Protection of Chickens against H9N2 Avian Influenza Isolates with a Live Vector Vaccine Expressing Influenza Hemagglutinin Gene Derived from Y280 Avian Influenza Virus
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses and Cell Culture
2.2. Construction of Plasmids Expressing CAS9/gRNA and Donor Plasmids
2.3. Generation of rHVT/Y280
2.4. Growth Kinetics
2.5. Genetic Stability
2.6. Preparation of Formalin-Inactivated Viruses
2.7. Chickens and Vaccination Programs
2.8. Serology
2.9. Clinical Signs, Mortality, and Gross Lesions
2.10. Assessment of Virus Shedding
2.11. Virus Replication in Tissues
2.12. Statistical Analysis
3. Results
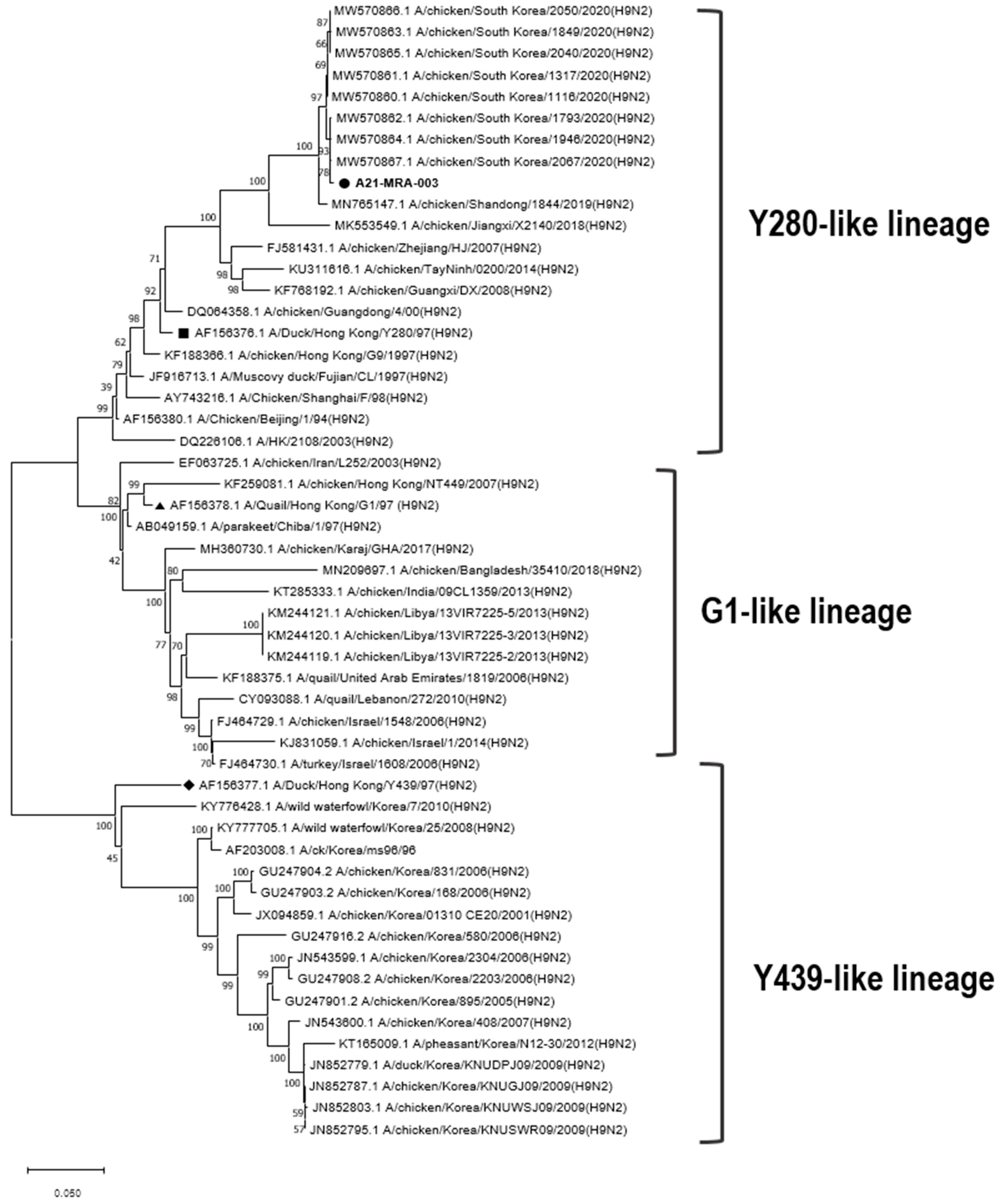
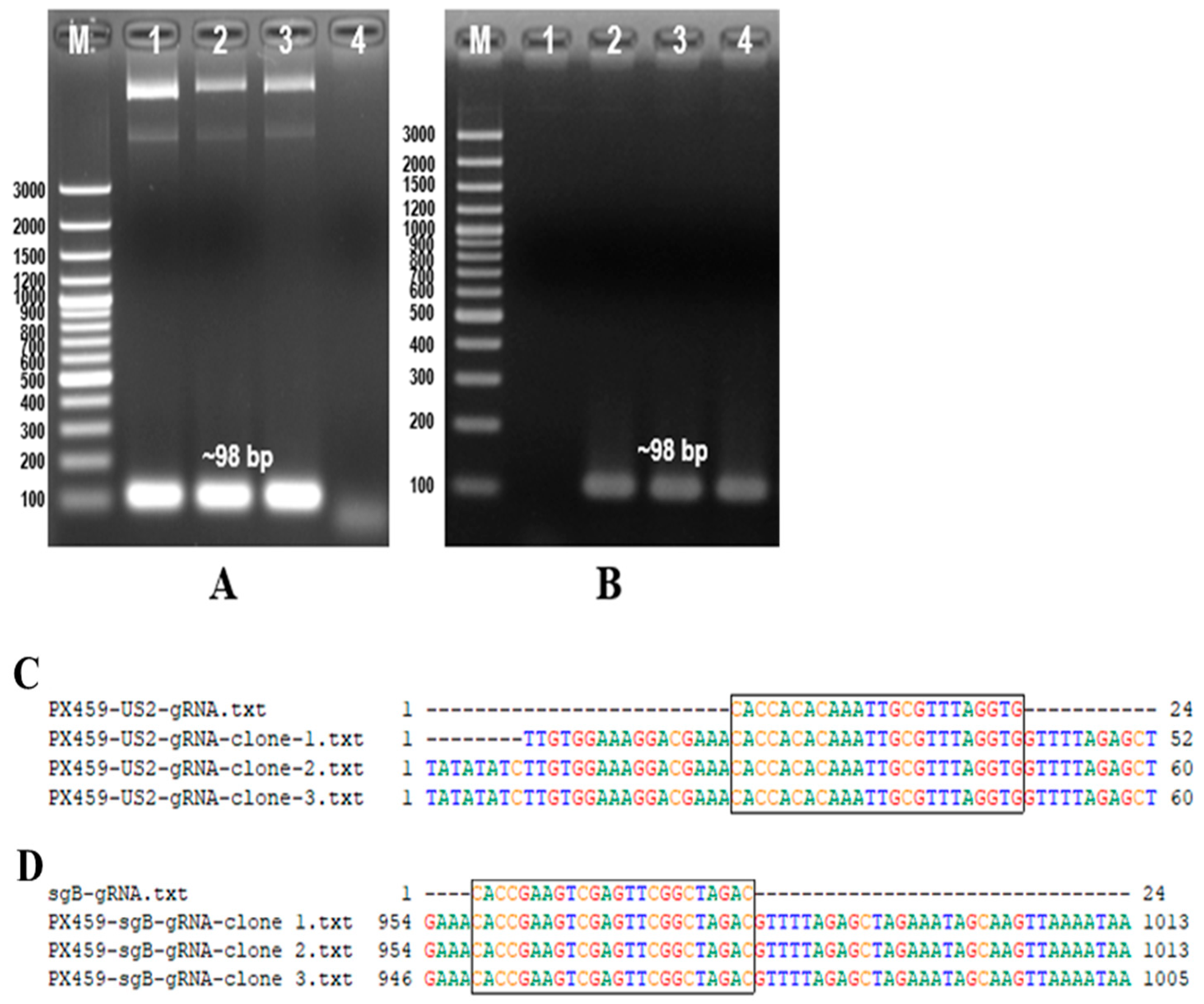
3.1. Identification of PX459-US2-gRNA and PX459-sgB-gRNA
3.2. Generation of rHVT/Y280
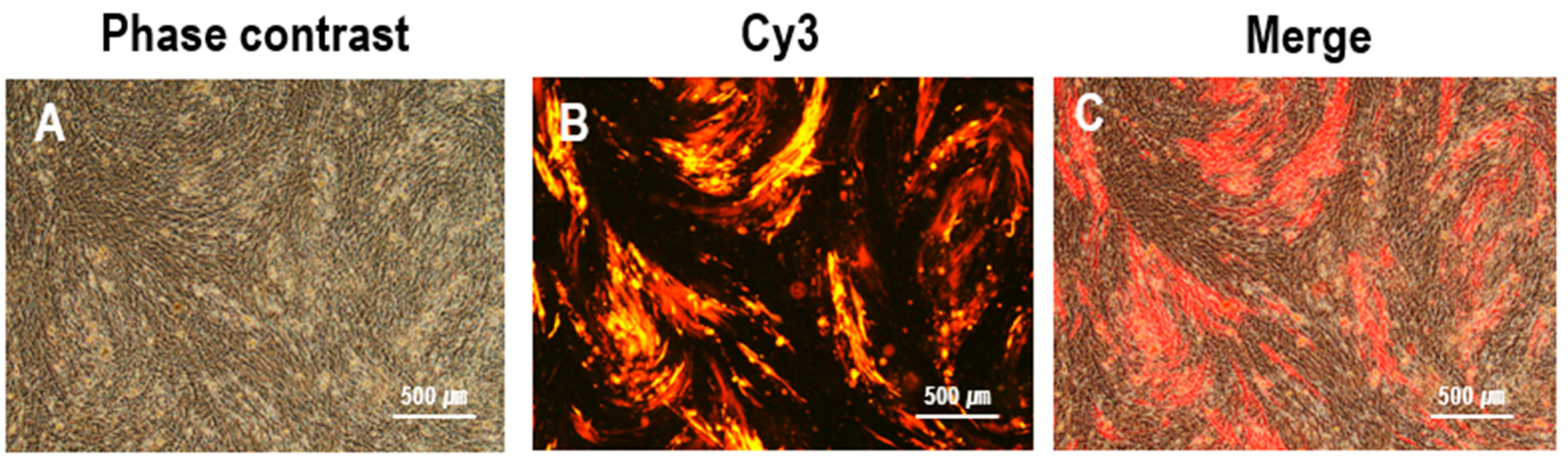
3.3. Purification of rHVT/Y280
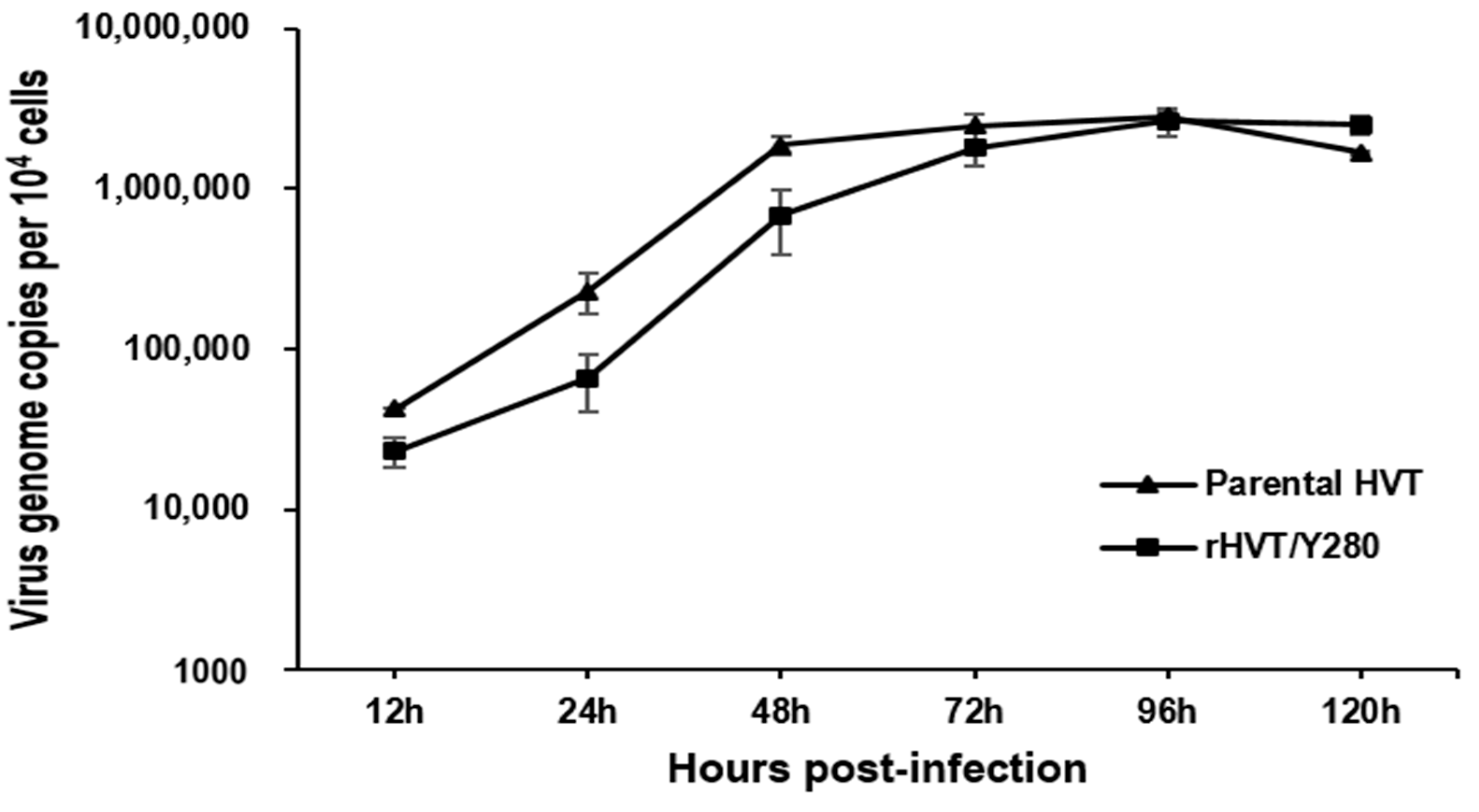
3.4. Growth Kinetics
3.5. Genetic Stability
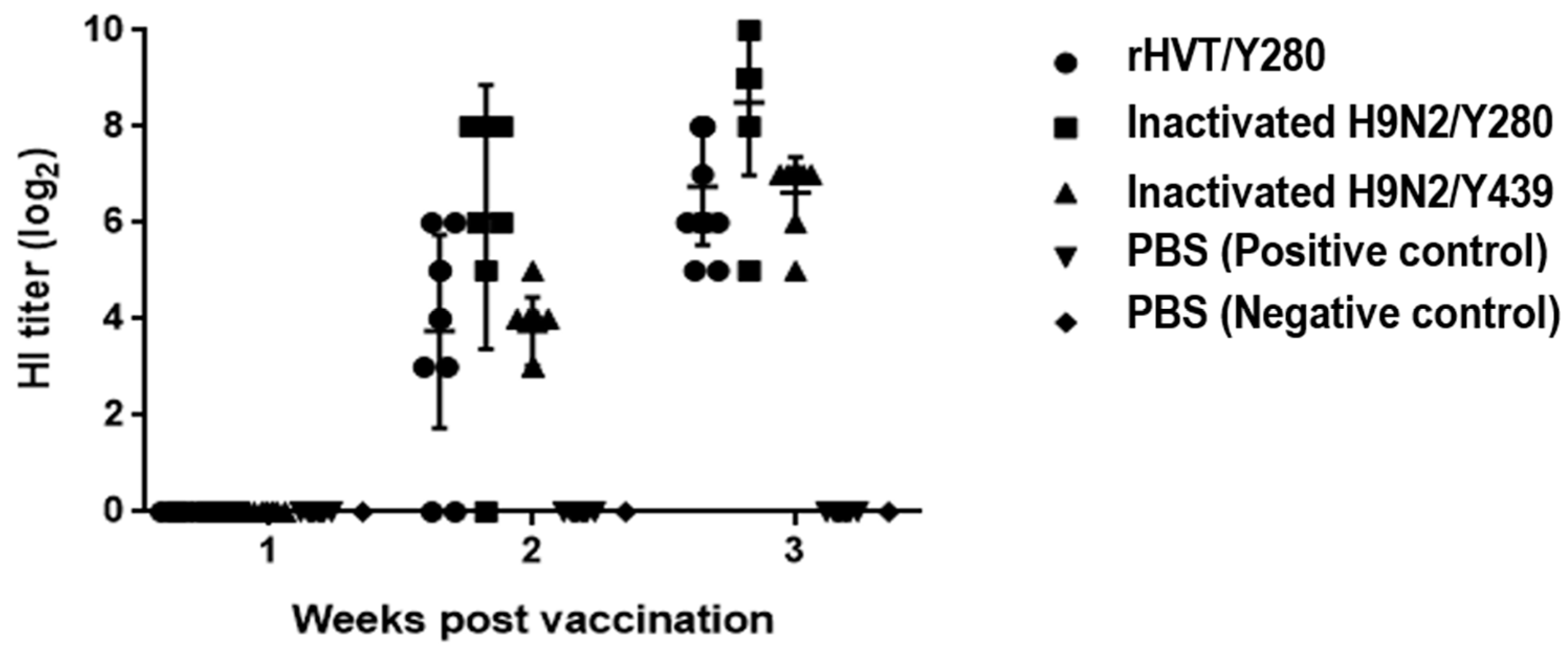
3.6. Humoral Immune Response
3.7. Protective Efficacy in Chickens
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Swayne, D.E. Avian Influenza; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Peiris, J.M.; De Jong, M.D.; Guan, Y. Avian influenza virus (H5N1): A threat to human health. Clin. Microbiol. Rev. 2007, 20, 243–267. [Google Scholar] [CrossRef]
- Homme, P.; Easterday, B. Avian influenza virus infections. I. Characteristics of influenza A/Turkey/Wisconsin/1966 virus. Avian Dis. 1970, 14, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Butt, K.; Smith, G.J.; Chen, H.; Zhang, L.; Leung, Y.C.; Xu, K.; Lim, W.; Webster, R.G.; Yuen, K.; Peiris, J.M. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J. Clin. Microbiol. 2005, 43, 5760–5767. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-J.; Shin, J.-Y.; Song, M.-S.; Lee, Y.-M.; Choi, J.-G.; Lee, E.-K.; Jeong, O.-M.; Sung, H.-W.; Jae-Hong, K.; Kwon, Y.-K. Continuing evolution of H9 influenza viruses in Korean poultry. Virology 2007, 359, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Liu, L.; Pu, J.; Zhao, J.; Sun, Y.; Shen, G.; Wei, H.; Zhu, J.; Zheng, R.; Xiong, D. Risk perceptions for avian influenza virus infection among poultry workers, China. Emerg. Infect. Dis. 2013, 19, 313. [Google Scholar] [CrossRef]
