Estimating the Heterogeneous Causal Effects of Parent–Child Relationships among Chinese Children with Oppositional Defiant Symptoms: A Machine Learning Approach
Abstract
1. Introduction
1.1. Multilevel Family Model and Oppositional Defiant Symptoms
1.2. Parent–Child Relationship and Oppositional Defiant Symptoms
1.3. Causal Inference and Its Heterogeneity
1.4. Aims of the Study
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Assessment of Oppositional Defiant Symptoms (AODS)
2.2.2. PCR
2.2.3. Monthly Income
2.2.4. Family Cohesion/Adaptability
2.2.5. Marital Relationship
2.2.6. Parenting Style
2.2.7. Parent Emotion Regulation
2.2.8. Child Emotion Regulation
2.3. CF Modeling
2.3.1. Data Preprocessing
2.3.2. Model Construction
2.3.3. Model Evaluation
2.3.4. Analysis of Causal Effect and Its Heterogeneity
2.4. Analysis of HMR
3. Results
3.1. Descriptive Statistics
3.2. Causal Effect of PCR on Oppositional Defiant Symptoms
3.3. Heterogeneous Causal Effects
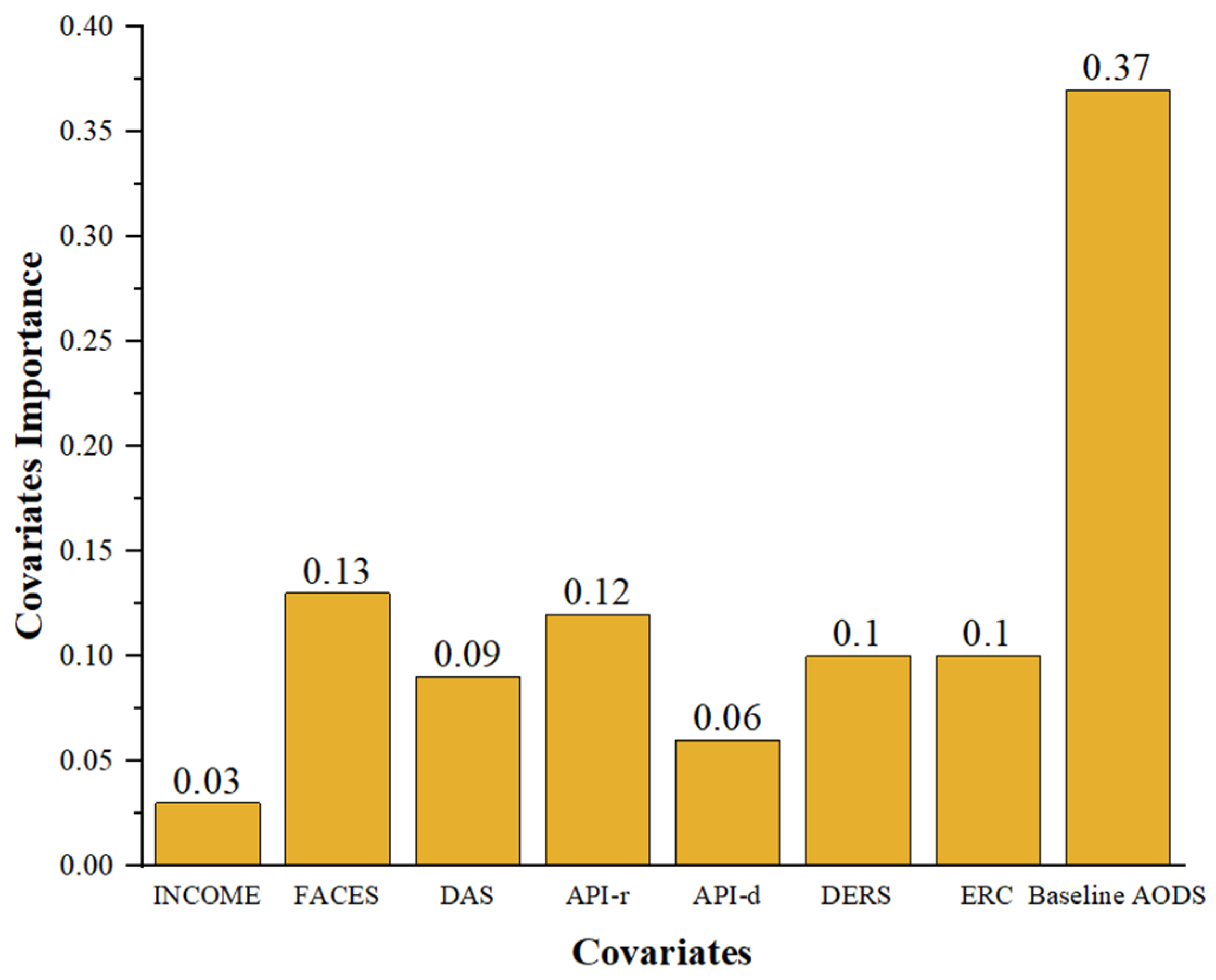
3.3.1. General Analysis of Heterogeneity
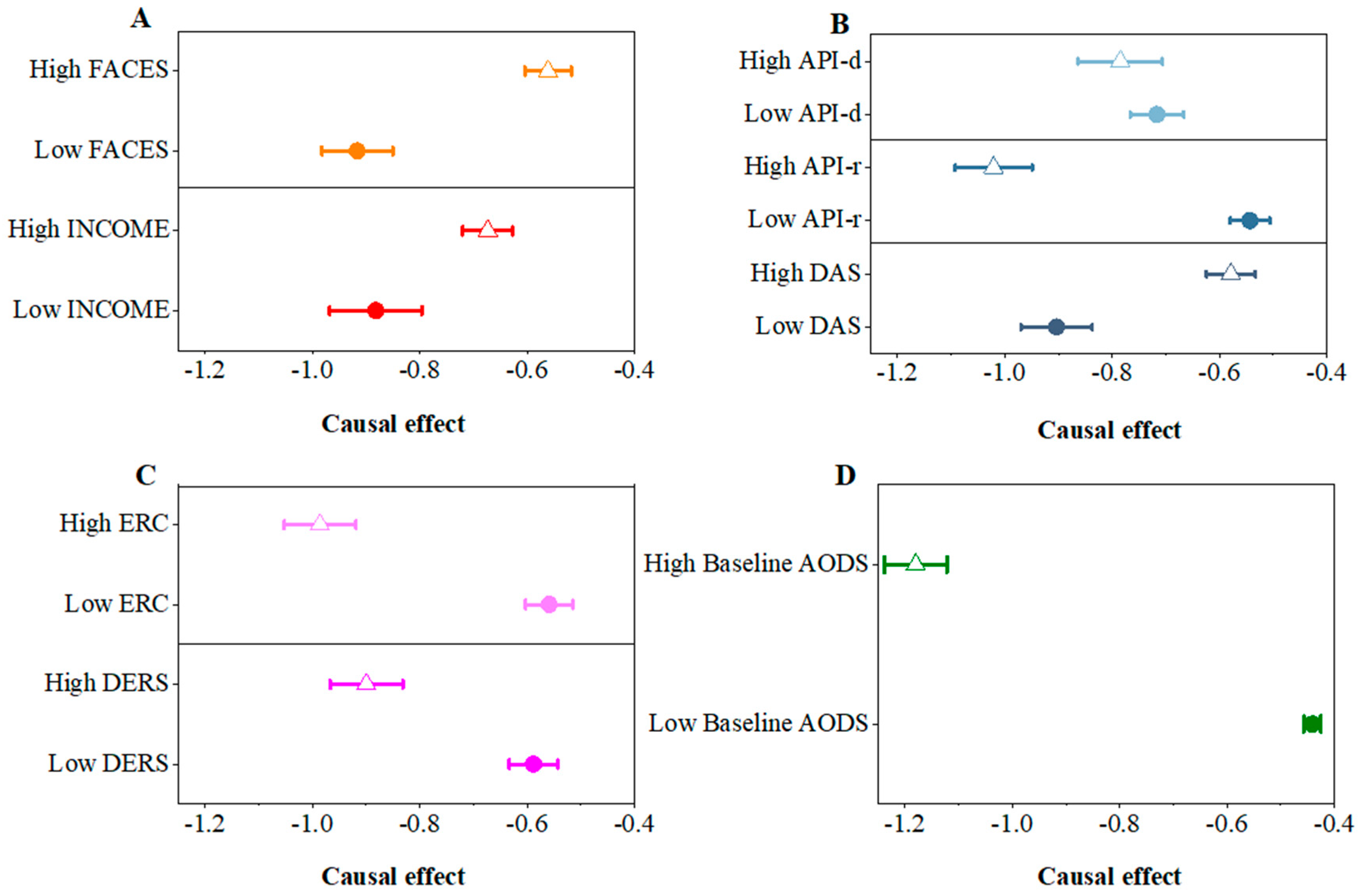
3.3.2. Heterogeneity among
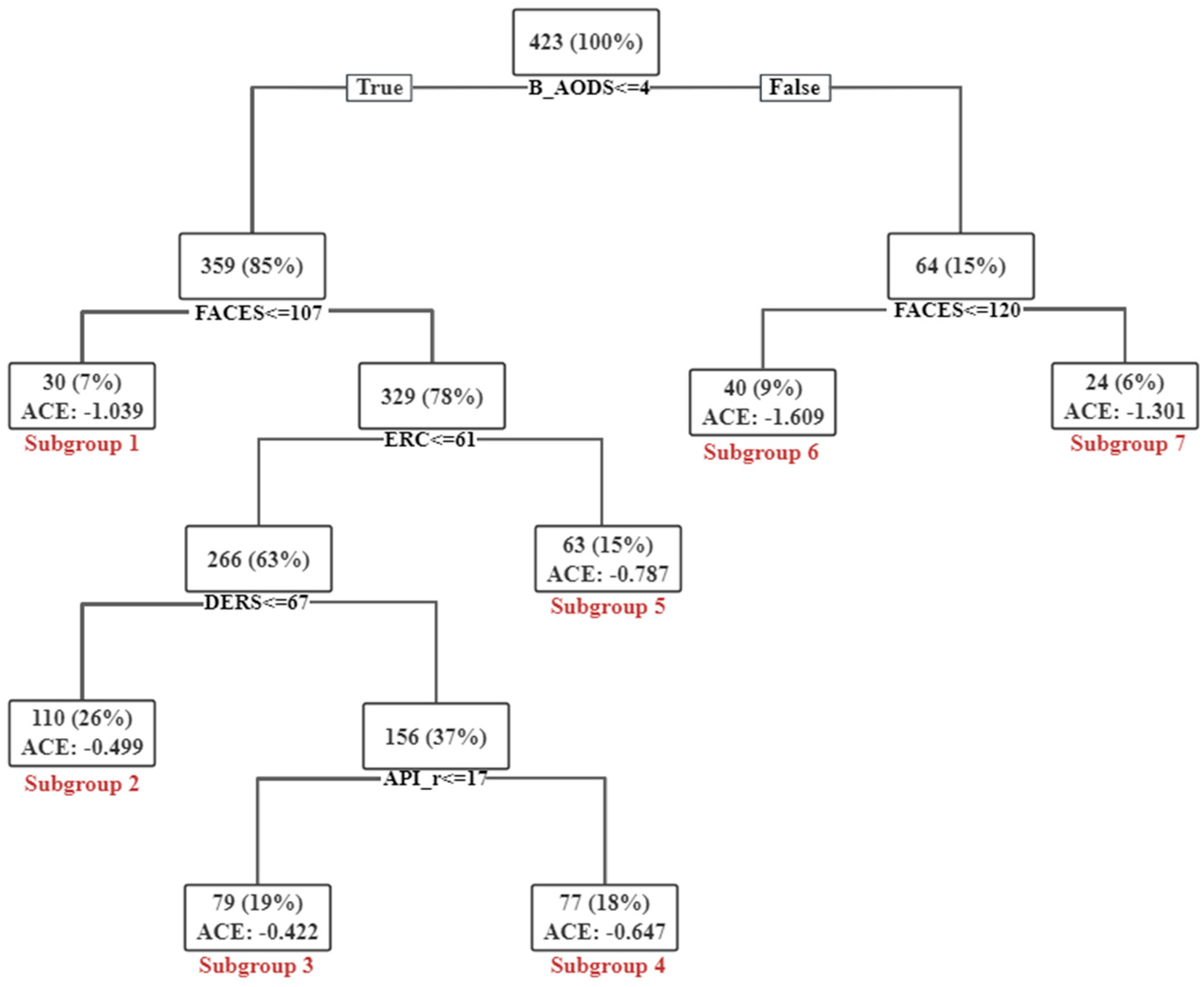
3.3.3. Heterogeneity Based on Causal Tree
3.4. Results of HMR Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Carter, M.J. Diagnostic and statistical manual of mental disorders. Ther. Recreat. J. 2014, 48, 275. [Google Scholar]
- Ayano, G.; Lin, A.; Betts, K.; Tait, R.; Dachew, B.A.; Alati, R. Risk of conduct and oppositional defiant disorder symptoms in offspring of parents with mental health problems: Findings from the Raine Study. J. Psychiatr. Res. 2021, 138, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Meza, J.; Lin, X.; He, T.; Chen, H.; Wang, Y.; Qin, S. Oppositional defiant disorder symptoms and children’s feelings of happiness and depression: Mediating roles of interpersonal relationships. Child Indic. Res. 2020, 13, 215–235. [Google Scholar] [CrossRef]
- He, T.; Su, J.; Jiang, Y.; Qin, S.; Chi, P.; Lin, X. Parenting Stress and Depressive Symptoms among Chinese Parents of Children with and without Oppositional Defiant Disorder: A Three-Wave Longitudinal Study. Child Psychiatry Hum. Dev. 2020, 51, 855–867. [Google Scholar] [CrossRef]
