The Impact of the COVID-19 Lockdown on European Students’ Negative Emotional Symptoms: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
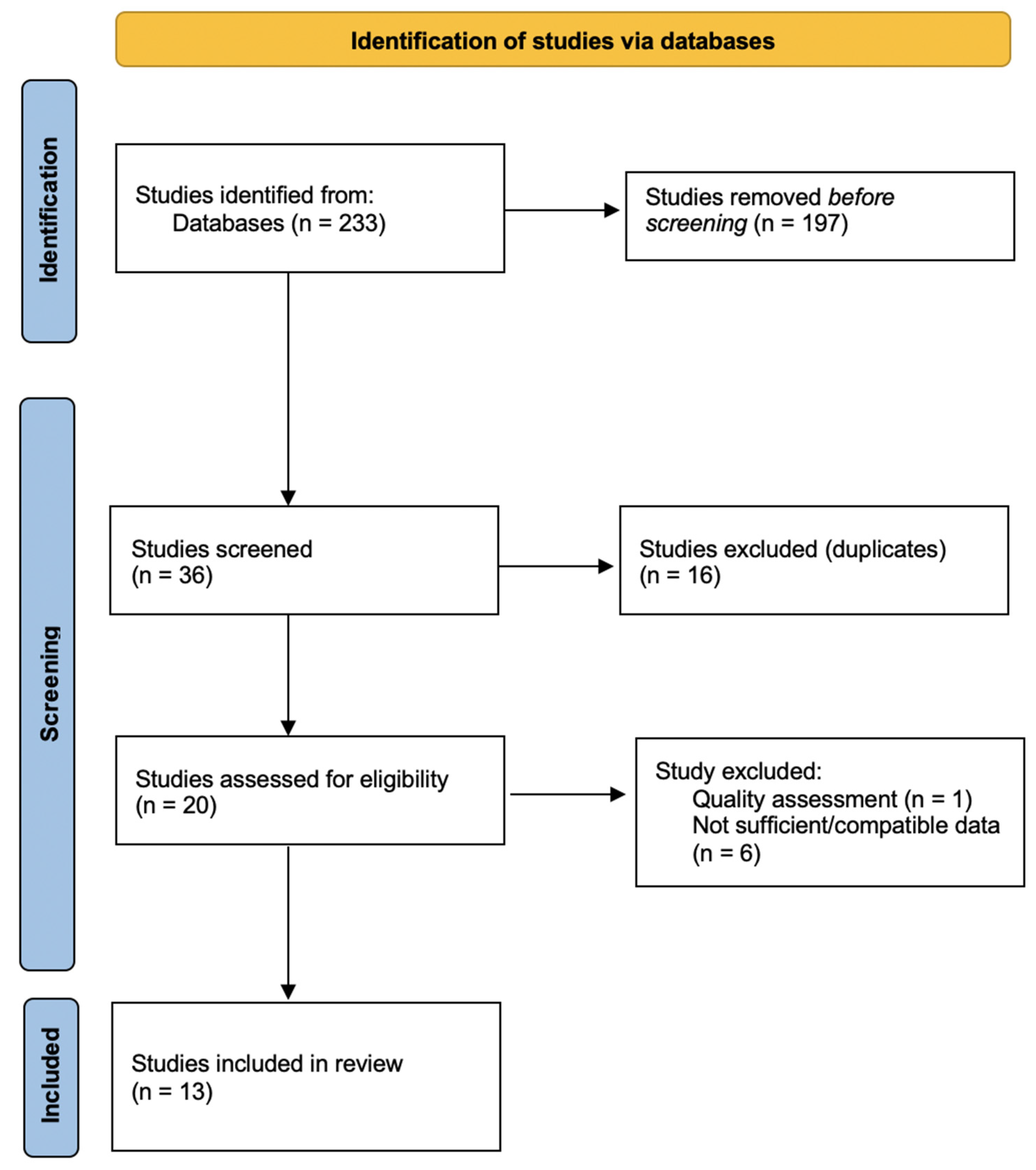
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Statistical Analysis
3. Results
3.1. Anxiety
3.2. Depression
3.3. Stress
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Timeline of WHO’s Response to COVID-19. Available online: https://www.who.int/news-room/detail/29-06-2020-COVIDtimeline (accessed on 1 May 2021).