- Guo, Y.; Krauss, S.; Senne, D.; Mo, I.; Lo, K.; Xiong, X.; Norwood, M.; Shortridge, K.; Webster, R.; Guan, Y. Characterization of the pathogenicity of members of the newly established H9N2 influenza virus lineages in Asia. Virology 2000, 267, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Heo, G.-B.; Kye, S.-J.; Sagong, M.; Lee, E.-K.; Lee, K.-N.; Lee, Y.-N.; Choi, K.-S.; Lee, M.-H.; Lee, Y.-J. Genetic characterization of H9N2 avian influenza virus previously unrecognized in Korea. J. Vet. Sci. 2021, 22, e21. [Google Scholar] [CrossRef]
- Kye, S.-J.; Park, M.-J.; Kim, N.-Y.; Lee, Y.-N.; Heo, G.-B.; Baek, Y.-K.; Shin, J.-I.; Lee, M.-H.; Lee, Y.-J. Pathogenicity of H9N2 low pathogenic avian influenza viruses of different lineages isolated from live bird markets tested in three animal models: SPF chickens, Korean native chickens, and ducks. Poult. Sci. 2021, 100, 101318. [Google Scholar] [CrossRef]
- Song, W.; Qin, K. Human-infecting influenza A (H9N2) virus: A forgotten potential pandemic strain? Zoonoses Public Health 2020, 67, 203–212. [Google Scholar] [CrossRef]
- Gu, M.; Xu, L.; Wang, X.; Liu, X. Current situation of H9N2 subtype avian influenza in China. Vet. Res. 2017, 48, 49. [Google Scholar] [CrossRef]
- Chen, H.; Yuan, H.; Gao, R.; Zhang, J.; Wang, D.; Xiong, Y.; Fan, G.; Yang, F.; Li, X.; Zhou, J. Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: A descriptive study. Lancet 2014, 383, 714–721. [Google Scholar] [CrossRef]
- Liu, D.; Shi, W.; Shi, Y.; Wang, D.; Xiao, H.; Li, W.; Bi, Y.; Wu, Y.; Li, X.; Yan, J. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: Phylogenetic, structural, and coalescent analyses. Lancet 2013, 381, 1926–1932. [Google Scholar] [CrossRef]
- Youk, S.-s.; Lee, D.-H.; Jeong, J.-H.; Pantin-Jackwood, M.J.; Song, C.-S.; Swayne, D.E. Live bird markets as evolutionary epicentres of H9N2 low pathogenicity avian influenza viruses in Korea. Emerg. Microbes Infect. 2020, 9, 616–627. [Google Scholar] [CrossRef]