- Lin, X.; Li, W.; Li, Y.; Zhao, Y.; Shen, J.; Fang, X. The family factors and family intervention program for child who have oppositional defiant disorder. Adv. Psychol. Sci. 2013, 21, 1983. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Gouze, K.R.; Hopkins, J.; Bryant, F.B.; LeBailly, S.A. A multi-domain model of risk factors for oppositional defiant symptoms in a community sample of 4-year-olds. J. Abnorm. Child Psychol. 2012, 40, 741–757. [Google Scholar] [CrossRef] [PubMed]
- Antúnez, Z.; de la Osa, N.; Granero, R.; Ezpeleta, L. Parental psychopathology levels as a moderator of temperament and oppositional defiant disorder symptoms in preschoolers. J. Child Fam. Stud. 2016, 25, 3124–3135. [Google Scholar] [CrossRef]
- Lin, X.; Li, L.; Heath, M.A.; Chi, P.; Xu, S.; Fang, X. Multiple levels of family factors and oppositional defiant disorder symptoms among Chinese children. Fam. Process 2018, 57, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Lin, X.; Chi, P.; Zhou, Q.; Hou, X. Multi-level family factors and affective and behavioral symptoms of oppositional defiant disorder in Chinese children. Front. Psychol. 2017, 8, 1123. [Google Scholar] [CrossRef]
- Lin, X.; He, T.; Heath, M.; Chi, P.; Hinshaw, S. A Systematic Review of Multiple Family Factors Associated with Oppositional Defiant Disorder. Int. J. Environ. Res. Public Health 2022, 19, 10866. [Google Scholar] [CrossRef]
- Burke, J.D.; Hipwell, A.E.; Loeber, R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 484–492. [Google Scholar] [CrossRef]
- Harvey, E.A.; Metcalfe, L.A.; Herbert, S.D.; Fanton, J.H. The role of family experiences and ADHD in the early development of oppositional defiant disorder. J. Consult. Clin. Psychol. 2011, 79, 784–795. [Google Scholar] [CrossRef]
- Chen, H.; Lin, X.; Heath, M.A.; Ding, W. Family violence and oppositional defiant disorder symptoms in Chinese children: The role of parental alienation and child emotion regulation. Child Fam. Soc. Work 2020, 25, 964–972. [Google Scholar] [CrossRef]
- Forssman, L.; Eninger, L.; Tillman, C.M.; Rodriguez, A.; Bohlin, G. Cognitive functioning and family risk factors in relation to symptom behaviors of ADHD and ODD in adolescents. J. Atten. Disord. 2012, 16, 284–294. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Gouze, K.R.; Hopkins, J.; Bryant, F.B. A multidomain cascade model of early childhood risk factors associated with oppositional defiant disorder symptoms in a community sample of 6-year-olds. Dev. Psychopathol. 2016, 28, 1547–1562. [Google Scholar] [CrossRef]
