrossRef]
- Aqib, A.I.; Ijaz, M.; Anjum, A.A.; Malik, M.A.R.; Mehmood, K.; Farooqi, S.H.; Hussain, K. Antibiotic susceptibilities and prevalence of Methicillin resistant Staphylococcus aureus (MRSA) isolated from bovine milk in Pakistan. Acta Trop. 2017, 176, 168–172. [Google Scholar] [CrossRef]
- Positive MIC 29 MicroScan Panel. Available online: https://punchout.medline.com/product/Positive-MIC-29-MicroScan-Panel/Discs/Z05-PF181930 (accessed on 21 December 2023).
- Kaczorek-Łukowska, E.; Małaczewska, J.; Sowińska, P.; Szymańska, M.; Wójcik, E.A.; Siwicki, A.K. Staphylococcus aureus from subclinical cases of mastitis in dairy cattle in Poland, what are they hiding? Antibiotic resistance and virulence profile. Pathogens 2022, 11, 1404. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Okpo, N.O.; Abdullahi, I.O.; Whong, C.M.Z.; Ameh, J.B. Occurrence and antibiogram of staphylococcus aureus in dairy products consumed in parts of Kaduna state, Nigeria. Bayero J. Pure Appl. Sci. 2017, 9, 2. [Google Scholar] [CrossRef]
- Kiš, M.; Kolačko, I.; Zdolec, N. Unprocessed milk as a source of multidrug-resistant Staphylococcus aureus strains. Acta Vet. Brno 2021, 90, 357–363. [Google Scholar] [CrossRef]
- Igbinosa, E.O.; Beshiru, A.; Igbinosa, I.H.; Ogofure, A.G.; Ekundayo, T.C.; Okoh, A.I. Prevalence, multiple antibiotic resistanceand virulence profile of methicillin-resistant Staphylococcus aureus (MRSA) in retail poultry meat from Edo, Nigeria. Front. Cell. Infect. Microbiol. 2023, 13, 1122059. [Google Scholar] [CrossRef] [PubMed]
- Gizaw, F.; Kekeba, T.; Teshome, F.; Kebede, M.; Abreham, T.; Berhe, H.H.; Ayana, D.; Edao, B.M.; Waktole, H.; Tufa, T.B.; et al. Multidrug-Resistant Staphylococcus aureus Strains Thrive in Dairy and Beef Production, Processing, and Supply Lines in Five Geographical Areas in Ethiopia. Vet. Sci. 2023, 10, 663. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.T.F.; Gonçalves, J.L.; Dantas, S.T.A.; Rall, V.L.M.; de Oliveira, P.R.F.; dos Santos, M.V.; Peixoto, R.d.M.; Mota, R.A. Genetic and phenotypic characterization of subclinical mastitis-causing multidrug-resistant Staphylococcus aureus. Antibiotics 2023, 12, 1353. [Google Scholar] [CrossRef] [PubMed]
- Oladipo, A.O.; Oladipo, O.G.; Bezuidenhout, C.C. Multi-drug resistance traits of methicillin-resistant Staphylococcus aureus and other Staphylococcal species from clinical and environmental sources. J. Water Health 2019, 17, 930–943. [Google Scholar] [CrossRef]
- Afunwa, R.A.; Ezeanyinka, J.; Afunwa, E.C.; Udeh, A.S.; Oli, A.N.; Unachukwu, M. Multiple antibiotic resistant index of gram-negative bacteria from bird droppings in two commercial poultries in Enugu, Nigeria. Open J. Med. Microbiol. 2020, 10, 171–181. [Google Scholar] [CrossRef]
- Mesquita, A.A.; Rocha, C.M.B.M.; Bruhn, F.R.P.; Custódio, D.A.C.; Braz, M.S.; Pinto, S.M.; Silva, D.B.; Costa, G.M. Staphylococcus aureus and Streptococcus agalactiae: Prevalence, resistance to antimicrobials, and their relationship with the milk quality dairy cattle herds in Minas Geraisstate, Brazil. Pesqui. Vet. Bras. 2019, 39, 308–316. [Google Scholar] [CrossRef]
- Badawy, B.; Elafify, M.; Farag, A.M.M.; Moustafa, S.M.; Sayed-Ahmed, M.Z.; Moawad, A.A.; Algammal, A.M.; Ramadan, H.; Eltholth, M. Ecological distribution of virulent multidrug-resistant Staphylococcus aureus in livestock, environment, and dairy products. Antibiotics 2022, 11, 1651. [Google Scholar] [CrossRef]


