Abstract
Background: Urinary tract infections (UTIs) are major healthcare problems that are usually treated empirically. However, antimicrobial resistance has been increasing across many settings. This study aims to elucidate the antibiotic resistance profiles of three common uropathogens, Escherichia coli (E. coli), Klebsiella pneumoniae (K. pneumoniae), and Proteus mirabilis (P. mirabilis) and compare between extended spectrum beta-lactamase (ESBL) and non-ESBL strains among Lebanese patients. Methods: This retrospective study was conducted at multiple tertiary healthcare centers in South Lebanon, between January and September 2017, including 551 patients of all age groups. Demographic, clinical, and laboratory data of patients were collected and analyzed statistically. Results: The prevalence of UTI in Lebanon was highest in adults between 19 and 64 years (44%). E. coli was the predominant uropathogenic organism (67.1%) followed by K. pneumoniae (10%) and P. mirabilis (3.7%). ESBL represented 32.9% of the UTI agents. The three common uropathogens studied were found to be most susceptible to imipenem (100%) and meropenem (100%). Interestingly, 115 (25.1%) out of the 458 E. coli isolates were resistant to more than eight antibiotics while 107 (23.4%) were susceptible to all antibiotics studied. Conclusions: Our study underlined the importance of adequate antimicrobial prescription for UTIs in Lebanon to avoid multidrug resistance.
1. Introduction
Urinary tract infections (UTIs) are major healthcare problems commonly acquired in both community—community-associated urinary tract infections (CAUTIs)—and hospital—hospital-associated urinary tract infections (HAUTIs)—settings [1]. UTIs are usually caused by bacterial infections, including Gram positive and Gram negative organisms [2]. They occur in females more than males due to anatomical variations, and they mostly affect the bladder—cystitis—and the urethra—urethritis [3]. In this context, approximately 60% of females develop a UTI at least once in their lifetime [3]. UTIs can affect both the lower (bladder and urethra) or upper (pyelonephritis) urinary system, and can be either classified as uncomplicated (occurring in a normal non-pregnant host with no anatomical or functional abnormalities) or complicated [4].
To be diagnosed with a UTI, a patient must have urinary signs/symptoms in addition to positive urine culture demonstrating >1000 cfu/mL of a known uropathogen [5]. In this context, the presence of bacteria in the collected urine of a patient is defined as bacteriuria [6]. The most commonly isolated bacterium in urine cultures is Escherichia coli (E. coli; around 80% of cases [7]) followed by Klebsiella pneumoniae (K. pneumoniae) and Proteus mirabilis (P. mirabilis) [8,9]. In a retrospective study of 10 years duration by Daoud et al., E. coli was found to be the most commonly isolated organism from positive urine cultures among Lebanese people [10].
The treatment of UTIs usually comprises administering empiric antibiotic therapy, while there is no need, in most cases, to order urine culture and antibiotic susceptibility test [11]. Nevertheless, antimicrobial resistance has been increasing across many settings [12,13], which is attributed in large part to antibiotic misuse. Multidrug resistant (MDR) organism, by definition, is a germ that is resistant to more than three classes of antibiotics [14]. A review of literature shows that there is an increase in extended spectrum beta-lactamase (ESBL)-producing MDR organisms among both CAUTIs and HAUTIs, threatening the public health sector as a whole [15]. Infections caused by MDR organisms are associated with longer hospital stay and increased financial burden [16], not to mention poorer patient outcomes, delayed symptoms resolution, and advanced disease progression in case of ascending infections [17]. In Lebanon, the frequency of UTIs caused by ESBL-producing organisms is around 32% as reported by Chamoun et al. [16].
A wide range of antimicrobial agents is used to treat infections caused by E. coli, K. pneumoniae, and P. mirabilis [18,19,20]. Nevertheless, these organisms produce the beta-lactamase enzyme which render them resistant to most classes of antibiotics, hence referred to as ESBL-producing organisms [21]. Nowadays, carbapenems are considered the treatment of choice for such organisms [22]. In our present study, we analyzed the epidemiology of UTI in Lebanese hospitals in South Lebanon over a period of 9 months. In addition, we elucidated the profiles of antimicrobial susceptibility to the three common uropathogens: E. coli, K. pneumoniae, and P. mirabilis, and compared between ESBL and non-ESBL producing strains among Lebanese patients.
2. Materials and Methods
2.1. Study Design and Setting
This retrospective cohort study was conducted at multiple tertiary healthcare centers located in South Lebanon, including patients of all age groups attending the medical laboratories or urology departments of the healthcare centers between 1 January and 30 September 2017.
