1. Introduction
Computed tomography (CT) is an essential and powerful radiological tool. CT imaging allows for the detection and assessment of diseases and other medical conditions, providing a basis for medical diagnosis and treatment. This method benefits from speed, accuracy, versatility, and non-invasiveness, which has led to its increased utilization for medical diagnoses. However, CT delivers a markedly higher radiation dose than alternative imaging technologies, which disproportionately affects children owing to their smaller body proportion. The use of CT on paediatric patients increases the probability of developing cancer throughout their lifetimes since their still developing tissues and organs are more susceptible to the effects of cellular deterioration and destruction than those of adults. At present, CT accounts for approximately 50% of medically produced radiation exposure [
1,
2]. Since CT results in the exposure to the effects of ionising radiation, there are concerns that the increased use of CT could induce delayed deleterious effects, particularly for young patients [
3]. Results from several large, long-term studies suggest that the frequency of leukaemia and brain cancer is slightly increased in patients who received a CT at a young age [
4,
5,
6]. While the causation of a lifetime cancer risk due to low dose radiation exposure (<100 mSv) has not been fully established, the danger is roughly calculated as two to five times greater for paediatric patients than adults [
6,
7,
8,
9].
CT scan practitioners, particularly radiographers and radiologists, must apply a risk-benefit analysis for each exposure to medical radiation, as prescribed by national and international regulations [
9,
10,
11]. Consequently, along with establishing the necessity for a paediatric CT investigation, it is also essential that the CT examination be optimised according to the child’s physical characteristics and/or underlying clinical manifestations [
11,
12,
13,
14,
15]. To successfully perform their crucial roles, radiographers and radiologists need to be fully educated and thoroughly trained in the CT strategies they implement. The healthcare practitioners keep enhancing the ionizing radiation exposure protocols to achieve low delivered doses without affecting the produced image quality. Most CT examinations require that patients be exposed to the lowest amount of radiation achievable to safeguard the patients while maintaining the benefits of CT. There are various parameters for managing and controlling the radiation output and image quality of CT, including peak kilovoltage (kVp), tube current-time (mAs), slice thickness, pitch, automatic tube current modulation (ATCM), reconstruction algorithms, and detector configuration. It is paramount that the technologists determine the radiation dose needed to obtain the best image quality with minimal radiation exposure [
16,
17]. Despite numerous attempts to educate health professionals, including radiographers and radiologists, regarding the use of CT in paediatrics, analytical studies indicate a low level of cognizance relating to radiation quantities and the dangers associated with frequent CT use on paediatric patients, thus, leading to the exposure of patients to undesirable quantities of ionising radiation [
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32]. Therefore, it is necessary that radiographers participate in continuing professional development (CPD) training to guarantee radiological safeguards [
3,
33,
34,
35]. This will require continued study to stay up-to-date with the field [
36,
37].
In this work, the existing protocols of the paediatric population to CT radiation was assessed by surveying the knowledge and expertise of radiologists in Saudi Arabian hospitals. The findings of this study can be used to develop a strategy to reduce unnecessary radiation exposure via the use of alternative techniques and improved training courses.
2. Materials and Methods
2.1. Survey Preparation and Administration
To assess the existing knowledge and expertise for the radiologists, and provide a comprehensive view about the wide spectrum of CT techniques of the paediatric population in Saudi Arabia, a questionnaire has been designed to cover the primary aspects related to the provided CT services and evaluating the potential radiation risk qualitatively. The first draft was reviewed by experts to determine content validity and the appropriateness of the knowledge parameters. Based on this review, a second draft was prepared and used in a pilot survey to evaluate the reliability of the data and the nature of the responses. Although the reliability was acceptable, a number of the respondents reported difficulties in understanding the question with respect to the answer options. Based on these results, a third draft was prepared to simplify the questions and prevent any misunderstandings in the questionnaire design (see
Supplementary). The final survey was generated on Google Surveys. The majority of the questions in this study provided options from which participants had to choose a response and furnished candidates with an index containing pre-defined, conceivable responses; although, participants were able to give more detailed answers if they preferred.
The survey was structured and close-ended. Ethical approval for this study was obtained from the Ethics Committee at the College of Medicine, King Khalid University, Abha, Kingdom of Saudi Arabia (REC# 2015-0l-29). Completion of the anonymized questionnaire was considered to be consent for inclusion in the study. The survey link was distributed to a random selection of 600 radiologists within the Kingdom of Saudi Arabia. A total of 127 responses was received, 26 of which were incomplete and omitted from the data set, leaving 101 surveys for the final analysis. The population contains a spectrum of radiologists holding various academic and professional degrees following the official classifications provided by the Saudi Commission for Health Specialties, which include bachelor of medicine degree (MBBS), postgraduate diploma, master′s degree and academic philosophy of doctorate (PhD) or medical professional graduate (MD) degrees.