- Raudino, A.; Fergusson, D.M.; Horwood, L.J. The quality of parent/child relationships in adolescence is associated with poor adult psychosocial adjustment. J. Adolesc. 2013, 36, 331–340. [Google Scholar] [CrossRef]
- Lucia, V.; Breslau, N. Family cohesion and children’s behavior problems: A longitudinal investigation. Psychiatry Res. 2006, 141, 141–149. [Google Scholar] [CrossRef]
- Bornovalova, M.A.; Cummings, J.R.; Hunt, E.; Blazei, R.; Malone, S.; Iacono, W.G. Understanding the relative contributions of direct environmental effects and passive genotype–environment correlations in the association between familial risk factors and child disruptive behavior disorders. Psychol. Med. 2014, 44, 831–844. [Google Scholar] [CrossRef]
- Braithwaite, S.R.; Steele, E.; Spjut, K.; Dowdle, K.K.; Harper, J. Parent–child connectedness mediates the association between marital conflict and children’s internalizing/externalizing outcomes. J. Child Fam. Stud. 2015, 24, 3690–3699. [Google Scholar] [CrossRef]
- Munkvold, L.H.; Lundervold, A.J.; Manger, T. Oppositional defiant disorder—Gender differences in co-occurring symptoms of mental health problems in a general population of children. J. Abnorm. Child Psychol. 2011, 39, 577–587. [Google Scholar] [CrossRef]
- Lin, X.; Li, L.; Chi, P.; Wang, Z.; Heath, M.A.; Du, H.; Fang, X. Child maltreatment and interpersonal relationship among Chinese children with oppositional defiant disorder. Child Abus. Negl. 2016, 51, 192–202. [Google Scholar] [CrossRef]
- Tseng, W.L.; Kawabata, Y.; Gau, S.S.F. Social adjustment among Taiwanese children with symptoms of ADHD, ODD, and ADHD comorbid with ODD. Child Psychiatry Hum. Dev. 2011, 42, 134–151. [Google Scholar] [CrossRef]
- Duncombe, M.E.; Havighurst, S.S.; Holland, K.A.; Frankling, E.J. The contribution of parenting practices and parent emotion factors in children at risk for disruptive behavior disorders. Child Psychiatry Hum. Dev. 2012, 43, 715–733. [Google Scholar] [CrossRef]
- Eisenberg, N.; Fabes, R.A. Emotion regulation and children’s socioemotional competence. In Child Psychology: A Handbook of Contemporary Issues; Balter, L., Tamis-LeMonda, C., Eds.; Psychology Press: New York, NY, USA, 2006; pp. 357–381. [Google Scholar]