- Cho, H.-K.; Kang, Y.-M.; Kim, H.-M.; Lee, C.-H.; Kim, D.-Y.; Choi, S.-H.; Lee, M.-H.; Kang, H.-M. Sales and immunogenicity of commercial vaccines to H9N2 low pathogenic avian influenza virus in Korea from 2007 to 2017. Vaccine 2020, 38, 3191–3195. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.J.; Song, M.S.; Cruz, D.J.M.; Park, K.J.; Pascua, P.N.Q.; Lee, J.H.; Baek, Y.H.; Choi, D.H.; Choi, Y.K.; Kim, C.J. Active reassortment of H9 influenza viruses between wild birds and live-poultry markets in Korea. Arch. Virol. 2010, 155, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-R.; Park, C.-K.; Oem, J.-K.; Bae, Y.-C.; Choi, J.-G.; Lee, O.-S.; Lee, Y.-J. Characterization of H5N2 influenza viruses isolated in South Korea and their influence on the emergence of a novel H9N2 influenza virus. J. Gen. Virol. 2010, 91, 1978–1983. [Google Scholar] [CrossRef] [PubMed]
- Youk, S.; Cho, A.Y.; Lee, D.H.; Jeong, S.; Kim, Y.j.; Lee, S.; Kim, T.H.; Pantin-Jackwood, M.J.; Song, C.S. Detection of newly introduced Y280-lineage H9N2 avian influenza viruses in live bird markets in Korea. Transbound. Emerg. Dis. 2022, 69, 881–885. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-Y.; Kang, Y.-M.; Cho, H.-K.; Park, S.-j.; Lee, M.-H.; Lee, Y.-J.; Kang, H.-M. Development of a recombinant H9N2 influenza vaccine candidate against the Y280 lineage field virus and its protective efficacy. Vaccine 2021, 39, 6201–6205. [Google Scholar] [CrossRef] [PubMed]
- Eidson, C.; Villegas, P.; Page, R.; Kleven, S. A comparison of the efficacy against Marek’s disease of cell-free and cell-associated turkey herpesvirus vaccine. Avian Dis. 1975, 19, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Teng, M.; Yao, Y.; Nair, V.; Luo, J. Latest advances of virology research using CRISPR/Cas9-based gene-editing technology and its application to vaccine development. Viruses 2021, 13, 779. [Google Scholar] [CrossRef]
- Vilela, J.; Rohaim, M.A.; Munir, M. Application of CRISPR/Cas9 in understanding avian viruses and developing poultry vaccines. Front. Cell. Infect. Microbiol. 2020, 10, 581504. [Google Scholar] [CrossRef]