2.2. Study Participants
Electronic search in the records of the laboratory information system for urine samples and the results of each antibiogram was conducted. Patients whose urine culture results did not meet the definition for UTI established according to the clinical practice guidelines (CPGs) [23] and those who were non-Lebanese were excluded from the study.
2.3. Sample Size and Power of the Study
In our region, the detected prevalence of UTI upon hospital admission was 24.2% [24]. A prior statistical power analysis using GPower 3.1.9.2 software (Heinrich-Heine-Universität, Düsseldorf, Germany) revealed that the sample size n = 551 was enough to attain a statistical power of at least 80% with alpha error of 5%, balanced on each side, and effect size set to 5%.
2.4. Data Collection
Patient data was also collected in a special form designed for this study. These data included patients’ demographics (age, gender, and date of collection), type of hospital admission (outpatient or inpatient), urine cultures and antibiograms, and patients’ laboratory findings (White Blood Cell—WBC, C-reactive Protein—CRP, Blood Urea Nitrogen—BUN, creatinine, and urine pH).
2.5. Ethics Approval and Consent to Participate and Publication
The study was conducted under the Research Ethics Committee approval of the Lebanese University. In accordance with the Declaration of Helsinki, all patients enrolled in this study provided written informed consent for both participation and publication of identifying information. Ethical clearance was taken as per the norms and in accordance with relevant guidelines and regulations of the Lebanese University and the tertiary healthcare centers included. This study will be done in a manner that ensures the confidentiality of patients. In addition, chart review was carried out by CITI (Collaborative Institutional Training Initiative) certified researchers. All data collected were de-identified and stored at the principal investigator’s office.
2.6. Determination of Extended-Spectrum β-Lactamases (ESBL)
ESBL production was assessed by the medical laboratory team of the healthcare centers. Strain ATCC 25,922 was used as a quality control strain for antibiotic susceptibility testing. For initial ESBL screening of each common uropathogen, isolates showing resistance to a third-generation cephalosporin antibiotic (30 μg) using the disk diffusion method were identified as potential ESBL producers. The double-disc synergy test (DDST) was carried out for the phenotypic confirmation of ESBL production. For this test, a third-generation cephalosporin (ceftriaxone) antibiotic disc (30 μg) was placed 25 mm away from a combination disc containing this last in addition to clavulanic acid (20/10 μg). According to clinical and laboratory standards institute (CLSI) guidelines [25], the zone of inhibition between the combination disc and the third-generation cephalosporin disc differed by ≥5 mm, the strain was identified as ESBL-producing.
2.7. Statistical Analysis
Quantitative variables were tested for normality distribution using the Kolmogorov–Smirnov test. Descriptive statistics were carried out and reported as frequencies and percentages for categorical variables and median and interquartile range (quartile 1–quartile 3) for continuous ones. After tabulating the patients’ demographic factors, baseline comparisons between the three studied groups (E. coli, K. pneumoniae, and P. mirabilis) were performed using the Jonckheere–Terpstra test for continuous variables. A chi-squared test was used to evaluate any significant difference between the categorical variables. Mann–Whitney test were used to assess differences between ESBL and non-ESBL groups for laboratory data. Statistical Package for Social Science software (SPSS, Inc., version 24.0, Armonk, NY, USA) was used for conducting the statistical analyses. The level of significance was set at p < 0.05 for all statistical analyses.
3. Results
3.1. Demographic Characteristics of Patients
During the study period (from January until September 2017), 3080 patients presented to the urology departments of the multiple tertiary healthcare centers in South Lebanon involved in our study. Out of this population, 682 (22.1%) met our inclusion criteria.
Regarding gender and age distributions, females had the highest incidence rates with 85% of the total population, with adults between 19 and 64 years old being the predominant group (44.0%). The prevalence of bacterial UTI was lowest in adolescents between 12 and 18 years old (3.7%). The number of non-hospitalized patients outnumbered approximately twice those hospitalized for UTI (data not shown). Regarding the monthly distribution, the highest incidence of UTI was in January (15.4%), and the lowest was in June (6.2%).
3.2. Prevalence of Common Uropathogens
Out of 682 isolates from patients with UTI, E. coli was the predominant uropathogenic organism (67.1%) followed by K. pneumoniae (10.0%) and P. mirabilis (3.7%). The other less common uropathogens constituted 19.2% of the cases and were not included in the analysis within our study. The prevalence of ESBL was 32.9%, and E. coli was the major ESBL-producing organism (35.2%) followed by K. pneumoniae (27.7%) (Table 1).

Table 1.
Prevalence of ESBL among the three common uropathogens.