- Wang, M.; Wang, J. Negative parental attribution and emotional dysregulation in Chinese early adolescents: Harsh fathering and harsh mothering as potential mediators. Child Abus. Negl. 2018, 81, 12–20. [Google Scholar] [CrossRef]
- Muhtadie, L.; Zhou, Q.; Eisenberg, N.; Wang, Y. Predicting internalizing problems in Chinese children: The unique and interactive effects of parenting and child temperament. Dev. Psychopathol. 2013, 25, 653–667. [Google Scholar] [CrossRef]
- Gong, J.; Zhou, Y.; Wang, Y.; Liang, Z.; Hao, J.; Su, L.; Wang, T.; Du, X.; Zhou, Y.; Wang, Y. How parental smartphone addiction affects adolescent smartphone addiction: The effect of the parent-child relationship and parental bonding. J. Affect. Disord. 2022, 307, 271–277. [Google Scholar] [CrossRef]
- Brown, C.A.; Granero, R.; Ezpeleta, L. The Reciprocal Influence of Callous-Unemotional Traits, Oppositional Defiant Disorder and Parenting Practices in Preschoolers. Child Psychiatry Hum. Dev. 2017, 48, 298–307. [Google Scholar] [CrossRef]
- Villodas, M.T.; Moses, J.O.; Cromer, K.D.; Mendez, L.; Magariño, L.S.; Villodas, F.M.; Bagner, D.M. Feasibility and promise of community providers implementing home-based parent-child interaction therapy for families investigated for child abuse: A pilot randomized controlled trial. Child Abus. Negl. 2021, 117, 105063. [Google Scholar] [CrossRef]
- Parent, J.; Anton, M.T.; Loiselle, R.; Highlander, A.; Breslend, N.; Forehand, R.; Hare, M.; Youngstrom, J.K.; Jones, D.J. A randomized controlled trial of technology-enhanced behavioral parent training: Sustained parent skill use and child outcomes at follow-up. J. Child Psychol. Psychiatry 2022, 63, 992–1001. [Google Scholar] [CrossRef]
- Scudder, A.; Wong, C.; Ober, N.; Hoffman, M.; Toscolani, J.; Handen, B.L. Parent–child interaction therapy (PCIT) in young children with autism spectrum disorder. Child Fam. Behav. Ther. 2019, 41, 201–220. [Google Scholar] [CrossRef]
- Bjørseth, Å.; Wichstrøm, L. Effectiveness of parent-child interaction therapy (PCIT) in the treatment of young children’s behavior problems. A randomized controlled study. PLoS ONE 2016, 11, e0159845. [Google Scholar] [CrossRef]