- Ingrao, F.; Rauw, F.; van den Berg, T.; Lambrecht, B. Characterization of two recombinant HVT-IBD vaccines by VP2 insert detection and cell-mediated immunity after vaccination of specific pathogen-free chickens. Avian Pathol. 2017, 46, 289–299. [Google Scholar] [CrossRef]
- Kapczynski, D.R.; Esaki, M.; Dorsey, K.M.; Jiang, H.; Jackwood, M.; Moraes, M.; Gardin, Y. Vaccine protection of chickens against antigenically diverse H5 highly pathogenic avian influenza isolates with a live HVT vector vaccine expressing the influenza hemagglutinin gene derived from a clade 2.2 avian influenza virus. Vaccine 2015, 33, 1197–1205. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wang, T.; Wang, M.; Tong, Q.; Sun, Y.; Pu, J.; Sun, H.; Liu, J. Recombinant turkey herpesvirus expressing H9 hemagglutinin providing protection against H9N2 avian influenza. Virology 2019, 529, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Kamel, M.; El-Sayed, A. Utilization of herpesviridae as recombinant viral vectors in vaccine development against animal pathogens. Virus Res. 2019, 270, 197648. [Google Scholar] [CrossRef] [PubMed]
- Ran, F.A.; Hsu, P.D.; Wright, J.; Agarwala, V.; Scott, D.A.; Zhang, F. Genome engineering using the CRISPR-Cas9 system. Nat. Protoc. 2013, 8, 2281–2308. [Google Scholar] [CrossRef]
- Cong, L.; Ran, F.A.; Cox, D.; Lin, S.; Barretto, R.; Habib, N.; Hsu, P.D.; Wu, X.; Jiang, W.; Marraffini, L.A. Multiplex genome engineering using CRISPR/Cas systems. Science 2013, 339, 819–823. [Google Scholar] [CrossRef]
- Sternberg, S.H.; LaFrance, B.; Kaplan, M.; Doudna, J.A. Conformational control of DNA target cleavage by CRISPR–Cas9. Nature 2015, 527, 110–113. [Google Scholar] [CrossRef]
- Doudna, J.A.; Charpentier, E. The new frontier of genome engineering with CRISPR-Cas9. Science 2014, 346, 1258096. [Google Scholar] [CrossRef] [PubMed]
- Jinek, M.; Chylinski, K.; Fonfara, I.; Hauer, M.; Doudna, J.A.; Charpentier, E. A programmable dual-RNA–guided DNA endonuclease in adaptive bacterial immunity. Science 2012, 337, 816–821. [Google Scholar] [CrossRef]
- Bi, Y.; Sun, L.; Gao, D.; Ding, C.; Li, Z.; Li, Y.; Cun, W.; Li, Q. High-efficiency targeted editing of large viral genomes by RNA-guided nucleases. PLoS Pathog. 2014, 10, e1004090. [Google Scholar] [CrossRef] [PubMed]