3.3. Correlation between Different Uropathogens and Demographic Parameters
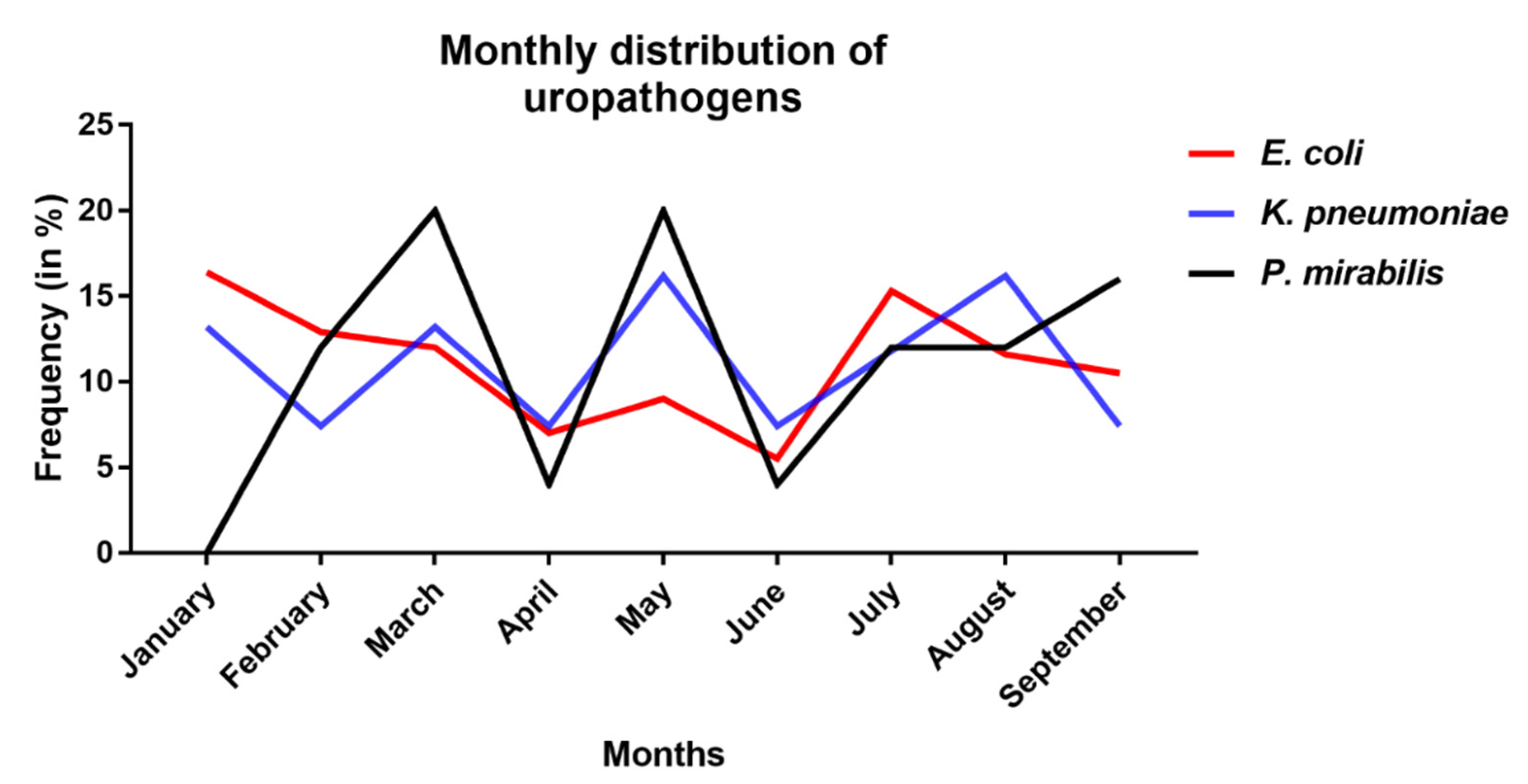
Table 2 shows no significant association between the distribution of different uropathogenic bacteria and the demographic factors (different age groups, gender, and type of hospital admission). Monthly distribution of uropathogens reveals no difference between the three uropathogens as regarding their frequency of occurrence in specific months (Figure 1). With respect to the age groups, E. coli and K. pneumoniae primarily occur in adults and elderly whereas P. mirabilis is mainly found in children. Females are always more prone to contract UTIs regardless of the uropathogen than males as expected.

Table 2.
Distribution of the three studied uropathogens according to patients’ demographic factors. Chi-squared test was used to evaluate any significant difference between the categorical variables of patients’ demographic factors between the three studied groups (E. coli, K. pneumonia, and P. mirabilis). The level of statistical significance was set at p < 0.05.
Figure 1.
Monthly distribution of different uropathogens from January to September 2017 in UTI patients. E. coli (in red), K. pneumoniae (in blue), and P. mirabilis (in black).
