Kindness Isn’t Just about Being Nice: The Value Proposition of Kindness as Viewed through the Lens of Incivility in the Healthcare Workplace
Abstract
1. Introduction
2. Scope of Medical Errors as a Problem: Taking Good Care of the Customer (Patient)
3. Stress and Burnout in Health Care
4. Disruptive Behaviors in the Health Care Workplace
5. Experimental Effects of Incivility
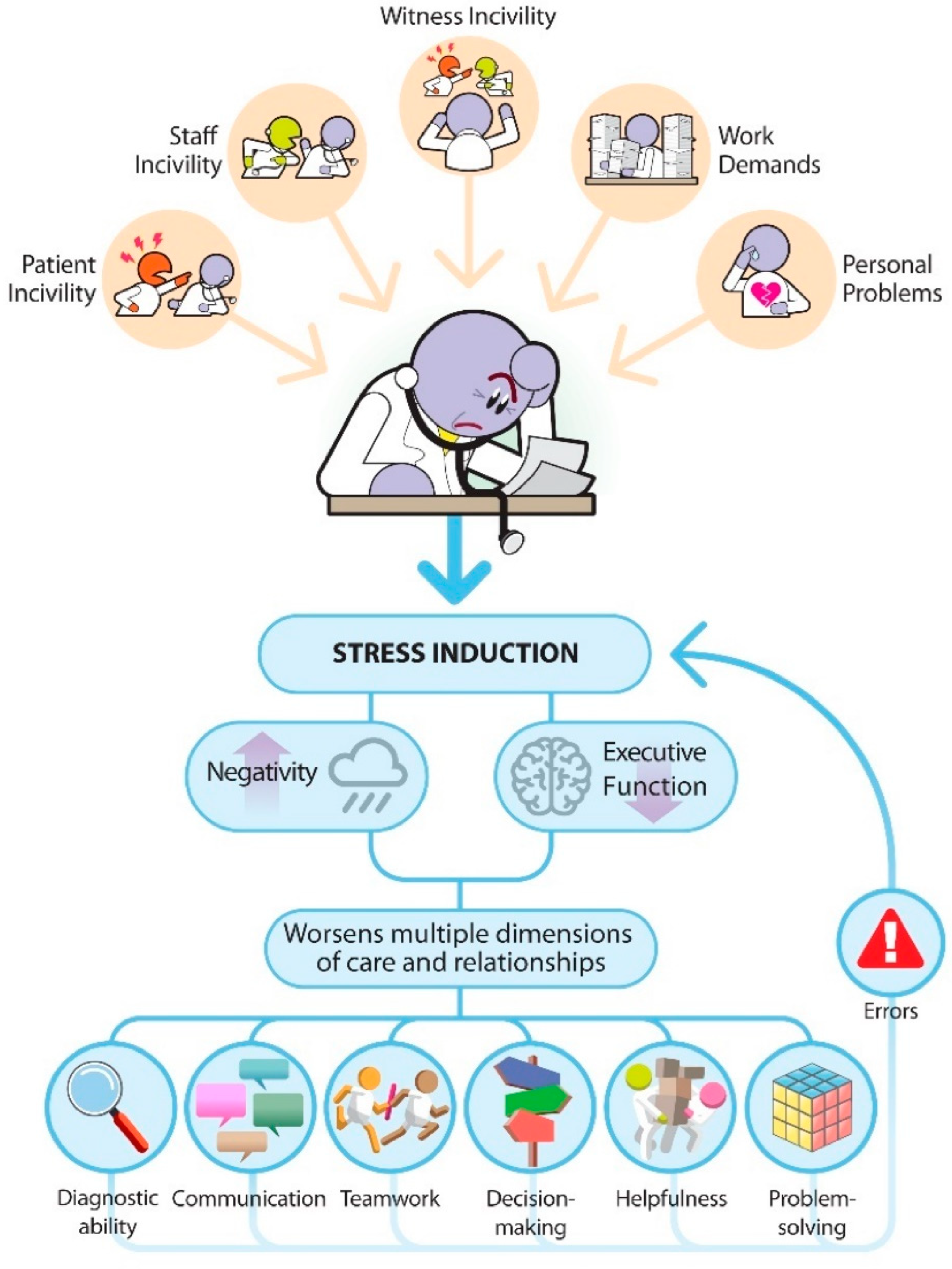
6. Effect of Rudeness on Cognitive Function
7. The Vicious Cycle of Stress and Disruptive Behavior in Health Care
8. Stakeholder Involvement in the Problem
9. Positive Emotions, Clinical Performance, and Cognitive Function
10. Kindness Is Not Just about Being Nice
11. Promoting Kindness and Connection in the Health Care Workplace
12. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Institute of Medicine Committee on Quality of Health Care. To Err Is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press (US): Washington, DC, USA, 2000. [Google Scholar]
- James, J.T. A new, evidence-based estimate of patient harms associated with hospital care. J. Patient Saf. 2013, 9, 122–128. [Google Scholar] [CrossRef]
- Singh, H.; Meyer, A.N.; Thomas, E.J. The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving US adult populations. BMJ Qual. Saf. 2014, 23, 727–731. [Google Scholar] [CrossRef]
- AHRQ. AHRQ National Scorecard on Hospital-Acquired Conditions: Final Results for 2014 through 2017. 2020. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/pfp/Updated-hacreportFInal2017data.pdf (accessed on 10 January 2023).