- Xu, A.; Qin, C.; Lang, Y.; Wang, M.; Lin, M.; Li, C.; Zhang, R.; Tang, J. A simple and rapid approach to manipulate pseudorabies virus genome by CRISPR/Cas9 system. Biotechnol. Lett. 2015, 37, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Yuan, M.; Zhang, W.; Wang, J.; Al Yaghchi, C.; Ahmed, J.; Chard, L.; Lemoine, N.R.; Wang, Y. Efficiently editing the vaccinia virus genome by using the CRISPR-Cas9 system. J. Virol. 2015, 89, 5176–5179. [Google Scholar] [CrossRef]
- Yuen, K.-S.; Chan, C.-P.; Wong, N.-H.M.; Ho, C.-H.; Ho, T.-H.; Lei, T.; Deng, W.; Tsao, S.W.; Chen, H.; Kok, K.-H. CRISPR/Cas9-mediated genome editing of Epstein–Barr virus in human cells. J. Gen. Virol. 2015, 96, 626–636. [Google Scholar] [CrossRef]
- Bierle, C.J.; Anderholm, K.M.; Wang, J.B.; McVoy, M.A.; Schleiss, M.R. Targeted mutagenesis of guinea pig cytomegalovirus using CRISPR/Cas9-mediated gene editing. J. Virol. 2016, 90, 6989–6998. [Google Scholar] [CrossRef]
- Chang, P.; Yao, Y.; Tang, N.; Sadeyen, J.-R.; Sealy, J.; Clements, A.; Bhat, S.; Munir, M.; Bryant, J.E.; Iqbal, M. The application of NHEJ-CRISPR/Cas9 and Cre-Lox system in the generation of bivalent duck enteritis virus vaccine against avian influenza virus. Viruses 2018, 10, 81. [Google Scholar] [CrossRef]
- Atasoy, M.O.; Rohaim, M.A.; Munir, M. Simultaneous deletion of virulence factors and insertion of antigens into the infectious laryngotracheitis virus using NHEJ-CRISPR/Cas9 and cre–lox system for construction of a stable vaccine vector. Vaccines 2019, 7, 207. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Xu, J.; Cheng, M.; Liao, X.; Peng, S. Review of CRISPR/Cas9 sgRNA design tools. Interdiscip. Sci. Comput. Life Sci. 2018, 10, 455–465. [Google Scholar] [CrossRef]
- Tang, N.; Zhang, Y.; Pedrera, M.; Chang, P.; Baigent, S.; Moffat, K.; Shen, Z.; Nair, V.; Yao, Y. A simple and rapid approach to develop recombinant avian herpesvirus vectored vaccines using CRISPR/Cas9 system. Vaccine 2018, 36, 716–722. [Google Scholar] [CrossRef]