3.4. Distribution of ESBL-Producing Organisms among In- and Out-Patients
As expected, ESBL-producing organisms almost equally occur in in-patients (51.1%) and out-patients (48.9%) indicating that ESBL is both a hospital- and community-acquired infection, while non-ESBL is more common among out-patients (65.4%) than in-patients (34.6%) with a statistically significant different difference between the two groups (p < 0.001) (Table 3).

Table 3.
Non-ESBL vs. ESBL producing organisms among in- and out-patients. A chi-squared test was used to evaluate any significant difference between ESBL and non-ESBL groups for the hospital admission. The level of statistical significance was set at p < 0.05.
3.5. Laboratory Analysis Profile of the Three Different Studied Uropathogens
When comparing blood and urine laboratory analysis related to each of the three studied uropathogens in Table 4, data showed highest median urine pH levels (6.5; Q1–Q3: 5.5–7.5) in patients with UTI caused by P. mirabilis (p = 0.480) and highest median white blood cells (WBCs) levels in those with UTI caused by E. coli (10.81; Q1–Q3: 8.25–16.27; p = 0.020). Results are consistent with what has been previously published where urine with E. coli or K. pneumoniae demonstrated the most acidic pH while P. mirabilis exhibited the least acidic pH [26,27,28]. The pathophysiological mechanism behind this is that P. mirabilis produces urease which hydrolyzes urea in urine into CO2 and ammonia, both of which cause urine pH to increase [27,29]. As for the lower WBC count in the K. pneumoniae group, an explanation could be that WBCs have been shown in a study on rats to be reduced in the first few days post-infection and only increase after seven days of infection [30]. In addition, since urease-producing uropathogens such as P. mirabilis often convert normally acidic urine into an alkaline state which can lyse WBCs, the WBC count is reduced during an infection [31,32].

Table 4.
Laboratory data related to each of the three studied uropathogens. Jonckheere–Terpstra test was used to compare the medians of the laboratory data of patients among the three uropathogen groups (E. coli, K. pneumoniae, and P. mirabilis). The level of statistical significance was set at p < 0.05.
3.6. Comparison of Laboratory Analysis Profiles between ESBL and Non-ESBL Producing Organisms
Laboratory data revealed that median WBC, C-reactive protein (CRP), blood urea nitrogen (BUN), and creatinine levels were higher in patients with UTI caused by ESBL-producing organism as compared to patients with UTI caused by non-ESBL producing organism (p = 0.015, p = 0.288, p = 0.269, and p = 0.063, respectively) (Table 5).

Table 5.
Laboratory data related to non-ESBL vs. ESBL uropathogens. Mann–Whitney test were used to assess differences between ESBL and non-ESBL groups for laboratory data. The level of statistical significance was set at p < 0.05.
3.7. Antibiotic Susceptibility Profiles of the Common Uropathogens
Based on CLSI guidelines, all E. coli, K. pneumoniae, and P. mirabilis were sensitive to carbapenems and 24.7%, 44.8%, and 80% were sensitive to cephalothin antibiotic, respectively. Cefoxitin and fosfomycin showed high levels of sensitivity ranging between 85% and 97%. Susceptibility to aminoglycosides (including gentamicin and amikacin), piperacillin/tazobactam, ceftazidime, and cefepime ranged from 72% to 92% for E. coli, K. pneumoniae and P. mirabilis (Table 6).

Table 6.
Antibiotic susceptibility profiles of the three studied uropathogens.
3.8. Prevalence of MDR Strains among UTI Isolates
Upon studying the antibiotic resistance profiles of the three common uropathogens, we found that out of the 458 E. coli isolates, two were resistant to 15 different antibiotics, 115 (25.1%) were resistant to more than eight antibiotics, while 107 (23.4%) isolates were susceptible to all current antibiotics studied. On the other hand, only one K. pneumoniae isolate was resistant to 16 different antibiotics, 19 (27.9%) were resistant to more than eight antibiotics, and 21 (30.9%) were susceptible to all studied antibiotics. Remarkably, one isolate of P. mirabilis was resistant to 12 antibiotics (Data not shown).
4. Discussion
The emergence of MDR organisms has been recently acknowledged as an important global concern, and infections caused by ESBL-producing MDR organisms are specifically being perceived as major threats to both physicians and patients [33]. Our study focused on assessing the epidemiology of UTI among Lebanese patients attending tertiary healthcare centers in South Lebanon over a period of 9 months and evaluating the profiles of antimicrobial susceptibility to three common uropathogens, namely E. coli, K. pneumoniae, and P. mirabilis.