- Ozamiz-Etxebarria, N.; Dosil-Santamaria, M.; Picaza-Gorrochategui, M.; Idoiaga-Mondragon, N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saude Publica 2020, 36, e00054020. [Google Scholar] [CrossRef]
- Padrón, I.; Fraga, I.; Vieitez, L.; Montes, C.; Romero, E. A Study on the psychological wound of COVID-19 in university students. Front. Psychol. 2021, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Gross, J.J. Handbook of Emotion Regulation, 2nd ed.; Guilford: New York, NY, USA, 2014. [Google Scholar]
- Westerhof, G.J.; Keyes, C.L.M. Mental illness and mental health: The two continua model across the lifespan. J. Adult Dev. 2010, 17, 110–119. [Google Scholar] [CrossRef] [Green Version]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS control and psychological effects of quarantine, Toronto Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Beiter, R.; Nash, R.; McCrady, M.; Rhoades, D.; Linscomb, M.; Clarahan, M.; Sammut, S. The prevalence and correlates of depression, anxiety and stress in a sample of college students. J. Affect. Disord. 2015, 173, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, R.P.; Alonso, J.; Axinn, W.G.; Cuijpers, P.; Ebert, D.D.; Green, J.G.; Hwand, I.; Kessler, R.C.; Liu, H.; Mortier, P.; et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol. Med. 2016, 46, 2955–2970. [Google Scholar] [CrossRef] [Green Version]
- Wieczorek, T.; Kołodziejczyk, A.; Ciułkowicz, M.; Maciaszek, J.; Misiak, B.; Rymaszewska, J.; Szcześniak, D. Class of 2020 in Poland: Students’ mental health during the COVID-19 outbreak in an academic setting. Int. J. Environ. Res. Public Health 2021, 18, 2884. [Google Scholar] [CrossRef] [PubMed]
- Lyons, Z.; Wilcox, H.; Leung, L.; Dearsley, O. COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australas. Psychiatry 2020, 28, 649–652. [Google Scholar] [CrossRef]
- Bueno-Notivol, J.; Gracia-García, P.; Olaya, B.; Lasheras, I.; López-Antón, R.; Santabárbara, J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021, 21, 100196. [Google Scholar] [CrossRef] [PubMed]
- Savage, M.J.; James, R.; Magistro, D.; Donaldson, J.; Healy, L.C.; Nevill, M.; Hennis, P.J. Mental health and movement behaviour during the COVID-19 pandemic in UK university students: Prospective cohort study. Ment. Health Phys. Act. 2020, 19, 100357. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Barendregt, J.; Doi, S.; Lee, Y.Y.; Pacella, R.; Vos, T. Meta-analysis of prevalence. J. Epidemiol. Community Health 2013, 67, 974–978. [Google Scholar] [CrossRef]
- Freeman, M.F.; Tukey, J.W. Transformations related to the angular and the square root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- Gavaghan, D.J.; Moore, A.R.; McQuay, H.J. An evaluation of homogeneity tests in meta-analyses in pain using simulations of individual patient data. Pain 2000, 85, 415–424. [Google Scholar] [CrossRef]
- Higgins, J.P.T. Measuring inconsistency in mate-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef]
- Arënliu, A.; Bërxulli, D.; Perolli-Shehu, B.; Krasniqi, B.; Gola, A.; Hyseni, F. Anxiety and depression among Kosovar university students during the initial phase of outbreak and lockdown of COVID-19 pandemic. Health Psychol. Behav. Med. 2021, 9, 239–250. [Google Scholar] [CrossRef]
- Arsandaux, J.; Montagni, I.; Macalli, M.; Texier, N.; Pouriel, M.; Germain, R.; Mebarki, A.; Kinouani, S.; Tournier, M.; Schuck, S.; et al. Mental health condition of college students compared to non-students during COVID-19 lockdown: The CONFINS study. BMJ Open 2021, 11, e053231. [Google Scholar] [CrossRef]
