- Article
Sociodemographic and Clinical Predictors of Chronic Disease Outcomes in a Colombian Population: A Cross-Sectional Analysis of 2495 Patients
- Adriana Guzmán Sánchez,
- Lilibeth Sánchez-Guette and
- Carlos Andrés Collazos Morales
- + 3 authors
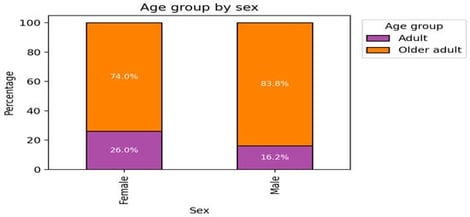
Objectives: This study sought to identify sociodemographic and clinical predictors associated with the absence versus presence of alterations in mental, neurological, cardiovascular, osteomuscular, and pulmonary conditions, to provide information towards targeted interventions for non-communicable diseases (NCDs) in urban Colombian populations. Methods: A cross-sectional analysis was performed on 2495 patients (70.1% women) from public health facilities in Bogotá, using the Colombia Open Data “Enfermedades Crónicas” dataset collected between January and December 2023. Associations between sociodemographic variables (sex, age groups, education, and ethnicity) and clinical variables (BMI, type of disability, COVID-19 vaccination status, psychiatric risk, and the modified Medical Research Council dyspnea scale) were examined in relation to health outcomes. Data cleaning involved the exclusion of 107 outliers identified by z-scores >|3| using Microsoft Excel 365. Categorical variables were summarized using frequencies and proportions, and Pearson’s chi-square tests were applied to assess bivariate associations (e.g., BMI–health conditions, and sex–disability associations). Multivariable Firth’s penalized logistic regression models (implemented in Python 3.14 and Jamovi 2.3) were used to predict the absence of alteration (reference category: presence), adjusting for multicollinearity (variable inflation factor, VIF) and events-per-variable ratios. Odds ratios (ORs), 95% confidence intervals (CIs), and two-tailed p-values were estimated, with statistical significance set at p < 0.05. Results: Women predominated in obesity (81% vs. 19% in men, p < 0.001) and in unaltered conditions (e.g., 71% of cases without pulmonary alterations) but exhibited a lower crude prevalence of disability (6% vs. 16% in men, p < 0.001). Men represented higher proportions of alterations (e.g., 53.8% of pulmonary cases vs. 46.2%, p = 0.006) and mental disabilities (70%, p < 0.001). Firth regression models identified the following predictors: for mental alteration, a single COVID-19 vaccine dose (OR = 2.39, 95% CI 1.12–5.09, p = 0.024), occupation (OR = 1.07, 95% CI 1.05–1.10, p < 0.001), BMI (OR = 0.96, 95% CI 0.93–0.98, p < 0.001), and disability (inverted OR = 4.35, 95% CI 2.56–7.69, p < 0.001); for neurological alteration, occupation (OR = 1.15, 95% CI 1.10–1.21, p < 0.001) and disability (inverted OR = 3.45, 95% CI 1.43–8.33, p = 0.006); for cardiovascular alteration, BMI (OR = 1.02, 95% CI 1.00–1.03, p = 0.042); for osteomuscular alteration, occupation (OR = 1.03, 95% CI 1.01–1.06, p = 0.011); and for pulmonary alteration, occupation (OR = 1.07, 95% CI 1.03–1.11, p = 0.001). The models demonstrated a moderate to excellent goodness-of-fit (R2 = 0.25–0.72). Conclusions: Sex, BMI, disability status, occupation, and COVID-19 vaccination status emerged as key predictors of NCD-related alterations, highlighting specific vulnerabilities such as partial immunization for mental health risk, and disability for mental and neurological outcomes. Targeted interventions, including completion of vaccination schedules, mitigation of occupational exposure, BMI management, and disability-inclusive care, may reduce health disparities and support PAHO/WHO 2025 targets. Longitudinal studies are recommended to establish causal relationships in the context of Colombia’s fragmented subnational NCD evidence base.
7 February 2026