Epidemiological Profile of Ophir Loyola Cancer Hospital: A Snapshot of the Incidence of Solid Neoplasms in the Eastern Amazon
Abstract
:1. Introduction
2. Method
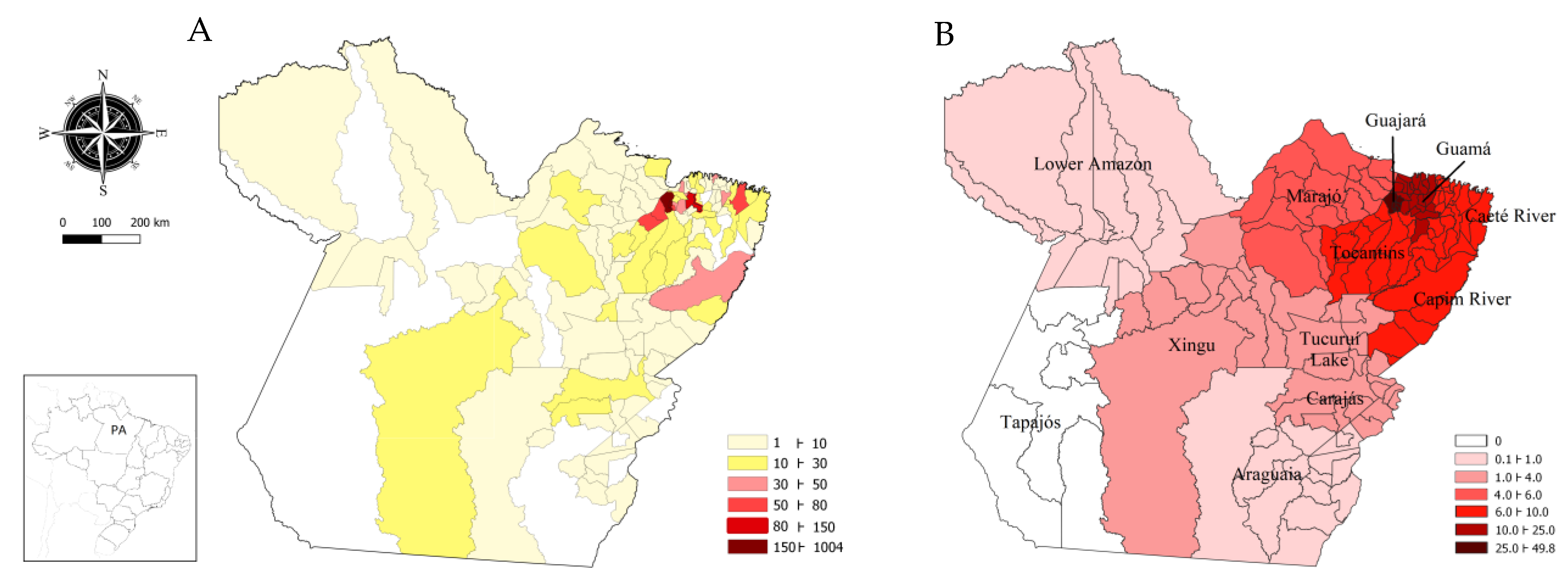
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, R.J.; Madan, R.A.; Kim, J.; Posadas, E.M.; Yu, E.Y. Disparities in Cancer Care and the Asian American Population. Oncologist 2021, 26, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Moura, R.R.; Coelho, A.V.; Balbino, V.Q.; Crovella, S.; Brandão, L.A. Meta-analysis of Brazilian genetic admixture and comparison with other Latin America countries. Am. J. Hum. Biol. 2015, 27, 674–680. [Google Scholar] [CrossRef]
- Allemani, C.; Matsuda, T.; Di Carla, V.; Harewood, R.; Matz, M.; Niksic, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Estève, J.; et al. Global surveillance of trendsin cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [PubMed]
- de Oliveira, N.P.D.; Santos Siqueira, C.A.D.; Lima, K.Y.N.; de Camargo Cancela, M.; Souza, D.L.B. Association of cervical and breast cancer mortality with socioeconomic indicators and availability of health services. Cancer Epidemiol. 2020, 64, 101660. [Google Scholar] [CrossRef]
- Korkes, F.; Rodrigues, A.F.S.; Baccaglini, W.; Cunha, F.T.S.; Slongo, J.; Spiess, P.; Glina, S. Penile cancer trends and economic burden in the Brazilian public health system. Einstein 2020, 18, eAO5577. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.A.; da Silva, B.E.B.; Hora, E.C.; Lima, M.S.; Brito, E.A.C.; Santos, M.O.; da Silva, A.M.; Nunes, M.A.P.; Brito, H.L.F.; Lima, M.M.M. Trends in prostate cancer incidence and mortality to monitor control policies in a northeastern Brazilian state. PLoS ONE 2021, 16, e0249009. [Google Scholar] [CrossRef]
- Iser, D.A.; Cobalchini, G.R.; Oliveira, M.M.; Teixeira, R.; Malta, D.C.; Naghavi, M.; Iser, B.P.M. Prostate cancer mortality in Brazil 1990–2019: Geographical distribution and trends. Rev. Soc. Bras. Med. Trop. 2022, 55, e0277. [Google Scholar] [CrossRef]