| Gene | Primer | Primer Sequence | Annealing Temperature (°C) | Amplicon Size (bp) | Authors |
|---|---|---|---|---|---|
| (5′-3′) | |||||
| blaZ | blaZFw | ACT TCA ACA CCT GCT GCT TTC | 60 °C | 490 | Abdolmaleki Z et al., 2019 [50] |
| blaZ R | TGA CCA CTT TTA TCA GCA ACC | ||||
| cfr | cfrFw | ATG AAT TTT AAT AAT AAA ACA AAG | 58 °C | 746 | Kehrenberg et al., 2006 [51] |
| cfr R | TAC ACC CAA AAT TAC ATC CG | ||||
| erm(B) | erm(B)Fw | CAT TTA ACG ACG AAA CTG GC | 60 °C | 745 | Malhotra-Kumar et al., 2005 [52] |
| erm(B) R | GGA ACA TCT GTG GTA TGG CG | ||||
| erm(C) | erm(C)Fw | ATC TTT GAA ATC GGC TCA GG | 58 °C | 299 | Klare I. et al., 2007 [53] |
| erm(C) R | CAA ACC CGT ATT CCA CGA TT | ||||
| mecA | mecAFw | CTG ATG GTA TGC AAC AAG TCG | 55 °C | 533 | Lee, 2003 [54] |
| mecA R | TGA GTT CTG CAG TAC CGG ATT | ||||
| tet(K) | tet(K)Fw | GTA GCG ACA ATA GGT AAT AGT | 60 °C | 360 | Abdolmaleki et al., 2019 [50] |
| tet(K) R | GTA GTG ACA ATA AAC CTC CTA |
| Class | Antibiotic | MIC (µg/mL) | Susceptible (S) | Resistant (R) | Total Isolates | |||
|---|---|---|---|---|---|---|---|---|
| Cows | Humans | Cows | Humans | S | R | |||
| Aminoglycosides |
| 4–8 | 126 (84%) | 16 (80%) | 24 (16%) | 4 (20%) | 142 | 28 |
| 8–16 | 128 (85.3%) | 20 (100%) | 22 (14.7%) | 0 (0%) | 148 | 22 | |
| Amphenicols |
| 8–16 | 106 (70.7%) | 20 (100%) | 44 (29.3%) | 0 (0%) | 126 | 44 |
| Beta-lactam-lactamase-inhibitor (1st gen. Cephalosporins, 2nd gen. Cephalosporins and Penicillins) |
| 4/2 | 72 (48%) | 12 (60%) | 78 (52%) | 8 (40%) | 84 | 86 |
| 8–16 | 70 (46.7%) | 12 (60%) | 80 (53.3%) | 8 (40%) | 82 | 88 | |
| 4 | 120 (80%) | 20 (100%) | 30 (20%) | 0 (0%) | 140 | 30 | |
| 0.25–8 | 0 (0%) | 0 (0%) | 150 (100%) | 20 (100%) | 0 | 170 | |
| 4 | 119 (79%) | 20 (100%) | 31 (21%) | 0 (0%) | 139 | 31 | |
| 0.03–8 | 0 (0%) | 0 (0%) | 150 (100%) | 20 (100%) | 0 | 170 | |
| Fluoroquinolones |
| 1–2 | 130 (86.7%) | 18 (90%) | 20 (13.3%) | 2 (10%) | 148 | 22 |
| 1–4 | 128 (85.3%) | 18 (90%) | 22 (14.7%) | 2 (10%) | 146 | 24 | |
| 0.5–1 | 120 (80%) | 18 (90%) | 30 (20%) | 2 (10%) | 138 | 32 | |
| Glycopeptides |
| 0.5–16 | 96 (64%) | 16 (80%) | 54 (36%) | 4 (20%) | 112 | 58 |
| 1–16 | 104 (69.3%) | 16 (80%) | 46 (30.7%) | 4 (20%) | 120 | 50 | |
| Lincosamides |
| 0.25–2 | 38 (25.3%) | 12 (60%) | 112 (74.7%) | 8 (40%) | 50 | 120 |
| Lipopeptides |
| 1.4 | 96 (64%) | 16 (80%) | 54 (36%) | 4 (20%) | 112 | 58 |
| Macrolides |
| 2–4 | 84 (56%) | 10 (50%) | 66 (44%) | 10 (50%) | 94 | 76 |
| 0.5–4 | 80 (53.3%) | 12 (60%) | 70 (46.7%) | 8 (40%) | 92 | 78 | |
| Oxazolidinones |
| 4–8 | 147 (98%) | 20 (100%) | 3 (2%) | 0 (0%) | 167 | 3 |
| Phosphonics |
| 32 | 130 (86.7%) | 20 (100%) | 20 (13.3%) | 0 (0%) | 150 | 20 |
| Rifamycins |
| 1–2 | 108 (72%) | 16 (80%) | 42 (28%) | 4 (20%) | 124 | 46 |
| Steroid antibacterials |
| 2.16 | 120 (80%) | 16 (80%) | 30 (20%) | 4 (20%) | 136 | 34 |
| Sulfonamide-trimethoprim—combinations |
| 2/38 | 120 (80%) | 18 (90%) | 30 (20%) | 2 (10%) | 138 | 32 |
| Streptogramins |
| 1–2 | 94 (62.7%) | 16 (80%) | 56 (37.3%) | 4 (20%) | 110 | 60 |
| Tetracyclines |
| 2–8 | 106 (70.7%) | 16 (80%) | 44 (29.3%) | 4 (20%) | 122 | 48 |
| Genes | Antibiotics | R | S | Penetrance (%) | DOR | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | RG+ | RG− | Total | SG+ | SG− | ||||
