Sodium Chloride, Migraine and Salt Withdrawal: Controversy and Insights
Abstract
1. Introduction
2. Migraine, Salt Intake, and Fluid Retention
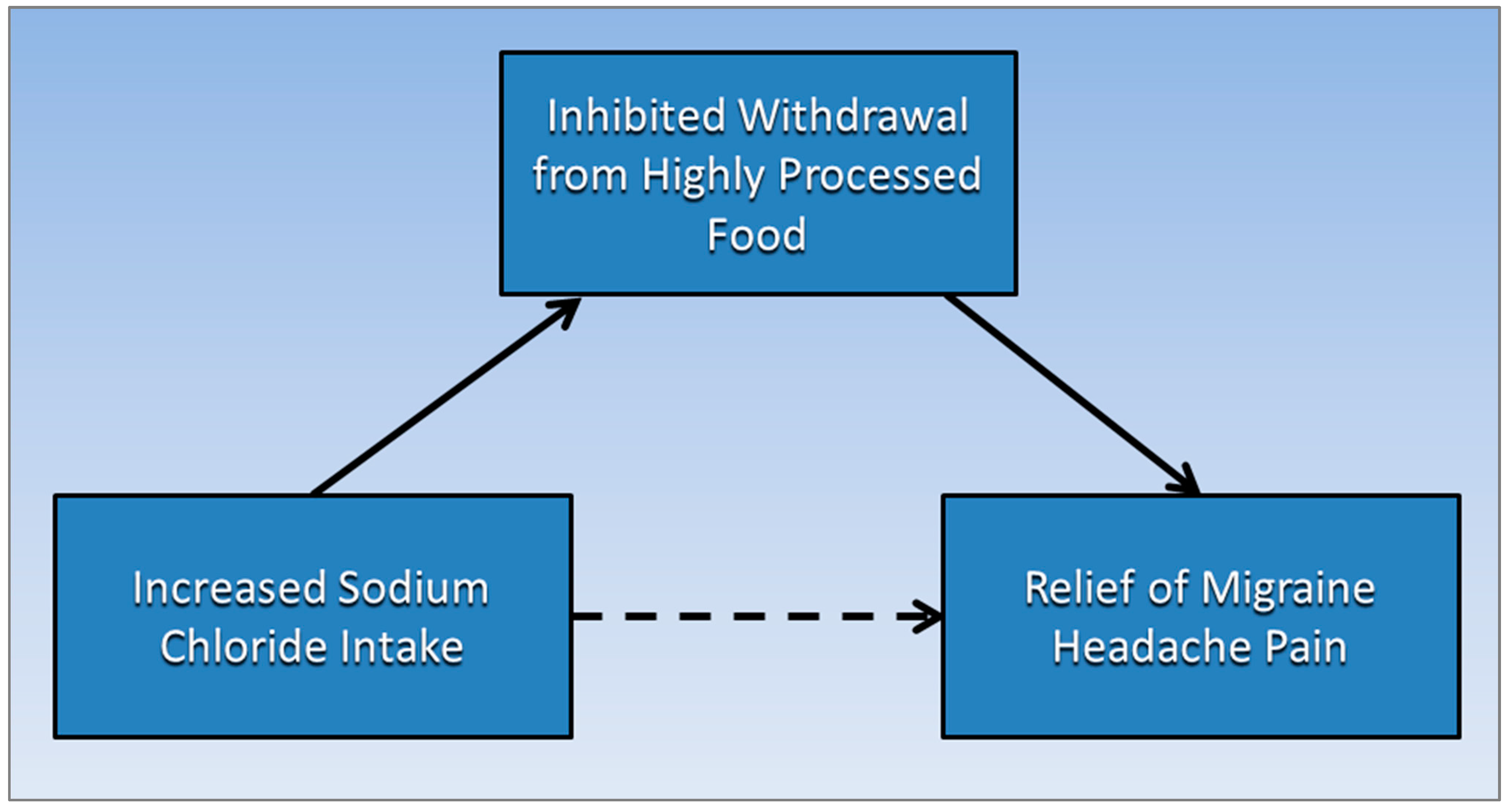
3. Sodium Chloride and Controversial Migraine Relief
4. Highly Processed Food Withdrawal
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tekol, Y. Salt addiction: A different kind of drug addiction. Med. Hypotheses 2006, 67, 1233–1234. [Google Scholar] [CrossRef]
- Hasin, D.S.; O’Brien, C.P.; Auriacombe, M.; Borges, G.; Bucholz, K.; Budney, A.; Compton, W.M.; Crowley, T.; Ling, W.; Petry, N.M.; et al. DSM-5 criteria for substance use disorders: Recommendations and rationale. Am. J. Psychiatry 2013, 170, 834–851. [Google Scholar] [CrossRef] [PubMed]
- IHS. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef] [PubMed]
- Wolfswinkel, J.F.; Furtmueller, E.; Wilderom, C.P.M. Using grounded theory as a method for rigorously reviewing literature. Eur. J. Inf. Syst. 2013, 22, 45–55. [Google Scholar] [CrossRef]
- Stovner, L.J.; Nichols, E.; Steiner, T.J.; Abd-Allah, F.; Abdelalim, A.; Al-Raddadi, R.M.; Ansha, M.G.; Barac, A.; Bensenor, I.M.; Doan, L.P. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 954–976. [Google Scholar] [CrossRef]
- Steiner, T.J.; Stovner, L.J.; Vos, T.; Jensen, R.; Katsarava, Z. Migraine is first cause of disability in under 50s: Will health politicians now take notice? J. Headache Pain 2018, 19, 17. [Google Scholar] [CrossRef]
- Buse, D.C.; Reed, M.L.; Fanning, K.M.; Bostic, R.; Dodick, D.W.; Schwedt, T.J.; Munjal, S.; Singh, P.; Lipton, R.B. Comorbid and co-occurring conditions in migraine and associated risk of increasing headache pain intensity and headache frequency: Results of the migraine in America symptoms and treatment (MAST) study. J. Headache Pain 2020, 21, 23. [Google Scholar] [CrossRef]
- Patel, Y.; Joseph, J. Sodium Intake and Heart Failure. Int. J. Mol. Sci. 2020, 21, 9474. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Holland, P.R.; Martins-Oliveira, M.; Hoffmann, J.; Schankin, C.; Akerman, S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol. Rev. 2017, 97, 553–622. [Google Scholar] [CrossRef]