- Aslan, I.; Ochnik, D.; Çınar, O. Exploring perceived stress among students in Turkey during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8961. [Google Scholar] [CrossRef]
- Essadek, A.; Rabeyron, T. Mental health of French students during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 392–393. [Google Scholar] [CrossRef]
- Giannopoulou, I.; Efstathiou, V.; Triantafyllou, G.; Korkoliakou, P.; Douzenis, A. Adding stress to the stressed: Senior high school students’ mental health amidst the COVID-19 nationwide lockdown in Greece. Psychiatry Res. 2021, 295, 113560. [Google Scholar] [CrossRef]
- Giusti, L.; Salza, A.; Mammarella, S.; Bianco, D.; Ussorio, D.; Casacchia, M.; Roncone, R. Everything will be fine. Duration of home confinement and “All-or-Nothing” cognitive thinking style as predictors of traumatic distress in young university students on a digital platform during the COVID-19 Italian lockdown. Front. Psychiatry 2020, 11, 574812. [Google Scholar] [CrossRef] [PubMed]
- Konstantopoulou, G.; Raikou, N. Clinical evaluation of depression in university students during quarantine due to COVID-19 pandemic. Eur. J. Public Health 2020, 3, 1. [Google Scholar] [CrossRef]
- Lischer, S.; Safi, N.; Dickson, C. Remote learning and students’ mental health during the COVID-19 pandemic: A mixed-method enquiry. Prospects 2021, 5, 1. [Google Scholar] [CrossRef]
- Odriozola-González, P.; Planchuelo-Gómez, Á.; Irurtia, M.J.; de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef] [PubMed]
- Patelarou, A.; Mechili, E.A.; Galanis, P.; Zografakis-Sfakianakis, M.; Konstantinidis, T.; Saliaj, A.; Bucaj, J.; Alushi, E.; Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; et al. Nursing students, mental health status during COVID-19 quarantine: Evidence from three European countries. J. Ment. Health 2021, 30, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Schlichtinger, J.; Brunner, S.; Steffen, J.; Huber, B.C. Mental health impairment triggered by the COVID-19 pandemic in a sample population of German students. J. Investig. Med. 2020, 68, 1394–1396. [Google Scholar] [CrossRef] [PubMed]
- Werner, A.M.; Tibubos, A.N.; Mülder, L.M.; Reichel, J.L.; Schäfer, M.; Heller, S.; Pfirrmann, D.; Edelmann, D.; Dietz, P.; Rigotti, T.; et al. The impact of lockdown stress and loneliness during the COVID-19 pandemic on mental health among university students in Germany. Sci. Rep. 2021, 11, 22637. [Google Scholar] [CrossRef]
- Campion, J.; Javed, A.; Sartorius, N.; Marmot, M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry 2020, 7, 657–659. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Koretz, D.; Merikangas, K.R.; Rush, A.J.; Walters, E.E.; Wang, P.S. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003, 289, 3095–3105. [Google Scholar] [CrossRef] [PubMed]
- Johansson, R.; Carlbring, P.; Heedman, Å.; Paxling, B.; Andersson, G. Depression, anxiety and their comorbidity in the Swedish general population: Point prevalence and the effect on health-related quality of life. PeerJ 2013, 1, e98. [Google Scholar] [CrossRef] [PubMed]
- ESEMeD/MHEDEA 2000 Investigators; Alonso, J.; Angermeyer, M.C.; Bernert, S.; Bruffaerts, R.; Brugha, T.S.; Bryson, H.; de Girolamo, G.; de Graaf, R.; Demyttenaere, K.; et al. Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. 2004, 109, 21–27. [Google Scholar]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, E181. [Google Scholar] [CrossRef]