- Budnitz, D.S.; Pollock, D.A.; Weidenbach, K.N.; Mendelsohn, A.B.; Schroeder, T.J.; Annest, J.L. National surveillance of emergency department visits for outpatient adverse drug events. JAMA 2006, 296, 1858–1866. [Google Scholar] [CrossRef] [PubMed]
- Budnitz, D.S.; Shehab, N.; Lovegrove, M.C.; Geller, A.I.; Lind, J.N.; Pollock, D.A. US Emergency Department Visits Attributed to Medication Harms, 2017–2019. JAMA 2021, 326, 1299–1309. [Google Scholar] [CrossRef]
- Center, B.L. The Financial and Human Cost of Medical Error; Betsy Lehman Center for Patient Safety: Boston, MA, USA, 2019. [Google Scholar]
- Rosenstein, A.H. Measuring and managing the economic impact of disruptive behaviors in the hospital. J. Healthc. Risk Manag. 2010, 30, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Adler, L.; Yi, D.; Li, M.; McBroom, B.; Hauck, L.; Sammer, C.; Jones, C.; Shaw, T.; Classen, D. Impact of Inpatient Harms on Hospital Finances and Patient Clinical Outcomes. J. Patient Saf. 2018, 14, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Prentice, J.C.; Bell, S.K.; Thomas, E.J.; Schneider, E.C.; Weingart, S.N.; Weissman, J.S.; Schlesinger, M.J. Association of open communication and the emotional and behavioural impact of medical error on patients and families: State-wide cross-sectional survey. BMJ Qual. Saf. 2020, 29, 883–894. [Google Scholar] [CrossRef] [PubMed]
- Slawomirski, L.; Klazinga, N. The Economics of Patient Safety: From Analysis to Action; OECD Publishing: Paris, France, 2022. [Google Scholar] [CrossRef]
- Glavin, R.J. Human performance limitations (communication, stress, prospective memory and fatigue). Best Pract. Res. Clin. Anaesthesiol. 2011, 25, 193–206. [Google Scholar] [CrossRef]
- Rosenstein, A.H.; O’Daniel, M. A survey of the impact of disruptive behaviors and communication defects on patient safety. Jt. Comm. J. Qual. Patient Saf. 2008, 34, 464–471. [Google Scholar] [CrossRef]
- Leonard, M.W.; Frankel, A.S. Role of effective teamwork and communication in delivering safe, high-quality care. Mt. Sinai J. Med. 2011, 78, 820–826. [Google Scholar] [CrossRef]
- Fryburg, D.A. What’s Playing in Your Waiting Room? Patient and Provider Stress and the Impact of Waiting Room Media. J. Patient Exp. 2021, 8, 23743735211049880. [Google Scholar] [CrossRef]
- Sherwin, H.N.; McKeown, M.; Evans, M.F.; Bhattacharyya, O.K. The waiting room “wait”: From annoyance to opportunity. Can. Fam. Physician 2013, 59, 479–481. [Google Scholar] [PubMed]
- Franklin, S.S.; Thijs, L.; Hansen, T.W.; O’Brien, E.; Staessen, J.A. White-Coat Hypertension. Hypertension 2013, 62, 982–987. [Google Scholar] [CrossRef] [PubMed]
- Gaffney, A.; Woolhandler, S.; Cai, C.; Bor, D.; Himmelstein, J.; McCormick, D.; Himmelstein, D.U. Medical Documentation Burden Among US Office-Based Physicians in 2019: A National Study. JAMA Intern. Med. 2022, 182, 564–566. [Google Scholar] [CrossRef]
- Dewa, C.S.; Loong, D.; Bonato, S.; Trojanowski, L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open 2017, 7, e015141. [Google Scholar] [CrossRef] [PubMed]
- Singh Ospina, N.; Phillips, K.A.; Rodriguez-Gutierrez, R.; Castaneda-Guarderas, A.; Gionfriddo, M.R.; Branda, M.E.; Montori, V.M. Eliciting the Patient’s Agenda- Secondary Analysis of Recorded Clinical Encounters. J. Gen. Intern. Med. 2019, 34, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Kushnir, T.; Kushnir, J.; Sarel, A.; Cohen, A.H. Exploring physician perceptions of the impact of emotions on behaviour during interactions with patients. Fam. Pract. 2011, 28, 75–81. [Google Scholar] [CrossRef]
- Stewart, M.; Brown, J.B.; Donner, A.; McWhinney, I.R.; Oates, J.; Weston, W.W.; Jordan, J. The impact of patient-centered care on outcomes. J. Fam. Pract. 2000, 49, 796–804. [Google Scholar]