- Karsan, N.; Goadsby, P.J. Biological insights from the premonitory symptoms of migraine. Nat. Rev. Neurol. 2018, 14, 699–710. [Google Scholar] [CrossRef]
- Ravisankar, P.; Hundia, A.; Sindhura, J.; Rani, B.S.; Sai, P. Migraine—A comprehensive review. Indo Am. J. Pharm. Res. 2015, 5, 3170–3190. [Google Scholar]
- Wilson, C.W.; Kirker, J.G.; Warnes, H.; O’Malley, M. The clinical features of migraine as a manifestation of allergic disease. Postgrad. Med J. 1980, 56, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Dalkara, T.; Kılıç, K. How Does Fasting Trigger Migraine? A Hypothesis. Curr. Pain Headache Rep. 2013, 17, 368. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.A.; Hay, K.; Tonks, E.M. An investigation of the salt and water balance in migraine. Br. Med. J. 1951, 2, 1424. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Harding, M. Idiopathic Oedema. Available online: https://patient.info/signs-symptoms/oedema-swelling/idiopathic-oedema (accessed on 30 July 2021).
- Demirci, K.; Demirci, S.; Akpinar, A.; Demirdaş, A.; Atay, İ.M. Evaluation of Eating Attitude in Patients with Migraine. Nöro Psikiyatri Arşivi 2015, 52, 367–370. [Google Scholar] [CrossRef]
- D’Andrea, G.; Ostuzzi, R.; Bolner, A.; Colavito, D.; Leon, A. Is migraine a risk factor for the occurrence of eating disorders? Prevalence and biochemical evidences. Neurol. Sci. 2012, 33 (Suppl. 1), S71–S76. [Google Scholar] [CrossRef]
- Mustelin, L.; Raevuori, A.; Kaprio, J.; Keski-Rahkonen, A. Association between eating disorders and migraine may be explained by major depression. Int. J. Eat Disord. 2014, 47, 884–887. [Google Scholar] [CrossRef]
- Kristoffersen, E.S.; Børte, S.; Hagen, K.; Zwart, J.-A.; Winsvold, B.S. Migraine, obesity and body fat distribution—A population-based study. J. Headache Pain 2020, 21, 97. [Google Scholar] [CrossRef]
- Robbins, L. Migraine Treatment: What’s Old, What’s New. Available online: https://www.practicalpainmanagement.com/pain/headache/migraine/migraine-treatment-what-old-what-new (accessed on 30 July 2021).