- Filho, M.F.B.; Santana, M.E.; Mendes, C.P.; Jesus Costa, D.; Santos, C.A.A.S.D.; Araújo, M.F.M.; Oliveira Serra, M.A.A. Cultural, social, and healthcare access factors associated with delays in gastric cancer presentation, diagnosis, and treatment: A cross-sectional study. J. Cancer Policy 2021, 28, 100277. [Google Scholar] [CrossRef]
- Oliveira, M.M.; Silva, I.P.B.; Teixeira, R.; Malta, D.C.; Iser, B.P.M. Esophageal cancer mortality in brazil: A time-series analysis from the global burden of disease study. Arq. Gastroenterol. 2021, 58, 100–106. [Google Scholar] [CrossRef]
- Zamudio, R.; Pereira, L.; Rocha, C.D.; Berg, D.E.; Muniz-Queiroz, T.; Anna, H.P.S.; Cabrera, L.; Combe, J.M.; Herrera, P.; Jahuira, M.H.; et al. Population, Epidemiological, and Functional Genetics of Gastric Cancer Candidate Genes in Peruvians with Predominant Amerindian Ancestry. Dig. Dis. Sci. 2016, 61, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Gibbon, S. Translating Population Difference: The Use and Re-Use of Genetic Ancestry in Brazilian Cancer Genetics. Med. Anthropol. 2016, 35, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Hoffecker, J.F.; Scott, A.E.; O’Rourke, D.H.; Scott, G.R.; Bigelow, N.H. Beringiaand the global dispersal of modern humans. Evol. Anthropol. 2016, 25, 64–78. [Google Scholar] [CrossRef] [PubMed]
- Carroll, C.B.; Gomide, M. Análise de redesnaregulação do tratamento do câncer do aparelhodigestivo. Cad. SaúdePública 2020, 36, e00041518. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística. Estimativas da Populaçãoresidente para Osmunicípios e para as Unidades da Federaçãobrasileiros com Datadereferênciaem 1º de Julho de 2019; IBGE: Rio de Janeiro, Brazil, 2019. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv101662.pdf (accessed on 15 March 2023).