- Stewart, M.A. Effective physician-patient communication and health outcomes: A review. CMAJ 1995, 152, 1423–1433. [Google Scholar]
- Randall, C.L.; Shulman, G.P.; Crout, R.J.; McNeil, D.W. Gagging and its associations with dental care-related fear, fear of pain and beliefs about treatment. J. Am. Dent. Assoc. 2014, 145, 452–458. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; West, C.P.; Hunderfund, A.L.; Sinsky, C.A.; Trockel, M.; Tutty, M.; Carlasare, L.; Satele, D.; Shanafelt, T. Relationship between Burnout, Professional Behaviors, and Cost-Conscious Attitudes Among US Physicians. J. Gen. Intern. Med. 2020, 35, 1465–1476. [Google Scholar] [CrossRef]
- Giménez Lozano, J.M.; Martínez Ramón, J.P.; Morales Rodríguez, F.M. Doctors and Nurses: A Systematic Review of the Risk and Protective Factors in Workplace Violence and Burnout. Int. J. Environ. Res. Public Health 2021, 18, 3280. [Google Scholar] [CrossRef]
- Martínez-Zaragoza, F.; Fernández-Castro, J.; Benavides-Gil, G.; García-Sierra, R. How the Lagged and Accumulated Effects of Stress, Coping, and Tasks Affect Mood and Fatigue during Nurses’ Shifts. Int. J. Environ. Res. Public Health 2020, 17, 7277. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Shanafelt, T.D.; Johnson, P.O.; Johnson, L.A.; Satele, D.; West, C.P. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. 2019, 18, 57. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Balch, C.M.; Bechamps, G.; Russell, T.; Dyrbye, L.; Satele, D.; Collicott, P.; Novotny, P.J.; Sloan, J.; Freischlag, J. Burnout and medical errors among American surgeons. Ann. Surg. 2010, 251, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Sinsky, C.; Trockel, M.; Tutty, M.; Nedelec, L.; Carlasare, L.E.; Shanafelt, T.D. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw. Open 2020, 3, e209385. [Google Scholar] [CrossRef]
- Khan, A.; Teoh, K.R.; Islam, S.; Hassard, J. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: A cross-sectional study of NHS consultants in the UK. BMJ Open 2018, 8, e018720. [Google Scholar] [CrossRef] [PubMed]
- Carter, M.; Thompson, N.; Crampton, P.; Morrow, G.; Burford, B.; Gray, C.; Illing, J. Workplace bullying in the UK NHS: A questionnaire and interview study on prevalence, impact and barriers to reporting. BMJ Open 2013, 3, e002628. [Google Scholar] [CrossRef]
- Han, S.; Shanafelt, T.D.; Sinsky, C.A.; Awad, K.M.; Dyrbye, L.N.; Fiscus, L.C.; Trockel, M.; Goh, J. Estimating the Attributable Cost of Physician Burnout in the United States. Ann. Intern. Med. 2019, 170, 784–790. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Tan, A.; Hsieh, A.P.; Gawlik, K.; Arslanian-Engoren, C.; Braun, L.T.; Dunbar, S.; Dunbar-Jacob, J.; Lewis, L.M.; Millan, A.; et al. Critical Care Nurses’ Physical and Mental Health, Worksite Wellness Support, and Medical Errors. Am. J. Crit. Care 2021, 30, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Tawfik, D.S.; Profit, J.; Morgenthaler, T.I.; Satele, D.V.; Sinsky, C.A.; Dyrbye, L.N.; Tutty, M.A.; West, C.P.; Shanafelt, T.D. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin. Proc. 2018, 93, 1571–1580. [Google Scholar] [CrossRef] [PubMed]
- Menon, N.K.; Shanafelt, T.D.; Sinsky, C.A.; Linzer, M.; Carlasare, L.; Brady, K.J.S.; Stillman, M.J.; Trockel, M.T. Association of Physician Burnout With Suicidal Ideation and Medical Errors. JAMA Netw. Open 2020, 3, e2028780. [Google Scholar] [CrossRef] [PubMed]
- Jun, J.; Ojemeni, M.M.; Kalamani, R.; Tong, J.; Crecelius, M.L. Relationship between nurse burnout, patient and organizational outcomes: Systematic review. Int. J. Nurs. Stud. 2021, 119, 103933. [Google Scholar] [CrossRef] [PubMed]