Section A of the questionnaire inquired about the participant’s background, particularly academic qualification, CT experience, training and education on the risks associated with paediatric CT radiation, and participation in the various workshops, seminars, conferences, and self-directed studies (books, journals, etc.) related to CT. This section also focused on their experience in accredited courses conducted by professional associations.
Section B was concerned with the respondent’s knowledge regarding CT protocols. The main queries focused on the frequency of updating CT scan protocols, the confidence of the radiologist regarding the correct modulation of the CT parameters, and basic questions relating to CT scan procedures.
Section C was related to the participant’s knowledge regarding CT doses in paediatric patients. It tested their knowledge regarding familiarity with the ‘as low as reasonably achievable’ (ALARA) principle, the relationship between cancer and CT dose, alternative medical imaging techniques, organisational policy for explaining the effects of CT radiation on the child, explaining these effects to the child’s guardian(s), etc.
2.2. Data Management and Analysis
Data were analysed using Statistical Product and Service Solutions (SPSS) v20. The reliability of the data was determined by calculating Cronbach’s alpha (0.871) and indicated that the data was suitable for further analysis. A knowledge score was calculated for each question with correct and incorrect responses given a score of 1 and 0, respectively. The knowledge score of all participants was represented as a percentage for CT protocol, radiation dose, and radiation risk (
Table 1 and
Table 2). Furthermore, descriptive statistics were performed to compare knowledge scores (in percentages) regarding CT protocol and radiation dose and risk based on education, experience and training (
Table 3,
Table 4,
Table 5 and
Table 6). Analysis of variance (ANOVA) was used to compare CT protocol and radiation dose and risk knowledge on various parameters.
3. Results
Of the 600 radiologists included in the study, a total of 101 (16.8%) from different health sectors completed the questionnaire. Most of the participants came from the Ministry of Health (44.6%). The majority of participants had a PhD or MD (70.7%), with the remaining responses coming from holders of a Master’s degree (13.8%), an MBBS (13.8%), or a postgraduate diploma (1.9%). Among the participants, 50% had greater than 10 years of experience in radiology and 60% regularly participated in periodically organized training and education concerning CT radiation risk in paediatrics.
Most participants (65%) were aware of CT radiation dose and the associated risks in paediatric CT examinations (
Table 1 and
Figure 1). The majority of respondents (65% ± 13.5%) comprehended the dangers of carcinogenicity to the patient that occur as a consequence of a CT scan and 80% believed that the dangers of carcinogenicity are elevated due to CT scans. However, some respondents underestimated the risk associated with CT radiation in paediatric investigations of the head (51.5%), the chest (43.5%), and the abdomen (35%).
The understanding of the risk of cancer to the patient that results from a CT scan (R1); increase of risk of cancer as a result of CT scan (R2); radiation risk in paediatric CT examination of the head (R3); radiation risk in paediatric CT examination of the chest (R4); and radiation risk in paediatric CT examination of the abdomen (R5).