Our results showed that the highest incidence of UTI was during the Fall season, mostly in January, suggesting that weather conditions may be implicated in increasing the risk of UTIs and affecting the outcome of patients as well. A study by Elo et al. showed comparable results to ours [34]. In terms of demography, females had higher prevalence of UTIs owing to the anatomical and physical factors, particularly their short urethras and the small distance between the urinary system from one side and the genital/intestinal system from the other side [10]. In our study, the number of out-patients outnumbered those hospitalized for UTI, as the vast majority of cases represented uncomplicated cystitis that do not necessitate hospitalization, a fact that was reinforced by Schmiemann et al. [35].
In this study, E. coli was the most commonly detected isolate (67.1%) followed by K. pneumoniae, and P. mirabilis, representing the three mostly reported uropathogens as shown in other publications [36,37]. Our study results are consistent with results from a previous study done in Lebanon revealing that E. coli has the highest incidence (60.53–73.98%) followed by K. pneumoniae (5.32–8.33%) [37] and another study demonstrating most frequent UTI isolates as E. coli (70%), K. pneumoniae (14%), and Pseudomonas (5%) [38]. Similar results were also obtained in antimicrobial resistance epidemiological survey on cystitis (ARESC) study where E. coli was the most common isolate with a prevalence of 76.7% followed by Enterococcus faecalis, Staphylococcus saprophyticus, K. pneumoniae, and P. mirabilis [39]. In addition, the average ESBL production was found to be 32.9% during our study period and again E. coli was the major ESBL-producing organism (35.2%) followed by K. pneumoniae (27.7%). These data were consistent with a study conducted by Chamoun et al., revealing ESBL production rates in E. coli and Klebsiella spp. of 32.3% and 29.2%, respectively [16].
Our results showed that the rate of ESBL-producing organisms was significantly higher among in-patients compared to out-patients (p < 0.001). This pattern could be explained by the extensive misuse, overuse, and abuse of different antibiotics by healthcare workers or patients themselves who tend to take antibiotics without medical consultation and prescriptions [40].
Laboratory data showed that urine pH levels were highest in patients with UTI caused by P. mirabilis, an expected outcome as this organism produces urease and the direct result of urease activity is an increase in local pH level [41]. In addition, the WBC counts were higher in patients with UTI caused by E. coli. The results shown in this study were similar to the results obtained by Peltola et al., where the total WBC counts were increased in E. coli infections [42]. When it comes to the association between the laboratory results and the antimicrobial resistance among clinical bacterial isolates, conflicting reports were noted. Our study showed a clear correlation between WBC, BUN, creatinine levels and ESBL-producing organisms. However, Park et al. showed no significant association [43], which indicates the need for further studies to clarify this point and to potentially set guidelines for future management.
As for antimicrobial susceptibility, the three common uropathogens studied herein were found to be most susceptible to imipenem (100%) and meropenem (100%). This is consistent with a study conducted by Daoud et al. in which imipenem remained the only antibiotic with 100% of susceptibility [10]. It is well appreciated that rates of uropathogens with high resistance towards antibiotics have increased in recent years [44]. Indeed, in our study, some uropathogens were found to be resistant to various antibiotics. Therefore, continuous surveillance and monitoring of MDR organisms is highly needed and recommended to reduce their prevalence and prevent treatment failure.
We acknowledge that our study had several limitations, one of which is related to its short duration and missing data pertaining to some of the collected information. However, there is a scarcity of data regarding the epidemiology of UTI and the profiles of antibiotic susceptibility in South Lebanon, which constituted the main strength of this study.
5. Conclusions
As a conclusion, this study revealed the predominance of E. coli among other uropathogens among Lebanese patients with UTIs. It also underlined the threat of ESBL-producing bacteria which constituted around a third of the studied population. These results highlighted the importance of an adequate antimicrobial prescription for UTIs—clearance of the infection, avoiding recurrence, and being aware of multidrug resistance should all be priorities by physicians when treating patients with UTIs. This study offers a “terrain” to set new guidelines in the management of UTI; further studies are still needed in order to stratify these infections based on severity and to adjust the management accordingly.