- Pará (Estado); Governo do Estado do Pará; Secretaria de Estado de SaúdePública; CoordenaçãoEstadual de AtençãoOncológica. Protocolo de Acesso da Rede de Assistência de Média e Altacomplexidadeemoncologia do Estado do Pará; CEAO/DDRA/SESPA: Belém, Pará, Brazil, 2021. [Google Scholar]
- Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2020: Incidência de Câncer no Brasil; INCA: Rio de Janeiro, Brazil, 2019. [Google Scholar]
- De Vincentiis, L.; Carr, R.A.; Mariani, M.P.; Ferrara, G. Cancer diagnostic rates during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared with the 2018–2019: An audit study from cellular pathology. J. Clin. Pathol. 2020, 74, 187–189. [Google Scholar] [CrossRef]
- Kaufman, H.W.; Chen, Z.; Niles, J.; Fesko, Y. Changes in the number of US patients with newly identified cancer before and during the Coronavirus Disease 2019 (COVID-19) pandemic. JAMA Netw. Open 2020, 3, e2017267. [Google Scholar] [CrossRef]
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A practical approach to the management of cancer patients during the novel Coronavirus disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef]
- Simões e Silva, A.C.; Oliveira, E.A.; Martelli Júnior, H. Coronavirus disease pandemic is a real challenge for Brazil. Front. Public Health 2020, 8, 268. [Google Scholar] [CrossRef]
- Nascimento, J.H.F.; Vieira, A.T.S.; Souza Filho, B.M.; Tomaz, S.C.; Delgado Bocanegra, R.E.; Melo Costa, V.S.; Johnson, L.F.P.; Gusmão-Cunha, A.; Silva Neto, M.M.; Andrade, A.B. Breast cancer in Brazil: Screening program and surgical approach. Cancer Epidemiol. 2021, 73, 101970. [Google Scholar] [CrossRef]
- Lee, O.P.; Cesario, F.C. Relationship between food choices and the development of gastric cancer: A systematic review. Braz. J. Health Rev. 2019, 2, 2640–2656. [Google Scholar] [CrossRef]
- das Neves, I.S.; Cruz, M.S.Q.V.; de Jesus, D.L.; Lima, F.G.F.; Nazeba, K.V.J.F.O.; Monteiro Júnior, M.A.C. Epidemiologicalanalysis of deaths from stomach cancer in Northern Brazil. Res. Soc. Dev. 2021, 10, e39410917503. [Google Scholar] [CrossRef]
- Braga, L.L.B.C.; Ferreira, A.F.; Pinheiro, F.A.S.; Benigno, T.G.D.S.; Heukelbach, J.; de Castro, D.B.; Queiroz, D.M.M.; Miyajima, F.; Ramos, A.N., Jr. Temporal trends and spatial clusters of gastric cancer mortality in Brazil. Rev. Panam. Salud. Publica 2022, 46, e101. [Google Scholar] [CrossRef] [PubMed]
- Hora, B.K.S.; Pereira, P.C.; Brito, M.S.; Cedraz, M.E.S.; Britto Neto, H.S.; de Melo, A.C.C.; Gois, Y.D.C.; de Jesus, C.V.F.; Batista, J.F.C.; Lima, S.O. Spatialand temporal analysis of mortality from gastric cancer in Brazil, 2001 to 2020. Res. Soc. Dev. 2022, 11, e550111436909. [Google Scholar] [CrossRef]
- Meneses, H.d.N.d.M.; Oliveira-da-Costa, M.; Basta, P.C.; Morais, C.G.; Pereira, R.J.B.; de Souza, S.M.S.; Hacon, S.d.S. Mercury Contamination: A Growing Threatto Riverineand Urban Communities in the Brazilian Amazon. Int. J. Environ. Res. Public Health 2022, 19, 2816. [Google Scholar] [CrossRef] [PubMed]