- Baigent, S.J.; Petherbridge, L.J.; Howes, K.; Smith, L.P.; Currie, R.J.; Nair, V.K. Absolute quantitation of Marek’s disease virus genome copy number in chicken feather and lymphocyte samples using real-time PCR. J. Virol. Methods 2005, 123, 53–64. [Google Scholar] [CrossRef]
- Islam, A.; Harrison, B.; Cheetham, B.F.; Mahony, T.J.; Young, P.L.; Walkden-Brown, S.W. Differential amplification and quantitation of Marek’s disease viruses using real-time polymerase chain reaction. J. Virol. Methods 2004, 119, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Jadidi, B.R.; Erfan-Niya, H.; Ameghi, A. Optimizing the process of inactivating influenza virus subtype H9N2 by formalin in the production of killed avian influenza vaccine. Arch. Razi Inst. 2017, 72, 43–49. [Google Scholar]
- Pedersen, J.C. Hemagglutination-inhibition test for avian influenza virus subtype identification and the detection and quantitation of serum antibodies to the avian influenza virus. Avian Influenza Virus 2008, 436, 53–66. [Google Scholar]
- Gao, H.; Cui, H.; Cui, X.; Shi, X.; Zhao, Y.; Zhao, X.; Quan, Y.; Yan, S.; Zeng, W.; Wang, Y. Expression of HA of HPAI H5N1 virus at US2 gene insertion site of turkey herpesvirus induced better protection than that at US10 gene insertion site. PLoS ONE 2011, 6, e22549. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Chen, W.; Ma, C.; Zhang, Z.; Zhao, P.; Du, Y.; Zhang, Y.; Duan, L.; Fang, J.; Li, S. Transcriptional activity comparison of different sites in recombinant Marek’s disease virus for the expression of the H9N2 avian influenza virus hemagglutinin gene. J. Virol. Methods 2014, 207, 138–145. [Google Scholar] [CrossRef]
- Rauw, F.; Gardin, Y.; Palya, V.; Van den Berg, T.; Lambrecht, B. The combination of attenuated Newcastle disease (ND) vaccine with rHVT-ND vaccine at 1 day old is more protective against ND virus challenge than when combined with inactivated ND vaccine. Avian Pathol. 2014, 43, 26–36. [Google Scholar] [CrossRef]
- Tsukamoto, K.; Sato, T.; Saito, S.; Tanimura, N.; Hamazaki, N.; Mase, M.; Yamaguchi, S. Dual-viral vector approach induced strong and long-lasting protective immunity against very virulent infectious bursal disease virus. Virology 2000, 269, 257–267. [Google Scholar] [CrossRef]