Author Contributions
Conceptualization, G.G.; Methodology, E.S.S., A.S., and L.S.; Software, A.S.; Validation, H.F.B., E.S.S., and G.G.; Formal Analysis, A.S.; Investigation, L.S. and A.E.R.; Resources, A.S. and G.G.; Data Curation, L.S.; Writing—Original Draft Preparation, E.S.S., A.S., H.F.B., and G.G.; Writing—Review & Editing, A.E.R. and L.S.; Visualization, G.G.; Supervision, G.G. and H.F.B.; Project Administration, G.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
First: we would like to thank all patients enrolled in this study who granted us written informed consents to participate. Secondly, we would like to express our gratitude thanks to the healthcare centers involved, the Lebanese University, and Beirut Arab University for their support in the conduction of this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alanazi, M.Q.; Alqahtani, F.Y.; Aleanizy, F.S. An evaluation of E. coli in urinary tract infection in emergency department at KAMC in Riyadh, Saudi Arabia: Retrospective study. Ann. Clin. Microbiol. Antimicrob. 2018, 17, 3. [Google Scholar] [CrossRef]
- Hyun, M.; Lee, J.Y.; Kim, H.A.; Ryu, S.Y. Comparison of Escherichia coli and Klebsiella pneumoniae Acute Pyelonephritis in Korean Patients. Infect. Chemother. 2019, 51, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Al-Badr, A.; Al-Shaikh, G. Recurrent Urinary Tract Infections Management in Women: A review. Sultan Qaboos Univ. Med. J. 2013, 13, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Foxman, B. The epidemiology of urinary tract infection. Nat. Rev. Urol. 2010, 7, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Rubin, R.H.; Shapiro, E.D.; Andriole, V.T.; Davis, R.J.; Stamm, W.E. Evaluation of new anti-infective drugs for the treatment of urinary tract infection. Infectious Diseases Society of America and the Food and Drug Administration. Clin. Infect. Dis. An Off. Publ. Infect. Dis. Soc. Am. 1992, 15 (Suppl. 1), S216–S227. [Google Scholar] [CrossRef]
- Cortes-Penfield, N.W.; Trautner, B.W.; Jump, R.L.P. Urinary Tract Infection and Asymptomatic Bacteriuria in Older Adults. Infect. Dis. Clin. N. Am. 2017, 31, 673–688. [Google Scholar] [CrossRef]
- Stamm, W.E. Scientific and clinical challenges in the management of urinary tract infections. Am. J. Med. 2002, 113 (Suppl. 1A), 1s–4s. [Google Scholar] [CrossRef]
- Rizwan, M.; Akhtar, M.; Najmi, A.K.; Singh, K. Escherichia coli and Klebsiella pneumoniae Sensitivity/Resistance Pattern Towards Antimicrobial Agents in Primary and Simple Urinary Tract Infection Patients Visiting University Hospital of Jamia Hamdard New Delhi. Drug Res. 2018, 68, 415–420. [Google Scholar] [CrossRef]
- Zanichelli, V.; Huttner, A.; Harbarth, S.; Kronenberg, A.; Huttner, B.; Swiss Centre For Antibiotic Resistance Anresis. Antimicrobial resistance trends in Escherichia coli, Klebsiella pneumoniae and Proteus mirabilis urinary isolates from Switzerland: Retrospective analysis of data from a national surveillance network over an 8-year period (2009–2016). Swiss Med. Wkly. 2019, 149, w20110. [Google Scholar] [CrossRef]
- Daoud, Z.; Afif, C. Escherichia coli Isolated from Urinary Tract Infections of Lebanese Patients between 2000 and 2009: Epidemiology and Profiles of Resistance. Chemother. Res. Pract. 2011, 2011, 218431. [Google Scholar] [CrossRef]
- Ho, H.J.; Tan, M.X.; Chen, M.I.; Tan, T.Y.; Koo, S.H.; Koong, A.Y.L.; Ng, L.P.; Hu, P.L.; Tan, K.T.; Moey, P.K.S.; et al. Interaction between Antibiotic Resistance, Resistance Genes, and Treatment Response for Urinary Tract Infections in Primary Care. J. Clin. Microbiol. 2019, 57. [Google Scholar] [CrossRef] [PubMed]