- Custódio, F.B.; Andrade, A.M.G.F.; Guidi, L.R.; Leal, C.A.G.; Gloria, M.B.A. Total mercury in commercialfishesandestimationofBraziliandietaryexposuretomethylmercury. J. Trace Elem. Med. Biol. 2020, 62, 126641. [Google Scholar] [CrossRef]
- Hacon, S.; Barrocas, P.R.G.; de Vasconcellos, A.C.S.; Barcellos, C.; Wasserman, J.C.; Campos, R.C.; Ribeiro, C.; Azevedo-Carloni, F.B. An over view of mercury contamination research in the Amazon basin with an emphasison Brazil. Cad. SaúdePública 2008, 24, 1479–1492. [Google Scholar] [CrossRef]
- Kim, S.; Song, S.H.; Lee, C.W.; Kwon, J.T.; Park, E.Y.; Oh, J.K.; Kim, H.J.; Park, E.; Kim, B. Low-Level Environmental Mercury Exposureand Thyroid Cancer Risk among Residents Living Near National Industrial Complexes in South Korea: A Population-Based Cohort Study. Thyroid 2022, 32, 1118–1128. [Google Scholar] [CrossRef]
- Camargo, J.D.A.S.; dos Santos, J.; Simões, T.C.; Carvalho, J.B.L.; Silva, G.W.D.S.; Dantas, E.S.O.; Rodrigues, W.T.D.S.; Freire, F.H.M.A.; Meira, K.C. Mortality due to breast cancer in a region of high socioeconomic vulnerability in Brazil: Analysis of the effect of age-period and cohort. PLoS ONE 2021, 16, e0255935. [Google Scholar] [CrossRef]
- Bonadio, R.C.; Moreira, O.A.; Testa, L. Breast cancer trends in women younger than 40 years in Brazil. Cancer Epidemiol. 2022, 78, 102139. [Google Scholar] [CrossRef]
- Santos, T.B.D.; Borges, A.K.D.M.; Ferreira, J.D.; Meira, K.C.; Souza, M.C.; Guimarães, R.M.; Jomar, R.T. Prevalence and factors associated with advanced stage breast cancer diagnosis. Cien. Saude Colet. 2022, 27, 471–482. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.A.E.; Alcantara, L.L.M.; Tomazelli, J.G.; Ribeiro, C.M.; Girianelli, V.R.; Santos, É.C.; Claro, I.B.; Almeida, P.F.; Lima, L.D. Evaluationof cervical cancer control actions within Braziland its regions based on data recorded in the Brazilian Unified National Health System. Cad. Saude Publica 2022, 38, e00041722. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, F.M.; Migowski, A.; de Almeida, L.M.; Soares, M.A. Cervical cancerscreening, treatment and prophylaxis in Brazil: Currentand future perspectives for cervical cancer elimination. Front. Med. 2022, 9, 945621. [Google Scholar] [CrossRef]
- Colpani, V.; Falcetta, F.S.; Bidinotto, A.B.; Kops, N.L.; Falavigna, M.; Hammes, L.S.; Benzaken, A.S.; Maranhão, A.G.K.; Domingues, C.M.A.S.; Wendland, E.M. Prevalence of human papillomavirus (HPV) in Brazil: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0229154. [Google Scholar] [CrossRef]
- Thrift, A.P.; El-Serag, H.B. Burden of Gastric Cancer. Clin. Gastroenterol. Hepatol. 2020, 18, 534–542. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, R.A.R.; Mourão, T.C.; Santana, T.B.M.; Favaretto, R.L.; Zequi, S.C.; Guimarães, G.C. Cost-Effectiveness Analysis of Prostate Cancer Screening in Brazil. Value Health Reg. Issues 2021, 26, 89–97. [Google Scholar] [CrossRef]
- GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 2022, 7, 627–647, Erratum in Lancet Gastroenterol. Hepatol. 2022, 7, 704. [Google Scholar] [CrossRef]
- Nascimento, A.Q.; Dantas, D.B.; Melo, G.S.; Gomes, F.C.; de Melo Neto, J.S. Impact of sociodemographic factors and screening, diagnosis, and treatment strategies on colorectal cancer mortality in Brazil: A 20-year ecological study. PLoS ONE 2022, 17, e0274572. [Google Scholar] [CrossRef]
- Dobiesz, B.A.; Oliveira, R.R.; Souza, M.P.; Pedroso, R.B.; Stevanato, K.P.; Pelloso, F.C.; Carvalho, M.D.B.; Pelloso, S.M. Colorectal cancer mortality in women: Trendanalysis in Braziland its regions and states. Rev. Bras. Enferm. 2022, 75, e20210751. [Google Scholar] [CrossRef]
- Kupper, B.E.C.; Ferreira, F.O.; Nakagawa, W.T.; Calsavara, V.F.; Chulam, T.C.; Lopes, A.; Aguiar-Junior, S. Colorectal cancer: Association between sociodemographic variables and the adherence to cancer screening. Arq. Bras. Cir. Dig. 2023, 36, e1729. [Google Scholar] [CrossRef]
- Sampaio, A.P.N.; de Souza, L.P.; de Lima Moreira, J.P.; Luiz, R.R.; Fogaça, H.S.; de Souza, H.S. Geographic Distribution and Time Trends of Colorectal Cancer in Brazil from 2005 to 2018. Dig. Dis. Sci. 2022, 67, 4708–4718. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.K.d.M.; Ferreira, J.D.; Koifman, S.; Koifman, R.J. Câncer de Thyroid no Brasil: Estudo descritivo dos casosinformadospelos registros hospitalares de câncer, 2000–2016. Epidemiol. Serv. Saúde. 2020, 29, e2019503. [Google Scholar] [CrossRef] [PubMed]
- de Morais Fernandes, F.C.G.; de Souza, D.L.B.; Curado, M.P.; de Souza, T.A.; de Almeida Medeiros, A.; Barbosa, I.R. Incidence and mortality from thyroid cancer in Latin America. Trop. Med. Int. Health 2021, 26, 800–809. [Google Scholar] [CrossRef] [PubMed]


| Variables | n (%) |
|---|---|
| Age group | |
| ≤19 years | 12 (0.41) |
| 20–49 years | 917 (31.06) |
| 50–79 years | 1844 (62.47) |
| ≥80 years | 179 (6.06) |
| Sex | |
| Male | 1196 (40.51) |
| Female | 1756 (59.49) |
| Education level | |
| None or <1 year | 238 (8.06) |
| <8 years | 1172 (39.70) |
| 8–10 years | 264 (8.94) |
| 11–14 years | 640 (21.68) |
| >15 years | 155 (6.47) |
| Not reported | 447 (15.14) |
| Previous diagnosis/treatment | |
| With diagnosis/without treatment | 2577 (87.30) |
| With diagnosis/with treatment | 373 (12.64) |
| Not reported | 2 (0.06) |
| Color/ethnicity | |
| Yellow | 183 (6.20) |
| Brown | 1865 (63.18) |
| Black | 52 (1.76) |
| White | 85 (2.88) |
| Indigenous | 4 (0.14) |
| Not reported | 763 (25.85) |
| Primary Tumor Location | OLCH | Pará | Brazil |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Breast | 489 (16.5) | 646 (15.56) | 51,025 (11.96) |
| Cervix | 396 (13.4) | 532 (12.82) | 25,683 (6.02) |
| Stomach | 265 (8.98) | 338 (8.14) | 16,680 (3.91) |
| Prostate | 225 (7.72) | 312 (7.52) | 32,681 (7.66) |
| Non-melanoma skin | 214 (7.25) | 373 (8.99) | 58,306 (13.67) |