- Regehr, C.; Glancy, D.; Pitts, A.; LeBlanc, V.R. Interventions to reduce the consequences of stress in physicians: A review and meta-analysis. J. Nerv. Ment. Dis. 2014, 202, 353–359. [Google Scholar] [CrossRef]
- Garcia, C.d.L.; Abreu, L.C.d.; Ramos, J.L.S.; Castro, C.F.D.d.; Smiderle, F.R.N.; Santos, J.A.d.; Bezerra, I.M.P. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina 2019, 55, 553. [Google Scholar] [CrossRef]
- Hodkinson, A.; Zhou, A.; Johnson, J.; Geraghty, K.; Riley, R.; Zhou, A.; Panagopoulou, E.; Chew-Graham, C.A.; Peters, D.; Esmail, A.; et al. Associations of physician burnout with career engagement and quality of patient care: Systematic review and meta-analysis. BMJ 2022, 378, e070442. [Google Scholar] [CrossRef]
- Jacobs, A.K. Rebuilding an Enduring Trust in Medicine. Circulation 2005, 111, 3494–3498. [Google Scholar] [CrossRef]
- Wiegmann, D.A.; ElBardissi, A.W.; Dearani, J.A.; Daly, R.C.; Sundt, T.M., 3rd. Disruptions in surgical flow and their relationship to surgical errors: An exploratory investigation. Surgery 2007, 142, 658–665. [Google Scholar] [CrossRef]
- Leonard, M.; Graham, S.; Bonacum, D. The human factor: The critical importance of effective teamwork and communication in providing safe care. Qual. Saf. Health Care 2004, 13 (Suppl. S1), i85–i90. [Google Scholar] [CrossRef]
- Paulmann, S.; Furnes, D.; Bøkenes, A.M.; Cozzolino, P.J. How Psychological Stress Affects Emotional Prosody. PLoS ONE 2016, 11, e0165022. [Google Scholar] [CrossRef]
- Mehrabian, A.; Ferris, S.R. Inference of attitudes from nonverbal communication in two channels. J. Consult. Psychol. 1967, 31, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Kappen, M.; van der Donckt, J.; Vanhollebeke, G.; Allaert, J.; Degraeve, V.; Madhu, N.; Van Hoecke, S.; Vanderhasselt, M.-A. Acoustic speech features in social comparison: How stress impacts the way you sound. Sci. Rep. 2022, 12, 22022. [Google Scholar] [CrossRef]
- Carlasare, L.E.; Hickson, G.B. Whose Responsibility Is It to Address Bullying in Health Care? AMA J. Ethics 2021, 23, E931–E936. [Google Scholar] [CrossRef]
- Andersson, L.M.; Pearson, C.M. Tit for Tat? The Spiraling Effect of Incivility in the Workplace. Acad. Manag. Rev. 1999, 24, 452–471. [Google Scholar] [CrossRef]
- Dabekaussen, K.F.A.A.; Scheepers, R.A.; Heineman, E.; Haber, A.L.; Lombarts, K.M.J.M.H.; Jaarsma, D.A.D.C.; Shapiro, J. Health care professionals’ perceptions of unprofessional behaviour in the clinical workplace. PLoS ONE 2023, 18, e0280444. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.F.; Arora, V.M.; Rasinski, K.A.; Curlin, F.A.; Yoon, J.D. The prevalence of medical student mistreatment and its association with burnout. Acad. Med. 2014, 89, 749–754. [Google Scholar] [CrossRef]
- Kemper, K.J.; Schwartz, A. Bullying, Discrimination, Sexual Harassment, and Physical Violence: Common and Associated With Burnout in Pediatric Residents. Acad. Pediatr. 2020, 20, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Leape, L.L.; Shore, M.F.; Dienstag, J.L.; Mayer, R.J.; Edgman-Levitan, S.; Meyer, G.S.; Healy, G.B. Perspective: A culture of respect, part 1: The nature and causes of disrespectful behavior by physicians. Acad. Med. 2012, 87, 845–852. [Google Scholar] [CrossRef]
- Einarsen, S.; Hoel, H.; Notelaers, G. Measuring exposure to bullying and harassment at work: Validity, factor structure and psychometric properties of the Negative Acts Questionnaire-Revised. Work. Stress 2009, 23, 24–44. [Google Scholar] [CrossRef]
- Westbrook, J.; Sunderland, N.; Li, L.; Koyama, A.; McMullan, R.; Urwin, R.; Churruca, K.; Baysari, M.T.; Jones, C.; Loh, E.; et al. The prevalence and impact of unprofessional behaviour among hospital workers: A survey in seven Australian hospitals. Med. J. Aust. 2021, 214, 31–37. [Google Scholar] [CrossRef]