- Liu, C.H.; Zhang, E.; Wong, G.T.; Hyun, S. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Son, C.; Hedge, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on college students mental health in the United States: Interview survey study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef]
- Knight, H.; Carlisle, S.; O’Connor, M.; Briggs, L.; Fothergill, L.; Al-Oraibi, A.; Yilidrim, M.; Morling, J.R.; Corner, J.; Ball, J.; et al. Impacts of the COVID-19 pandemic and self-isolation on students and staff in higher education: A qualitative study. Int. J. Environ. Res. Public Health 2021, 18, 10675. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Huang, X.; Zhang, S.; Yang, J.; Yang, L.; Xu, M. Comparison of prevalence and associated factors of anxiety and depression among people affected versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med. Sci. Monit. 2020, 26, e924609-1. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Jeong, H.J.; Kim, S. Stress, anxiety, and depression among undergraduate students during the COVID-19 pandemic and their use of mental health services. Innov. High. Educ. 2021, 23, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Douglas, P.K.; Douglas, D.B.; Harrigan, D.C.; Douglas, K.M. Preparing for pandemic influenza and its aftermath: Mental health issues considered. Int. J. Emerg. Ment. Health 2009, 11, 137. [Google Scholar] [PubMed]
- Estes, K.D.; Thompson, R.R. Preparing for the aftermath of COVID-19: Shifting risk and downstream health consequences. Psychol. Trauma 2020, 12, S31. [Google Scholar] [CrossRef]





| Author | Country | Sample Size (n) | Assessment Tools | Percentage of Anxiety | Percentage of Depression | Percentage of Stress |
|---|---|---|---|---|---|---|
| Arënliu et al. [22] | Kosovo | 904 | HADS | 37.30% | 28.30% | / |
| Arsandaux et al. [23] | France | 1335 | GAD-7/PHQ-9 | 52.50% | 36.80% | 55.10% |
| Aslan et al. [24] | Turkey | 358 | GAD-7/PHQ-8/PSS-10 | 87.43% | 90.50% | 94.41% |
| Essadek & Rabeyron [25] | France | 8004 | GAD-7/PHQ-9 | 47.30% | 46% | / |
| Giannopoulou et al. [26] | Greece | 452/435 | GAD-7/PHQ-9 | 67.60% | 91% | / |
| Giusti et al. [27] | Italy | 103 | SAS/BDI | 35.90% | 26.20% | / |
| Konstantopoulou & Raikou [28] | Greece | 570 | BDI | / | 80.20% | / |
| Lischer et al. [29] | Switzerland | 458 | PHQ-4 | 85.60% | / | / |
| Odriozola-Gonzalez et al. [30] | Spain | 1944 | DASS-21 | 41.40% | 54.70% | 46.60% |
| Padrón et al. [3] | Spain | 932 | GAD-7/PHQ-9 | 61.20% | 65.80% | / |
| Patelarou et al. [31] | Albania | 197 | PHQ-9 | / | 58.90% | / |
| Greece | 348 | PHQ-9 | / | 59.50% | / | |
| Spain | 242 | PHQ-9 | / | 86% | / | |
| Schlichtinger et al. [32] | Germany | 1943 | Self-reported questionnaire | / | / | 39.60% |
| Werner et al. [33] | Germany | 430 | GAD-2/PHQ-9 | 21.60% | 75.10% | / |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira Carvalho, P.; Hülsdünker, T.; Carson, F. The Impact of the COVID-19 Lockdown on European Students’ Negative Emotional Symptoms: A Systematic Review and Meta-Analysis. Behav. Sci. 2022, 12, 3. https://doi.org/10.3390/bs12010003
Oliveira Carvalho P, Hülsdünker T, Carson F. The Impact of the COVID-19 Lockdown on European Students’ Negative Emotional Symptoms: A Systematic Review and Meta-Analysis. Behavioral Sciences. 2022; 12(1):3. https://doi.org/10.3390/bs12010003
Chicago/Turabian StyleOliveira Carvalho, Patrick, Thorben Hülsdünker, and Fraser Carson. 2022. "The Impact of the COVID-19 Lockdown on European Students’ Negative Emotional Symptoms: A Systematic Review and Meta-Analysis" Behavioral Sciences 12, no. 1: 3. https://doi.org/10.3390/bs12010003