| Colon and rectum | 191 (6.47) | 251 (6.05) | 36,426 (8.54) |
| Leukemia, bone marrow | 120 (4.07) | 178 (4.29) | 7236 (1.70) |
| Thyroid | 108 (3.66) | 134 (3.23) | 6526 (1.53) |
| Lungs | 92 (3.12) | 128 (3.08) | 12,755 (2.99) |
| Lymphoma, unspecified | 87 (2.95) | 122 (2.94) | 19,464 (4.56) |
| Lip and oral cavity | 81 (2.74) | 98 (2.36) | 12,975 (3.04) |
| Kidney | 75 (2.54) | 90 (2.17) | 5001 (1.17) |
| Bones and soft tissues | 67 (2.27) | 120 (2.89) | 15,493 (3.63) |
| CNS | 54 (1.83) | 94 (2.26) | 6570 (1.54) |
| Ovary | 51 (1.73) | 70 (1.69) | 6593 (1.55) |
| Liver and intrahepatic bile ducts | 50 (1.69) | 63 (1.52) | 3292 (0.77) |
| Pancreas | 47 (1.59) | 65 (1.57) | 4222 (0.99) |
| Body of uterus | 43 (1.46) | 53 (1.28) | 7244 (1.70) |
| Esophagus | 38 (1.29) | 67 (1.61) | 7794 (1.83) |
| Bladder | 37 (1.25) | 49 (1.18) | 7365 (1.73) |
| Larynx | 33 (1.12) | 44 (1.06) | 5383 (1.26) |
| Penis | 32 (1.08) | 44 (1.06) | 1162 (0.27) |
| Not specified | 30 (1.02) | 59 (1.42) | 48,056 (11.27) |
| Hematopoietic and reticulo endothelial systems, not bone marrow | 23 (0.78) | 49 (1.18) | 3383 (0.79) |
| Testicle | 17 (0.58) | 27 (0.65) | 1873 (0.44) |
| Gallbladder and extrahepatic bile ducts | 15 (0.51) | 19 (0.46) | 2356 (0.55) |
| Small intestine | 10 (0.34) | 11 (0.26) | 1863 (0.44) |
| Nasopharynx | 10 (0.34) | 12 (0.29) | 1097 (0.26) |
| Vulva | 8 (0.27) | 13 (0.31) | 2375 (0.56) |
| Digestive system, unspecified | 8 (0.27) | 8 (0.19) | 3629 (0.85) |
| Ocular | 7 (0.24) | 18 (0.43) | 1035 (0.24) |
| Pharynx | 6 (0.20) | 31 (0.75) | 7114 (1.67) |
| Mediastinum | 5 (0.17) | 7 (0.17) | 1276 (0.30) |
| Nasal cavity and middle ear | 5 (0.17) | 5 (0.12) | 629 (0.15) |
| Paranasal sinuses | 4 (0.14) | 6 (0.14) | 810 (0.19) |
| Vagina | 4 (0.14) | 8 (0.19) | 554 (0.15) |
| Placenta | 3 (0.10) | 3 (0.07) | 307 (0.07) |
| Respiratory system, unspecified | 1 (0.03) | 2 (0.05) | 131 (0.03) |
| Thymus | 1 (0.03) | 2 (0.05) | 145 (0.03) |
| Total | 2952 (100.00) | 4151 (100.00) | 426,509 (100.00) |
| Primary Tumor Location | OLCH n (%) | Brazil n (%) | ||
|---|---|---|---|---|
| Males | Females | Males | Females | |
| Stomach | 179 (67.55) | 86 (32.45) | 8799 (52.75) | 7881 (47.25) |
| Non-melanoma skin | 116 (54.21) | 98 (45.79) | 27,827 (76.39) | 30,479 (23.61) |
| Colon and rectum | 89 (46.60) | 102 (53.40) | 17,965 (49.32) | 18,461 (50.68) |
| Leukemia, bone marrow | 69 (57.50) | 51 (42.50) | 4033 (55.74) | 3203 (44.26) |
| Thyroid | 15 (13.89) | 93 (86.11) | 1027 (15.74) | 5499 (84.26) |
| Lungs | 50 (54.35) | 42 (45.65) | 6950 (54.49) | 5805 (45.51) |
| Lymphoma, unspecified | 53 (60.92) | 34 (39.08) | 10,170 (52.25) | 9294 (47.75) |
| Lip and oral cavity | 50 (61.73) | 31 (38.27) | 8992 (69.30) | 3983 (30.70) |
| Kidney | 43 (57.33) | 32 (42.67) | 2856 (57.11) | 2145 (42.89) |
| Bones and soft tissues | 27 (40.30) | 40 (59.70) | 7747 (50.00) | 7746 (50.00) |
| CNS | 31 (57.41) | 23 (42.59) | 3433 (52.25) | 3137 (47.75) |