- Lim, S.; Goh, E.Y.; Tay, E.; Tong, Y.K.; Chung, D.; Devi, K.; Tan, C.H.; Indran, I.R. Disruptive behavior in a high-power distance culture and a three-dimensional framework for curbing it. Health Care Manag. Rev. 2022, 47, 133–143. [Google Scholar] [CrossRef]
- Oppel, E.M.; Mohr, D.C.; Benzer, J.K. Let’s be civil: Elaborating the link between civility climate and hospital performance. Health Care Manag. Rev. 2019, 44, 196–205. [Google Scholar] [CrossRef]
- Cooper, W.O.; Guillamondegui, O.; Hines, O.J.; Hultman, C.S.; Kelz, R.R.; Shen, P.; Spain, D.A.; Sweeney, J.F.; Moore, I.N.; Hopkins, J.; et al. Use of Unsolicited Patient Observations to Identify Surgeons with Increased Risk for Postoperative Complications. JAMA Surg. 2017, 152, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Lagoo, J.; Berry, W.R.; Miller, K.; Neal, B.J.; Sato, L.; Lillemoe, K.D.; Doherty, G.M.; Kasser, J.R.; Chaikof, E.L.; Gawande, A.A.; et al. Multisource Evaluation of Surgeon Behavior Is Associated with Malpractice Claims. Ann. Surg. 2019, 270, 84–90. [Google Scholar] [CrossRef]
- Rowe, S.G.; Stewart, M.T.; Van Horne, S.; Pierre, C.; Wang, H.; Manukyan, M.; Bair-Merritt, M.; Lee-Parritz, A.; Rowe, M.P.; Shanafelt, T.; et al. Mistreatment Experiences, Protective Workplace Systems, and Occupational Distress in Physicians. JAMA Netw. Open 2022, 5, e2210768. [Google Scholar] [CrossRef] [PubMed]
- Viotti, S.; Converso, D.; Hamblin, L.E.; Guidetti, G.; Arnetz, J.E. Organisational efficiency and co-worker incivility: A cross-national study of nurses in the USA and Italy. J. Nurs. Manag. 2018, 26, 597–604. [Google Scholar] [CrossRef]
- Gascon, S.; Leiter, M.P.; Andrés, E.; Santed, M.A.; Pereira, J.P.; Cunha, M.J.; Albesa, A.; Montero-Marín, J.; García-Campayo, J.; Martínez-Jarreta, B. The role of aggressions suffered by healthcare workers as predictors of burnout. J. Clin. Nurs. 2013, 22, 3120–3129. [Google Scholar] [CrossRef]
- Hatfield, M.; Ciaburri, R.; Shaikh, H.; Wilkins, K.M.; Bjorkman, K.; Goldenberg, M.; McCollum, S.; Shabanova, V.; Weiss, P. Addressing Mistreatment of Providers by Patients and Family Members as a Patient Safety Event. Hosp. Pediatr. 2022, 12, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-L.; Li, R.-Q.; Qiu, D.; Xiao, S.-Y. Prevalence of Workplace Physical Violence against Health Care Professionals by Patients and Visitors: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 299. [Google Scholar] [CrossRef] [PubMed]
- Weber-Shandwick. Civility in Americal 2019: Solutions for Tomorrow; Weber-Shandwick: New York, NY, USA, 2019. [Google Scholar]
- Philips, T.; Stuart, H. An Age of Incivility: Understanding the New Politics; Policy Exchange: London, UK, 2018. [Google Scholar]
- Schilpzand, P.; De Pater, I.E.; Erez, A. Workplace incivility: A review of the literature and agenda for future research. J. Organ. Behav. 2016, 37, S57–S88. [Google Scholar] [CrossRef]
- Loh, J.M.I.; Saleh, A. Lashing out: Emotional exhaustion triggers retaliatory incivility in the workplace. Heliyon 2022, 8, E08694. [Google Scholar] [CrossRef] [PubMed]
- Katz, D.; Blasius, K.; Isaak, R.; Lipps, J.; Kushelev, M.; Goldberg, A.; Fastman, J.; Marsh, B.; DeMaria, S. Exposure to incivility hinders clinical performance in a simulated operative crisis. BMJ Qual. Saf. 2019, 28, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Riskin, A.; Erez, A.; Foulk, T.A.; Riskin-Geuz, K.S.; Ziv, A.; Sela, R.; Pessach-Gelblum, L.; Bamberger, P.A. Rudeness and Medical Team Performance. Pediatrics 2017, 139, e20162305. [Google Scholar] [CrossRef]