- Brumariu, L.E.; Kerns, K.A. Pathways to Anxiety: Contributions of Attachment History, Temperament, Peer Competence, and Ability to Manage Intense Emotions. Child Psychiatry Hum. Dev. 2013, 44, 504–515. [Google Scholar] [CrossRef]
- Chen, H.; Xing, J.; Yang, X.; Zhan, K. Heterogeneous Effects of Health Insurance on Rural Children’s Health in China: A Causal Machine Learning Approach. Int. J. Environ. Res. Public Health 2021, 18, 9616. [Google Scholar] [CrossRef]
- Bareinboim, E.; Correa, J.D.; Ibeling, D.; Icard, T. On Pearl’s hierarchy and the foundations of causal inference. In Probabilistic and Causal Inference: The Works of Judea Pearl; ACM: New York, NY, USA, 2022; pp. 507–556. [Google Scholar]
- Pearl, J.; Mackenzie, D. The Book of Why: The New Science of Cause and Effect; Basic Books: New York, NY, USA, 2018. [Google Scholar]
- Montgomery, D.C.; Peck, E.A.; Vining, G.G. Introduction to Linear Regression Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Wang, Y.; Wen, Z.; Li, W.; Fang, J. Methodological research and model development on structural equation models in China’s mainland from 2001 to 2020. Adv. Psychol. Sci. 2022, 30, 1715–1733. [Google Scholar] [CrossRef]
- Athey, S.; Imbens, G. Recursive partitioning for heterogeneous causal effects. Proc. Natl. Acad. Sci. USA 2016, 113, 7353–7360. [Google Scholar] [CrossRef]
- Athey, S.; Wager, S. Estimating treatment effects with causal forests: An application. Obs. Stud. 2019, 5, 37–51. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, H.; Ren, G. Estimating heterogeneous treatment effects in road safety analysis using generalized random forests. Accid. Anal. Prev. 2022, 165, 106507. [Google Scholar] [CrossRef]
- Knittel, C.R.; Stolper, S. Using Machine Learning to Target Treatment: The Case of Household Energy Use (No. w26531); National Bureau of Economic Research: Cambridge, MA, USA, 2019. [Google Scholar] [CrossRef]
- Yoon, J.; Jordon, J.; Van Der Schaar, M. GANITE: Estimation of individualized treatment effects using generative adversarial nets. In Proceedings of the International Conference on Learning Representations, Vancouver, BC, Canada, 30 April–3 May 2018. [Google Scholar]
- Baum, A.; Scarpa, J.; Bruzelius, E.; Tamler, R.; Basu, S.; Faghmous, J. Targeting weight loss interventions to reduce cardiovascular complications of type 2 diabetes: A machine learning-based post-hoc analysis of heterogeneous treatment effects in the Look AHEAD trial. Lancet Diabetes Endocrinol. 2017, 5, 808–815. [Google Scholar] [CrossRef]