| Liver and intrahepatic bile ducts | 26 (52.00) | 24 (48.00) | 1710 (51.94) | 1582 (48.06) |
| Pancreas | 26 (55.32) | 21 (44.68) | 2098 (49.69) | 2124 (50.31) |
| Esophagus | 23 (60.53) | 15 (39.47) | 5457 (70.02) | 2337 (29.98) |
| Bladder | 30 (81.08) | 7 (18.92) | 5116 (69.63) | 2231 (30.37) |
| Larynx | 25 (75.76) | 8 (24.24) | 4610 (85.64) | 773 (14.36) |
| Hematopoietic and reticuloendothelial systems, not bone marrow | 11 (47.83) | 12 (52.17) | 1506 (44.52) | 1877 (55.48) |
| Gallbladder and extrahepatic bile ducts | 4 (26.67) | 11 (73.33) | 929 (39.43) | 1427 (60.57) |
| Small intestine | 4 (40.00) | 6 (60.00) | 910 (48.85) | 953 (51.15) |
| Nasopharynx | 4 (40.00) | 6 (60.00) | 768 (70.01) | 329 (29.99) |
| Digestive system, unspecified | 4 (50.00) | 4 (50.00) | 1662 (45.80) | 1967 (54.20) |
| Ocular | 6 (85.71) | 1 (14.29) | 569 (54.98) | 466 (45.02) |
| Pharynx | 4 (66.67) | 2 (33.33) | 5903 (82.98) | 1211 (17.02) |
| Mediastinum | 3 (60.00) | 2 (40.00) | 597 (46.79) | 679 (53.21) |
| Nasal cavity and middle ear | 2 (40.00) | 3 (60.00) | 398 (63.28) | 231 (36.72) |
| Paranasal sinuses | 2 (50.00) | 2 (50.00) | 456 (56.30) | 354 (43.70) |
| Respiratory system, unspecified | 1 (100.00) | - | 69 (52.67) | 62 (47.33) |
| Thymus | - | 1 (100.00) | 72 (49.66) | 73 (50.34) |
| Location (ICD-O) | Female (%) | Male (%) |
|---|---|---|
| Guajará | 864 (100) | 608 (100) |
| Stomach (C16) | 52 (6.02) | 86 (14.14) |
| Colon and rectum (C18–C21) | 48 (5.56) | 48 (7.9) |
| Bone marrow leukemia (C42.1) | 36 (4.17) | 41 (6.74) |
| Breast (C50) | 279 (32.29) | - |
| Cervix (C53) | 164 (18.98) | - |
| Prostate (C61) | - | 128 (21.05) |
| Thyroid (C73) | 39 (4.51) | 8 (1.32) |
| Guamá | 239 (100) | 143 (100) |
| Stomach (C16) | 13 (5.44) | 31 (21.68) |
| Colon and rectum (C18–C21) | 13 (5.44) | 10 (7.0) |
| Breast (C50) | 61 (25.52) | 2 (1.4) |
| Cervix (C53) | 59 (24.69) | - |
| Prostate (C61) | - | 25 (17.48) |
| Thyroid (C73) | 11 (4.6) | 2 (1.4) |
| Caeté River | 162 (100) | 103 (100) |
| Stomach (C16) | 7 (4.32) | 22 (21.36) |
| Colon and rectum (C18–C21) | 16 (9.87) | 8 (7.76) |
| Breast (C50) | 34 (20.99) | 1 (4.0) |
| Cervix (C53) | 48 (29.63) | - |
| Prostate (C61) | - | 17 (16.50) |
| Thyroid (C73) | 5 (3.09) | - |
| Lymphoma (C77) | 2 (1.23) | 5 (4.85) |
| Capim River | 148 (100) | 91 (100) |
| Stomach (C16) | 8 (5.41) | 17 (18.68) |
| Colon and rectum (C18–C21) | 8 (5.41) | 7 (7.7) |
| Breast (C50) | 29 (19.59) | 1 (1.10) |
| Cervix (C53) | 38 (25.68) | - |
| Prostate (C61) | - | 13 (14.29) |
| Thyroid (C73) | 10 (6.76) | - |
| Marajó | 82 (100) | 61 (100) |
| Stomach (C16) | - | 8 (13.11) |
| Breast (C50) | 16 (19.51) | 1 (4.0) |
| Cervix (C53) | 39 (47.56) | - |
| Prostate (C61) | - | 10 (16.39) |
| Thyroid (C73) | 6 (7.32) | - |
| Lymphoma (C77) | 2 (2.44) | 5 (8.20) |
| Tocantins | 148 (100) | 115 (100) |
| Stomach (C16) | 3 (2.03) | 12 (10.43) |
| Colon and rectum (C18–C21) | 13 (8.78) | 7 (6.09) |