- Le Gros, F.; Dancer, A.; Giacomini, C.; Pizzoni, L.; Bublot, M.; Graziani, M.; Prandini, F. Field efficacy trial of a novel HVT-IBD vector vaccine for 1-day-old broilers. Vaccine 2009, 27, 592–596. [Google Scholar] [CrossRef]
- Kilany, W.H.; Hassan, M.K.; Safwat, M.; Mohammed, S.; Selim, A.; VonDobschuetz, S.; Dauphin, G.; Lubroth, J.; Jobre, Y. Comparison of the effectiveness of rHVT-H5, inactivated H5 and rHVT-H5 with inactivated H5 prime/boost vaccination regimes in commercial broiler chickens carrying MDAs against HPAI H5N1 clade 2.2. 1 virus. Avian Pathol. 2015, 44, 333–341. [Google Scholar] [CrossRef]
- Bublot, M.; Pritchard, N.; Le Gros, F.-X.; Goutebroze, S. Use of a vectored vaccine against infectious bursal disease of chickens in the face of high-titred maternally derived antibody. J. Comp. Pathol. 2007, 137, S81–S84. [Google Scholar] [CrossRef]
- Johnson, D.I.; Vagnozzi, A.; Dorea, F.; Riblet, S.M.; Mundt, A.; Zavala, G.; García, M. Protection against infectious laryngotracheitis by in ovo vaccination with commercially available viral vector recombinant vaccines. Avian Dis. 2010, 54, 1251–1259. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.; Luo, H.; Akhter, J.; Islam, M.; Islam, M.; Rahman, M.; Cao, Y.; Xue, C. Protection effect of Vaxxitek HVT+ IBD vaccine against infectious bursal disease in broiler chickens. Progress. Agric. 2013, 24, 69–78. [Google Scholar] [CrossRef]
- Zhang, J.-F.; Park, J.-Y.; Kim, S.-W.; Choi, Y.-R.; Cha, S.-Y.; Jang, H.-K.; Wei, B.; Kang, M. Development of a Highly Efficient CRISPR/Cas9-Mediated Herpesvirus of Turkey-Based Vaccine against Novel Variant Infectious Bursal Disease Virus. Vaccines 2024, 12, 226. [Google Scholar] [CrossRef]
- Li, K.; Liu, Y.; Liu, C.; Gao, L.; Zhang, Y.; Cui, H.; Gao, Y.; Qi, X.; Zhong, L.; Wang, X. Recombinant Marek’s disease virus type 1 provides full protection against very virulent Marek’s and infectious bursal disease viruses in chickens. Sci. Rep. 2016, 6, 39263. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Zhang, Y.; Sadigh, Y.; Moffat, K.; Shen, Z.; Nair, V.; Yao, Y. Generation of a triple insert live avian herpesvirus vectored vaccine using CRISPR/Cas9-based gene editing. Vaccines 2020, 8, 97. [Google Scholar] [CrossRef] [PubMed]