- Gong, X.; Hu, M.; Basu, M.; Zhao, L. Heterogeneous treatment effect analysis based on machine-learning methodology. CPT Pharmacomet. Syst. Pharmacol. 2021, 10, 1433–1443. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, I.; Mast, E. Heterogeneity in the effect of federal spending on local crime: Evidence from causal forests. Reg. Sci. Urban Econ. 2019, 78, 103463. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; Text Revision Edition; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Pianta, R.C. Beyond the Parent: The Role of Other Adults in Children’s Lives; Jossey-Bass: San Francisco, CA, USA, 1992. [Google Scholar]
- Zhang, X.; Chen, H.; Zhang, G.; Zhou, B.; Wu, W. A longitudinal study of parent–child relationships and problem behaviors in early childhood: Transactional model. Acta Psychol. Sin. 2008, 40, 571–582. (In Chinese) [Google Scholar] [CrossRef]
- Olson, D.H. Circumplex model of marital and family systems. J. Fam. Ther. 2000, 22, 144–167. [Google Scholar] [CrossRef]
- Phillips, M.R.; West, C.L.; Shen, Q.; Zheng, Y. Comparison of schizophrenic patients’ families and normal families in China, using Chinese versions of FACES-II and the family environment scales. Fam. Process 1998, 37, 95–106. [Google Scholar] [CrossRef]
- Spanier, G.B. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J. Marriage Fam. 1976, 38, 15–28. [Google Scholar] [CrossRef]
- Weaver, S.R.; Prelow, H.M. A mediated-moderation model of maternal parenting style, association with deviant peers, and problem behaviors in urban African American and European American adolescents. J. Child Fam. Stud. 2005, 14, 343–356. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Han, Z.R.; Lei, X.; Qian, J.; Li, P.; Wang, H.; Zhang, X. Parent and child psychopathological symptoms: The mediating role of parental emotion dysregulation. Child Adolesc. Ment. Health 2016, 21, 161–168. [Google Scholar] [CrossRef]
- Shields, A.; Cicchetti, D. Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Dev. Psychol. 1997, 33, 906. [Google Scholar] [CrossRef]
- Athey, S.; Tibshirani, J.; Wager, S. Generalized random forests. Ann. Stat. 2019, 47, 1148–1178. [Google Scholar] [CrossRef]