- Hay, K. The Influence of Thyroid on Water Metabolism in Migraine. J. Coll. Gen. Pract. 1962, 5, 86. [Google Scholar] [PubMed]
- Ghaffari, H.; Grant, S.C.; Petzold, L.R.; Harrington, M.G. Regulation of CSF and brain tissue sodium levels by the blood-CSF and blood-brain barriers during migraine. Front. Comput. Neurosci. 2020, 14, 4. [Google Scholar] [CrossRef]
- Amer, M.; Woodward, M.; Appel, L.J. Effects of dietary sodium and the DASH diet on the occurrence of headaches: Results from randomised multicentre DASH-Sodium clinical trial. BMJ Open 2014, 4, e006671. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhang, Z.; Chen, W.; Whelton, P.K.; Appel, L.J. Lower Sodium Intake and Risk of Headaches: Results From the Trial of Nonpharmacologic Interventions in the Elderly. Am. J. Public Health 2016, 106, 1270–1275. [Google Scholar] [CrossRef]
- Mirzababaei, A.; Khorsha, F.; Togha, M.; Yekaninejad, M.S.; Okhovat, A.A.; Mirzaei, K. Associations between adherence to dietary approaches to stop hypertension (DASH) diet and migraine headache severity and duration among women. Nutr. Neurosci. 2020, 23, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Cianchetti, C.; Hmaidan, Y.; Finco, G.; Ledda, M.G. Scalp periarterial saline efficacy in migraine and relation to exploding and imploding headache. J. Neurol. 2009, 256, 1109–1113. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.C. Treatment of Pain. Available online: https://www.merckmanuals.com/en-ca/home/brain,-spinal-cord,-and-nerve-disorders/pain/treatment-of-pain (accessed on 30 July 2021).
- Kim, S.; Joo, K.W. Electrolyte and acid-base disturbances associated with non-steroidal anti-inflammatory drugs. Electrolytes Blood Press. E BP 2007, 5, 116. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.T.; Ornello, R.; Quatrosi, G.; Torrente, A.; Albanese, M.; Vigneri, S.; Guglielmetti, M.; Maria De Marco, C.; Dutordoir, C.; Colangeli, E.; et al. Medication overuse and drug addiction: A narrative review from addiction perspective. J. Headache Pain 2021, 22, 32. [Google Scholar] [CrossRef] [PubMed]
- Pogoda, J.M.; Gross, N.B.; Arakaki, X.; Fonteh, A.N.; Cowan, R.P.; Harrington, M.G. Severe headache or migraine history is inversely correlated with dietary sodium intake: NHANES 1999–2004. Headache J. Head Face Pain 2016, 56, 688–698. [Google Scholar] [CrossRef]
- Stanton, A.A. Migraine Cause and Treatment. Ment. Health Fam. Med. 2015, 11, 69–72. [Google Scholar] [CrossRef]
- Salt and Sodium. Available online: https://www.hsph.harvard.edu/nutritionsource/salt-and-sodium/ (accessed on 4 June 2020).
- Get the Facts: Sodium’s Role in Processed Food. Available online: https://www.cdc.gov/salt/pdfs/sodium_role_processed.pdf (accessed on 30 July 2021).
- Onaolapo, A.Y.; Onaolapo, O.J. Food additives, food and the concept of ‘food addiction’: Is stimulation of the brain reward circuit by food sufficient to trigger addiction? Pathophysiology 2018, 25, 263–276. [Google Scholar] [CrossRef]
- Schulte, E.M.; Smeal, J.K.; Lewis, J.; Gearhardt, A.N. Development of the Highly Processed Food Withdrawal Scale. Appetite 2018, 131, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Youssef, P.E.; Mack, K.J. Episodic and chronic migraine in children. Dev Med Child Neurol 2020, 62, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Parnarouskis, L.; Schulte, E.M.; Lumeng, J.C.; Gearhardt, A.N. Development of the Highly Processed Food Withdrawal Scale for Children. Appetite 2020, 147, 104553. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, R.B. Sodium Chloride, Migraine and Salt Withdrawal: Controversy and Insights. Med. Sci. 2021, 9, 67. https://doi.org/10.3390/medsci9040067
Brown RB. Sodium Chloride, Migraine and Salt Withdrawal: Controversy and Insights. Medical Sciences. 2021; 9(4):67. https://doi.org/10.3390/medsci9040067
Chicago/Turabian StyleBrown, Ronald B. 2021. "Sodium Chloride, Migraine and Salt Withdrawal: Controversy and Insights" Medical Sciences 9, no. 4: 67. https://doi.org/10.3390/medsci9040067
APA StyleBrown, R. B. (2021). Sodium Chloride, Migraine and Salt Withdrawal: Controversy and Insights. Medical Sciences, 9(4), 67. https://doi.org/10.3390/medsci9040067