| blaZ | Amoxycillin/clavulanicacid | 86 | 78(91%) | 8(9%) | 84 | 82(98%) | 2(2%) | 49% | 0.24 |
| Penicillin | 170 | 160(94%) | 10(6%) | 0 | 0 | 0 | 100% | - | |
| Ampicillin | 170 | 160(94%) | 10(6%) | 0 | 0 | 0 | 100% | - | |
| Subtotal | 426 | 398 | 28 | 84 | 82 | 2 | 83% | 0.35 | |
| mecA | Amoxycillin/clavulanic acid | 86 | 68(79%) | 18(21%) | 84 | 64(76%) | 20(24%) | 51% | 1.18 |
| Ampicillin | 170 | 132(78%) | 38(22%) | 0 | 0 | 0 | 100% | - | |
| Cefalotin | 88 | 68(77%) | 20(23%) | 82 | 64(78%) | 18(22%) | 52% | 0.96 | |
| Cefoxitin screening | 30 | 26(87%) | 4(13%) | 140 | 106(76%) | 34(24%) | 20% | 2.08 | |
| Oxacillin | 31 | 27(87%) | 4 (13%) | 139 | 108(78%) | 31(22%) | 20% | 1.94 | |
| Penicillin | 170 | 132(78%) | 38(22%) | 0 | 0 | 0 | 100% | - | |
| Subtotal | 575 | 453 | 122 | 445 | 342 | 103 | 57% | 1.12 | |
| cfr | Chloramphenicol | 44 | 28(64%) | 16(36%) | 126 | 48(38%) | 78(62%) | 37% | 2.84 |
| Linezolid | 3 | 3(100%) | 0(0%) | 167 | 4(2%) | 163(98%) | 43% | - | |
| Synercid | 60 | 38(63%) | 22(37%) | 110 | 38(35%) | 72(65%) | 50% | 3.27 | |
| Clindamycin | 120 | 62(52%) | 58(48%) | 50 | 14(28%) | 36(72%) | 82% | 2.75 | |
| Subtotal | 227 | 131 | 96 | 453 | 104 | 349 | 56% | 4.58 | |
| erm(B) | Clarithromycin | 76 | 58(76%) | 18(24%) | 94 | 62(66%) | 32(34%) | 48% | 1.66 |
| Clindamycin | 120 | 84(70%) | 36(30%) | 50 | 36(72%) | 14(28%) | 70% | 0.91 | |
| Erythromycin | 80 | 58(70%) | 22(30%) | 90 | 62(69%) | 28(31%) | 48% | 1.19 | |
| Synercid | 60 | 42(70%) | 18(30%) | 110 | 78(71%) | 32(29%) | 35% | 0.96 | |
| Subtotal | 336 | 242 | 94 | 344 | 238 | 106 | 50% | 1.15 | |
| erm(C) | Clarithromycin | 76 | 58(76%) | 18(24%) | 94 | 58(62%) | 36(38%) | 50% | 2 |
| Clindamycin | 120 | 80(67%) | 40(33%) | 50 | 36(72%) | 14(28%) | 69% | 0.78 | |
| Erythromycin | 78 | 60(77%) | 18(23%) | 92 | 56(61%) | 36(39%) | 52% | 2.14 | |
| Synercid | 60 | 48(80%) | 12(20%) | 110 | 68(62%) | 42(38%) | 41% | 2.47 | |
| Subtotal | 334 | 246 | 88 | 346 | 218 | 128 | 53% | 1.64 | |
| tet(K) | Tetracycline | 48 | 40(83%) | 8(17%) | 122 | 86(70%) | 36(30%) | 32% | 2.09 |
| Subtotal | 48 | 40 | 8 | 122 | 86 | 36 | 32% | 2.09 | |
| Total study | 1946 | 1510 | 436 | 1794 | 1070 | 724 | 58.53% | 2.34 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hutu, I.; Lungu, B.C.; Spataru, I.I.; Torda, I.; Iancu, T.; Barrow, P.A.; Mircu, C. Microbiological and Molecular Investigation of Antimicrobial Resistance in Staphylococcus aureus Isolates from Western Romanian Dairy Farms: An Epidemiological Approach. Animals 2024, 14, 2266. https://doi.org/10.3390/ani14152266
Hutu I, Lungu BC, Spataru II, Torda I, Iancu T, Barrow PA, Mircu C. Microbiological and Molecular Investigation of Antimicrobial Resistance in Staphylococcus aureus Isolates from Western Romanian Dairy Farms: An Epidemiological Approach. Animals. 2024; 14(15):2266. https://doi.org/10.3390/ani14152266
Chicago/Turabian StyleHutu, Ioan, Bianca Cornelia Lungu, Ioana Irina Spataru, Iuliu Torda, Tiberiu Iancu, Paul Andrew Barrow, and Calin Mircu. 2024. "Microbiological and Molecular Investigation of Antimicrobial Resistance in Staphylococcus aureus Isolates from Western Romanian Dairy Farms: An Epidemiological Approach" Animals 14, no. 15: 2266. https://doi.org/10.3390/ani14152266