- Woolum, A.; Echeto, L.F.; Cooper, B.; Gale, J.; Erez, A.; Katz, J.; Guelmann, M.; Jerrell, R.G.; Zoidis, P. How witnessing rudeness can disrupt psycho-motor performance of dental students. J. Dent. Educ. 2021, 85, 1588–1595. [Google Scholar] [CrossRef]
- Mamede, S.; Van Gog, T.; Schuit, S.C.E.; Van den Berge, K.; Van Daele, P.L.A.; Bueving, H.; Van der Zee, T.; Van den Broek, W.W.; Van Saase, J.L.C.M.; Schmidt, H.G. Why patients’ disruptive behaviours impair diagnostic reasoning: A randomised experiment. BMJ Qual. Saf. 2017, 26, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Porath, C.L.; Foulk, T.; Erez, A. How incivility hijacks performance: It robs cognitive resources, increases dysfunctional behavior, and infects team dynamics and functioning. Organ. Dyn. 2015, 44, 258–265. [Google Scholar] [CrossRef]
- Simons, D.J.; Chabris, C.F. Gorillas in our midst: Sustained inattentional blindness for dynamic events. Perception 1999, 28, 1059–1074. [Google Scholar] [CrossRef]
- Drew, T.; Võ, M.L.; Wolfe, J.M. The invisible gorilla strikes again: Sustained inattentional blindness in expert observers. Psychol. Sci. 2013, 24, 1848–1853. [Google Scholar] [CrossRef]
- Belfi, L.M.; Chetlen, A.; Frigini, A.; Jay, A.; Methratta, S.T.; Robbins, J.; Woods, R.; Deitte, L. Recovering Joy in the Workplace Requires PRACTICE. Acad. Radiol. 2023, 30, 536–540. [Google Scholar] [CrossRef]
- LeBlanc, V.R.; McConnell, M.M.; Monteiro, S.D. Predictable chaos: A review of the effects of emotions on attention, memory and decision making. Adv. Health Sci. Educ. Theory Pract. 2015, 20, 265–282. [Google Scholar] [CrossRef]
- Arnsten, A.F.T. Stress weakens prefrontal networks: Molecular insults to higher cognition. Nat. Neurosci. 2015, 18, 1376–1385. [Google Scholar] [CrossRef]
- Arnsten, A.F.T.; Shanafelt, T. Physician Distress and Burnout: The Neurobiological Perspective. Mayo Clin. Proc. 2021, 96, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Liston, C.; McEwen, B.S.; Casey, B.J. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proc. Natl. Acad. Sci. USA 2009, 106, 912–917. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Executive functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed]
- de Kloet, E.R.; Joëls, M.; Holsboer, F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005, 6, 463–475. [Google Scholar] [CrossRef]
- Heyhoe, J.; Lawton, R. Social emotion and patient safety: An important and understudied intersection. BMJ Qual. Saf. 2020, 29, 1–2. [Google Scholar] [CrossRef]
- Croskerry, P.; Abbass, A.; Wu, A.W. Emotional influences in patient safety. J. Patient Saf. 2010, 6, 199–205. [Google Scholar] [CrossRef]
- Croskerry, P.; Abbass, A.A.; Wu, A.W. How doctors feel: Affective issues in patients’ safety. Lancet 2008, 372, 1205–1206. [Google Scholar] [CrossRef]
- Liu, G.; Chimowitz, H.; Isbell, L.M. Affective influences on clinical reasoning and diagnosis: Insights from social psychology and new research opportunities. Diagnosis 2022, 9, 295–305. [Google Scholar] [CrossRef]
- Wu, A.W.; Steckelberg, R.C. Medical error, incident investigation and the second victim: Doing better but feeling worse? BMJ Qual. Saf. 2012, 21, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.; Lawton, R.; Stewart, K. Doctors’ experiences of adverse events in secondary care: The professional and personal impact. Clin. Med. 2014, 14, 585–590. [Google Scholar] [CrossRef]
- Ferguson, M. You cannot leave it at the office: Spillover and crossover of coworker incivility. J. Organ. Behav. 2012, 33, 571–588. [Google Scholar] [CrossRef]
- Barsade, S.G.; Coutifaris, C.G.V.; Pillemer, J. Emotional contagion in organizational life. Res. Organ. Behav. 2018, 38, 137–151. [Google Scholar] [CrossRef]