- Cullen, I.M.; Manecksha, R.P.; McCullagh, E.; Ahmad, S.; O’Kelly, F.; Flynn, R.; McDermott, T.E.; Murphy, P.; Grainger, R.; Fennell, J.P.; et al. An 11-year analysis of the prevalent uropathogens and the changing pattern of Escherichia coli antibiotic resistance in 38,530 community urinary tract infections, Dublin 1999–2009. Ir. J. Med. Sci. 2013, 182, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, N.; Agus, N.; Bayram, A.; Samlioglu, P.; Sirin, M.C.; Derici, Y.K.; Hanci, S.Y. Antimicrobial susceptibilities of Escherichia coli isolates as agents of community-acquired urinary tract infection (2008–2014). Turk. J. Urol. 2016, 42, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Salem, S.E.; Dahdouh, E.; Daoud, Z. Resistance of Gram-Negative Bacilli in Lebanon. ISRN Infect. Dis. 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Yazdansetad, S.; Alkhudhairy, M.K.; Najafpour, R.; Farajtabrizi, E.; Al-Mosawi, R.M.; Saki, M.; Jafarzadeh, E.; Izadpour, F.; Ameri, A. Preliminary survey of extended-spectrum b-lactamases (ESBLs) in nosocomial uropathogen Klebsiella pneumoniae in north-central Iran. Heliyon 2019, 5, e02349. [Google Scholar] [CrossRef]
- Chamoun, K.; Farah, M.; Araj, G.; Daoud, Z.; Moghnieh, R.; Salameh, P.; Saade, D.; Mokhbat, J.; Abboud, E.; Hamze, M.; et al. Surveillance of antimicrobial resistance in Lebanese hospitals: Retrospective nationwide compiled data. Int. J. Infect. Dis. 2016, 46, 64–70. [Google Scholar] [CrossRef]
- McNulty, C.A.; Richards, J.; Livermore, D.M.; Little, P.; Charlett, A.; Freeman, E.; Harvey, I.; Thomas, M. Clinical relevance of laboratory-reported antibiotic resistance in acute uncomplicated urinary tract infection in primary care. J. Antimicrob. Chemother. 2006, 58, 1000–1008. [Google Scholar] [CrossRef]
- Vranic, S.M.; Uzunovic, A. Antimicrobial Resistance of Escherichia Coli Strains Isolated from Urine at Outpatient Population: A Single Laboratory Experience. Mater. Socio Med. 2016, 28, 121–124. [Google Scholar] [CrossRef]
- Navon-Venezia, S.; Kondratyeva, K.; Carattoli, A. Klebsiella pneumoniae: A major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol. Rev. 2017, 41, 252–275. [Google Scholar] [CrossRef]
- Wang, J.T.; Chen, P.C.; Chang, S.C.; Shiau, Y.R.; Wang, H.Y.; Lai, J.F.; Huang, I.W.; Tan, M.C.; Lauderdale, T.L.; Hospitals, T. Antimicrobial susceptibilities of Proteus mirabilis: A longitudinal nationwide study from the Taiwan surveillance of antimicrobial resistance (TSAR) program. BMC Infect. Dis 2014, 14, 486. [Google Scholar] [CrossRef]
- Montso, K.P.; Dlamini, S.B.; Ateba, C.N.; Kumar, A.; Garcia-Perdomo, H.A. Antimicrobial Resistance Factors of Extended-Spectrum Beta-Lactamases Producing Escherichia coli and Klebsiella pneumoniae Isolated from Cattle Farms and Raw Beef in North-West Province, South Africa. BioMed. Res. Int. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Al-Tamimi, M.; Abu-Raideh, J.; Albalawi, H.; Shalabi, M.; Saleh, S. Effective Oral Combination Treatment for Extended-Spectrum Beta-Lactamase-Producing Escherichia coli. Microb. Drug Resist. 2019, 25, 1132–1141. [Google Scholar] [CrossRef] [PubMed]
- Grabe, M.; Bjerklund-Johansen, T.E.; Botto, H.; Çek, M.; Naber, K.G.; Tenke, P.; Wagenlehner, F. Guidelines on Urological Infections. Eur. Assoc. Urol. 2010, 1–112. [Google Scholar]
- Nesher, L.; Novack, V.; Riesenberg, K.; Schlaeffer, F. Regional community-acquired urinary tract infections in Israel: Diagnosis, pathogens, and antibiotic guidelines adherence: A prospective study. Int. J. Infect. Dis. 2007, 11, 245–250. [Google Scholar] [CrossRef]
- Clinical Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012; Volume 32, pp. 70–71. [Google Scholar]
- Lai, H.-C.; Chang, S.-N.; Lin, H.-C.; Hsu, Y.-L.; Wei, H.-M.; Kuo, C.-C.; Hwang, K.-P.; Chiang, H.-Y. Association between urine pH and common uropathogens in children with urinary tract infections. J. Microbiol. Immunol. Infect. 2019. [Google Scholar] [CrossRef]
- Mobley, H.L.; Hausinger, R.P. Microbial ureases: Significance, regulation, and molecular characterization. Microbiol. Rev. 1989, 53, 85–108. [Google Scholar] [CrossRef]
- Simerville, J.A.; Maxted, W.C.; Pahira, J.J. Urinalysis: A comprehensive review. Am. Fam. Physician 2005, 71, 1153–1162. [Google Scholar]