- Chernozhukov, V.; Demirer, M.; Duflo, E.; Fernandez-Val, I. Generic Machine Learning Inference on Heterogeneous Treatment Effects in Randomized Experiments, with an Application to Immunization in India (No. w24678); National Bureau of Economic Research: Cambridge, MA, USA, 2018. [Google Scholar] [CrossRef]
- Hwang, W.J.; Park, E.H. Developing a structural equation model from Grandey’s emotional regulation model to measure nurses’ emotional labor, job satisfaction, and job performance. Appl. Nurs. Res. 2022, 64, 151557. [Google Scholar] [CrossRef]
- Kong, J.; Lim, J.; Lindsey, D. The longitudinal influence of parent–child relationships and depression on cyber delinquency in South Korean adolescents: A latent growth curve model. Child. Youth Serv. Rev. 2012, 34, 908–913. [Google Scholar] [CrossRef]
- Grant, K.E.; Compas, B.E.; Thurm, A.E.; McMahon, S.D.; Gipson, P.Y.; Campbell, A.J.; Krochock, K.; Westerholm, R.I. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clin. Psychol. Rev. 2006, 26, 257–283. [Google Scholar] [CrossRef]
- Hopkins, J.; Lavigne, J.V.; Gouze, K.R.; LeBailly, S.A.; Bryant, F.B. Multi-domain models of risk factors for depression and anxiety symptoms in preschoolers: Evidence for common and specific factors. J. Abnorm. Child Psychol. 2013, 41, 705–722. [Google Scholar] [CrossRef]
- Morris, A.S.; Criss, M.M.; Silk, J.S.; Houltberg, B.J. The impact of parenting on emotion regulation during childhood and adolescence. Child Dev. Perspect. 2017, 11, 233–238. [Google Scholar] [CrossRef]
- Cruz-Alaniz, Y.; Martin, A.B.; Ballabriga, M. Parents’ executive functions, parenting styles, and oppositional defiant disorder symptoms: A relational model. Univ. Psychol. 2018, 17, 39–48. [Google Scholar]
- Ma, J.; Wan, M.; Yang, L.; Li, J.; Hecht, B.; Teevan, J. Learning causal effects on hypergraphs. In Proceedings of the 28th ACM SIGKDD Conference on Knowledge Discovery and Data Mining, Washington, DC, USA, 14–18 August 2022; pp. 1202–1212. [Google Scholar]


| Improved | Control | t | p | |
|---|---|---|---|---|
| Mean/SD | Mean/SD | |||
| Outcome AODS | 0.94/1.40 | 1.39/1.93 | 2.571 | <0.001 |
| Baseline AODS | 2.12/2.29 | 1.62/2.23 | −2.215 | 0.276 |
| Income | 2.87/0.87 | 3.07/1.05 | 1.970 | 0.066 |