| Group | Vaccination | Serology at 3 wpv (log2 HI titer) a | Virus Shedding (log10EID50/0.1 mL) b | Virus Replication in Tissues (log10EID50/0.1 mL) c | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 dpi | 5 dpi | 5 dpi | |||||||||
| OP | CL | OP | CL | Trachea | Lung | Bursa | Brain | Cecal Tonsil | |||
| A | rHVT/Y280 | 12/12 (6.8) | 3/12 (0.5) | 0/12 (−) | 0/12 (−) | 0/12 (−) | 1/12 (0.1) | 1/12 (0.1) | 0/12 (−) | 0/12 (−) | 0/12 (−) |
| B | Inactivated H9N2/Y439 | 8/8 (8.5) | 1/8 (0.3) | 1/8 (0.2) | 0/8 (−) | 0/8 (−) | 1/8 (0.1) | 1/8 (0.2) | 0/8 (−) | 1/8 (0.2) | 0/8 (−) |
| C | Inactivated H9N2/Y280 | 8/8 (6.9) | 8/8 (4.0) | 6/8 (1.4) | 8/8 (1.8) | 3/8 (0.6) | 7/8 (2.0) | 5/8 (1.4) | 1/8 (0.2) | 5/8 (1.2) | 2/8 (0.5) |
| PC | PBS | 0/10 (0) | 10/10 (4.7) | 8/10 (1.4) | 10/10 (2.7) | 9/10 (1.7) | 10/10 (2.7) | 7/10 (1.8) | 5/10 (1.1) | 6/10 (1.2) | 6/10 (1.1) |
| NC | PBS | 0/6 (0) | 0/6 (−) | 0/6 (−) | 0/6 (−) | 0/6 (−) | 0/6 (−) | 0/6 (−) | 0/6 (−) | 0/6 (−) | 0/6 (−) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.-F.; Kim, S.-W.; Shang, K.; Park, J.-Y.; Choi, Y.-R.; Jang, H.-K.; Wei, B.; Kang, M.; Cha, S.-Y. Protection of Chickens against H9N2 Avian Influenza Isolates with a Live Vector Vaccine Expressing Influenza Hemagglutinin Gene Derived from Y280 Avian Influenza Virus. Animals 2024, 14, 872. https://doi.org/10.3390/ani14060872
Zhang J-F, Kim S-W, Shang K, Park J-Y, Choi Y-R, Jang H-K, Wei B, Kang M, Cha S-Y. Protection of Chickens against H9N2 Avian Influenza Isolates with a Live Vector Vaccine Expressing Influenza Hemagglutinin Gene Derived from Y280 Avian Influenza Virus. Animals. 2024; 14(6):872. https://doi.org/10.3390/ani14060872
Chicago/Turabian StyleZhang, Jun-Feng, Sang-Won Kim, Ke Shang, Jong-Yeol Park, Yu-Ri Choi, Hyung-Kwan Jang, Bai Wei, Min Kang, and Se-Yeoun Cha. 2024. "Protection of Chickens against H9N2 Avian Influenza Isolates with a Live Vector Vaccine Expressing Influenza Hemagglutinin Gene Derived from Y280 Avian Influenza Virus" Animals 14, no. 6: 872. https://doi.org/10.3390/ani14060872