- Chen, C.Y.; Chen, Y.H.; Lu, P.L.; Lin, W.R.; Chen, T.C.; Lin, C.Y. Proteus mirabilis urinary tract infection and bacteremia: Risk factors, clinical presentation, and outcomes. J. Microbiol. Immunol. Infect. 2012, 45, 228–236. [Google Scholar] [CrossRef]
- Dong, F.; Wang, B.; Zhang, L.; Tang, H.; Li, J.; Wang, Y. Metabolic response to Klebsiella pneumoniae infection in an experimental rat model. PLoS ONE 2012, 7, e51060. [Google Scholar] [CrossRef]
- Tambyah, P.A.; Maki, D.G. The relationship between pyuria and infection in patients with indwelling urinary catheters: A prospective study of 761 patients. Arch. Intern. Med. 2000, 160, 673–677. [Google Scholar] [CrossRef]
- Jacobsen, S.M.; Stickler, D.J.; Mobley, H.L.T.; Shirtliff, M.E. Complicated Catheter-Associated Urinary Tract Infections Due to Escherichia coli and Proteus mirabilis. Clin. Microbiol. Rev. 2008, 21, 26–59. [Google Scholar] [CrossRef] [PubMed]
- Alqasim, A.; Abu Jaffal, A.; Alyousef, A.A. Prevalence of Multidrug Resistance and Extended-Spectrum beta-Lactamase Carriage of Clinical Uropathogenic Escherichia coli Isolates in Riyadh, Saudi Arabia. Int. J. Microbiol. 2018, 2018, 3026851. [Google Scholar] [CrossRef] [PubMed]
- Elo, J.; Sarna, S.; Tallgren, L.G. Seasonal variations in the occurrence of urinary tract infections among children in an urban area in Finland. Ann. Clin. Res. 1979, 11, 101–106. [Google Scholar] [PubMed]
- Schmiemann, G.; Kniehl, E.; Gebhardt, K.; Matejczyk, M.M.; Hummers-Pradier, E. The diagnosis of urinary tract infection: A systematic review. Dtsch. Arztebl. Int. 2010, 107, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Soubra, L.; Kabbani, S.; Anwar, M.F.; Dbouk, R. Spectrum and patterns of antimicrobial resistance of uropathogens isolated from a sample of hospitalised Lebanese patients with urinary tract infections. J. Glob. Antimicrob. Resist. 2014, 2, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Daoud, Z.; Salem Sokhn, E.; Masri, K.; Matar, G.M.; Doron, S. Escherichia coli Isolated from Urinary Tract Infections of Lebanese Patients between 2005 and 2012: Epidemiology and Profiles of Resistance. Front. Med. 2015, 2, 26. [Google Scholar] [CrossRef]
- Hayajneh, W.A.; Hajj, A.; Hulliel, F.; Sarkis, D.K.; Irani-Hakimeh, N.; Kazan, L.; Badal, R.E. Susceptibility trends and molecular characterization of Gram-negative bacilli associated with urinary tract and intra-abdominal infections in Jordan and Lebanon: SMART 2011–2013. Int. J. Infect. Dis. 2015, 35, 56–61. [Google Scholar] [CrossRef]
- Vranic, S.M.; Zatric, N.; Rebic, V.; Aljicevic, M.; Abdulzaimovic, A. The Most Frequent Isolates from Outpatients with Urinary Tract Infection. Mater. Socio Med. 2017, 29, 17–20. [Google Scholar] [CrossRef]
- Ouchar Mahamat, O.; Lounnas, M.; Hide, M.; Dumont, Y.; Tidjani, A.; Kamougam, K.; Abderrahmane, M.; Benavides, J.; Solassol, J.; Bañuls, A.L.; et al. High prevalence and characterization of extended-spectrum ß-lactamase producing Enterobacteriaceae in Chadian hospitals. BMC Infect. Dis. 2019, 19, 205. [Google Scholar] [CrossRef]
- Schaffer, J.N.; Pearson, M.M. Proteus mirabilis and Urinary Tract Infections. Microbiol. Spectr. 2015, 3. [Google Scholar] [CrossRef]
- Peltola, V.; Mertsola, J.; Ruuskanen, O. Comparison of total white blood cell count and serum C-reactive protein levels in confirmed bacterial and viral infections. J. Pediatrics 2006, 149, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, J.H. Clinical Significance of Extended-spectrum b-lactamase-producing Bacteria in First Pediatric Febrile Urinary Tract Infections and Differences between Age Groups. Child. Kidney Dis. 2017, 21, 128–135. [Google Scholar] [CrossRef]
- Ramirez-Castillo, F.Y.; Moreno-Flores, A.C.; Avelar-Gonzalez, F.J.; Marquez-Diaz, F.; Harel, J.; Guerrero-Barrera, A.L. An evaluation of multidrug-resistant Escherichia coli isolates in urinary tract infections from Aguascalientes, Mexico: Cross-sectional study. Ann. Clin. Microbiol. Antimicrob. 2018, 17, 34. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).