| FACES | 121.97/14.18 | 124.94/15.69 | 1.941 | 0.734 |
| DAS | 134.63/15.08 | 135.13/17.70 | 0.294 | 0.755 |
| API-r | 18.96/3.75 | 17.71/3.63 | −3.367 | 0.444 |
| API-d | 13.88/3.50 | 13.51/3.03 | −1.131 | <0.05 |
| DERS | 76.64/14.07 | 72.98/14.19 | −2.564 | 0.639 |
| ERC | 56.94/11.35 | 52.41/17.88 | −2.834 | <0.001 |
| Estimated | S.E. | p-Value | |
|---|---|---|---|
| 0.94 | 0.16 | <0.001 | |
| 1.37 | 0.36 | <0.001 |
| Estimated | 95% CI | |
|---|---|---|
| ACE | −0.727 | (−0.974, −0.480) |
| ACI | −0.854 | (−0.881, −0.827) |
| ACC | −0.653 | (−0.892, −0.414) |
| Outcome AODS | ||
|---|---|---|
| Predictors | Beta | |
| Model l | 0.505 *** | |
| Baseline AODS | 0.609 *** | |
| Income | −0.035 | |
| FACES | 0.010 | |
| DAS | −0.244 *** | |
| API-r | 0.031 | |
| API-d | −0.116 ** | |
| DERS | −0.011 | |
| ERC | −0.048 | |
| Model 2 | 0.064 *** | |
| Baseline AODS | 0.623 *** | |
| Income | −0.042 | |
| FACES | −0.019 | |
| DAS | −0.193 *** | |
| API-r | 0.052 | |
| API-d | −0.094 ** | |
| DERS | 0.002 | |
| ERC | 0.002 | |
| Change in PCR | −0.266 *** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, H.; Han, F.; Chen, R.; Huang, J.; Chen, J.; Lin, X. Estimating the Heterogeneous Causal Effects of Parent–Child Relationships among Chinese Children with Oppositional Defiant Symptoms: A Machine Learning Approach. Behav. Sci. 2024, 14, 504. https://doi.org/10.3390/bs14060504
Zhou H, Han F, Chen R, Huang J, Chen J, Lin X. Estimating the Heterogeneous Causal Effects of Parent–Child Relationships among Chinese Children with Oppositional Defiant Symptoms: A Machine Learning Approach. Behavioral Sciences. 2024; 14(6):504. https://doi.org/10.3390/bs14060504
Chicago/Turabian StyleZhou, Haiyan, Fengkai Han, Ruoxi Chen, Jiajin Huang, Jianhui Chen, and Xiuyun Lin. 2024. "Estimating the Heterogeneous Causal Effects of Parent–Child Relationships among Chinese Children with Oppositional Defiant Symptoms: A Machine Learning Approach" Behavioral Sciences 14, no. 6: 504. https://doi.org/10.3390/bs14060504
APA StyleZhou, H., Han, F., Chen, R., Huang, J., Chen, J., & Lin, X. (2024). Estimating the Heterogeneous Causal Effects of Parent–Child Relationships among Chinese Children with Oppositional Defiant Symptoms: A Machine Learning Approach. Behavioral Sciences, 14(6), 504. https://doi.org/10.3390/bs14060504