| Breast (C50) | 34 (22.97) | - |
| Cervix (C53) | 31 (20.95) | - |
| Prostate (C61) | - | 26 (22.61) |
| Thyroid (C73) | 8 (5.41) | - |
| Topography (ICD-O) | Female (%) | Male (%) |
|---|---|---|
| Tucuruí Lake | 26 (100) | 25 (100) |
| Stomach (C16) | 1 (3.85) | 1 (4.0) |
| Liver and intrahepatic bile ducts (C22) | 1 (3.85) | 3 (12.0) |
| Breast (C50) | 7 (26.92) | 1 (4.0) |
| Cervix (C53) | 4 (15.38) | - |
| Thyroid (C73) | 6 (23.08) | 1 (4.0) |
| Carajás | 36 (100) | 16 (100) |
| Stomach (C16) | 1 (2.78) | 1 (6.25) |
| Larynx (C32) | - | 2 (12.5) |
| Lung (C34) | 1 (2.78) | 1 (6.25) |
| Bone marrow leukemia (C42.1) | 3 (8.33) | 4 (25.0) |
| Breast (C50) | 12 (33.33) | - |
| Cervix (C53) | 3 (8.33) | - |
| Thyroid (C73) | 6 (16.67) | 2 (12.5) |
| Xingu | 19 (100) | 19 (100) |
| Bone marrow leukemia (C42.1) | - | 4 (21.05) |
| Breast (C50) | 5 (26.32) | - |
| Cervix (C53) | 4 (21.05) | - |
| Prostate (C61) | - | 2 (10.53) |
| Araguaia | 11 (100) | 6 (100) |
| Bone marrow leukemia (C42.1) | - | 1 (16.67) |
| Breast (C50) | 2 (18.18) | 1 (16.67) |
| Cervix (C53) | 3 (27.27) | - |
| Prostate (C61) | - | 1 (16.67) |
| Frontal lobe of the CNS (C71) | 2 (18.18) | - |
| Lower Amazon | 7 (100) | 4 (100) |
| Stomach (C16) | 1 (14.29) | - |
| Lung (C34) | 2 (28.57) | - |
| Breast (C50) | 2 (28.57) | - |
| Cervix (C53) | 1 (14.29) | - |
| Prostate (C61) | - | 1 (25.0) |
| Thyroid (C73) | - | 2 (50.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaves, J.R.; Otake, M.I.T.; Alcantara, D.D.F.Á.; Lima, R.S.; de Souza, A.P.B.; da Costa Rodrigues, J.S.; Imbiriba, M.M.B.G.; Burbano, R.M.R. Epidemiological Profile of Ophir Loyola Cancer Hospital: A Snapshot of the Incidence of Solid Neoplasms in the Eastern Amazon. Med. Sci. 2023, 11, 68. https://doi.org/10.3390/medsci11040068
Chaves JR, Otake MIT, Alcantara DDFÁ, Lima RS, de Souza APB, da Costa Rodrigues JS, Imbiriba MMBG, Burbano RMR. Epidemiological Profile of Ophir Loyola Cancer Hospital: A Snapshot of the Incidence of Solid Neoplasms in the Eastern Amazon. Medical Sciences. 2023; 11(4):68. https://doi.org/10.3390/medsci11040068
Chicago/Turabian StyleChaves, Juliana Ramos, Mateus Itiro Tamazawskas Otake, Diego Di Felipe Ávila Alcantara, Rosilene Silva Lima, Ana Paula Borges de Souza, Janaina Silva da Costa Rodrigues, Margareth Maria Braun Guimarães Imbiriba, and Rommel Mario Rodriguez Burbano. 2023. "Epidemiological Profile of Ophir Loyola Cancer Hospital: A Snapshot of the Incidence of Solid Neoplasms in the Eastern Amazon" Medical Sciences 11, no. 4: 68. https://doi.org/10.3390/medsci11040068
APA StyleChaves, J. R., Otake, M. I. T., Alcantara, D. D. F. Á., Lima, R. S., de Souza, A. P. B., da Costa Rodrigues, J. S., Imbiriba, M. M. B. G., & Burbano, R. M. R. (2023). Epidemiological Profile of Ophir Loyola Cancer Hospital: A Snapshot of the Incidence of Solid Neoplasms in the Eastern Amazon. Medical Sciences, 11(4), 68. https://doi.org/10.3390/medsci11040068