- Foulk, T.; Woolum, A.; Erez, A. Catching rudeness is like catching a cold: The contagion effects of low-intensity negative behaviors. J. Appl. Psychol. 2016, 101, 50–67. [Google Scholar] [CrossRef] [PubMed]
- Petitta, L.; Jiang, L. Burning out? Watch your own incivility and the emotions you spread. Work 2019, 64, 671–683. [Google Scholar] [CrossRef]
- Rawson, J.V.; Thompson, N.; Sostre, G.; Deitte, L. The cost of disruptive and unprofessional behaviors in health care. Acad. Radiol. 2013, 20, 1074–1076. [Google Scholar] [CrossRef]
- Hickson, G.B.; Federspiel, C.F.; Pichert, J.W.; Miller, C.S.; Gauld-Jaeger, J.; Bost, P. Patient complaints and malpractice risk. JAMA 2002, 287, 2951–2957. [Google Scholar] [CrossRef]
- Oyebode, F. Clinical Errors and Medical Negligence. Med. Princ. Pract. 2013, 22, 323–333. [Google Scholar] [CrossRef]
- Oppel, E.M.; Mohr, D.C. “Paying it forward”: The link between providers’ civility climate, civility toward patients and patient experience outcomes. Health Care Manag. Rev. 2020, 45, 141–150. [Google Scholar] [CrossRef]
- Estrada, C.A.; Isen, A.M.; Young, M.J. Positive affect facilitates integration of information and decreases anchoring in reasoning among physicians. Organ. Behav. Hum. Decis. Process. 1997, 72, 117–135. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Branigan, C. Positive emotions broaden the scope of attention and thought-action repertoires. Cogn. Emot. 2005, 19, 313–332. [Google Scholar] [CrossRef]
- Isen, A.M. An Influence of Positive Affect on Decision Making in Complex Situations: Theoretical Issues With Practical Implications. J. Consum. Psychol. 2001, 11, 75–85. [Google Scholar] [CrossRef]
- Yang, H.; Yang, S.; Isen, A.M. Positive affect improves working memory: Implications for controlled cognitive processing. Cogn. Emot. 2013, 27, 474–482. [Google Scholar] [CrossRef]
- Sigwalt, F.; Petit, G.; Evain, J.N.; Claverie, D.; Bui, M.; Guinet-Lebreton, A.; Trousselard, M.; Canini, F.; Chassard, D.; Duclos, A.; et al. Stress Management Training Improves Overall Performance during Critical Simulated Situations: A Prospective Randomized Controlled Trial. Anesthesiology 2020, 133, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Schlatter, S.T.; Thérond, C.C.; Guillot, A.; Louisy, S.P.; Duclos, A.; Lehot, J.-J.; Rimmelé, T.; Debarnot, U.S.; Lilot, M.E. Effects of relaxing breathing paired with cardiac biofeedback on performance and relaxation during critical simulated situations: A prospective randomized controlled trial. BMC Med. Educ. 2022, 22, 422. [Google Scholar] [CrossRef] [PubMed]
- Lilot, M.; Evain, J.N.; Bauer, C.; Cejka, J.C.; Faure, A.; Balança, B.; Vassal, O.; Payet, C.; Bui Xuan, B.; Duclos, A.; et al. Relaxation before Debriefing during High-fidelity Simulation Improves Memory Retention of Residents at Three Months: A Prospective Randomized Controlled Study. Anesthesiology 2018, 128, 638–649. [Google Scholar] [CrossRef]
- Viotti, S.; Cortese, C.G.; Garlasco, J.; Rainero, E.; Emelurumonye, I.N.; Passi, S.; Boraso, F.; Gianino, M.M. The Buffering Effect of Humanity of Care in the Relationship between Patient Satisfaction and Waiting Time: A Cross-sectional Study in an Emergency Department. Int. J. Environ. Res. Public Health 2020, 17, 2939. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- Aknin, L.B.; Dunn, E.W.; Norton, M.I. Happiness Runs in a Circular Motion: Evidence for a Positive Feedback Loop between Prosocial Spending and Happiness. J. Happiness Stud. 2012, 13, 347–355. [Google Scholar] [CrossRef]
- Ekman, P. Darwin’s compassionate view of human nature. JAMA 2010, 303, 557–558. [Google Scholar] [CrossRef]