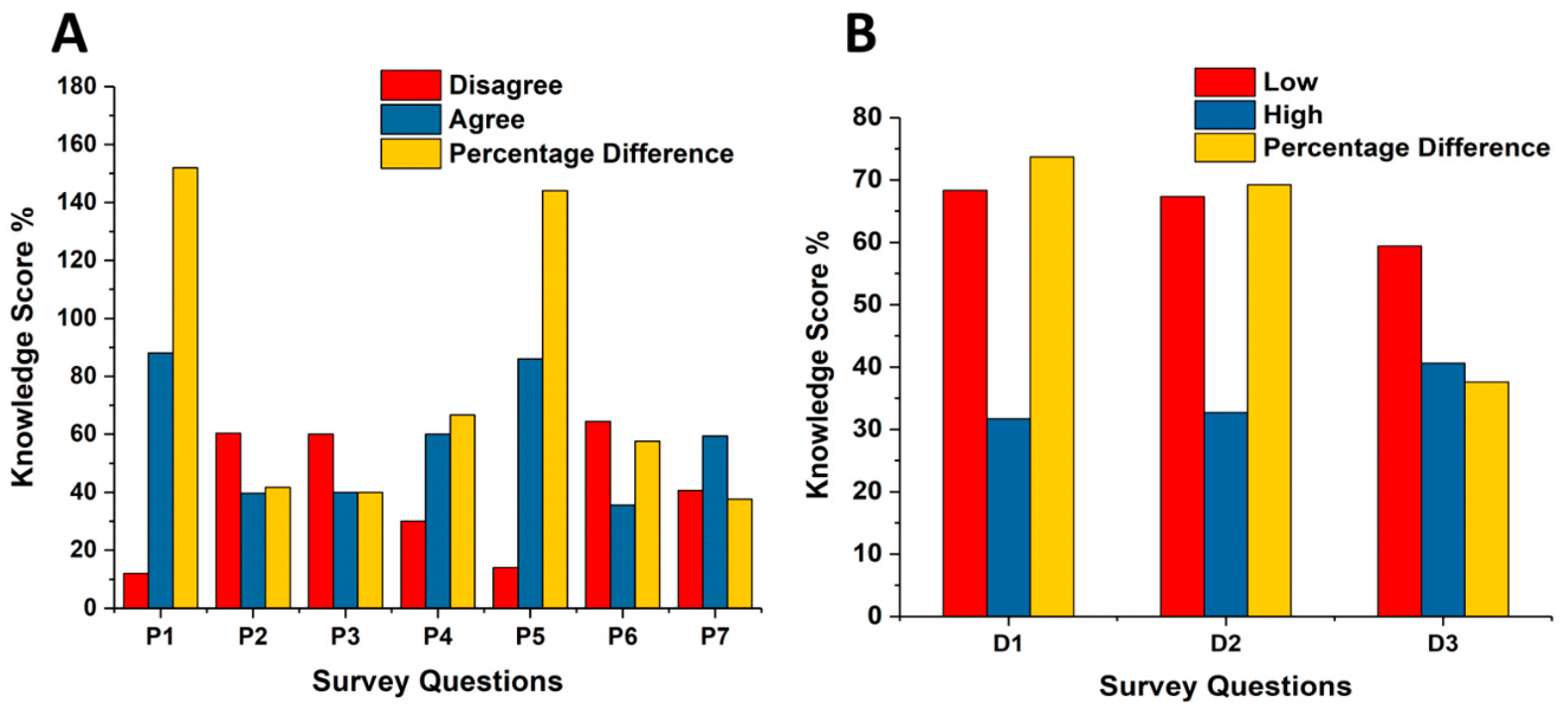
Participants were asked about the procedures within their department and their knowledge about CT protocols (
Table 2 and
Figure 2). Most of the respondents (88%) were familiar with the ALARA principle and 60% of the participants were not familiar with the effect of updating and altering the CT protocol on image quality and radiation dose. A significant number of participants (86%) considered an alternative imaging modality other than CT for paediatric examinations. Over half of the participants (59.4%) indicated that their departments had a policy to inform patients′ families about radiation benefit versus risk and the radiation dose in CT examinations. Many participants believed that the radiation dose for CT examinations of the head (68.3%), chest (67.3%), and abdomen (58.4%) in their department are considerably low. These score results indicate that most of the participants have a good estimation for the CT examination of the head and underestimated the radiation doses for the chest and abdomen CT examinations compared to the reported estimated values in the Saudi Arabia CT centres for head, the abdomen, and chest examinations, which were found to be in the range of 0.6 and 2.5 mSv, 6.7 and 11.2 mSv, and 4.3 and 11.6 mSv [
38,
39]; i.e., the majority of the participants were able to recognize the potential risk based on their knowledge of the delivered dose.
Familiarity with ALARA (as low as reasonably achievable) principle (P1); familiarity with CT protocols updating (P2). Participants’ confidence in altering CT protocol (P3); knowledge and confident regarding the correct modulation of the CT parameters (P4). Participants’ consideration of alternative imaging techniques (P5); discussion with parents involving explanations concerning the radiation dose (P6); organisational policy for explaining the impact of CT radiation on the paediatric patient to the parent (P7); radiation dose for head CT scan (D1); radiation dose for chest CT scan (D2); and radiation dose for abdominal CT scan (D3).
The impact of the participants’ academic qualification, experience, and training on their knowledge concerning CT protocols and radiation dose and risk was then analysed.
Table 3,
Table 4 and
Table 5 and
Figure 3,
Figure 4 and
Figure 5 represent the participants knowledge scores as a percentage for CT protocol, radiation dose, and radiation risk based on their academic qualification, experience, and training. The overall mean score of the correct answers for CT protocol information and CT radiation dose were 55.6% and 64%, respectively. The PhD/MD participants reported the highest percentage of the correct answers (57.6%) about CT protocol information (
Table 3 and
Figure 3). No significant difference was observed in the CT protocol knowledge score based on academic qualifications. Postgraduate diploma participants reported the highest percentage of correct answers (91.67%) regarding CT radiation dose and its impact in diagnostic radiology, followed by Master’s (69%) and PhD/MD (64.3%) participants. No significant difference was observed for the CT radiation dose knowledge score based on academic qualifications (
Table 3).