- Keltner, D. Born to Be Good: The Science of a Meaningful Life; W. W. Norton & Co.: New York, NY, USA, 2009; p. 209. [Google Scholar]
- Fryburg, D.A. Kindness as a Stress Reduction-Health Promotion Intervention: A Review of the Psychobiology of Caring. Am. J. Lifestyle Med. 2022, 16, 89–100. [Google Scholar] [CrossRef]
- Kozlowski, D.; Hutchinson, M.; Hurley, J.; Rowley, J.; Sutherland, J. The role of emotion in clinical decision making: An integrative literature review. BMC Med. Educ. 2017, 17, 255. [Google Scholar] [CrossRef]
- Trzeciak, S.; Mazzarelli, A.; Booker, C. Compassionomics: The Revolutionary Scientific Evidence That Caring Makes a Difference; Studer Group: Pensacola, FL, USA, 2019. [Google Scholar]
- Shanafelt, T.D.; Noseworthy, J.H. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clin. Proc. 2017, 92, 129–146. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Hamblin, L.; Russell, J.; Upfal, M.J.; Luborsky, M.; Janisse, J.; Essenmacher, L. Preventing Patient-to-Worker Violence in Hospitals: Outcome of a Randomized Controlled Intervention. J. Occup. Environ. Med. 2017, 59, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.; Murray, L.; Donnelly, M. Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Fam. Pract. 2016, 17, 36. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Plowman, S. The Increasing Importance of a Best Friend at Work; Gallup: Washington, DC, USA, 2022. [Google Scholar]
- Holt-Lunstad, J. Fostering Social Connection in the Workplace. Am. J. Health Promot. 2018, 32, 1307–1312. [Google Scholar] [CrossRef]
- Leape, L.L.; Shore, M.F.; Dienstag, J.L.; Mayer, R.J.; Edgman-Levitan, S.; Meyer, G.S.; Healy, G.B. Perspective: A culture of respect, part 2: Creating a culture of respect. Acad. Med. 2012, 87, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Ellithorpe, M.E.; Ewoldsen, D.R.; Oliver, M.B. Elevation (sometimes) increases altruism: Choice and number of outcomes in elevating media effects. Psychol. Pop. Media Cult. 2015, 4, 236–250. [Google Scholar] [CrossRef]
- Algoe, S.B.; Haidt, J. Witnessing excellence in action: The ‘other-praising’ emotions of elevation, gratitude, and admiration. J. Posit. Psychol. 2009, 4, 105–127. [Google Scholar] [CrossRef]
- Freeman, D.; Aquino, K.; McFerran, B. Overcoming beneficiary race as an impediment to charitable donations: Social dominance orientation, the experience of moral elevation, and donation behavior. Pers. Soc. Psychol. Bull. 2009, 35, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Fryburg, D.A.; Ureles, S.D.; Myrick, J.G.; Carpentier, F.D.; Oliver, M.B. Kindness Media Rapidly Inspires Viewers and Increases Happiness, Calm, Gratitude, and Generosity in a Healthcare Setting. Front. Psychol. 2020, 11, 591942. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fryburg, D.A. Kindness Isn’t Just about Being Nice: The Value Proposition of Kindness as Viewed through the Lens of Incivility in the Healthcare Workplace. Behav. Sci. 2023, 13, 457. https://doi.org/10.3390/bs13060457
Fryburg DA. Kindness Isn’t Just about Being Nice: The Value Proposition of Kindness as Viewed through the Lens of Incivility in the Healthcare Workplace. Behavioral Sciences. 2023; 13(6):457. https://doi.org/10.3390/bs13060457
Chicago/Turabian StyleFryburg, David A. 2023. "Kindness Isn’t Just about Being Nice: The Value Proposition of Kindness as Viewed through the Lens of Incivility in the Healthcare Workplace" Behavioral Sciences 13, no. 6: 457. https://doi.org/10.3390/bs13060457
APA StyleFryburg, D. A. (2023). Kindness Isn’t Just about Being Nice: The Value Proposition of Kindness as Viewed through the Lens of Incivility in the Healthcare Workplace. Behavioral Sciences, 13(6), 457. https://doi.org/10.3390/bs13060457