Participants with more than 20 years of experience had the highest knowledge score for both CT protocol (61%) and radiation dose (72.7%) information (
Table 4 and
Figure 4). No significant difference was observed between any other experience groups.
Participants having monthly training reported the greatest number of accurate replies regarding CT protocol (60%) and radiation dose (70%) information (
Table 5 and
Figure 5). There were no significant differences among participants who received training at longer intervals (
Table 5).
Taken together, these analyses show that there was no correlation between knowledge scores and qualification, experience, or training (
Table 6).
4. Discussion
Due to the rapid increase in the use of CT technology in paediatric medicine, special consideration and precautions should be taken. Many organisations, such as the International Commission on Radiation Protection (ICRP), National Cancer Institute (NCI), United States Food and Drug Administration (FDA), and International Atomic Energy Agency (IAEA), have developed guidelines for CT radiation doses in paediatric examinations [
40,
41,
42]. These guidelines were established on the concepts of radiation safety, justification, optimisation, and constraints, the most important being justification. Many studies have been conducted to optimise CT radiation dose for paediatric examinations, most of which show that many centres were still using an adult protocol for imaging paediatric patients [
43]. Without establishing appropriate guidelines and knowledge, paediatric patients could be at high risk during these examinations. It is, therefore, important not only to abide by these principles but to consider alternative, non-ionising radiation examinations in paediatrics. Our results show a good understanding and awareness of alternative medical imaging investigations, other than CT.
The potential risk from CT radiation in paediatric examinations must be justified based on risk to benefit evaluation and optimized based on ALARA principle [
14,
44,
45]. Health centres, together with authorities, should regulate CT clinical practices based on published guidelines or by developing their own guidelines to minimize paediatric patients’ exposure. Considering an alternative imaging modality other than CT examinations will reduce the level of risk. In addition, clinical centres should have a coherent policy to provide patients’ families with clear information regarding the radiation dose, as well as the risk associated with CT radiation exposure versus the benefits of this particular examination.
This work evaluated the knowledge of radiologists regarding the quantity of CT radiation used and its potential risk in paediatrics examinations. The study includes their comprehension of the concepts of protection against radiation and its associated risks. Additionally, the influence of their qualifications, experience, and training on their understanding of CT radiation dose and protocols was investigated.
Out of the 600 contacted radiologists, 101 (16.8%) from different health sectors completed the questionnaire, most of whom held PhDs/MD (70.7%). Of the respondents, 88% were familiar with the ALARA principle and 86% were in favour of considering alternative imaging modalities other than CT for paediatric examinations. This is comparable to Almohiy et al. (2015) study concerning ophthalmologists, of whom 92% were in favour of using another imaging modality [
46]. Most respondents (65% ± 13.5) had a satisfactory understanding of the risks of carcinogenicity that occurs as a consequence of a CT scan. These high scores, when compared with previous findings [
6,
30,
46], indicate an improvement in the level of knowledge and awareness of the ALARA principle and the fundamental principles of radiation protection.
Although the respondents showed a good comprehension of the dangers of carcinogenicity to the patient arising from CT scans, the comprehension of the quantity of CT radiation and risks in specific examination protocols was variable across the participants, many of whom underestimated the risk to paediatric patients during CT of the head (51.5%), chest (43.5%), and abdomen (35%) (
Figure 1). This is consistent with previous results found in the literature [
6,
30]. The majority of respondents were aware that the radiation risk during abdominal and chest examinations is significantly higher than during head CT examinations, which is consistent with reported dose data form Saudi Arabic CT centres [
38,
39].
A minimal variation of the knowledge of the participants about CT protocols has been recognised with the years of experience. For instance, the knowledge score for the participants with 6 to 20 Years working experience is slightly lower than the score of participants with ≥5 years (i.e., ~8.54% difference). This variation is mainly due to the recognised differences of the number of participants, when they classified based on their years of experience.
This study has some limitations. The study was based on self-reporting, which cannot fully validate the comprehension of radiologists regarding exposure in a radiological protocol. Nevertheless, it surveys the viewpoints and perspectives of radiologists who are involved in performing these examinations. This analysis takes into account the experience, qualification, and training of the radiologists when assessing their knowledge score. However, we found no correlation between knowledge and qualification or training (
p > 0.05). Furthermore, this study involved randomly selected radiologists from different specialities. It is possible that radiologists specializing in head, chest or abdominal imaging would have superior knowledge scores. An insignificant correlation between knowledge score and qualification and training was also reported by Saeed et al. [
47]. Therefore, the radiation protection training programme for radiologists supported by several health institutes may be inefficient.